gullible consumer
In the UK – this post is mainly for UK readers – journalists and opinion leaders are currently falling over themselves reporting about a major breakthrough: an Alzheimer’s drug has been shown to slow the disease by around 36%. “After 20 years with no new Alzheimer’s disease drugs in the UK, we now have two potential new drugs in 12 just months,” wrote Dr Richard Oakley, associate director at the Alzheimer’s Society. And the Daily Mail headlined: “New drug which claims to slow mental decline caused by Alzheimer’s by 36% could spell ‘the beginning of the end’ for the degenerative brain disease”.
That’s excellent news!
Many people will have made a sigh of relief!
So, why does it make me angry?
Once we listen to the news more closely we learn that:
- the drug only works for patients who are diagnosed early;
- for an early diagnosis, we need a PET scan;
- the UK hardly has any PET scanners, in fact, we have the lowest number among developed countries;
- these scanners are very expensive;
- the costs for the new drug are as yet unknown but will also be high.
Collectively these facts mean that we have a major advance in healthcare that could help many patients. At the same time, we all know that this is mere theory and that the practice will be very different.
Why?
- Because the NHS has been run down and is on its knees.
- Because our government will again say that they have invested xy millions into this area.
- The statement might be true or not, but in any case, the funds will be far too little.
- The UK has become a country where some patients suffering from severe toothache currently resort to pulling out their own teeth at home with pairs of pliers.
- In the foreseeable future, the NHS will not be allocated the money to invest in sufficient numbers of PET scans (not to mention the funds to buy the new and expensive drug).
In other words, the UK celebrates yet another medical advance raising many people’s expectations, while everyone in the know is well aware of the fact that the UK public will not benefit from it.
Does that not make you angry too?
It been reported that the German HEILPRAKTIKER, Holger G. has been sentenced to serve a total of 4 years and three months behind bars. He made himself a pair of glasses out of aluminum foil and appeared at the start of his trial wearing a Corona protective mask. The accusations against him were fierce: He was accused of having issued false Corona vaccination certificates en masse in Munich and of having given medication to patients. A woman, who had contracted Corona and had been treated by Holger G. with vitamin solutions, had died last year.
According to the verdict, Holger G. had violated the German Medicines Act. The court announced he was also convicted of 96 counts of dangerous bodily harm and 102 counts of unauthorized trading in prescription drugs. In addition, the court ordered the HEILPRAKTIKER to be placed in a rehab facility.
The 71-year-old MAN had issued Corona vaccination cards since April 2021, without actually vaccinating the people concerned. For the forged vaccination cards, he charged several tens of thousands of Euros. In addition, the former HEILPRAKTIKER illegally sold prescription drugs. The judgment is so severe because Holger G. has form. He also ordered to bear the costs of the proceedings.
___________________________
I have long criticized the German HEILPRAKTIKER. In my recent book on the subject, I make the following points:
– Today, no one can provide reliable data on the number of HEILPRAKTIKER in Germany.
– The training of HEILPRAKTIKER is woefully inadequate.
– The far-reaching rights of the HEILPRAKTIKER are out of proportion to their overt lack of competence.
– This disproportion poses a serious danger to patients.
– This danger is further increased by the fact that there is no effective control of the activity of the HEILPRAKTIKER does not take place.
– Existing laws are almost never applied to the HEILPRAKTIKER.
– Most HEILPRAKTIKER mislead the public unhindered with untenable therapeutic claims.
– The federal government seems to put off over and over again any serious discussion of the HEILPRAKTIKER.
Cases like the one above show that it is high time for reform – or, should that prove impossible, the discontinuation of this utterly obsolete and highly dangerous profession.
An impressive article by John Mac Ghlionn caught my attention. Allow me to quote a few passages from it:
The U.S. House of Representatives and the U.S. Senate recently reintroduced legislation to increase access to Medicare-covered services provided by chiropractors. Last year, the US chiropractic market size was worth $13.13 Billion. By the end of the decade, it will be worth over $18 billion. Each year, a whopping 35 million Americans seek chiropractic care.
But why? It’s a questionable science full of questionable characters.
Last year, a Georgia woman was left paralyzed and unable to speak after receiving a neck adjustment from a chiropractor. She’s not the first person to have had her life utterly ruined by a chiropractor, and chances are she won’t be the last. Many patients who visit chiropractors suffer severe side effects; some lose their lives…
As Dr. Steven Novella has noted, what used to be fraud is now known as holistic medicine. Dr. Edzard Ernst, a retired British-German physician and researcher, has expertly demonstrated the many ways in which chiropractic treatments are rooted not in science, but in mystical concepts…
Spinal adjustments, also known as “subluxations,” are also common. A dangerous practice that has been heavily criticized, spinal manipulations are associated with a number of adverse effects, including the risk of stroke. As Dr. Ernst has noted, the cost-effectiveness of this particular treatment “has not been demonstrated beyond reasonable doubt.”
Not content with spinal and neck manipulations, some chiropractors offer to treat other conditions — like diabetes, for example. They are not trained to treat diabetes. Other chiropractors appear to take joy in torturing infants. In August of 2018, a chiropractor made headlines for all the wrong reasons when a video emerged showing him hanging a two-week-old newborn upside down by the ankles…
Finally, as I alluded to earlier, the chiropractic community is full of fraudsters. In 2019, in the US, 15 chiropractors were charged in an insurance fraud and illegal kickback operation. More recently, in February of this year, a New York federal judge sentenced Patrick Khaziran to 30 months in prison after he pleaded guilty to being part of a widespread scheme that defrauded the NBA out of at least $5 million. In recent times, the chiropractic community has come under scrutiny for abusive care and illegal billing practices. When it comes to instances of healthcare fraud, chiropractic medicine is unrivaled.
None of this should come as a surprise. After all, the entire chiropractic community was constructed on a foundation of lies. As the aforementioned Dr. Ernst told me, we should be skeptical of what chiropractors are offering, largely because the whole practice was founded “by a deluded charlatan, who insisted that all human diseases are due to subluxations of the spine. Today, we know that chiropractic subluxations are mere figments of Palmer’s imagination. Yet, the chiropractic profession is unable to separate itself from the myth. It is easy to see why: without it, they would at best become poorly trained physiotherapists without any raison d’etre.”
… Dr. William T. Jarvis famously referred to chiropractic as “the most significant nonscientific health-care delivery system in the United States.” Comparing the chiropractic community to a cult, Dr. Jarvis wondered, somewhat incredulously, why chiropractors are licensed to practice in all 50 US states. The entire profession, he warned, “should be viewed as a societal problem, not simply as a competitor of regular health-care.”
___________________________
In my view, this is an impressive article, not least because it is refreshingly devoid of the phenomenon known as ‘false balance, e.g. a chiropractor being invited to add his self-interested views at the end of the paper claiming, for instance, “we have years of experience and cause far less harm than real doctors”.
This systematic review evaluated all available randomized controlled trials (RCTs) investigating the clinical effects of hydrotherapy according to Kneipp which is characterized by cold water applications. All RCTs on therapy and prevention with Kneipp hydrotherapy were included. Study participants were patients and healthy volunteers of all age groups. MEDLINE (via PubMed), Scopus, Central, CAMbase, and opengrey.eu were systematically searched through April 2021 without language restrictions and updated by searching PubMed until April 6th 2023. The risk of bias was assessed using the Cochrane tool version 1.
Twenty RCTs (N=4247) were included. Due to the high heterogeneity of the RCTs, no meta-analysis was performed. The risk of bias was rated as unclear in most of the domains. Of 132 comparisons, 46 showed significant positive effects in favor of hydrotherapy on chronic venous insufficiency, menopausal symptoms, fever, cognition, emotional function, and sickness absenteeism. However, 81 comparisons showed no differences between groups, and 5 were in favor of the respective control group. Only half of the studies reported safety issues.
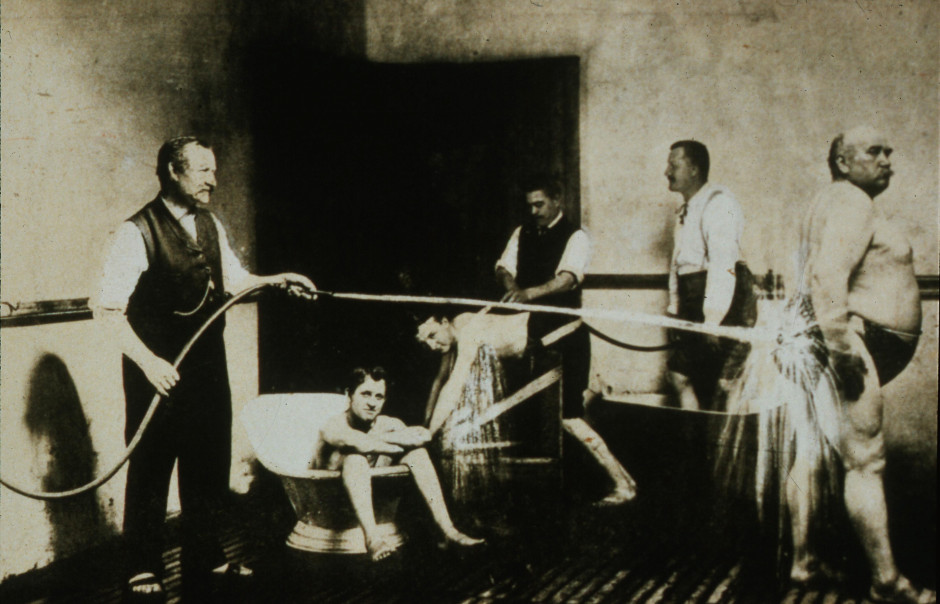
The authors concluded that although RCTs on Kneipp hydrotherapy seem to show positive effects in some conditions and outcomes, it remains difficult to ascertain treatment effects due to the high risk of bias and heterogeneity of most of the considered studies. Further high-quality RCTs on Kneipp hydrotherapy are urgently warranted.
This is certainly the best review of the subject so far. It makes it very clear that the evidence for Kneipp hydrotherapy is weak, mostly because of the many flaws in the primary studies. One needs to add, I think, that 20 RCTs are an absurdly small amount considering that many indications this type of therapy is advocated for – many enthusiasts even consider it a panacea.
It follows, I fear, that Kneipp hydrotherapy is almost entirely not evidence-based. This should be bad news for the numerous institutions and Spa towns (mostly in Germany) that live on employing this treatment and telling patients that it is effective. They usually claim that experience shows this to be true. But this was the mantra of medicine ~100 years ago. Since then, we have learned that experience is a very poor guide that regularly leads us up the garden path.
Kneippians will counter that clinical trials are difficult to conduct and expensive to finance. Both arguments are of course true but, considering that an entire industry lives on telling patients something that essentially amounts to a lie (i.e. the claim that it works), it surely is obligatory to overcome these obstacles.
This review assessed the role of homoeopathy in the therapeutic management of substance use disorders (SUD) through a systematic web-based literature search. A comprehensive search was conducted online and manually to identify homoeopathic research studies published between 1993 and 2022 on SUD in international databases and the Central Council of Research in Homoeopathy library. Relevant studies were categorised and assessed in terms of study designs, number of participants, evidence grades and clinical outcome parameters. A total of 21 full-text studies were screened and evaluated. Risk of bias (RoB) was assessed for all studies and model validity was appraised for the included RCTs’.
10 studies were included:
- 3 Randomised Controlled Trials,
- 3 Observational studies,
- 1 Pilot study,
- 1 observational comparative study,
- 1 retrospective cohort study,
- 1 case series.
Three studies have a level of evidence of 1b with an ‘A’ grade of recommendation, which consists of the RCTs only. The most commonly prescribed medicines identified were:
- Arsenic album,
- Nux vomica,
- Lycopodium,
- Pulsatilla,
- Sulphur,
- Staphysagria,
- Belladonna,
- Ipecac,
- Chamomilla,
- Rhustox,
- Phosphorus,
- Lachesis.
A high risk of bias was elicited in most of the observational studies accentuating the need for more robust methodological studies.
The authors concluded that the majority of the studies have a small number of recruitments. Pragmatic studies with larger sample sizes and validated outcome measures may be designed further to validate the
promising role of homoeopathic medicines in SUDs and generate quality evidence.
The paper is surprising! Most of the studies are not RCTs and thus cannot come even near suggesting a causal effect of homeopathy. The three RCTs are the following:
- Manchanda RK, Janardanan Nair KR, Varanasi R, Oberai P, Bhuvaneswari R, Bhalerao R, et al. A randomised comparative trial in the management of alcohol dependence: Individualised homoeopathy versus standard allopathic treatment. Indian J Res Homoeopathy; 2016.
- Adler UC, Acorinte AC, Calzavara FO, et al. Double-blind evaluation of homeopathy on cocaine craving: A randomised controlled pilot study. J Integr Med. 2018; 16(3):178-184.
- Grover A, Bhushan B, Goel R. Double-blind placebo-controlled trial of homoeopathic medicines in the
management of withdrawal symptoms in opium addicts and its alkaloid derivatives dependents. Indian J Res Homoeopathy. 2009;3:41-4.
All of these 3 studies were assessed by the review authors as having major flaws. Only one is available on Medline:
Background: Brazil is among the nations with the greatest rates of annual cocaine usage. Pharmacological treatment of cocaine addiction is still limited, opening space for nonconventional interventions. Homeopathic Q-potencies of opium and Erythroxylum coca have been tested in the integrative treatment of cocaine craving among homeless addicts, but this setting had not proven feasible, due to insufficient recruitment.
Objective: This study investigates the effectiveness and tolerability of homeopathic Q-potencies of opium and E. coca in the integrative treatment of cocaine craving in a community-based psychosocial rehabilitation setting.
Design, setting, participants, and interventions: A randomized, double-blind, placebo-controlled, parallel-group, eight-week pilot trial was performed at the Psychosocial Attention Center for Alcohol and Other Drugs (CAPS-AD), Sao Carlos/SP, Brazil. Eligible subjects included CAPS-AD patients between 18 and 65 years of age, with an International Classification of Diseases-10 diagnosis of cocaine dependence (F14.2). The patients were randomly assigned to two treatment groups: psychosocial rehabilitation plus homeopathic Q-potencies of opium and E. coca (homeopathy group), and psychosocial rehabilitation plus indistinguishable placebo (placebo group).
Main outcome measures: The main outcome measure was the percentage of cocaine-using days. Secondary measures were the Minnesota Cocaine Craving Scale and 12-Item Short-Form Health Survey scores. Adverse events were reported in both groups.
Results: The study population comprised 54 patients who attended at least one post-baseline assessment, out of the 104 subjects initially enrolled. The mean percentage of cocaine-using days in the homeopathy group was 18.1% (standard deviation (SD): 22.3%), compared to 29.8% (SD: 30.6%) in the placebo group (P < 0.01). Analysis of the Minnesota Cocaine Craving Scale scores showed no between-group differences in the intensity of cravings, but results significantly favored homeopathy over placebo in the proportion of weeks without craving episodes and the patients’ appraisal of treatment efficacy for reduction of cravings. Analysis of 12-Item Short-Form Health Survey scores found no significant differences. Few adverse events were reported: 0.57 adverse events/patient in the homeopathy group compared to 0.69 adverse events/patient in the placebo group (P = 0.41).
Conclusions: A psychosocial rehabilitation setting improved recruitment but was not sufficient to decrease dropout frequency among Brazilian cocaine treatment seekers. Psychosocial rehabilitation plus homeopathic Q-potencies of opium and E. coca were more effective than psychosocial rehabilitation alone in reducing cocaine cravings. Due to high dropout rate and risk of bias, further research is required to confirm our findings, with specific focus on strategies to increase patient retention.
This study can hardly be said to show convincing evidence for homeopathy.
This paper is all the more surprising if we consider the affiliations of the authors:
- Clinical Research Unit (H), Aizawl under Central Council for Research in Homoeopathy, Ministry of AYUSH, Govt. of India, India.
- All India Institute of Ayurveda, New Delhi, India.
- Department of Materia Medica, Madhav Homoeopathic Medical College and Hospital, Madhav Hills,
Opposite Banas River, Abu Road, Rajasthan, India.
It is time, I think, that Indian officials and researchers learn some critical thinking and formulate the conclusions of reviews based on the evidence they produced. This would be a start:
Our review has not generated convincing evidence to suggest that homeopathy is effective in treating SUDs.
Guest post by Ken McLeod
Readers will have no trouble recalling that crank ‘naturopath’ Barbara O’Neill has graced these pages several times. She is subject to a Permanent Prohibition Order by the New South Wales Health Care Complaints Commission. It goes like this:
“The Commission is satisfied that Mrs O’Neill poses a risk to the health and safety of members of the public and therefore makes the following prohibition order:
“Mrs O’Neill is permanently prohibited from providing any health services, as defined in s4 Of the Health Care Complaints Act 1993, whether in a paid or voluntary capacity.’ 1
Evidently Ms O’Neill has scrambled her chakras or muddled her meridians because she continues to forget the Order. For example;
O’Neill did a video interview concerning the Prohibition Order and that has been posted online at YouTube.2 The video was posted ‘1 year ago,’ has had 323,000 views and had 1,598 comments. She goes into great detail what she regards as the appalling treatment at the hands of the HCCC.
In the video she admits that she has continued to travel the world spreading her lies and misrepresentations. Some of the lies are that she is a naturopath, and was a nurse, and ‘I used to work in the Operating Theatre as a psychiatric nurse….’
In the video at 53:20 in the video she refers to an aboriginal man ‘Dan’ who works at her Misty Mountain Lifestyle Retreat, (note the present tense), who is in his 50s was obese and recently had a heart attack, ‘was on a lot of medications,’ ‘was a bit scared of coming off medications,’ ‘I said Dan, I think it’s time to stop your blood pressure medications, you’re going too low, you’re a 100 over 60,’ ‘three days later his blood pressure was 100 over 75,….’ 3
Call me a cynic, but that strikes me as rather dangerous advice, worthy of an investigation by the HCCC. Meanwhile, there is no sign of ‘Dan ‘ in Misty Mountain’s ‘About page.’ Dan’s brother Dave appears, but no Dan.4 Could it be that O’Neill’s advice led to some incapacity? Tips are welcome.
Meanwhile, readers could learn much more about Barbara O’Neill at Wikipedia.5
This article first appeared in the June issue of the Australian Skeptic Magazine,6 reprinted with kind permission.
REFERENCES
1 https://www.hccc.nsw.gov.au/decisions-orders/public-statements-and-warnings/public-statement-and-statement-of-decision-in-relation-to-in-relation-to-mrs-barbara-o-neill
2 https://www.youtube.com/watch?v=tsbK5TLdAPo
3 This was dangerous and reckless advice. The full transcript is here
4 https://www.mmh.com.au/our-story
5 https://en.wikipedia.org/wiki/Barbara_O%27Neill
6 https://www.skeptics.com.au/magazine/
It has been reported that a GP has been erased from the medical register after a disciplinary tribunal concluded yesterday that her statements on vaccines amounted to misconduct.
Dr Jayne Donegan, who no longer works as an NHS GP, was found by the tribunal to have ‘encouraged parents to mislead healthcare professionals about their children’s diet or immunization history’. The UK General Medical Council (GMC) brought several allegations against Dr Donegan, about statements made between 2019 and 2020, however, the determination of impaired fitness to practise (FTP) and subsequent erasure was based solely on her suggestions to parents.
The tribunal determined that her misconduct ‘posed an ongoing risk to patient safety given her lack of insight and lack of remediation’ and that ‘public confidence would be undermined’ if such a doctor was allowed to remain in practice. An immediate order of suspension was imposed, which the tribunal determined necessary for the ‘protection of the public’. Other GMC allegations, such as Dr. Donegan’s statements failing to ‘give balanced information on the risks and benefits of immunization’, were proved true by the tribunal but were not determined to be serious misconduct.
Dr. Donegan works as a homeopathic and naturopathic practitioner and has been ‘researching disease ecology and vaccination since 1994’, according to her website. The tribunal considered statements made by Dr. Donegan in a consultation with an undercover reporter and during her lectures on vaccination. She had said that the historical decline in deaths from whooping cough was because of sanitation and surgeons, not vaccinations. She had also suggested to audiences at her lectures that they could avoid answering questions from healthcare professionals about their child’s immunization history. When asked by an audience member about this, Dr. Donegan had said: ‘I thought what am I going to do because if I were you, I could just forge something but I can’t do that because I am a doctor and I would get struck off and I really would get struck off. What can I do? I thought maybe I can do something homeopathic because they are not having it. In the meantime, I wrote “Yes, I’ll get it done” thinking what will I do and they never came back to me, so when the next one went I just said “yes. The main thing is, don’t stick your head above the parapet because you make it difficult for them. If you say they are not vaccinated, they say they can’t go on the trip or they say “They could but the insurers won’t insure us”, so just keep saying “yes” but don’t say I said that.’
The tribunal concluded that comments like this made it clear Dr. Donegan was aware this was a ‘serious matter that could result in her being struck off’, despite her defense that she was simply ‘making people laugh’. The MPTS tribunal chair Mr Julian Weinberg said: ‘The Tribunal considered that honest and accurate communication of an individual’s medical history forms an essential part of ongoing patient healthcare and that any attempt to undermine this risks the safety of patients. It noted that whilst no dishonesty was found against Dr. Donegan, the Tribunal has found that she encouraged parents to be dishonest with healthcare professionals by, for example, forging medical documents/records, thereby undermined this essential quality of the doctor/patient relationship.’ Mr Weinberg highlighted that the tribunal’s findings did not concern ‘the rights or wrongs of her views on immunization’ but rather her encouragement to parents to mislead healthcare professionals.
Dr. Donegan said in response to the decision: ‘I boycotted the GMC’s political show trial against me which ended today. Serious irregularities include bogus dishonesty charges and bogus accusations that I put newborns at risk of serious harm.’ She added: ‘Being struck off by a corrupt GMC is a small price to pay for taking a lawful ethical stand for the safety of British children.’
Apparently, Dr. Donegan even claimed that she is delighted to be struck off the register of medical practitioners – and so, I presume, are many of us reading this post!
I have seen some daft meta-analyses in my time – this one, however, takes the biscuit. Here is its unaltered abstract:
Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
___________________________
This meta-analysis has too many serious flaws to mention. Let me therefore just focus on the main two:
- Craniosacral Therapy is not an MBMBT.
- Craniosacral Therapy is not effective for NLBP. The false positive result was generated on the basis of 4 studies. All of them have serious methodological problems that prevent an overall positive conclusion about the effectiveness of this treatment. In case you don’t believe me, here are the 4 abstracts:
1) Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
2) Background: Craniosacral therapy (CST) and sensorimotor training (SMT) are two recommended interventions for nonspecific chronic low back pain (NCLBP). This study compares the effects of CST and SMT on pain, functional disability, depression and quality of life in patients with NCLBP.
Methodology: A total of 31 patients with NCLBP were randomly assigned to the CST group (n=16) and SMT (n=15). The study patients received 10 sessions of interventions during 5 weeks. Visual analogue scale (VAS), Oswestry disability index (ODI), Beck depression inventory-II (BDI-II), and Short Form-36 (SF-36) questionnaires were used at baseline (before the treatment), after the treatment, and 2 months after the last intervention session. Results were compared and analyzed statistically.
Results: Both groups showed significant improvement from baseline to after treatment (p < 0.05). In the CST group, this improvement continued during the follow-up period in all outcomes (p < 0.05), except role emotional domain of SF-36. In the SMT group, VAS, ODI and BDI-II increased during follow-up. Also, all domains of SF-36 decreased over this period. Results of group analysis indicate a significant difference between groups at the end of treatment phase (p < 0.05), except social functioning.
Conclusions: Results of our research confirm that 10 sessions of craniosacral therapy (CST) or sensorimotor training (SMT) can significantly control pain, disability, depression, and quality of life in patients with NCLBP; but the efficacy of CST is significantly better than SMT.
3) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
4) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
_______________________________
I REST MY CASE
“A Nutrient Mix Designed at the Dr. Rath Research Institute is Effective Against Different Types of Coronavirus.” With these words (and the picture below), the ‘Dr. Rath Research Institute’ recently announced its sensational finding on Twitter.
Clicking on the link they provided, got me to the following article:
In this new study we wanted to find out whether certain natural substances could help fight against SARS-CoV-2 (the virus that causes COVID-19), and another type of coronavirus known as HCoV-229E which infects humans and is associated with the common cold and its symptoms.
The importance of the study relates to the fact that COVID-19 is still a big problem, especially for older people and those with weak immune systems. Current approaches using RNA- and DNA -based vaccines are not effective in preventing the infection and spread of SARS-CoV-2, or its variants such as Omicron. The anti-viral drugs used against the pandemic are similarly not fully effective. It is therefore important to develop other approaches, especially those involving safe, natural substances, that could be used alongside or instead of conventional treatments.
For the study, scientists at the Dr. Rath Research Institute used a combination of natural substances including vitamin C, polyphenols, and other nutrients. They gave the nutrient mix to mice infected with one or other of the two types of coronaviruses, to see if it could reduce the numbers of viral particles and spike proteins in the animals’ lungs.
Based on our earlier work using human cells growing in culture we already knew that the combination of nutrients in this mixture was effective in controlling key cellular mechanisms of SARS-CoV-2 infection, including inhibiting the multiplication of the virus.
We had found that the nutrient mix could inhibit an enzyme, RNA-dependent RNA polymerase (RdRp), which is needed for a virus to make copies of itself. The mix was also effective in preventing viral spike protein from binding to cell surfaces and entering cells. It additionally worked in decreasing the number of so-called ACE2 receptor proteins, which are expressed by cells in the lungs, blood vessels, and other organs, and that help the virus to get into cells.
In this latest study the nutrient mix was administered daily to mice infected with either SARS-CoV-2 or HCoV-229E, to see if it could reduce infectivity in terms of the amounts of viral particles and spike proteins found in the lungs. Infected mice in the control group were fed a normal diet without nutrient supplementation. The amounts of viral particles and spike proteins in the lungs were evaluated using special molecular-based tests. We also examined the effects of the nutrient mix on the presence of immune cells in the lungs, as an indication of tissue inflammation.
The results showed that, compared to mice in the control group, the nutrients significantly reduced the amounts of viral particles and spike proteins in the lungs of infected mice. Moreover, the mix was equally effective in mice infected with either of the two types of coronaviruses. This indicates that the nutrients affected common mechanisms of infection and were not specific to a particular type of virus. It also explains the results of our previous studies, which showed that the nutrient mix was effective in stopping SARS-CoV-2 and several of its mutated forms, including Omicron variants, from entering the cells.
Crucially, we found the nutrient mix affected not only the virus itself; it also reduced the ability of the virus to enter cells by decreasing the number of ACE2 receptors on cell surfaces. In the presence of inflammation, which is commonly associated with infections, there were similarly less ACE2 receptors on cells. Nutrient anti-inflammatory effects were also observed in the lung tissue of the mice.
In conclusion, our study showed that the nutrient mix could help reduce the infectivity of SARS-CoV-2 and the associated common cold virus HCoV-229E in mice at different stages of infectivity. The fact that different mechanisms were affected simultaneously demonstrates the superior efficacy of nutrients compared to drugs, the latter of which usually target only a single mechanism and allow the virus to escape by mutating.
The unique composition and efficacy of our nutrient mix has been awarded US and international patents. While more research is needed in order to fully confirm its efficacy in human clinical trials, the application of this safe micronutrient combination as soon as possible should ultimately benefit people worldwide and save on healthcare costs.
So, the claim that a Nutrient Mix is “Effective Against Different Types of Coronavirus” rests on some lousy experiments on rats?
Might we call this misleading or dishonest?
And what is the Dr. Rath Research Institute?
Could it belong to the Dr. Rath Foundation?
The very foundation that once published this about me:
Professor Edzard Ernst: A Career Built On Discrediting Natural Health Science?
Professor Edzard Ernst, a retired German physician and academic, has recently become a prominent advocate of plans that could potentially outlaw the entire profession of naturopathic doctors in Germany. Promoting the nonsensical idea that naturopathic medicine somehow poses a risk to public health, Ernst attacks its practitioners as supposedly having been educated in “nonsense”. Tellingly, however, given that he himself has seemingly not published even so much as one completely original scientific trial of his own, Ernst’s apparent attempts to discredit natural healthcare approaches are largely reliant instead on his analysis or review of handpicked negative studies carried out by others.
SAY NO MORE!
A German paper reported the following horrific story about a Heilpraktiker, an alternative practitioner without a medical degree:
Starting July 7, Torben K. (46) from Solingen will have to answer to the Wuppertal Regional Court. The Heilpraktiker is said to have injected silicone oil into the penis and testicles of a man († 32) at his request. Shortly thereafter, the patient developed health problems and later died.
The prosecution accuses the Heilpraktiker from Solingen of bodily injury resulting in death and violation of the Heilpraktikergesetz.
According to the report, the victim had traveled to Solingen in June 2019, where the defendant had given him the injection in his apartment.
Back home, the 32-year-old patient suddenly developed shortness of breath, had to be hospitalized, then transferred to the university hospital in Giessen. Seven months after the injection, he is dead. According to the indictment, the patient suffered multiple organ failure as a result of blood poisoning.
Three days of trial are scheduled. The defendant faces up to 15 years in prison.
_________________________
I had never heard of intra-testicular injections. So, I did a Medline search and found just two papers of the procedure in human patients:
Blunt trauma is the most common mechanism of injury to the scrotum and testicle. Surgical exploration with primary repair, hematoma evacuation, and de-torsion are common surgical interventions. A 20-year-old male with no previous medical history presented after a high-speed motor vehicle collision. Ultrasonography demonstrated heterogeneous changes of the tunica albuginea and decreased arterial flow to bilateral testicles. He was subsequently taken to the operating room for surgical exploration, which revealed bilateral mottled testes with questionable viability. Papaverine was injected into each testicle, which resulted in visibly increased perfusion and subsequent preservation of the testicles. Conclusion: Current evidence on the use of papaverine is isolated to testicular torsion. Additional research should be conducted on the use of papaverine in blunt testicular trauma. Papaverine injection may be a valuable treatment option when inadequate perfusion is observed intra-operatively.
No 2:
Purpose: We describe a simple technique to deliver local anaesthetic for percutaneous testis biopsies.
Materials and methods: With the testis held firmly, a 25 gage needle is used to inject lidocaine, without epinephrine, into the skin and dartos superficial to the testis, then the needle is advanced through the tunica albuginea and 0.5 mL to 1.0 mL of lidocaine is injected directly into the testis. The testis becomes slightly more turgid with the injection. A percutaneous biopsy is then immediately performed.
Results: Intra-testicular lidocaine, (without the need of a cord block or any sedation) was used on a total of 45 consecutive patients having percutaneous testicular biopsies. Procedure time was short (averages less than 5 minutes) and anaesthesia was profound. There was no change in the number of seminiferous tubules for evaluation compared to biopsies on men using a cord block. Only 1/45 men had a post-procedure testicular hematoma (this resolved in 4 weeks).
Conclusions: Intra-testicular lidocaine appears to be a simple, rapid and safe method to provide anaesthesia for a percutaneous testis biopsy.
All the other papers on intra-testicular injections were about animal experiments, mostly for exploring means of castration. This renders the above case even more unusual. The Heilpraktiker’s defense might stress that the patient wanted the treatment. That may be so but is it a valid excuse? No, of course not. In my view – and I am just a medic, not a lawyer – the Heilpraktiker is responsible for the treatment regardless of how much the patient insisted on it.




