fallacy
This case report aims to describe the effects of craniosacral therapy and acupuncture in a patient with chronic migraine.
A 33-year-old man with chronic migraine was treated with 20 sessions of craniosacral therapy and acupuncture for 8 weeks. The number of migraine and headache days were monitored every month. The pain intensity of headache was measured on the visual analog scale (VAS). Korean Headache Impact Test-6 (HIT-6) and Migraine Specific Quality of Life (MSQoL) were also used.
The number of headache days per month reduced from 28 to 7 after 8 weeks of treatment and to 3 after 3 months of treatment. The pain intensity of headache based on VAS reduced from 7.5 to 3 after 8 weeks and further to < 1 after 3 months of treatment. Furthermore, the patient’s HIT-6 and MSQoL scores improved during the treatment period, which was maintained or further improved at the 3 month follow-up. No side effects were observed during or after the treatment.
The authors concluded that this case indicates that craniosacral therapy and acupuncture could be effective treatments for chronic
migraine. Further studies are required to validate the efficacy of craniosacral therapy for chronic migraine.
So, was the treatment period 8 weeks long or was it 3 months?
No, I am not discussing this article merely for making a fairly petty point. The reason I mention it is diffteren. I think it is time to discuss the relevance of case reports.
What is the purpose of a case report in medicine/healthcare. Here is the abstract of an article entitled “The Importance of Writing and Publishing Case Reports During Medical Training“:
Case reports are valuable resources of unusual information that may lead to new research and advances in clinical practice. Many journals and medical databases recognize the time-honored importance of case reports as a valuable source of new ideas and information in clinical medicine. There are published editorials available on the continued importance of open-access case reports in our modern information-flowing world. Writing case reports is an academic duty with an artistic element.
An article in the BMJ is, I think, more informative:
It is common practice in medicine that when we come across an interesting case with an unusual presentation or a surprise twist, we must tell the rest of the medical world. This is how we continue our lifelong learning and aid faster diagnosis and treatment for patients.
It usually falls to the junior to write up the case, so here are a few simple tips to get you started.
First steps
Begin by sitting down with your medical team to discuss the interesting aspects of the case and the learning points to highlight. Ideally, a registrar or middle grade will mentor you and give you guidance. Another junior doctor or medical student may also be keen to be involved. Allocate jobs to split the workload, set a deadline and work timeframe, and discuss the order in which the authors will be listed. All listed authors should contribute substantially, with the person doing most of the work put first and the guarantor (usually the most senior team member) at the end.
Getting consent
Gain permission and written consent to write up the case from the patient or parents, if your patient is a child, and keep a copy because you will need it later for submission to journals.
Information gathering
Gather all the information from the medical notes and the hospital’s electronic systems, including copies of blood results and imaging, as medical notes often disappear when the patient is discharged and are notoriously difficult to find again. Remember to anonymise the data according to your local hospital policy.
Writing up
Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Coming up with a title
Discuss a title with your supervisor and other members of the team, as this provides the focus for your article. The title should be concise and interesting but should also enable people to find it in medical literature search engines. Also think about how you will present your case study—for example, a poster presentation or scientific paper—and consider potential journals or conferences, as you may need to write in a particular style or format.
Background research
Research the disease/pathology that is the focus of your article and write a background paragraph or two, highlighting the relevance of your case report in relation to this. If you are struggling, seek the opinion of a specialist who may know of relevant articles or texts. Another good resource is your hospital library, where staff are often more than happy to help with literature searches.
How your case is different
Move on to explore how the case presented differently to the admitting team. Alternatively, if your report is focused on management, explore the difficulties the team came across and alternative options for treatment.
Conclusion
Finish by explaining why your case report adds to the medical literature and highlight any learning points.
Writing an abstract
The abstract should be no longer than 100-200 words and should highlight all your key points concisely. This can be harder than writing the full article and needs special care as it will be used to judge whether your case is accepted for presentation or publication.
What next
Discuss with your supervisor or team about options for presenting or publishing your case report. At the very least, you should present your article locally within a departmental or team meeting or at a hospital grand round. Well done!
Both papers agree that case reports can be important. They may provide valuable resources of unusual information that may lead to new research and advances in clinical practice and should offer an interesting case with an unusual presentation or a surprise twist.
I agree!
But perhaps it is more constructive to consider what a case report cannot do.
It cannot provide evidence about the effectiveness of a therapy. To publish something like:
- I had a patient with the common condition xy;
- I treated her with therapy yz;
- this was followed by patient feeling better;
is totally bonkers – even more so if the outcome was subjective and the therapy consisted of more than one intervention, as in the article above. We have no means of telling whether it was treatment A, or treatment B, or a placebo effect, or the regression towards the mean, or the natural history of the condition that caused the outcome. The authors might just as well just have reported:
WE RECENTLY TREATED A PATIENT WHO GOT BETTER
full stop.
Sadly – and this is the reason why I spend some time on this subject – this sort of thing happens very often in the realm of SCAM.
Case reports are particularly valuable if they enable and stimulate others to do more research on a defined and under-researched issue (e.g. an adverse effect of a therapy). Case reports like the one above do not do this. They are a waste of space and tend to be abused as some sort of indication that the treatments in question might be valuable.
So-called alternative medicine (SCAM) is widely used in Saudi Arabia. One of the common practices is the use of camel urine alone or mixed with camel milk for the treatment of cancer, which is often supported by religious beliefs.
This study observed cancer patients who insisted on using camel urine, and to offer some clinically relevant recommendations. The authors observed 20 cancer patients (15 male, 5 female) from September 2020 to January 2022 who insisted on using camel urine for treatment. They documented the demographics of each patient, the method of administering the urine, reasons for refusing conventional treatment, period of follow-up, and the outcome and side effects.
All the patients had radiological investigations before and after their treatment with camel urine. All of them used a combination of camel urine and camel milk, and their treatment ranged from a few days to 6 months. They consumed an average of 60 ml urine/milk per day. No clinical benefit was observed after the treatment; 2 patients developed brucellosis. Eleven patients changed their mind and accepted conventional antineoplastic treatment and 7 were too weak to receive further treatment; they died from the disease.
The authors concluded that camel urine had no clinical benefits for any of the cancer patients, it may even have caused zoonotic infection. The promotion of camel urine as a traditional medicine should be stopped because there is no scientific evidence to support it.
If you suspected that this was a hoax, you were wrong!
Here is a recent paper on the ‘therapeutic potentials of camel urine’:
Camel urine has traditionally been used to treat multiple human diseases and possesses the most beneficial effects amongst the urine of other animals. However, scientific review evaluating the anticancer, antiplatelet, gastroprotective and hepatoprotective effects of camel urine is still scarce. Thus, this scoping review aimed to provide scientific evidence on the therapeutic potentials of camel urine. Three databases were searched to identify relevant articles (Web of Science, PubMed and Scopus) up to September 2020. Original articles published in English that investigated the effects of camel urine in various diseases were included. The literature search identified six potential articles that met all the inclusion criteria. Three articles showed that camel urine possesses cytotoxic activities against different types of cancer cells. Two studies revealed camel urine’s protective effects against liver toxicity and gastric ulcers, whilst another study showed the role of camel urine as an antiplatelet agent. All studies demonstrated significant positive effects with different effective dosages. Thus, camel urine shows promising therapeutic potential in treating human diseases, especially cancer. However, the standardised dosage and potential side effects should be determined before camel urine could be offered as an alternative treatment.
I have often asked myself the question whether some SCAMs are too absurd to merit scientific study. Over the years, I changed my mind on it; while initially I tended to answer it in the negative, I now think that YES: some ideas – even those that are ancient and, as Charles Windsor would argue, have thus stood the ‘test of time’ – are not worth the effort. Camel urine as a therapy might well be one of them.
Homeopathic remedies are highly diluted formulations without proven clinical benefits, traditionally believed not to cause adverse events. Nonetheless, published literature reveals severe local and non–liver-related systemic side effects. Here is the first series on homeopathy-related severe drug-induced liver injury (DILI) from a single center.
A retrospective review of records from January 2019 to February 2022 identified 9 patients with liver injury attributed to homeopathic formulations. Competing causes were comprehensively excluded. Chemical analysis was performed on retrieved formulations using triple quadrupole gas chromatography-mass spectrometry and inductively coupled plasma atomic emission spectroscopy.
Males predominated with a median age of 54 years. The most typical clinical presentation was acute hepatitis, followed by acute or chronic liver failure. All patients developed jaundice, and ascites were notable in one-third of the patients. Five patients had underlying chronic liver disease. COVID-19 prevention was the most common indication for homeopathic use. Probable DILI was seen in 77.8%, and hepatocellular injury predominated (66.7%). Four (44.4%) patients died (3 with chronic liver disease) at a median follow-up of 194 days. Liver histopathology showed necrosis, portal and lobular neutrophilic inflammation, and eosinophilic infiltration with cholestasis. A total of 29 remedies were consumed between 9 patients, and 15 formulations were analyzed. Toxicology revealed industrial solvents, corticosteroids, antibiotics, sedatives, synthetic opioids, heavy metals, and toxic phyto-compounds, even in ‘supposed’ ultra-dilute formulations.
The authors concluded that homeopathic remedies potentially result in severe liver injury, leading to death in those with underlying liver disease. The use of mother tinctures, insufficient dilution, poor manufacturing practices, adulteration and contamination, and the presence of direct hepatotoxic herbals were the reasons for toxicity. Physicians, the public, and patients must realize that Homeopathic drugs are not ‘gentle placebos.’
The authors also cite our own work on this subject:
A detailed systematic review of homeopathic remedies-induced adverse events from published case reports and case series by Posadzski and colleagues showed that severe side effects, some leading to fatality, are possible with classic and unspecified homeopathic formulations. The total number of patients included was 1159, of which 1142 suffered adverse events directly related to homeopathy. The direct adverse events had acute pancreatitis, severe allergic reactions, arsenical keratosis, bullous pemphigoid, neurocognitive disorders, sudden cardiac arrest and coma, severe dyselectrolytemia, interstitial nephritis, kidney injury, thallium poisoning, syncopal attacks, and focal neurological deficits as well as movement disorders. Fatal events involved advanced renal failure requiring dialysis, toxic polyneuropathy, and quadriparesis. The duration of adverse events ranged from a few hours to 7 months, and 4 patients died. The authors state that in most cases, the mechanism of action for side effects of homeopathy involved allergic reactions or the presence of toxic substances—the use of strong mother tinctures, drug contaminants, adulterants, or poor manufacturing (incorrect dilutions).
When we published our paper back in 2012, it led to a seies of angry responses from defenders of homeopathy who claimed that one cannot ‘have the cake and eat it’; either homeopathic remedies are placebos and thus harmless, or they have effects and thus also side-effects, they claimed. As the new publication by Indian researchers yet again shows, they were mistaken. In fact, homeopathy is dangerous in more than one way:
- the homeopathic remedies can do harm if not diluted or wrongly manufactured;
- the homeopaths can do harm through their often wrong advice in health matters;
- homeopathy erodes rational thinking (as, for instance, the resopnses to our 2012 paper demonstrated).
The aim of this systematic review was to update the current level of evidence for spinal manipulation in influencing various biochemical markers in healthy and/or symptomatic population.
Various databases were searched (inception till May 2023) and fifteen trials (737 participants) that met the inclusion criteria were included in the review. Two authors independently screened, extracted and assessed the risk of bias in included studies. Outcome measure data were synthesized using standard mean differences and meta-analysis for the primary outcome (biochemical markers). The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) was used for assessing the quality of the body of evidence for each outcome of interest.
There was low-quality evidence that spinal manipulation influenced various biochemical markers (not pooled). There was low-quality evidence of significant difference that spinal manipulation is better (SMD -0.42, 95% CI – 0.74 to -0.1) than control in eliciting changes in cortisol levels immediately after intervention. Low-quality evidence further indicated (not pooled) that spinal manipulation can influence inflammatory markers such as interleukins levels post-intervention. There was also very low-quality evidence that spinal manipulation does not influence substance-P, neurotensin, oxytocin, orexin-A, testosterone and epinephrine/nor-epinephrine.
The authors concluded that spinal manipulation may influence inflammatory and cortisol post-intervention. However, the wider prediction intervals in most outcome measures point to the need for future research to clarify and establish the clinical relevance of these changes.
The majority of the studies were of low or very low quality. This means that the collective evidence is less than reliable. In turn, this means, I think, that the conclusions are misleading. A more honest conclusion would be this:
There is no reliable evidence that spinal manipulation influences inflammatory and cortisol levels.
As for the clinical relevance, I would like to point out that it would not be surprising if chiropractors could one day convincingly show that spinal manipulation do influence various biochemical markers. Many things do! If you fall down a staircase, for instance, plenty of biochemical markers will be affected. This, however, does not mean that throwing our patients down the stairs is of therapeutic value.
The objectives of this randomized double-blind placebo-controlled clinical trial were to determine if there:
- (a) is an overall effect of homeopathic treatment (homeopathic medicines plus consultation) in the treatment of ADHD;
- (b) are any specific effects the homeopathic consultation alone in the treatment of ADHD;
- (c) are any specific effects of homeopathic medicines in the treatment of ADHD.
Children aged 6–16 years diagnosed with ADHD were randomized to one of three arms:
- Arm 1 (Remedy and Consultation);
- Arm 2 (Placebo and Consultation);
- Arm 3 (Usual Care).
The primary outcome measure was the change of the Conner 3 Global Index-Parent T-score (CGI-P T score) between baseline and 28 weeks.
The results showed an improvement in ADHD symptoms as measured by the CGI-P T score in the two groups (Arms 1 and 2) that received consultations with a homeopathic practitioner when compared with the usual care control group (Arm 3). Parents of the children in the study who received homeopathic consultations (Arms 1 and 2) also reported greater coping efficacy compared with those receiving usual care (Arm 3). There was no difference in adverse events among the three study arms.
The authors concluded that, in this study, homeopathic consultations provided over 8 months with the use of homeopathic remedy was associated with a decrease in ADHD symptoms in children aging 6–16 years when compared with usual treatment alone. Children treated with homeopathic consultations and placebo experienced a similar decrease in ADHD symptoms; however, this finding did not reach statistical significance when correcting for multiple comparisons. Homeopathic remedies in and of themselves were not associated with any change in ADHD symptoms.
In the discussion section, the authors make their findings a little clearer: “The findings are generally consistent with a recent meta-analysis that concluded that (i)ndividualized homeopathy showed a clinically relevant and statistically robust effect in the treatment of ADHD. Similar to the meta-analysis, the authors found individualized homeopathy (consultation plus remedy) resulted in improvement in ADHD symptoms. However, the data suggest that this effect is not due to the remedy component of the intervention.”
The authors do not cite the (to the best of my knowledge) only study that had a very similar aim, namely differentiating between the effects of the homeopathic remedy and the homeopathic consultation. It was conducted by the late George Lweith who certainly was not against homeopathy. The conclusions of this trial were as follows: Homeopathic consultations but not homeopathic remedies are associated with clinically relevant benefits for patients with active but relatively stable rheumatoid arthritis.
Both trials confirm what rational thinkers have been saying for many years: the effects that many people experience after homeopathic therapy are not due to the homeopathic remedy but to the usually long and empathetic therapeutic encounter, the placebo effect, and other non-specific effects. To put it bluntly homeopathy is a kind of amateur psychotherapy.
Before someone now claims that this means homeopathy is fine, let me tell you this: no, it is not fine! If someone needs psychotherapy, he/she should see not an amateur but a professional, i.e. a psychologist who is properly trained in what she can and cannot do.
The website of the World Federation of Chiropractic (WFC) points out that public health is defined by the WHO as follows:
“Activities to strengthen public health capacities and service aim to provide conditions under which people can maintain to be healthy, improve their health and wellbeing, or prevent the deterioration of their health. Public health focuses on the entire spectrum of health and wellbeing, not only the eradication of particular diseases.”
The WFC then continues stating this:
As primary contact health professionals, chiropractors can play an important role as public health advocates. This can range from providing support and advice on health matters such as physical activity, diet, and fitness as well as lifestyle choices such as injury prevention and avoiding tobacco use. Chiropractors can also play a role in counselling patients and communities on the benefits of public health measures, especially as this relates to immediate health needs of each region.
I think that this might merit a few comments.
- Physical activity is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Diet is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Fitness is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Lifestyle choice is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Injury prevention is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Avoiding tobacco use is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Counseling is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
So, what is the real contribution of chiropractors to public health?
- Chiropractors tend to advise their clients against vaccinations.
- Some mislead the public by claiming they boost immunity and prevent serious infections.
- Many undermine evidence-based medicine by promoting obsolete myths such as ‘the innate’ or subluxations.
- Many sell supplements that could interact with prescription drugs.
- Many make bogus health claims for profit.
I would therefore argue that, on balance, the contribution of chiropractors to public health might be considerable …
sadly, however, it goes in the wrong direction.
An impressive article by John Mac Ghlionn caught my attention. Allow me to quote a few passages from it:
The U.S. House of Representatives and the U.S. Senate recently reintroduced legislation to increase access to Medicare-covered services provided by chiropractors. Last year, the US chiropractic market size was worth $13.13 Billion. By the end of the decade, it will be worth over $18 billion. Each year, a whopping 35 million Americans seek chiropractic care.
But why? It’s a questionable science full of questionable characters.
Last year, a Georgia woman was left paralyzed and unable to speak after receiving a neck adjustment from a chiropractor. She’s not the first person to have had her life utterly ruined by a chiropractor, and chances are she won’t be the last. Many patients who visit chiropractors suffer severe side effects; some lose their lives…
As Dr. Steven Novella has noted, what used to be fraud is now known as holistic medicine. Dr. Edzard Ernst, a retired British-German physician and researcher, has expertly demonstrated the many ways in which chiropractic treatments are rooted not in science, but in mystical concepts…
Spinal adjustments, also known as “subluxations,” are also common. A dangerous practice that has been heavily criticized, spinal manipulations are associated with a number of adverse effects, including the risk of stroke. As Dr. Ernst has noted, the cost-effectiveness of this particular treatment “has not been demonstrated beyond reasonable doubt.”
Not content with spinal and neck manipulations, some chiropractors offer to treat other conditions — like diabetes, for example. They are not trained to treat diabetes. Other chiropractors appear to take joy in torturing infants. In August of 2018, a chiropractor made headlines for all the wrong reasons when a video emerged showing him hanging a two-week-old newborn upside down by the ankles…
Finally, as I alluded to earlier, the chiropractic community is full of fraudsters. In 2019, in the US, 15 chiropractors were charged in an insurance fraud and illegal kickback operation. More recently, in February of this year, a New York federal judge sentenced Patrick Khaziran to 30 months in prison after he pleaded guilty to being part of a widespread scheme that defrauded the NBA out of at least $5 million. In recent times, the chiropractic community has come under scrutiny for abusive care and illegal billing practices. When it comes to instances of healthcare fraud, chiropractic medicine is unrivaled.
None of this should come as a surprise. After all, the entire chiropractic community was constructed on a foundation of lies. As the aforementioned Dr. Ernst told me, we should be skeptical of what chiropractors are offering, largely because the whole practice was founded “by a deluded charlatan, who insisted that all human diseases are due to subluxations of the spine. Today, we know that chiropractic subluxations are mere figments of Palmer’s imagination. Yet, the chiropractic profession is unable to separate itself from the myth. It is easy to see why: without it, they would at best become poorly trained physiotherapists without any raison d’etre.”
… Dr. William T. Jarvis famously referred to chiropractic as “the most significant nonscientific health-care delivery system in the United States.” Comparing the chiropractic community to a cult, Dr. Jarvis wondered, somewhat incredulously, why chiropractors are licensed to practice in all 50 US states. The entire profession, he warned, “should be viewed as a societal problem, not simply as a competitor of regular health-care.”
___________________________
In my view, this is an impressive article, not least because it is refreshingly devoid of the phenomenon known as ‘false balance, e.g. a chiropractor being invited to add his self-interested views at the end of the paper claiming, for instance, “we have years of experience and cause far less harm than real doctors”.
This systematic review evaluated all available randomized controlled trials (RCTs) investigating the clinical effects of hydrotherapy according to Kneipp which is characterized by cold water applications. All RCTs on therapy and prevention with Kneipp hydrotherapy were included. Study participants were patients and healthy volunteers of all age groups. MEDLINE (via PubMed), Scopus, Central, CAMbase, and opengrey.eu were systematically searched through April 2021 without language restrictions and updated by searching PubMed until April 6th 2023. The risk of bias was assessed using the Cochrane tool version 1.
Twenty RCTs (N=4247) were included. Due to the high heterogeneity of the RCTs, no meta-analysis was performed. The risk of bias was rated as unclear in most of the domains. Of 132 comparisons, 46 showed significant positive effects in favor of hydrotherapy on chronic venous insufficiency, menopausal symptoms, fever, cognition, emotional function, and sickness absenteeism. However, 81 comparisons showed no differences between groups, and 5 were in favor of the respective control group. Only half of the studies reported safety issues.
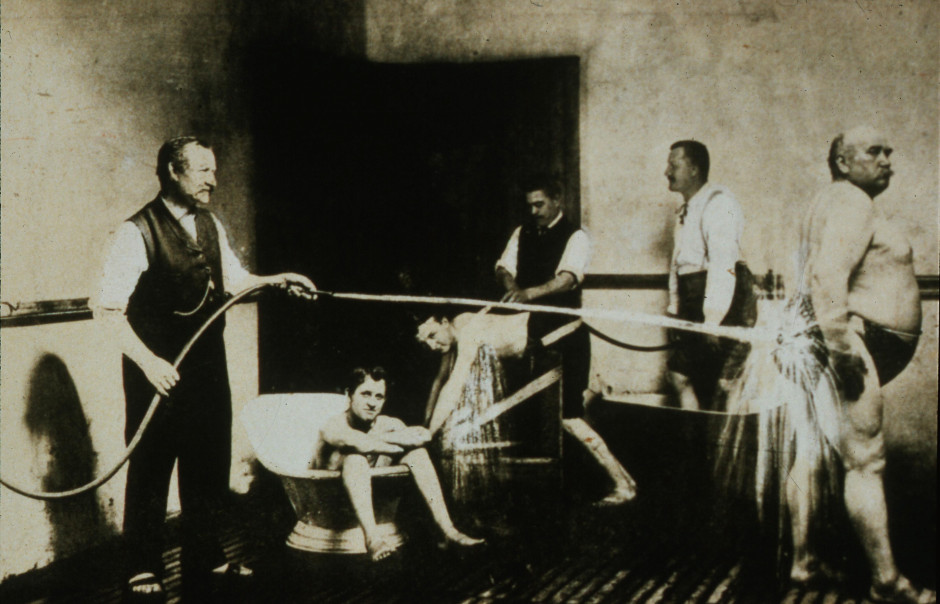
The authors concluded that although RCTs on Kneipp hydrotherapy seem to show positive effects in some conditions and outcomes, it remains difficult to ascertain treatment effects due to the high risk of bias and heterogeneity of most of the considered studies. Further high-quality RCTs on Kneipp hydrotherapy are urgently warranted.
This is certainly the best review of the subject so far. It makes it very clear that the evidence for Kneipp hydrotherapy is weak, mostly because of the many flaws in the primary studies. One needs to add, I think, that 20 RCTs are an absurdly small amount considering that many indications this type of therapy is advocated for – many enthusiasts even consider it a panacea.
It follows, I fear, that Kneipp hydrotherapy is almost entirely not evidence-based. This should be bad news for the numerous institutions and Spa towns (mostly in Germany) that live on employing this treatment and telling patients that it is effective. They usually claim that experience shows this to be true. But this was the mantra of medicine ~100 years ago. Since then, we have learned that experience is a very poor guide that regularly leads us up the garden path.
Kneippians will counter that clinical trials are difficult to conduct and expensive to finance. Both arguments are of course true but, considering that an entire industry lives on telling patients something that essentially amounts to a lie (i.e. the claim that it works), it surely is obligatory to overcome these obstacles.
The General Chiropractic Council (GCC) “regulates chiropractors in the UK to ensure the safety of patients undergoing chiropractic treatment”. One might have assumed that they thus fulfill the important role of controlling the profession. Yet, one would have assumed wrongly. Instead of controlling, the GCC usually prefers promoting the profession. Their recent Chiropractic Patient Satisfaction and Experience is a good example. Let me show you several important sections of this document:
The outcomes reported here highlight two key findings:
• Overwhelmingly, chiropractic patients report high levels of satisfaction and positive experiences with their care. This was true both in the literature that examined international patient cohorts as well as the specific data collected from UK based chiropractic patients.
• A strong therapeutic relationship and good communication between patient and chiropractor underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based chiropractic patients.
Conclusion
This report shows that both existing literature and de novo data collection from patients receiving chiropractic care in the UK highlight excellent perceived experience and high satisfaction with such care.
Factors such as therapeutic alliance and communication are strongly associated with these positive perceptions by patients although other factors such as treatment beliefs were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of care, both in terms of clinical outcomes and patient experience, chiropractors should be explicitly skilled at curating excellent therapeutic alliances and communication with patients.
• Such skills and competences within chiropractic care delivery should receive higher visibility within the chiropractic profession generally and more specifically through advocacy within leading institutions and core emphasis within chiropractic curricula.
__________________________
By changing a few words, I have adapted the above excerpts to become a Customer Satisfaction and Experience Report of a fictitious hamburger joint published by the Hamburger General Council (HGC) of Great Britain which regulates hamburger joints in the UK to ensure the safety of consumers undergoing hamburger nutrition:
The outcomes reported here highlight two key findings:
• Overwhelmingly, customers report high levels of satisfaction and positive experiences with their restaurant. This was true both in the literature that examined international consumer cohorts as well as the specific data collected from UK based customers.
• A strong professional relationship and good communication between customer and service personell underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based hamburger consumers.
Conclusion
This report shows that both existing literature and de novo data collection from consumers eating hamburgers in the UK highlight excellent perceived experience and high satisfaction with such service.
Factors such as personal alliance and communication are strongly associated with these positive perceptions by consumers although other factors such as appetite were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of service, both in terms of profit and patient experience, hamburger vendors should be explicitly skilled at curating excellent professional alliances and communication with customers.
• Such skills and competences within hamburger delivery should receive higher visibility within the gastronomic trade generally and more specifically through advocacy within leading institutions and core emphasis within servers’ curricula.
___________________________
If you get the impression that I am taking the Mickey of the GCC, you are not mistaken. Yet, this post also has slightly more serious purposes. I wanted to 1) show how, in the chiropractic profession, pure BS is often disguised as research, and 2) question whether the GCC is fit for purpose.
On a more constructive note: there are many open questions that urgently need addressing in the realm of chiropractic (e.g. do chiropractors more good than harm?). I, therefore, suggest that the GCC stops publishing idiotic promotional documents disguised as research and gets on with its responsibilities.
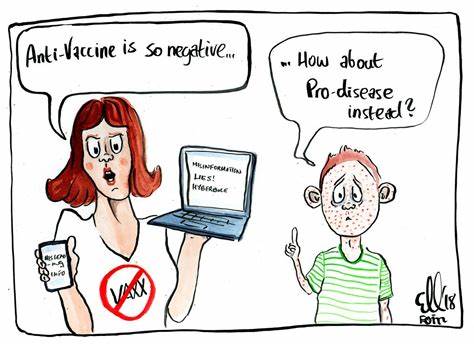
Numerous qualitative studies and a few quantitative studies have linked vaccine hesitancy or refusal with the belief in the efficacy of so-called alternative medicine (SCAM). Yet, large-scale data on this topic are scarce. In this study, the French researchers investigated the factors associated with the coverage rates of seven childhood vaccines or vaccine groups in the ninety-six metropolitan French departments. One of the factors investigated was the local interest in SCAM. In order to assess this interest, they built an Alternative Medicine Index based on departmental internet searches regarding SCAM—internet searches being a reliable indicator of the public’s actual interest in a given topic. They then conducted multiple regression analyses, which showed that this Index is a significant explanatory factor for the departmental variance in vaccination coverage rates, exceeding in importance the effect of other relevant local sociodemographic factors.
A further recent study from France adds to the picture. It presents the results of a survey conducted in July 2021 among a representative sample of the French mainland adult population (n = 3087). Using cluster analysis, the researchers identified five profiles of SCAM attitudes and found that even among the most pro-SCAM group, very few respondents disagreed with the idea that SCAM should only be used as a complement to conventional medicine. They then compared these SCAM attitudes to vaccine attitudes. Attitudes to SCAM had a distinct impact as well as a combined effect on attitudes to different vaccines and vaccines in general. They found that:
- attitudes to SCAM provide a very limited explanation of vaccine hesitancy;
- among the hesitant, pro-SCAM attitudes are often combined with other traits associated with vaccine hesitancy such as distrust of health agencies, radical political preferences, and low income.
Both SCAM endorsement and vaccine hesitancy are more prevalent among the socially disadvantaged. Drawing on these results, the researchers argue that, to better understand the relationship between SCAM and vaccine hesitancy, it is necessary to look at how both can reflect a lack of access and recourse to mainstream medicine and distrust of public institutions.
 The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- Sorry, I was wrong about homeopathy and vaccination
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
What seems fairly clear to me is that a cross-correlation exists: an attitude against modern medicine and the ‘scientific establishment’ determines both the enthusiasm for SCAM and the aversion to vaccination. What is, however, far from clear to me is what we could do about it.
Yes, better education seems important – and that’s precisely what I aim at achieving with this blog. Sadly, judging from some of the comments we receive, it does not seem crowned with much success.
Any other ideas?
