alternative therapist
Exactly 20 years ago, I published a review concluding that the generally high and possibly growing prevalence of complementary/alternative medicine use by children renders this topic an important candidate for rigorous investigation. Since then, many papers have emerged, and most of them are worrying in one way or another. Here is the latest one.
This Canadian survey assessed chiropractic (DC) and naturopathic doctors’ (ND) natural health product (NHP) recommendations for paediatric care. It was developed in collaboration with DC and ND educators, and delivered as an on-line national survey. NHP dose, form of delivery, and indications across paediatric age ranges (from newborn to 16 years) for each practitioner’s top five NHPs were assessed. Data were analysed using descriptive statistics, t-tests, and non-parametric tests.
Of the 421 respondents seeing one or more paediatric patients per week, 172 (41%, 107 DCs, 65 NDs) provided 440 NHP recommendations, categorized as:
- vitamins and minerals (89 practitioners, 127 recommendations),
- probiotics (110 practitioners, 110 recommendations),
- essential fatty acids (EFAs: 72 practitioners, 72 recommendations),
- homeopathics (56 practitioners, 66 recommendations),
- botanicals (29 practitioners, 31 recommendations),
- other NHPs (33 practitioners, 34 recommendations).
Indications for the NHP recommendations were tabulated for NHPs with 10 or more recommendations in any age category:
- 596 total indications for probiotics,
- 318 indications for essential fatty acids,
- 138 indications for vitamin D,
- 71 indications for multi-vitamins.
Good evidence regarding the efficacy, safety, and dosing for NHP use in children is scarce or even absent. Therefore, the finding that so many DCs and NDs recommend unproven NHPs for use in children is worrying, to say the least. It seems to indicate that, at least in Canada, DCs and NDs are peddling unproven, mostly useless and potentially harmful children.
In an earlier, similar survey the same group of researchers had disclosed that the majority of Canadian DCs and NDs seem to see infants, children, and youth for a variety of health conditions and issues, while, according to their own admission, not having adequate paediatric training.
Is this a Canadian phenomenon? If you think so, read this abstract:
AIM:
This systematic review is aimed at estimating the prevalence of complementary and alternative medicine (CAM)-use by paediatric populations in the United Kingdom (UK).
METHOD:
AMED, CINAHL, COCHRANE, EMBASE and MEDLINE were searched for English language peer-reviewed surveys published between 01 January 2000 and September 2011. Additionally, relevant book chapters and our own departmental files were searched manually.
RESULTS:
Eleven surveys were included with a total of 17,631 paediatric patients. The majority were of poor methodological quality. Due to significant heterogeneity of the data, a formal meta-analysis was deemed inappropriate. Ten surveys related to CAM in general, while one was specifically on homeopathy. Across all surveys on CAM in general, the average one-year prevalence rate was 34% and the average lifetime prevalence was 42%. In surveys with a sample size of more than 500, the prevalence rates were considerably lower than in surveys with the sample size of lower than 500. Herbal medicine was the most popular CAM modality, followed by homeopathy and aromatherapy.
CONCLUSIONS:
Many paediatric patients in the UK seem to use CAM. Paediatricians should therefore have sufficient knowledge about CAM to issue responsible advice.
This means, I fear, that children are regularly treated by SCAM practitioners who are devoid of the medical competence to do so, and who prescribe or recommend treatments of unknown value, usually without the children needing them.
Why are regulators not more concerned about this obvious abuse?
The purpose of this recently published survey was to obtain the demographic profile and educational background of chiropractors with paediatric patients on a multinational scale.
A multinational online cross-sectional demographic survey was conducted over a 15-day period in July 2010. The survey was electronically administered via chiropractic associations in 17 countries, using SurveyMonkey for data acquisition, transfer, and descriptive analysis.
The response rate was 10.1%, and 1498 responses were received from 17 countries on 6 continents. Of these, 90.4% accepted paediatric cases. The average practitioner was male (61.1%) and 41.4 years old, had 13.6 years in practice, and saw 107 patient visits per week. Regarding educational background, 63.4% had a bachelor’s degree or higher in addition to their chiropractic qualification, and 18.4% had a postgraduate certificate or higher in paediatric chiropractic.
The authors from the Anglo-European College of Chiropractic (AECC), Bournemouth University, United Kingdom, drew the following conclusion: this is the first study about chiropractors who treat children from the United Arab Emirates, Peru, Japan, South Africa, and Spain. Although the response rate was low, the results of this multinational survey suggest that pediatric chiropractic care may be a common component of usual chiropractic practice on a multinational level for these respondents.
A survey with a response rate of 10%?
An investigation published 9 years after it has been conducted?
Who at the AECC is responsible for controlling the quality of the research output?
Or is this paper perhaps an attempt to get the AECC into the ‘Guinness Book of Records’ for outstanding research incompetence?
But let’s just for a minute pretend that this paper is of acceptable quality. If the finding that ~90% of chiropractors tread kids is approximately correct, one has to be very concerned indeed.
I am not aware of any good evidence that chiropractic care is effective for paediatric conditions. On the contrary, it can do quite a bit of direct harm! To this, we sadly also have to add the indirect harm many chiropractors cause, for instance, by advising parents against vaccinating their kids.
This clearly begs the question: is it not time to stop these charlatans?
What do you think?
The ‘International Federation of Anthroposophic Medical Associations’ have just published a ‘Statement on Vaccination‘. Here it is in its full beauty:
Vaccines, together with health education, hygiene and adequate nutrition, are essential tools for preventing infectious diseases. Vaccines have saved countless lives over the last century; for example, they allowed the eradication of small pox and are currently allowing the world to approach the elimination of polio.
Anthroposophic Medicine fully appreciates the contribution of vaccines to global health and firmly supports vaccination as an important measure to prevent life threatening diseases. Anthroposophic Medicine is not anti-vaccine and does not support anti-vaccine movements.
Physicians with training in Anthroposophic Medicine are expected to act in accordance with national legislation and to carefully advise patients (or their caregivers) to help them understand the relevant scientific information and national vaccination recommendations. In countries where vaccination is not mandatory and informed consent is needed, this may include coming to agreement with the patient (or the caregivers) about an individualized vaccination schedule, for example by adapting the timing of vaccination during infancy.
Taking into account ongoing research, local infectious disease patterns and socioeconomic risk factors, individual anthroposophic physicians are at times involved in the scientific discussion about specific vaccines and appropriate vaccine schedules. Anthroposophic Medicine is pro-science and continued scientific debate is more important than ever in today’s polarized vaccine environment.
Already in 2010, The European Council for Steiner Waldorf Education published a press release, implying a similar stance:
We wish to state unequivocally that opposition to immunization per se, or resistance to national strategies for childhood immunization in general, forms no part of our specific educational objectives. We believe that a matter such as whether or not to innoculate a child against communicable disease should be a matter of parental choice. Consequently, we believe that families provide the proper context for such decisions to be made on the basis of medical, social and ethical considerations, and upon the perceived balance of risks. Insofar as schools have any role to play in these matters, we believe it is in making available a range of balanced information both from the appropriate national agencies and qualified health professionals with expertise in the filed. Schools themselves are not, nor should they attempt to become, determiners of decisions regarding these matters.
Such statements sound about right. Why then am I not convinced?
Perhaps because there are hundreds of anthroposophic texts that seem to contradict this pro-vaccination stance (not least those from Rudolf Steiner himself). Today, anthroposophy enthusiasts are frequently rampant anti-vax; look at this quote, for instance:
… anthroposophic and conventional medicine have dramatically different viewpoints as to what causes common childhood illnesses. Conventional medicine views childhood illnesses for which vaccines have been developed as a physical disease, inherently bad, to be prevented. Their main goal, therefore, is protection against contracting the disease making one free of illness. In contrast, these childhood illnesses are viewed by anthroposophic medicine as a necessary instrument in dealing with karma and, as discussed by Husemann, and Wolff, 6 the incarnation of the child. During childhood illnesses, anthroposophic medical practitioners administer medical remedies to assist the child in dealing with the illness not only as a disease affecting their physical body in the physical plane, but also for soul spiritual development, thereby promoting healing. In contrast, allopathic medicaments are aimed at suppression of symptoms and not necessarily the promotion of healing.
In Manifestations of Karma, Rudolf Steiner states that humans may be able to influence their karma and remove the manifestation of certain conditions, i.e., disease, but they may not be liberated from the karmic effect which attempted to produce them. Says Steiner, “…if the karmic reparation is escaped in one direction, it will have to be sought in another … the souls in question would then be forced to seek another way for karmic compensation either in this or in another incarnation.” 7
In his lecture, Karma of Higher Beings 8, Steiner poses the question, “If someone seeks an opportunity of being infected in an epidemic, this is the result of the necessary reaction against an earlier karmic cause. Have we the right now to take hygienic or other measures?” The answer to this question must be decided by each person and may vary. For example, some may accept the risk of disease but not of vaccine side effects, while others may accept the risk associated with vaccination but not with the disease.
Anthroposophic medicine teaches that to prevent a disease in the physical body only postpones what will then be produced in another incarnation. Thus, when health measures are undertaken to eliminate the susceptibility to a disease, only the external nature of the illness is eliminated. To deal with the karmic activity from within, Anthroposphy states that spiritual education is required. This does not mean that one should automatically be opposed to vaccination. Steiner indicates that “Vaccination will not be harmful if, subsequent to vaccination, a person receives a spiritual education.”
Or consider this little statistic from the US:
Waldorf schools are the leading Nonmedical Exemption [of vaccinations] schools in various states, such as:
- Waldorf School of Mendocino County (California) – 79.1%
- Tucson Waldorf Schools (Arizona) – 69.6%
- Cedar Springs Waldorf School (California) – 64.7%
- Waldorf School of San Diego (California) – 63.6%
- Orchard Valley Waldorf School (Vermont) – 59.4%
- Whidbey Island Waldorf School (Washington) – 54.9%
- Lake Champlain Waldorf School (Vermont) – 49.6%
- Austin Waldorf School (Texas) – 48%
Or what about this quote?
Q: I am a mother who does not immunize my children. I feel as though I have to keep this a secret. I recently had to take my son to the ER for a tetanus shot when he got a fish hook in his foot, and I was so worried about the doctor asking if his shots were current. His grandmother also does not understand. What do you suggest?
A: You didn’t give your reasons for not vaccinating your children. Perhaps you feel intuitively that vaccinations just aren’t good for children in the long run, but you can’t explain why. If that’s the case, I think your intuition is correct, but in today’s contentious world it is best to understand the reasons for our decisions and actions.
There are many good reasons today for not vaccinating children in the United States I recommend you consult the book, The Vaccination Dilemma edited by Christine Murphy, published by SteinerBooks.
So, where is the evidence that anthroposophy-enthusiasts discourage vaccinations?
It turns out, there is plenty of it! In 2011, I summarised some of it in a review concluding that numerous reports from different countries about measles outbreaks centered around Steiner schools seem nevertheless to imply that a problem does exist. In the interest of public health, we should address it.
All this begs a few questions:
- Are anthroposophy-enthusiasts and their professional organisations generally for or against vaccinations?
- Are the statements above honest or mere distractions from the truth?
- Why are these professional organisations not going after their members who fail to conform with their published stance on vaccination?
I suspect I know the answers.
What do you think?
This paper reports a survey amongst European chiropractors during early 2017. Dissemination was through an on-line platform with links to the survey being sent to all European chiropractic associations regardless of European Chiropractors’ Union (ECU) membership and additionally through the European Academy of Chiropractic (EAC). Social media via Facebook groups was also used to disseminate links to the survey.
One thousand three hundred twenty and two responses from chiropractors across Europe representing approximately 17.2% of the profession were collected. Five initial self-determined chiropractic identities were collapsed into 2 groups categorised as orthodox (79.9%) and unorthodox (20.1%); by the latter term, the investigators mean the subluxationists/vitalists.
When comparing the percentage of new patients chiropractors x-rayed, 23% of the unorthodox group x-rayed > 50% of their new patients compared to 5% in the orthodox group. Furthermore, the proportion of respondents reporting > 150 patient encounters per week in the unorthodox group were double compared to the orthodox (22 v 11%). Lastly the proportion of those respondents disagreeing or strongly disagreeing with the statement “In general, vaccinations have had a positive effect on global public health” was 57 and 4% in unorthodox and orthodox categories respectively. Logistic regression models identified male gender, seeing more than 150 patients per week, no routine differential diagnosis, and not strongly agreeing that vaccines have generally had a positive impact on health as highly predictive of unorthodox categorisation.
The authors concluded that despite limitations with generalisability in this survey, the proportion of respondents adhering to the different belief categories are remarkably similar to other studies exploring this phenomenon. In addition, and in parallel with other research, this survey suggests that key practice characteristics in contravention of national radiation guidelines or opposition to evidence based public health policy are significantly more associated with non-orthodox chiropractic paradigms.
|
Country |
N (%) Orthodox |
N (%) Unorthodox |
|---|---|---|
|
Belgium |
51 (92.7) |
4 (7.3) |
|
Germany |
43 (66.2) |
22 (33.8) |
|
Ireland |
31 (79.5) |
8 (20.5) |
|
Italy |
23 (59.0) |
16 (41.0) |
|
Norway |
132 (93.0) |
10 (7.0) |
|
Spain |
34 (43.6) |
44 (56.4) |
|
Sweden |
101 (82.8) |
21 (17.2) |
|
Switzerland |
102 (90.3) |
11 (9.7) |
|
The Netherlands |
81 (82.7) |
17 (17.3) |
|
UK |
236 (80.0) |
59 (20.0) |
Mr William Harvey Lillard was the janitor contracted to clean the Ryan Building where D. D. Palmer’s magnetic healing office was located. In 1895, he became Palmer’s very first chiropractic patient and thus entered the history books. The very foundations of chiropractic are based on this story.
[Testimony of Harvey Lillard regarding the events surrounding the first chiropractic adjustment, printed in the January 1897 issue of the Chiropractor]To call the ‘Chiropractor’ a reliable source would probably be stretching it a bit, and there are various versions of the event, even one where BJ Palmer, DD’s son, changed significant details of the story. Nevertheless, it’s a nice story, if there ever was one. But, like many nice stories, it’s just that: a tall tale, a story that might be not based on reality. In this case, the reality getting in the way of a good story is human anatomy.
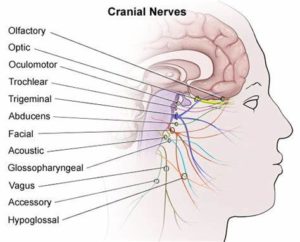
The nerve supply of the inner ear, the bit that enables us to hear, does not, like most other nerves of our body, run through the spine; it comes directly from the brain: the acoustic nerve is one of the 12 cranial nerves.
But chiropractors never let the facts get in the way of a good story! Thus they still tell it and presumably even believe it. Take this website, for instance, as an example of hundreds of similar sources:
… the very first chiropractic patient in history was named William Harvey Lillard, who experienced difficulty hearing due to compression of the nerves leading to his ears. He was treated by “the founder of chiropractic care,” David. D. Palmer, who gave Lillard spinal adjustments in order to reduce destructive nerve compressions and restore his hearing. After doing extensive research about physiology, Palmer believed that Lillard’s hearing loss was due to a misalignment that blocked the spinal nerves that controlled the inner ear (an example of vertebral subluxation). Palmer went on to successfully treat other patients and eventually trained other practitioners how to do the same.
How often have we been told that chiropractors receive a medical training that is at least as thorough as that of proper doctors? But that’s just another tall story, I guess.
 Chiropractic may be nonsense, but it nevertheless earns chiros very good money. Chiropractors tend to treat their patients for unnecessarily long periods of time. This, of course, costs money, and even if the treatment in question ever was indicated (which, according to the best evidence, is more than doubtful), this phenomenon would significantly inflate healthcare expenditure. It was reported that over 80% of the money that the US Medicare paid to chiropractors in 2013 went for medically unnecessary procedures. The federal insurance program for senior citizens thus spent roughly $359 million on unnecessary chiropractic care that year.
Chiropractic may be nonsense, but it nevertheless earns chiros very good money. Chiropractors tend to treat their patients for unnecessarily long periods of time. This, of course, costs money, and even if the treatment in question ever was indicated (which, according to the best evidence, is more than doubtful), this phenomenon would significantly inflate healthcare expenditure. It was reported that over 80% of the money that the US Medicare paid to chiropractors in 2013 went for medically unnecessary procedures. The federal insurance program for senior citizens thus spent roughly $359 million on unnecessary chiropractic care that year.
Such expenditure may not benefit patients, but it surely benefits the chiropractors. A recent article in Forbes informed us that, according to the US Bureau of Labor Statistics’ Occupational Outlook Handbook, the employment of chiropractors is expected to grow 12% from 2016 to 2026, faster than the average for all occupations.
According to the latest data from the Bureau Occupational Employment Statistics, as of 2017, the average income of an US chiropractor amounts to US $ 85,870. However, chiropractors’ salaries aren’t this high in every US state. The lowest average income (US$ 45 000) per year is in the state of Wyoming.
Below you’ll find a breakdown of where chiropractors’ incomes are the highest.
| 1 | Rhode Island | $147,900 |
| 2 | Tennessee | $122,620 |
| 3 | Connecticut | $113,130 |
| 4 | Alaska | $106,600 |
| 5 | Colorado | $99,350 |
| 6 | New Hampshire | $99,330 |
| 7 | Nevada | $99,140 |
| 8 | Delaware | $97,650 |
| 9 | Massachusetts | $96,110 |
| 10 | Maryland | $95,190 |
These are tidy sums indeed – remember, they merely depict the averages. Individual chiropractors will earn substantially more than the average, of course. And there are hundreds of websites, books, etc. to teach chiros how to maximise their cash-flow. Some of the most popular ‘tricks of the chiro trade’ include:
- maintenance therapy,
- treatment of children,
- making unsupported therapeutic claims,
- disregarding the risks of spinal manipulation,
- selling useless dietary supplements.
Considering the sums of money that are at stake, I am beginning to understand why chiropractors tend to get so nervous, often even furious and aggressive, when I point out that they might be causing more harm than good to their patients.
Its the money, stupid!
As you can imagine, I get quite a lot of ‘fan-post’. Most of the correspondence amounts to personal attacks and insults which I usually discard. But some of these ‘love-letters’ are so remarkable in one way or another that I answer them. This short email was received on 20/3/19; it belongs to the latter category:
Dr Ernst,
You have been trashing homeopathy ad nauseum for so many years based on your limited understanding of it. You seem to know little more than that the remedies are so extremely dilute as to be impossibly effective in your opinion. Everybody knows this and has to confront their initial disbelief.
Why dont you get some direct understanding of homeopathy by doing a homeopathic proving of an unknown (to you) remedy? Only once was I able to convince a skeptic to take the challenge to do a homeopathic proving. He was amazed at all the new symptoms he experienced after taking the remedy repeatedly over several days.
Please have a similar bravery in your approach to homeopathy instead of basing your thoughts purely on your speculation on the subject, grounded in little understanding and no experience of it.
THIS IS HOW I RESPONDED
Dear Mr …
thank you for this email which I would like to answer as follows.
Your lines give the impression that you might not be familiar with the concept of critical analysis. In fact, you seem to confuse my criticism of homeopathy with ‘trashing it’. I strongly recommend you read up about critical analysis. No doubt you will then realise that it is a necessary and valuable process towards generating progress in healthcare and beyond.
You assume that I have limited understanding of homeopathy. In fact, I grew up with homeopathy, practised homeopathy as a young doctor, researched the subject for more than 25 years and published several books as well as over 100 peer-reviewed scientific papers about it. All of this, I have disclosed publicly, for instance, in my memoir which might interest you.
The challenge you mention has been taken by me and others many times. It cannot convince critical thinkers and, frankly, I am surprised that you found a sceptic who was convinced by what essentially amounts to little more than a party trick. But, as you seem to like challenges, I invite you to consider taking the challenge of the INH which even offers a sizable amount of money, in case you are successful.
Your final claim that my thoughts are based purely on speculation is almost farcically wrong. The truth is that sceptics try their very best to counter-balance the mostly weird speculations of homeopaths with scientific facts. I am sure that, once you have acquired the skills of critical thinking, you will do the same.
Best of luck.
Edzard Ernst
An impressive 17% of US chiropractic patients are 17 years of age or younger. This figure increases to 39% among US chiropractors who have specialized in paediatrics. Data for other countries can be assumed to be similar. But is chiropractic effective for children? All previous reviews concluded that there is a paucity of evidence for the effectiveness of manual therapy for conditions within paediatric populations.
This systematic review is an attempt to shed more light on the issue by evaluating the use of manual therapy for clinical conditions in the paediatric population, assessing the methodological quality of the studies found, and synthesizing findings based on health condition.
Of the 3563 articles identified through various literature searches, 165 full articles were screened, and 50 studies (32 RCTs and 18 observational studies) met the inclusion criteria. Only 18 studies were judged to be of high quality. Conditions evaluated were:
- attention deficit hyperactivity disorder (ADHD),
- autism,
- asthma,
- cerebral palsy,
- clubfoot,
- constipation,
- cranial asymmetry,
- cuboid syndrome,
- headache,
- infantile colic,
- low back pain,
- obstructive apnoea,
- otitis media,
- paediatric dysfunctional voiding,
- paediatric nocturnal enuresis,
- postural asymmetry,
- preterm infants,
- pulled elbow,
- suboptimal infant breastfeeding,
- scoliosis,
- suboptimal infant breastfeeding,
- temporomandibular dysfunction,
- torticollis,
- upper cervical dysfunction.
Musculoskeletal conditions, including low back pain and headache, were evaluated in seven studies. Only 20 studies reported adverse events.
The authors concluded that fifty studies investigated the clinical effects of manual therapies for a wide variety of pediatric conditions. Moderate-positive overall assessment was found for 3 conditions: low back pain, pulled elbow, and premature infants. Inconclusive unfavorable outcomes were found for 2 conditions: scoliosis (OMT) and torticollis (MT). All other condition’s overall assessments were either inconclusive favorable or unclear. Adverse events were uncommonly reported. More robust clinical trials in this area of healthcare are needed.
There are many things that I find remarkable about this review:
- The list of indications for which studies have been published confirms the notion that manual therapists – especially chiropractors – regard their approach as a panacea.
- A systematic review evaluating the effectiveness of a therapy that includes observational studies without a control group is, in my view, highly suspect.
- Many of the RCTs included in the review are meaningless; for instance, if a trial compares the effectiveness of two different manual therapies none of which has been shown to work, it cannot generate a meaningful result.
- Again, we find that the majority of trialists fail to report adverse effects. This is unethical to a degree that I lose faith in such studies altogether.
- Only three conditions are, according to the authors, based on evidence. This is hardly enough to sustain an entire speciality of paediatric chiropractors.
Allow me to have a closer look at these three conditions.
- Low back pain: the verdict ‘moderate positive’ is based on two RCTs and two observational studies. The latter are irrelevant for evaluating the effectiveness of a therapy. One of the two RCTs should have been excluded because the age of the patients exceeded the age range named by the authors as an inclusion criterion. This leaves us with one single ‘medium quality’ RCT that included a mere 35 patients. In my view, it would be foolish to base a positive verdict on such evidence.
- Pulled elbow: here the verdict is based on one RCT that compared two different approaches of unknown value. In my view, it would be foolish to base a positive verdict on such evidence.
- Preterm: Here we have 4 RCTs; one was a mere pilot study of craniosacral therapy following the infamous A+B vs B design. The other three RCTs were all from the same Italian research group; their findings have never been independently replicated. In my view, it would be foolish to base a positive verdict on such evidence.
So, what can be concluded from this?
I would say that there is no good evidence for chiropractic, osteopathic or other manual treatments for children suffering from any condition.
And why do the authors of this new review arrive at such dramatically different conclusion? I am not sure. Could it perhaps have something to do with their affiliations?
- Palmer College of Chiropractic,
- Canadian Memorial Chiropractic College,
- Performance Chiropractic.
What do you think?
I stared my Exeter post in October 1993. It took the best part of a year to set up a research team, find rooms etc. So, our research began in earnest only mid 1994. From the very outset, it was clear to me that investigating the risks of so-called alternative medicine (SCAM) should be our priority. The reason, I felt, was simple: SCAM was being used a million times every day; therefore it was an ethical imperative to check whether these treatments were as really safe as most people seemed to believe.
In the course of this line of investigation, we did discover many surprises (and lost many friends). One of the very first revelation was that homeopathy might not be harmless. Our initial results on this topic were published in this 1995 article. In view of the still ongoing debate about homeopathy, I’d like to re-publish the short paper here:
Homoeopathic remedies are believed by doctors and patients to be almost totally safe. Is homoeopathic advice safe, for example on the subject of immunization? In order to answer this question, a questionnaire survey was undertaken in 1995 of all 45 homoeopaths listed in the Exeter ‘yellow pages’ business directory. A total of 23 replies (51%) were received, 10 from medically qualified and 13 from non-medically qualified homoeopaths.
The homoeopaths were asked to suggest which conditions they perceived as being most responsive to homoeopathy. The three most frequently cited conditions were allergies (suggested by 10 respondents), gynaecological problems (seven) and bowel problems (five).
They were then asked to estimate the proportion of patients that were referred to them by orthodox doctors and the proportion that they referred to orthodox doctors. The mean estimated percentages were 1 % and 8%, respectively. The 23 respondents estimated that they spent a mean of 73 minutes on the first consultation.
The homoeopaths were asked whether they used or recommended orthodox immunization for children and whether they only used and recommended homoeopathic immunization. Seven of the 10 homoeopaths who were medically qualified recommended orthodox immunization but none of the 13 non-medically qualified homoeopaths did. One non-medically qualified homoeopath only used and recommended homoeopathic immunization.
Homoeopaths have been reported as being against orthodox immunization’ and advocating homoeopathic immunization for which no evidence of effectiveness exists. As yet there has been no attempt in the United Kingdom to monitor homoeopaths’ attitudes in this respect. The above findings imply that there may be a problem. The British homoeopathic doctors’ organization (the Faculty of Homoeopathy) has distanced itself from the polemic of other homoeopaths against orthodox immunization, and editorials in the British Homoeopathic Journal call the abandonment of mass immunization ‘criminally irresponsible’ and ‘most unfortunate, in that it will be seen by most people as irresponsible and poorly based’.’
Homoeopathic remedies may be safe, but do all homoeopaths merit this attribute?
This tiny and seemingly insignificant piece of research triggered debate and research (my group must have published well over 100 papers in the years that followed) that continue to the present day. The debate has spread to many other countries and now involves numerous forms of SCAM other than just homeopathy. It relates to many complex issues such as the competence of SCAM practitioners, their ethical standards, education, regulation, trustworthiness and the risk of neglect.
Looking back, it feels odd that, at least for me, all this started with such a humble investigation almost a quarter of a century ago. Looking towards the future, I predict that we have so far merely seen the tip of the iceberg. The investigation of the risks of SCAM has finally started in earnest and will, I am sure, continue thus leading to a better protection of patients and consumers from charlatans and their bogus claims.
Osteopathy is a tricky subject:
- Osteopathic manipulations/mobilisations are advocated mainly for spinal complaints.
- Yet many osteopaths use them also for a myriad of non-spinal conditions.
- Osteopathy comprises two entirely different professions; in the US, osteopaths are very similar to medically trained doctors, and many hardly ever employ osteopathic manual techniques; outside the US, osteopaths are alternative practitioners who use mainly osteopathic techniques and believe in the obsolete gospel of their guru Andrew Taylor Still (this post relates to the latter type of osteopathy).
- The question whether osteopathic manual therapies are effective is still open – even for the indication that osteopaths treat most, spinal complaints.
- Like chiropractors, osteopaths now insist that osteopathy is not a treatment but a profession; the transparent reason for this argument is to gain more wriggle-room when faced with negative evidence regarding they hallmark treatment of osteopathic manipulation/mobilisation.
A new paper authored by osteopaths is an attempt to shed more light on the effectiveness of osteopathy. The aim of this systematic review evaluated the impact of osteopathic care for spinal complaints. Only randomized controlled trials conducted in high-income Western countries were considered. Two authors independently screened the titles and abstracts. Primary outcomes included ‘pain’ and ‘functional status’, while secondary outcomes included ‘medication use’ and ‘health status’.
Nineteen studies were included and qualitatively synthesized. Nine studies were from the US, followed by Germany with 7 studies. The majority of studies (n = 13) focused on low back pain.
In general, mixed findings related to the impact of osteopathic care on primary and secondary outcomes were observed. For the primary outcomes, a clear distinction between US and European studies was found, where the latter RCTs reported positive results more frequently. Studies were characterized by substantial methodological differences in sample sizes, number of treatments, control groups, and follow-up.
The authors concluded that “the findings of the current literature review suggested that osteopathic care may improve pain and functional status in patients suffering from spinal complaints. A clear distinction was observed between studies conducted in the US and those in Europe, in favor of the latter. Today, no clear conclusions of the impact of osteopathic care for spinal complaints can be drawn. Further studies with larger study samples also assessing the long-term impact of osteopathic care for spinal complaints are required to further strengthen the body of evidence.”
Some of the most obvious weaknesses of this review include the following:
- In none of the studies employed blinding of patients, care provider or outcome assessor occurred, or it was unclear. Blinding of outcome assessors is easily implemented and should be standard in any RCT.
- In three studies, the study groups differed to some extent at baseline indicating that randomisation was not successful..
- Five studies were derived from the ‘grey literature’ and were therefore not peer-reviewed.
- One study (the UK BEAM trial) employed not just osteopaths but also chiropractors and physiotherapists for administering the spinal manipulations. It is therefore hardly an adequate test of osteopathy.
- The study was funded by an unrestricted grant from the GNRPO, the umbrella organization of the ‘Belgian Professional Associations for Osteopaths’.
Considering this last point, the authors’ honesty in admitting that no clear conclusions of the impact of osteopathic care for spinal complaints can be drawn is remarkable and deserves praise.
Considering that the evidence for osteopathy is even far worse for non-spinal conditions (numerous trials exist for all sorts of other conditions, but they tend to be flimsy and usually lack independent replications), it is fair to conclude that osteopathy is NOT an evidence-based therapy.