Monthly Archives: June 2023
Yesterday, I was alerted of this remarkable tweet. 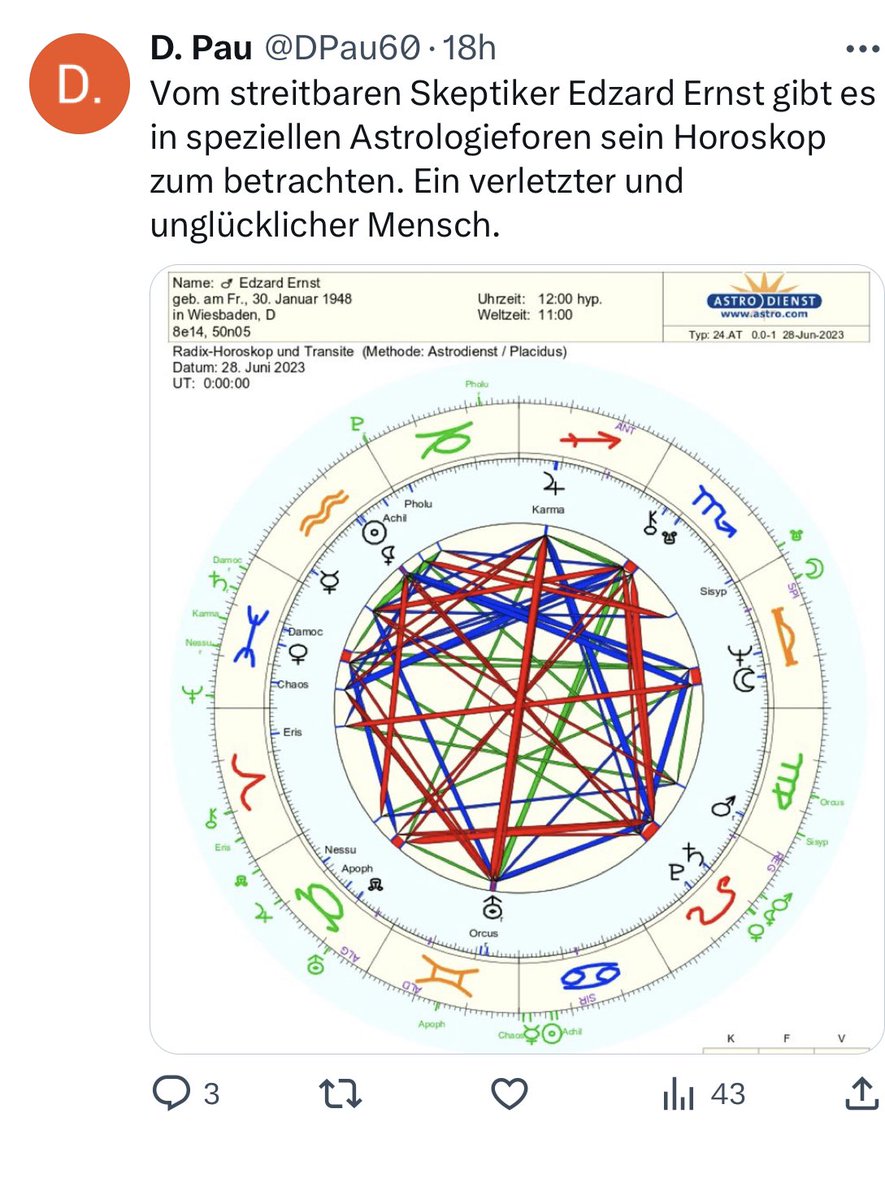 Yes, you guessed correctly, it is indeed a horoscope that the ‘Astro Dienst’ did on me. And it seems to conclude that I am an ‘injured and unhappy’ man which, in turn, is said to explain my skepticism.
Yes, you guessed correctly, it is indeed a horoscope that the ‘Astro Dienst’ did on me. And it seems to conclude that I am an ‘injured and unhappy’ man which, in turn, is said to explain my skepticism.
So, it is all written in the stars!!!
Fascinating!
Who would have thought?
Inspired by such profound insights, I went on Medline and looked for evidence on the subject of horoscopes. Here is a recent article that I found:
Purpose of the study: Established over 2000 years ago, horoscopes remain a regular feature in contemporary society. We aimed to assess whether there could be a link between zodiac sign and medical occupation, asking the question-did your specialty choose you?
Study design: A questionnaire-based study was distributed using an online survey tool. Questions explored the zodiac sign, specialty preferences and personality features of physicians.
Results: 1923 physicians responded between February and March 2020. Variations in personality types between different medical specialties were observed, introverts being highly represented in oncology (71.4%) and rheumatology (65.4%), and extroverts in sexual health (55%), gastroenterology (44.4%) and obstetrics and gynaecology (44.2%) (p<0.01). Proportions of zodiac signs in each specialty also varied; for example, cardiologists were more likely to be Leo compared with Aries (14.4% vs 3.9%, p=0.047), medical physicians more likely Capricorn than Aquarius (10.4% vs 6.7%, p=0.02) and obstetricians and gynaecologists more likely Pisces than Sagittarius (17.5% vs 0%, p=0.036). Intensive care was the most commonly reported second choice career, but this also varied between zodiac signs and specialties. Fountain pen use was associated with extroversion (p=0.049) and gastroenterology (p<0.01).
Conclusions: Personality types vary in different specialties. There may be links to zodiac signs which warrant further investigation.
Now I am even more fascinated!
Horoscopes are for real?
They actually predict things accurately?
Hold on, in my case, the horoscope was totally wrong!
The thing about me being ‘injured’ they clearly got from Wiki and similar accounts of the old tale with Chucky Windsor etc. But what about the claim that I am ‘unhappy’? I feel happy as a lark!
Perhaps I delude myself?
As a true skeptic, I conducted a quick survey with people who know me well. It turns out that 0% of them think I am unhappy!
And then it dawned on me: the methodology of the horoscope is, of course, entirely correct but they supplied it with the wrong data: the birthday and place are correct. However, the time of day is incorrect.
The only possible conclusion is that the incorrect time must be the reason why an otherwise fool-proof method failed.
PS
No, I will not provide the correct time; it would enable the ‘Astro Dienst’ to disclose all my deepest secrets.
This study allegedly evaluated the efficacy of osteopathic manipulative therapy (OMT) compared to that of the Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) for patients with chronic LBP.
It included 68 participants of both genders, aged 30 to 60, with chronic LBP. Participants were randomly assigned to one of two parallel groups, each with 34 members. The OMT group received, as a direct technique, a high-velocity/low-amplitude (HVLA) impulse, and as indirect techniques, strain counterstrain (SCS), myofascial release (MFR), and visceral mobilization therapy (VMT). The KEOMT group received lumbar segmental traction and lumbar segmental mobilization-flexion and gliding therapy grade 3. The participants in both groups received 10 treatments, two per week for five weeks. The primary outcome was pain severity, using a numeric pain rating scale (NPRS). The secondary outcome was the measurement of functional disability, using the Oswestry Disability Index (ODI).
The OMT and KEOMT both decreased pain and disability; however, the changes on the NPRS and ODI postintervention were statistically greater for the OMT group compared to the KEOMT group (P < .05).
The authors concluded that the OMT was better at reducing pain and improving quality of life. It reduced functional disability more than KEOMT in patients with chronic LBP.
The Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) concept is a treatment and training system based upon a comprehensive biomechanical evaluation of the arthro-neuro-muscular system and an individual’s functional abilities. This system of diagnosis and patient management applies to both patients with acute, subacute and chronic conditions of the spine and extremities and to athletes seeking to improve performance. It offers a reliable and practical approach that focuses on optimal physical health and function.
Has the KEOMT concept been tested and shown to be effective for LBP?
No!
So, what we have here is an equivalence trial of two manual techniques. As such it is FAR too small to yield a meaningful result. If the findings were meaningful, would they show that OMT is effective?
No!
As we have no proof that KEOMT does not impede recovery from LBP, the result could merely be due to the fact that OMT does not influence the natural history of LBP, while KEOMT has a detrimental effect.
Last question: which journal publishes such rubbish?
Ahh, it’s the remarkable Alternative therapies in health and medicine. That explains a lot!
I missed this paper when it first came out in 2022. Yet, it seems potentially quite important and I, therefore, feel like discussing it here:
President of the UNESCO Committee on Bioethics Stefan Semplici called on the governments of all countries to ensure free and wider access of their citizens to alternative medicine and pay for this therapy through health insurance. Alternative medicine based on tradition – traditional medicine, in many poor countries is the only treatment option for the population. In developed countries, and especially in China and India, it enjoys well-deserved prestige (for example, acupuncture and herbal medicine) and is often integrated into the public health system.
The International Committee on Bioethics of UNESCO announced the recognition of these alternative therapies as an option for medical practice and, at the same time, as part of the identity of the cultural traditions of various nations. The UNESCO Universal Declaration on Bioethics and Human Rights includes the right to the highest attainable standard of health (Article 14), the right to respect for pluralism and cultural diversity (Article 12) and traditional knowledge (Article 17). The purpose of this document is to establish criteria for the respect and acceptability of different types of medicine without compromising the assurance of quality and patient safety that is essential in all treatments.
In order to adapt the traditions of traditional therapies to advances in medicine, this international organization calls on governments and the scientific community to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety and develop therapeutic standards and protocols for integrating traditional medicine into healthcare system. The UNESCO International Bioethics Committee believes that these methods should be seen as complementary to modern medicine, and not just an alternative to it.
_________________________
The United Nations Educational, Scientific and Cultural Organization (UNESCO) is an agency of the United Nations aimed at promoting world peace and security through international cooperation in education, arts, sciences, and culture. UNESCO’s International Bioethics Committee (IBC) is a body of 36 independent experts that follows progress in the life sciences and its applications in order to ensure respect for human dignity and freedom.
I have to say that I rarely have seen an announcement in so-called alternative medicine (SCAM) that is more confusing and less well thought through. The UNESCO Committee on Bioethics wants:
- alternative therapies as an option for medical practice,
- the highest attainable standard of health,
- to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety.
When I first read these lines, I asked myself: who on earth wrote such nonsense? It was certainly not written by someone who understands healthcare, SCAM, and evidence-based medicine.
As discussed almost permanently on this blog, most forms of SCAM have not been shown to generate more good than harm. This means that employing them ‘as an option in medical practice’ cannot possibly produce ‘the highest attainable standards of health’. In fact, the UNESCO plan would lead to lower not higher standards. How can a committee on bioethics not realize that this is profoundly unethical?
Collaboration with practitioners of alternative therapies to evaluate SCAM’s effectiveness and safety sounds a bit more reasonable. It ignores, however, that tons of evidence already exist but fail to be positive. Why do these experts in bioethics not advocate to first make a sober assessment of the published literature?
I must say that the initiative of the UNESCO Committee on Bioethics puzzles me a lot and disturbs me even more.
I’d be keen to learn what you think of it.
This article by a Postgraduate Trainee (Dept. of Case Taking and Repertory, National Institute of Homoeopathy, Govt. of India) an Assistant Professor (Dept. of Surgery, National Institute of Homoeopathy Govt. of India) and another Assistant Professor (Dept. of Obstetrics & Gynaecology, Midnapore Homoeopathic Medical College & Hospital, Govt. of West Bengal) might not be available online (Clinical Medicine and Health Research Journal, Volume 03, Issue 03, May – June 2023 Page No. 444-446) but it is I think worth discussing. Here is its abstract:
Warts are one of the common dermatological disorders caused by human papilloma viruses encountered in our day to day life. These are cutaneous or mucosal infection needs proper care and treatment to prevent its transmission and complete healing. Although mostly warts are dealt with the therapeutic approach, i.e. on the basis of its peculiar type and location but it can even be successfully treated by constitutional approach. This article is regarding a case of warts treated successfully with Rhus Tox followed by Ferrum Met selected as the simillimum and proved its effectiveness in a short period of time.
As the abstract is not very informative, let me show you also some sections from the paper itself:
The patient presented with warts on right wrist for 1 year. There were plane warts at back of wrist, which was smooth, slightly elevated and skin coloured. There was no history of warts or other benign skin disease in the family. This case treated with individualized homoeopathic medicine showed complete resolution of the warts. There is no cure for wart in conventional medicine except removal of them with various methods. Although it does not rule out the chance of recurrence, later on may deep organic disease. That is why a substantial number of warts patients resort to Complementary and Alternative Medicine (CAM), especially homoeopathy.
In this case, Ferrum Metallicum 0/1 was selected as a ‘similimum’ based on totality of symptoms, repertorial analysis and consultation with Homoeopathic Materia Medica, which was given more priority in this case. After seeing improvement, succeeding potency was prescribed. After Ferrum Met 0/4 all her complaints including warts disappeared. Thus, the outcome of this case of Plane Warts of the lady shows the success of individualized homoeopathic medicine in treatment of wart.
Conclusion:
This case report suggests homoeopathic treatment as a promising complementary or alternative therapy and emphasizes the need of repertorisation in individualized homoeopathic prescription. This case shows a positive role of homoeopathic in treating Warts. However, this is a single case study and requires well designed studies which may be taken up for future scientific validation.
This case report reminded me of an exciting and quite lovely story: at Exeter, we once conducted a wart study. It was a placebo-controlled, double-blind trial where the verum group received distant healing and the controls nothing at all. After planning the study, I was no longer involved in its running. As I happened to have a wart at the time, I offered myself to my team as a patient. They checked me out and admitted me into the study. For the next weeks, I either received the distant healing energy or nothing; neither I nor my team knew which. My wart was photographed and measured regularly.
And then it happened: shortly after the treatment period was over, my wart had gone. Everyone was excited, especially the UK healing scene. But we had to wait until the trial was finished, the results were calculated, and the random code was opened. The result: no difference between verum and placebo! We concluded that distant healing from experienced healers had no effect on the number or size of patients’ warts.
And my own, very personal wart?
It had disappeared spontaneously – I had been in the control group!
I know Indian homeopaths have a thing about healing warts (we discussed this before) but I am afraid the conclusions of this new paper ought to be re-written:
This case report does not suggest that homeopathic treatment is a promising complementary or alternative therapy. It shows the natural history of the condition in the disappearance of warts.
The current secondary analysis based on the WHO database (VigiBase) of individual case safety reports (ICSRs) focuses on the suspected cutaneous adverse drug reactions (ADRs) linked to traditional medicines (TMs).
All the ICSRs reported between 1st January 2016 and 30th June 2021 from the UN Asia region in VigiBase where at least one TM was suspected to cause cutaneous ADRs were included in the study. Data regarding demographic details, suspected drug, adverse reaction as per MedDRA term, the seriousness of the reaction, de-challenge, re-challenge, and clinical outcome for suspected cutaneous ADRs associated with TM were obtained from VigiBase and analyzed for frequency of reported events and suspected medicines.
A total of 3,523 ICSRs with 5,761 ADRs related to “skin and subcutaneous tissue disorders” were included in the analysis. Amongst these, 6.8% of ICSRs were reported as serious.
The most common ADRs were:
- pruritus (29.6%),
- rash (20.3%),
- urticaria (18.9%),
- hyperhidrosis (3.3%).
Artemisia argyi H.Lév. and Vaniot. (14.9%), Ginkgo biloba L. (5.1%), Vitis vinifera L. (4%), Vitex agnus-castus L. (3.8%), Silybum marianum (L.), Gaertn (3.5%), and Viscus album L. (2.7%) were some commonly suspected TMs for cutaneous ADRs. There were 46 cases of Stevens-Johnson syndrome and toxic epidermal necrolysis reported with TMs during the study period. Death was reported in 5 ICSRs.
The authors concluded that TMs are linked with various cutaneous ADRS ranging from pruritus to toxic epidermal necrolysis which may have serious consequences. TMs listed as suspected offending agents in this analysis, should be kept in mind while dealing with suspected cutaneous ADRs. Clinicians should be more vigilant in detecting and reporting events associated with TMs.
Herbal remedies have a reputation for being time-tested, gentle, harmless, and benign. Reports such as this one might make us doubt this cliche. More importantly, they should force us to ask whether the remedy we are tempted to try truly does generate more good than harm. In most instances, I fear, the answer is not positive.
Maintenance of cognitive abilities is of critical importance to older adults, yet only a few effective strategies to slow down cognitive decline currently exist. Multivitamin supplementation is used to promote general health; however, it is unclear whether it favorably affects cognition in older age. This study aimed to examine the effect of daily multivitamin/multimineral supplementation on memory in older adults.
The Cocoa Supplement and Multivitamin Outcomes Study Web (COSMOS-Web) ancillary study (NCT04582617) included 3562 older adults. Participants were randomly assigned to a daily multivitamin supplement (Centrum Silver) or placebo and evaluated annually with an Internet-based battery of neuropsychological tests for 3 y. The prespecified primary outcome measure was change in episodic memory, operationally defined as immediate recall performance on the ModRey test, after 1 y of intervention. Secondary outcome measures included changes in episodic memory over 3 y of follow-up and changes in performance on neuropsychological tasks of novel object recognition and executive function over 3 y.
Compared with placebo, participants randomly assigned to multivitamin supplementation had significantly better ModRey immediate recall at 1 y, the primary endpoint (t(5889) = 2.25, P = 0.025), as well as across the 3 y of follow-up on average (t(5889) = 2.54, P = 0.011). Multivitamin supplementation had no significant effects on secondary outcomes. Based on a cross-sectional analysis of the association between age and performance on the ModRey, it was estimated that the effect of the multivitamin intervention improved memory performance above placebo by the equivalent of 3.1 y of age-related memory change.
The authors concluded that daily multivitamin supplementation, compared with placebo, improves memory. Multivitamin supplementation holds promise as a safe and accessible approach to maintaining cognitive health in older age.
These findings are surprising, not least because similar studies have thus far failed to demonstrate such effects. A 2013 trial, for instance, concluded that, in male physicians aged 65 years or older, long-term use of a daily multivitamin did not provide cognitive benefits.
Judging from the abstract alone (unfortunately, I have no access to the full paper), this seems to be a rigorous trial. It was conducted by multiple researchers of high standing. One is therefore inclined to believe the results.
Yet, one might be wise to be cautious.
Provided that a full analysis of the study does not identify major flaws, I would still want to 1) have a plausible explanation as to the mode of action and 2) see an independent replication before I accept the findings.
PS
The study was partly funded by the National Institutes of Health. The vitamins were provided by Pfizer Inc. and Haleon, the makers of the supplement used in the study.
PPS
I have now seen the full paper [thank you Dan] and can confirm that the study was of high quality. Yet, it also has limitations, of course, e.g.:
- the effect size is modest;
- the study population is selected and thus the results are not generalizable;
- the outcome measures were assessed remotely;
- the success of blinding was not checked [I find it conceivable that some trial participants tried to find out what they were taking, e.g. by tasting the pills].
An article in the German publication T-online is, I think, relevant to us here on this blog. I translated part of it for you:
The suspicion of particularly serious fraud against a doctor from the German Meißen district has been substantiated. Since the beginning of the pandemic, the 66-year-old physician is said to have issued “certificates of convenience” in the thousands throughout Germany, a spokesman for the public prosecutor’s office said. In return for a payment of 25 euros, the doctor from Moritzburg is said to have issued blanket and unjustified certificates stating that the wearing of mouth and nose protection was not medically justifiable. In other cases, the physician stated an unlimited inoculation prohibition or that Corona quick tests were possible only over saliva.
After an initial search in February, the public prosecutor’s office had assumed to be dealing with merely 162 false vaccination and mask certificates. But the extent of the fraud seems to go far beyond that: The accused is now said to have taken in at least 60,000 euros with the fake certificates.
Based on further investigations, the public prosecutor’s office assumes that the medical practitioner has managed to issue false corona attestations “every minute” with so-called collective appointments. These appointments were arranged in cooperation with Heilpraktiker from all parts of Germany and partly even with funeral homes.
On Tuesday, more than 360 police officers searched 140 homes of exemption certificate holders in nine states – mainly in Bavaria. In the process, 174 incorrect Corona attestations were found. They now must face instigations into using illegal health certificates. In addition, the office of a Bavarian Heilpraktiker, as well as a further commercial area, were searched.
This is not the first time that the Moritzburg doctor has come into conflict with the law. The 66-year-old physician considers herself a ‘Reichsbuerger’ (citizen of the Reich, a right-wing extremist). She was a member of the Moritzburg shooting club, and owned eleven weapons. Because they were not all registered and several hundred rounds of ammunition were found in the house, she stood trial for the first time already in 2014.
Although the use of so-called alternative medicine (SCAM) is said to be rising among older adults, many do
not discuss these healthcare practices with their primary care practitioners (PCPs). This recent US survey sought to determine the prevalence of SCAM use and to identify factors associated with SCAM disclosure among patients ages 65 and older.
Participants completed an anonymous survey, which evaluated their SCAM use over the past year and disclosure of SCAM to a PCP. Additional questions queried demographics, patient health, and relationships with one’s PCP. Analyses included descriptive statistics, chi-square tests, and logistic regression.
One hundred seventy-three participants answered surveys (response rate=23%). The Main findings were as follows:
- Sixty percent reported the use of at least one form of SCAM in the past year.
- Among those using SCAM, 64% disclosed use to their PCP.
- Patients disclosed supplements/herbal products and naturopathy/homeopathy/acupuncture at a higher rate than bodywork techniques and mind-body practices (71.9% and 66.7% vs. 48% and 50%).
- The only factor significantly associated with disclosure was trust in one’s PCP (odds ratio=2.97; confidence interval=1.01–8.73).
- The most commonly used types of SCAM were herbal products/dietary supplements (37.0%), mind-body therapies (28.9%), bodywork techniques (26.6%), and naturopathy/acupuncture/homeopathy (8.7%).
The authors concluded that clinicians may improve SCAM disclosure rates in older adults by inquiring about all types of SCAM and continuing to invest in their patient relationships, specifically by building trust.
The one-year prevalence of SCAM use – 60% – is extraordinary and considerably higher than in other surveys. How can this be explained?
I think that two factors might have played a role: firstly the survey was tiny, and secondly, its response rate was dismal. People who have no interest in SCAM would probably have not responded. Thus the prevalence figure is way too high and the survey is not representative of any population.
Having said that, I believe that some of the conclusions are still correct. As I have pointed out so often already:
- doctors need to ask their patients about SCAM usage;
- once they have identified a SCAM user, they need to advise him/her responsibly;
- to do that, they need to know about SCAM;
- as most doctors have little knowledge about the subject, they need to learn;
- failing to do that is not ethical behavior.
The ‘American Heart Association News’ recently reported the case of a 33-year-old woman who suffered a stroke after consulting a chiropractor. I take the liberty of reproducing sections of this article:
Kate Adamson liked exercising so much, her goal was to become a fitness trainer. She grew up in New Zealand playing golf and later, living in California, she worked out often while raising her two young daughters. Although she was healthy and ate well, she had occasional migraines. At age 33, they were getting worse and more frequent. One week, she had the worst headache of her life. It went on for days. She wasn’t sleeping well and got up early to take a shower. She felt a wave of dizziness. Her left side seemed to collapse. Adamson made her way down to the edge of the tub to rest. She was able to return to bed, where she woke up her husband, Steven Klugman. “I need help now,” she said.
Her next memory was seeing paramedics rushing into the house while her 3-year-old daughter, Stephanie, was in the arms of a neighbor. Rachel, her other daughter, then 18 months old, was still asleep. When she woke up in the hospital, Adamson found herself surrounded by doctors. Klugman was by her side. She could see them, hear them and understand them. But she could not move or react.
Doctors told Klugman that his wife had experienced a massive brain stem stroke. It was later thought to be related to neck manipulations she had received from a chiropractor for the migraines. The stroke resulted in what’s known as locked-in syndrome, a disorder of the nervous system. She was paralyzed except for the muscles that control eye movement. Adamson realized she could answer yes-or-no questions by blinking her eyes.
Klugman was told that Adamson had a very minimal chance of recovery. She was put on a ventilator to breathe, given nutrition through a feeding tube, and had to use a catheter. She learned to coordinate eye movements to an alphabet chart. This enabled her to make short sentences. “Am I going to die?” she asked one of her doctors. “No, we’re going to get you into rehab,” he said.
Adamson stayed in the ICU on life support for 70 days before being transferred to an acute rehabilitation facility. She could barely move a finger, but that small bit of progress gave her hope. In rehab, she slowly started to regain use of her right side; her left side remained paralyzed. Therapists taught her to swallow and to speak. She had to relearn to blow her nose, use the toilet and tie her shoes.
She was particularly fond of a social worker named Amy who would incorporate therapy exercises into visits with her children, such as bubble blowing to help her breathing. Amy, who Adamson became friends with, also helped the children adjust to seeing their mother in a wheelchair.
Adamson changed her dream job from fitness trainer to hospital social worker. She left rehab three and a half months later, still in a wheelchair but able to breathe, eat and use the toilet on her own. She continued outpatient rehab for another year. She assumed her left side would improve as her right side did. But it remained paralyzed. She would need to use a brace on her left leg to walk and couldn’t use her left arm and hand. Still, two years after the stroke, which happened in 1995, Adamson was able to drive with a few equipment modifications…
In 2018, Adamson reached another milestone. She graduated with a master’s degree in social work; she’d started college in 2011 at age 49. “It wasn’t easy going to school. I just had to take it a day at a time, a semester at a time,” she said. “The stroke has taught me I can walk through anything.” …
Now 60, she works with renal transplant and pulmonary patients, helping coordinate their services and care with the rest of the medical team at Vanderbilt University Medical Center. “Knowing that you’re making a difference in somebody’s life is very satisfying. It takes me back to when I was a patient – I’m always looking at how I would want to be treated,” she said. “I’ve really come full circle.”
Adamson has adapted to doing things one-handed in a two-handed world, such as cooking and tying her shoes. She also walks with a cane. To stay in shape, she works with a trainer doing functional exercises and strength training. She has a special glove that pulls her left hand into a fist, allowing her to use a rowing machine and stationary bike….
Adamson is especially determined when it comes to helping her patients. “I work really hard to be an example to them, to show that we are all capable of going through difficult life challenges while still maintaining a positive attitude and making a difference in the world.”
________________________
What can we learn from this story?
Mainly two things, in my view:
- We probably should avoid chiropractors and certainly not allow them to manipulate our necks. I know, chiros will say that the case proves nothing. I agree, it does not prove anything, but the mere suspicion that the lock-in syndrome was caused by a stroke that, in turn, was due to upper spinal manipulation plus the plethora of cases where causality is much clearer are, I think, enough to issue that caution.
- Having been in rehab medicine for much of my early career, I feel it is good to occasionally point out how important this sector often neglected part of healthcare can be. Rehab medicine has been a sensible form of multidisciplinary, integrative healthcare long before the enthusiasts of so-called alternative medicine jumped on the integrative bandwagon.
At first glance, the article entitled ‘Homeopathy: A State of the Science Review With Recommendations for Practical Therapies in Midwifery Practice‘ looks interesting and fairly solid; it was published in a mainstream, peer-reviewed midwifery journal; it is lengthy and thus seems thorough; it cites 125 references; and its two American authors have respectable affiliations (Art of Nursing Care Inc., Playa del Ray, California. Sonoran University of Health Sciences, Tempe, Arizona.). Yet, it does not take long to discover that ‘solid’ is not the term to describe it accurately. In fact, the paper is one of the worst examples of pseudo-science that I have ever come across. Let me just show you its conclusions:
This state of the science review has explored the history of homeopathy, its evidence base, manufacturing, regulation, and licensure. We have examined some of the controversies between homeopathy and conventional medicine in an effort to provide an overview and understanding of homeopathic science. Suggestions for practical therapies for use in midwifery practice have been given.
Despite misperceptions, homeopathy has become a well-established global practice with a growing body of research to support its benefits. Homeopathic medicines provide a comprehensive treatment approach to the myriad of conditions encountered in the midwifery practice model of care. With homeopathy’s generally accepted safety profile, low risk of side effects, few drug interactions, and low risk of overdose, midwives educated in homeopathic science can be confident that homeopathy provides a satisfactory complement for patients seeking alternative practices.
Increased opportunities for clinical research of homeopathic medicines by large funding organizations is recommended to advance patient care, understanding, and acceptance of the whole person and inform future health policy. Researchers around the world have begun to investigate the unanswered questions verifying the safety and efficacy of homeopathic treatment and the future of homeopathic research is promising. As homeopathic science continues to evolve, many health care professionals, including midwives, now seem open to adding homeopathy to complement their system of care for the whole person.
_______________________
In the article, we find two short paragraphs dealing with the effectiveness of homeopathy:
Essential to these debates are questions surrounding theories of homeopathy, such as the Law of Minimum Dose, like cures like, nonstandardized dosing, and symptom evaluation in a manner different from that of conventional medicine. It has been argued that the homeopathic paradigm is different from conventional scientific concepts associated with evidence-based medicine such as independent replication, confirmation of findings, measurement, and interpretation of results based on homeopathy’s reliance on individualized treatments and it basic tenets of the Principle of Similars and Law of Minimum Dose.69, 68 Conventional medicine practitioners find it counterintuitive that further dilution of a substance is believed to enhance its healing power when compared with a less dilute substance.65 For example, if the level of dilution is unmeasurable, how can the active ingredient be found, and is it even there?22 Recent research using nanopharmacology is beginning to uncover, identify, and characterize these ingredients in ultradiluted remedies and may help to answer these questions.39, 70 Debates arise concerning why individuals with similar symptoms often receive different treatments.22 Others ask whether homeopathic remedies perhaps inadvertently lead consumers to forgo conventional treatments that have been proven to work.5, 21, 22, 65
Interestingly, studies examining placebo therapies have appeared in scientific literature with increasing frequency, and some have compared the effectiveness of placebos with homeopathic remedies.68, 71–73 Multiple studies that have examined homeopathic treatments have found them equivalent to or no more effective than placebo,65, 68 whereas other studies found either measurable success or that patients perceived their outcomes as improved following homeopathic treatment.26, 75, 74 Mathie et al conducted a systematic review and meta-analysis focused on randomized controlled trials of nonindividualized homeopathic treatments. Authors reported that the quality of evidence was too low to determine whether homeopathic treatment results were distinguishable from those of placebo.72 These issues cited above represent some of the inconsistencies surrounding the theoretical basis and effectiveness of homeopathic therapies.
WHY WOULD ANY RESPECTABLE AUTHOR WRITE SUCH MISLEADING NONSENSE?
WHY WOULD ANY RESPECTABLE JOURNAL PUBLISH IT?
The answers to these questions might be found at the end of the paper:
Support for this supplement has been provided by Boiron USA. Boiron representatives provided no input into the article content.
Sharon Bond, CNM, PhD, who was an Associate Editor of the Journal of Midwifery & Women’s Health during the initial drafting of the manuscript, received compensation from Boiron USA for the assistance she provided the authors with editing and proofreading of the manuscript. Dr. Bond was not involved in the editorial review of or decision to publish this article.
The findings and conclusions in this supplement are those of the authors and do not necessarily reflect the official position of the host organizations, the American College of Nurse-Midwives, John Wiley & Sons, Inc., or the opinions of the journal editors.
I would argue that publishing such an article is unethical and amounts to scientific misconduct!
