Monthly Archives: November 2017
This is a fascinating new review of upper neck manipulation. It raises many concerns that we, on this blog, have been struggling with for years. I take the liberty of quoting a few passages which I feel are important and encourage everyone to study the report in full:
The Minister of Health, Seniors and Active Living gave direction to the Health Professions Advisory Council (“the Council”) to undertake a review related to high neck manipulation.
Specifically, the Minister directed the Council to undertake:
1) A review of the status of the reserved act in other Canadian jurisdictions,
2) A literature review related to the benefits to patients and risks to patient safety associated with the procedure, and
3) A jurisprudence review or a review into the legal issues that have arisen in Canada with respect to the performance of the procedure that touch upon the risk of harm to a patient.
In addition, the Minister requested the Council to seek written input on the issue from:
- Manitoba Chiropractic Stroke Survivors
- Manitoba Chiropractic Association
- College of Physiotherapists of Manitoba
- Manitoba Naturopathic Association
- College of Physicians and Surgeons of Manitoba
- other relevant interested parties as determined by the Council
… The review indicated that further research is required to:
- strengthen evidence for the efficacy of cervical spinal manipulations (CSM) as a treatment for neck pain and headache, “as well as for other indications where evidence currently does not exist (i.e., upper back and should/arm pain, high blood pressure, etc.)”
- establish safety and efficacy of CSM in infants and children
- assess the risk versus benefit in consideration of using HVLA cervical spine manipulation, which also involve cost-benefit analyses that compare CSM to other standard treatments.
… the performance of “high neck manipulation” or cervical spine manipulation does present a risk of harm to patients. This risk of harm must be understood by both the patient and the practitioner.
Both the jurisprudence review and the research literature review point to the need for the following actions to mitigate the risk of harm associated with the performance of cervical spine manipulation:
- Action One: Ensure that the patient provides written informed consent prior to initiating treatment which includes a discussion about the risk associated with cervical spine manipulation.
- Action Two: Provide patients with information to assist in the early recognition of a serious adverse event.
Chiropractic is hugely popular, we are often told. The fallacious implication is, of course, that popularity can serve as a surrogate measure for effectiveness. In the United States, chiropractors provided 18.6 million clinical services under Medicare in 2015, and overall spending for chiropractic services was estimated at USD $12.5 billion. Elsewhere, chiropractic seems to be less commonly used, and the global situation has not recently been outlined. The authors of this ‘global overview‘ might fill this gap by summarizing the current literature on the utilization of chiropractic services, reasons for seeking care, patient profiles, and assessment and treatment provided.
Systematic searches were conducted in MEDLINE, CINAHL, and Index to Chiropractic Literature from database inception to January 2016. Eligible articles
1) were published in English or French (not all that global then!);
2) were case series, descriptive, cross-sectional, or cohort studies;
3) described patients receiving chiropractic services;
4) reported on the following theme(s): utilization rates of chiropractic services; reasons for attending chiropractic care; profiles of chiropractic patients; or, types of chiropractic services provided.
The literature searches retrieved 328 studies (reported in 337 articles) that reported on chiropractic utilization (245 studies), reason for attending chiropractic care (85 studies), patient demographics (130 studies), and assessment and treatment provided (34 studies).
Globally, the median 12-month utilization of chiropractic services was 9.1% (interquartile range (IQR): 6.7%-13.1%) and remained stable between 1980 and 2015. Most patients consulting chiropractors were female (57.0%, IQR: 53.2%-60.0%) with a median age of 43.4 years (IQR: 39.6-48.0), and were employed.
The most common reported reasons for people attending chiropractic care were (median) low back pain (49.7%, IQR: 43.0%-60.2%), neck pain (22.5%, IQR: 16.3%-24.5%), and extremity problems (10.0%, IQR: 4.3%-22.0%). The most common treatment provided by chiropractors included (median) spinal manipulation (79.3%, IQR: 55.4%-91.3%), soft-tissue therapy (35.1%, IQR: 16.5%-52.0%), and formal patient education (31.3%, IQR: 22.6%-65.0%).
The authors concluded that this comprehensive overview on the world-wide state of the chiropractic profession documented trends in the literature over the last four decades. The findings support the diverse nature of chiropractic practice, although common trends emerged.
My interpretation of the data presented is somewhat different from that of the authors. For instance, I fail to share the notion that utilization remained stable over time.
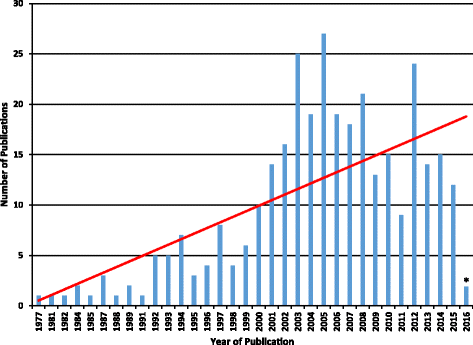
The figure might not be totally conclusive, but I seem to detect a peak in 2005, followed by a decline. Also, as the vast majority of studies originate from the US, I find it difficult to conclude anything about global trends in utilization.
Some of the more remarkable findings of this paper include the fact that 3.1% (IQR: 1.6%-6.1%) of the general population sought chiropractic care for visceral/non-musculoskeletal conditions. Some of the reasons for attending chiropractic care reported by the paediatric population are equally noteworthy: 7% for infections, 5% for asthma, and 5% for stomach problems. Globally, 5% of all consultations were for wellness/maintenance. None of these indications is even remotely evidence-based, of course.
Remarkably, 35% of chiropractors used X-ray diagnostics, and only 31% did a full history of their patients. Spinal manipulation was used by 79%, 31% sold nutritional supplements to their patients, and 10% used applied kinesiology.
In general, this is an informative paper. However, it suffers from a distinct lack of critical input. It seems to skip over almost all areas that might be less than favourable for chiropractors. The reason for this becomes clear, I think, when we read the source of funding for the research: PJHB, AEB, SAM and SDF have received research funding from the Canadian national and provincial chiropractic organizations, either as salary support or for research project funding. JJW received research project funding from the Ontario Chiropractic Association, outside the submitted work. SDF is Deputy Editor-in-Chief for Chiropractic and Manual Therapies; however, he did not have any involvement in the editorial process for this manuscript and was blinded from the editorial system for this paper from submission to decision.
Yes, I did promise to report on my participation in the ‘Goldenes Brett’ award which took place in Vienna and Hamburg on 23/11/2017. I had been asked to come to Vienna and do the laudation for the life-time achievement in producing ridiculous nonsense. This year, the award went to the ‘DEUTSCHER ZENTRALVEREIN HOMOEOPATHISCHER AERZTE’ (DZVhÄ), the German Central Society of Homoeopathic Doctors.
In my short speech, I pointed out that this group is a deserving recipient of this prestigious negative award. Founded in 1829, the DZVhÄ is a lobby-group aimed at promoting homeopathy where and how they can. It is partly responsible for the fact that homeopathy is still highly popular in Germany, and that many German consumers seem to think that homeopathy is an evidence-based therapy.
Cornelia Bajic, the current president of this organisation stated on her website that “Homöopathie hilft bei allen Krankheiten, die keiner chirurgischen oder intensivmedizinischen Behandlung bedürfen“ (homeopathy helps with all diseases which do not need surgical or intensive care), advice that, in my view, has the potential to kill millions.
The DZVhÄ also sponsors the publication of a large range of books such as ‘Was kann die Homoeopathie bei Krebs’ (What can homeopathy do for cancer?). This should be a very short volume consisting of just one page with just one word: NOTHING. But, in fact, it provides all sorts of therapeutic claims that are not supported by evidence and might seriously harm those cancer patients who take it seriously.
But the DZVhÄ does much, much more than just promotion. For instance it organises annual ‘scientific’ conferences – I have mentioned two of them previously here, here and here. In recent years one of its main activity must have been the defamation of certain critics of homeopathy. For instance, they supported Claus Fritzsche in his activities to defame me and others. And recently, they attacked Natalie Grams for her criticism of homeopathy. Only a few days ago, Cornelia Bajic attacked doctor Gram’s new book – embarrassingly, Bajic then had to admit that she had not even read the new book!
The master-stroke of the DZVhÄ , in my opinion, was the fact that they supported the 4 homeopathic doctors who went to Liberia during the Ebola crisis wanting to treat Ebola patients with homeopathy. At the time Bajic stated that “Unsere Erfahrung aus der Behandlung anderer Epidemien in der Geschichte der Medizin lässt den Schluss zu, dass eine homöopathische Behandlung die Sterblichkeitsrate der Ebola-Patienten signifikant verringern könnte” (Our experience with other epidemics in the history of medicine allows the conclusion that homeopathic treatment might significantly reduce the mortality of Ebola patients).
As I said: the DZVhÄ are a well-deserving winner of this award!
The fact that many dentists practice dubious alternative therapies receives relatively little attention. In 2016, for instance, Medline listed just 31 papers on the subject of ‘complementary alternative medicine, dentistry’, while there were more than 1800 on ‘complementary alternative medicine’. Similarly, I have discussed this topic just once before on this blog. Clearly, the practice of alternative medicine by dentists begs many questions – perhaps a new paper can answer some of them?
The aims of this study were to “analyse whether dentists offer or recommend complementary and alternative medicine (CAM) remedies in their clinical routine, and how effective these are rated by proponents and opponents. A second aim of this study was to give a profile of the dentists endorsing CAM.
A prospective, explorative, anonymised cross-sectional survey was spread among practicing dentists in Germany via congresses, dental periodicals and online (n=250, 55% male, 45% female; mean age 49.1±11.4years).
Of a set of 31 predefined CAM modalities, the dentists integrated plant extracts from Arnica montana (64%), chamomile (64%), clove (63%), Salvia officinalis (54%), relaxation therapies (62%), homeopathy (57%), osteopathic medicine (50%) and dietetics (50%). The effectiveness of specific treatments was rated significantly higher by CAM proponents than opponents. However, also CAM opponents classified some CAM remedies as highly effective, namely ear acupuncture, osteopathic medicine and clove.
With respect to the characteristic of the proponents, the majority of CAM-endorsing dentists were women. The mean age (50.4±0.9 vs 47.0±0.9years) and number of years of professional experience (24.2±1.0 vs 20.0±1.0years) were significantly higher for CAM proponents than the means for opponents. CAM proponents worked significantly less and their perceived workload was significantly lower. Their self-efficacy expectation (SEE) and work engagement (Utrecht work engagement, UWE) were significantly higher compared to dentists who abandoned these treatment options. The logistic regression model showed an increased association from CAM proponents with the UWES subscale dedication, with years of experience, and that men are less likely to be CAM proponents than women.
The authors concluded that various CAM treatments are recommended by German dentists and requested by their patients, but the scientific evidence for these treatments are often low or at least unclear. CAM proponents are often female, have higher SE and work engagement.
GIVE ME A BREAK!!!
These conclusion are mostly not based on the data provided.
The researchers seemed to insist on addressing utterly trivial questions.
They failed to engage in even a minimum amount of critical thinking.
If, for instance, dentists are convinced that ear-acupuncture is effective, they are in urgent need of some rigorous education in EBM, I would argue. And if they use a lot of unproven therapies, researchers should ask whether this phenomenon is not to a large extend motivated by their ambition to improve their income.
Holistic dentistry, as it is ironically often called (there is nothing ‘holistic’ about ripping off patients), is largely a con, and dentists who engage in such practices are mostly charlatans … but why does hardly anyone say so?
Malaria is an infection caused by protozoa usually transmitted via mosquito bites. Malaria is an important disease for homeopaths because of Hahnemann’s quinine experiment: it made him postulate his ‘like cures like’ theory. Today, many experts assume that Hahnemann misinterpreted the results of this experience. Yet most homeopaths are still convinced that potentised cinchona bark is an effective prophylaxis against malaria. Some homeopathic pharmacies still offer homeopathic immunisations against the infection. In several cases, this has caused people who believed to be protected fall ill with the infection.
Perhaps because of this long tradition, homeopaths seem to have difficulties giving up the idea that they hold the key to effective malaria prevention. An article published in THE INDIAN EXPRESS entitled ‘Research suggests hope for homoeopathic vaccine to treat malaria’ reminds us of this bizarre phenomenon:
…In a laboratory test set-up, an ultra-dilute homoeopathic preparation was prepared by extracting samples from Plasmodium falciparum, the parasite that causes malaria. The homoeopathic preparation was used in-vitro to check if it had anti-malarial activity… “Homoeopathy has been criticised for lack of scientific evidence. This lab-model test established that a medicine developed from an organism that causes malaria can be used to treat the infection,” said Dr Rajesh Shah, principal investigator in the research.
Following the tests, Shah is approaching the government in order to conduct a full-fledged clinical trial for the homoeopathic medicine. “We found that the homoeopathic medicine exhibited 65 per cent inhibition against malaria while chloroquine treatment has 54 per cent efficacy,” Shah claimed. The research was published in the International Journal of Medical and Health Research in July. It observed that the homoeopathic solution inhibited enzyme called hemozoin is known to have an anti-malarial effect…
END OF QUOTE
I thought this story was both remarkable and odd. So I looked up the original paper. Here is the abstract:
The inventor has developed malaria nosode and has subjected it for evaluation of antimalarial activity in vitro assay along with few other homeopathy preparations. The potential antimalarial activity of the Malaria nosode, Malaria officinalis and China officinalis was evaluated by β-Hematin Formation Assay. The hemozoin content was determined by measuring the absorbance at 400 nm. The results were recorded as % inhibition of heme crystallization compared to negative control (DMSO) Malaria nosode, Malaria officinalis and China officinalis exhibited inhibition of hemozoin and the inhibition was greater than the positive control Chloroquine diphosphate used in the study. The study has shown anti-disease activity of an ultra-dilute (potentized) homeopathic preparation. The Malaria nosode prepared by potentizing Plasmodium falciparum organisms has demonstrated antimalarial activity, which supports the basic principle behind homeopathy, the law of similar.
Now I am just as puzzled!
Why would any responsible scientist advocate running a ‘full-fledged clinical trial’ on the basis of such flimsy and implausible findings?
Would that not be highly unethical?
Would one not do further in-vitro tests?
Then perhaps some animal studies?
Followed by first studies in humans?
Followed perhaps by a small pilot study?
And, if all these have generated positive results, eventually a proper clinical trial?
The answers to all these questions is YES.
But not in homeopathy, it seems!
There has been a flurry of legal actions against manufacturers of homeopathic products (mostly) in the US. Many of these cases seem to settle out of court which means that we hardly hear about them. Of those that go to court, most are being won by the plaintiffs, but unfortunately some are also lost.
The recent case of Allen v. Hyland’s, Inc. is such an incidence. The US lawyer Robert G Knaier has analysed this case in detail and recently published a paper about it. The article is fascinating and well worth reading in full.
Here I take the liberty to show you a (shorted) section of Knaier’s paper where he asks what went wrong:
… How did a jury decide that Hyland’s did not misrepresent the efficacy of its products? Surely, the court’s instruction that Hyland’s would be liable only if the plaintiffs proved homeopathy “cannot work” contributed to the result. So long as defense experts were able to propose ways that homeopathy might work, the jury was left with the difficult decision—for laypersons, in any event—of rejecting that testimony.
But should the jury ever have been put in the position of having to make that choice? Should the defense experts ever have been allowed to testify? Had the court in Allen granted the plaintiffs’ motions to exclude those experts, the case likely would have ended with a settlement. Without the ability to put on evidence supporting its products, Hyland’s may very well have recognized that it had no realistic chance of prevailing at trial. But the court denied those motions.
In this respect, the court erred. There can be little doubt that expert testimony in support of the efficacy of homeopathy fails tests of admissibility. Consider the Federal Rules of Evidence and the factors that courts should evaluate under Daubert and its progeny. Is testimony that homeopathy is effective “the product of reliable principles and methods”?
In other words, does it have a “reliable foundation”? Is “the reasoning or methodology underlying [it] . . . scientifically valid”? As explained above, homeopathy’s core principles—provings, like cures like, and the law of minimum dose—are based on little more than Samuel Hahnemann’s late eighteenth-century speculations. They were not developed through, nor have they been validated by, controlled scientific studies… the principles and efficacy of homeopathy have been “tested” and “subjected to peer review and publication” — but they have consistently failed those tests and the scrutiny of that review process… Indeed, the FDA has stated that it simply is “not aware of scientific evidence to support homeopathy as effective.”
Thus, homeopathy’s “rate of error” is known, and far from gaining “general acceptance” in the scientific and medical community, it has gained near-universal condemnation. The defense of homeopathy, in some respects, presents a classic example of “unjustifiably extrapolat[ing] from an accepted premise to an unfounded conclusion.” Advocates extrapolate from the efficacy of vaccines that similia similibus currentur has a sound scientific basis, and from the concept of hormesis that providing ultralow doses is well-founded methodology. But as one contemporary skeptic has explained, unlike homeopathic remedies, vaccines actually “contain measurable numbers of antigen molecules,” and “act by well-understood scientific mechanisms”; and hormesis, even in the limited circumstances in which it appears to operate, “describes a response to a low dose, not to no dose.” As Martin Gardner noted many decades ago, the defense of homeopathy thus begins with plausible-sounding principles, and then “exaggerate[s] them to the point of absurdity.” In other words, it impermissibly extrapolates to “unfounded conclusion[s].”
Finally, the defense of homeopathy glaringly fails to “account for obvious alternative explanations.” Do people who take homeopathic remedies sometimes feel better? Of course they do. But studies of homeopathy have overwhelmingly concluded that the reason for this is not that homeopathy is actually efficacious, but rather because it is “the ideal placebo.” It is cheap. It has no side effects (unless, as discussed below, it is adulterated). And practitioners spend substantial time with their “patients,” thus encouraging psychosomatic effects.
In the end, advocates of homeopathy may have little to stand on other than that many people—including some “experts” who would gladly be paid to testify—inexplicably seem to believe that it works. But this will not do. That homeopathy has many believers does not validate it as a scientifically sound “field of expertise,” or color it, against nearly 200 years of evidence to the contrary, as one “known to reach reliable results for the type of opinion the expert would give.” As our Supreme Court perhaps most saliently observed, “general acceptance” of a principle cannot “help show that an expert’s testimony is reliable where the discipline itself lacks reliability.” As the Court explained, general acceptance of “principles of astrology or necromancy,” for example, would not transform those subjects into appropriately reliable subjects of expert testimony. The Court could easily have added homeopathy to that list.
Thus, in allowing the jury to receive testimony about the principles of homeopathy—not as a matter of historic curiosity, but as a matter of scientific validity—the Allen court arguably abdicated its gatekeeping responsibility to screen out unreliable expert testimony. By permitting “experts” to testify in favor of a field the bases of which defy basic principles of biology, chemistry, and physics — indeed, in some respects “basic logical principles” — the “integrity and fairness of the trial process” was compromised.
END OF QUOTE
I fully agree with Knaier. Allowing the ‘flat earth society’ to present to a court their views about the shape of our planet, while instructing the jury that they must accept them as ‘evidence’ (unless the plaintiff can prove it to be untrue) cannot be the right way forward. In fact, it is a method of preventing progress. Following this logic, I cannot imagine the proponents of any absurdity – however ridiculous – to not be victorious in court.
Knaier’s ultimate conclusion is, I think correct: “Trial courts have robust power and clear responsibility to preclude litigants from introducing irrelevant and unreliable evidence in support of purportedly scientific claims… To the extent that courts continue abdicating their evidentiary gatekeeping role in this way, they may contribute to a waste of time and resources, financial harm to consumers, and risks to public health. But to the extent that litigants and courts strengthen their spines in this regard, take seriously the dangers of unfounded expert testimony, and make genuine efforts to seek and grant its exclusion, they might contribute to the health and well-being of both the courts and those who turn to them for help.”
Several national organisations of sceptics give annual awards to people and institutions who do outstanding work and those who do the opposite. Later this week, I will travel to Vienna, for instance, to give away one of this year’s ‘GOLDENES BRETT’, a negative prize for the most outrageous BS of 2017. Such things are good fun but also important tools in fighting nonsense. I probably will report about it when I am back.
Earlier this year, the UK sceptics awarded Gwyneth Paltrow with the well-earned RUSTY RAZOR. The ‘Bent Spoon’ is a similar type of prize. It has just been awarded by the Australian Skeptics to the proponent of the most preposterous piece of pseudoscientific or paranormal piffle of the year. Past winners have included Pete ’Paleo’ Evans, the CSIRO’s head Larry Marshall, the ABC, the Pharmacy Guild of Australia, the University of Wollongong, and a psychic dentist.
This year’s nominations are listed here. The winner of the 2017 Bent Spoon is the National Institute of Complementary Medicine at the University of Western Sydney. “When they were nominated last year they said they’d have a closer look at their site,” said Eran Segev, president of Australian Skeptics Inc. “But they’re still promoting unproven treatments and now also involved in a project to establish a clinic for Traditional Chinese Medicine on the campus of the University of Western Sydney. The 2017 winner’s involvement is described as ‘clinical trials’, but the University acknowledges that the TCM clinic may be opened to the public – a highly dubious pseudomedicine given the imprimatur of university ‘research’. “
On this blog, we have discussed several of the NICM’s papers. An interesting article about the NICM can also be found here. To give you an additional flavour of their research, here are the conclusions of just 5 of their recent articles:
CONCLUSION: In our study of acupuncture for menopausal hot flashes, higher expectancy after the first treatment did not predict better treatment outcomes. Future research may focus on other determinants of outcomes in acupuncture such as therapist attention. The relationship between smoking and hot flashes is poorly understood and needs further exploration.
Conclusion: There is a clear need to understand breast cancer survivors’ needs for physical and psychological support as they aim to regain control over their life through their experience of illness. More studies are needed to measure and evaluate these outcomes and to help identify breast cancer survivors’ healthcare seeking behaviours, during and after the acute treatment stage that addresses their physical, emotional, and spiritual needs. These results aim to inform future research design and evaluate and develop support services that are patient-centred and focus on whole health outcomes, shared decision-making, and quality of life.
CONCLUSION: These results are important for healthcare providers as they work with patients to identify life experiences, including ‘loss/potential loss’ and ‘the need for preservation’, that have personal significance. Some patients may realize that ‘enough is enough’; something needs to change. These intrinsic motivating factors may also be the impetus for eventual recovery for some individuals.
CONCLUSIONS: 16 weeks of Bikram yoga significantly improved perceived stress, general self-efficacy and HRQoL in sedentary, stressed adults. Future research should consider ways to optimise adherence, and should investigate effects of Bikram yoga intervention in other populations at risk for stress-related illness.
CONCLUSIONS: These findings suggest that long-term acupuncture treatment has targeted regulatory effects on multiple brain regions in rats with Alzheimer’s disease.
The ‘Bent Spoon’ was awarded mostly, I think, because of the persistently misleading claims made on the websites of the NICM. Go and have a look – I am sure you will agree: they are highly deserving winners.
In my opinion, these awards deserve our support. They are an effective means of fighting charlatans and promoting progress. They should be publicised much more widely.
This is too wonderful (I found it on Twitter where it was posted by ‘Doctors Leonard and Michael Valentine’, chiropractors at Valentine Chiropractic in Fountain Valley, CA.) – I have to show it to you.

This could almost pass without a comment. But for what it’s worth, here are my 7 points:
- platitude,
- platitude,
- no, they do not easily move out of alignment, and if they do, you are severely ill and need urgent treatment but not chiropractic,
- subluxations as dreamt up by chiropractors are a myth; they simply do not exist,
- it is vital that we don’t disclose this BS, if not chiros need to find new jobs,
- chiros pretend to find subluxations because this is their livelihood,
- pathetic platitude.
This article is worth reading, I think.
It again begs the question whether the GCC is fit for purpose.
START OF QUOTE
AN ILKLEY chiropractor has been found guilty of unacceptable professional conduct by the General Chiropractic Council (GCC).
Dr John Rees, who works at Ilkley Chiropractic Clinic, Wilmot House, Railway Road, appeared before the Professional Conduct Committee of the Council at a hearing in London from November 6 to 8. Dr Rees faced allegations in relation to a female patient, known as patient A, who was registered under the care of Mr Rees on various dates between May 20, 2016 and June 10, 2016 and June 11, 2016 and June 15, 2016.
The committee found the admitted particulars proved, however, other, more serious allegations he had been facing, but had always denied, were dropped as there was no reliable evidence to support them. Ms Harris for the GCC told the hearing that notwithstanding the concessions made by the GCC the registrant’s behaviour, even if well received by the patient, was inappropriate, an abuse of the patient-practitioner relationship and the sort of behaviour that brings the profession into disrepute.
Dr Rees was represented at the hearing by Mr Kitching who described the events of 2016 as “a professional disaster for the registrant, an embarrassment which he regretted on a personal and professional level.” Mr Kitching submitted that physical contact with patient A had gone no further than drinks, a kiss, a hug and that the matters were at the lower end of the scale of breaches. He invited the committee to consider patient A had been a willing participant and was both intelligent and mature and could not be considered as vulnerable.
However, the committee determined that Dr Rees’s behaviour “embraced both a risk to the reputation of the profession and also the protection of patients. The committee added: “Whilst much of the behaviour had been consensual the registrant had been in a position of power, he had planned the progression of the relationship and this amounted to serious acts on his behalf.”
The hearing concluded that Dr Rees’s conduct “fell seriously below the standards expected of a chiropractor and that, consequently, Dr Rees is guilty of unacceptable professional conduct.” In making a sanction against Dr Rees the committee noted a wide range of supportive testimonials and references and his previous good character. The committee was satisfied that the misconduct was not “fundamentally incompatible with continued registration”. It imposed the sanction of an admonishment – a formal warning – upon Dr Rees.
Following the hearing Dr Rees told the Gazette: “My professional body has considered all the pertinent facts and come to its decision. The matter is now closed. I would like to thank my patients for their generous support during this difficult period.”
END OF QUOTE
ADDITIONAL INFO COPIED FROM THE GCC ‘NOTICE OF DECISION’:
- The kiss or attempted kiss was ‘on the lips’.
- Rees gave the patient presents, including a bikini.
- Rees attended patient’s home address.
- Rees seems to have falsified the patient’s case notes and thus ‘acted dishonestly’.
- Rees called the patient ‘an evil loose woman’, ‘a bunny boiler’ and ‘a slapper’.
Do I understand this right? The GCC concluded that “much of the behaviour had been consensual”. To me, this indicates that some of the behaviour was not consensual. How then could the GCC find that Rees’s behaviour was compatible with continued registration? And how could they imposed merely a formal warning upon Dr Rees?
I fail to comprehend this verdict.
Also I fail to understand why Rees allows himself to be called a ‘doctor’.
And I again ask: IS THE GCC FIT FOR PURPOSE?
Chiropractors are often proud of offering drugless treatments to their patients. Many even have an outright aversion against drugs which goes back to their founding father, DD Palmer, who disapproved of pharmaceuticals. On this background it seems surprising that, today, some chiropractors lobby hard to get prescription rights.
A recent article explains:
A legislative proposal that would allow Wisconsin chiropractors to prescribe narcotics has divided those in the profession and pitted those of them who support the idea against medical doctors. At a hearing on the bill Tuesday, representatives form the Wisconsin Chiropractic Association said back pain is a common reason people go see a medical doctor, but they argue that chiropractors with additional training could be helping those patients instead. Under the bill, chiropractors would be able to write prescriptions for painkillers and administer anesthesia under the direction of a physician.
Expanding the scope of practice, the WCA said, would give patients with pain faster relief when primary care physicians are busy. The Wisconsin Medical Society, though, has come out against the proposal. “This expands to something not seen anywhere else in the country,” said Don Dexter, chief medical officer for WMS.
Meanwhile, another chiropractic group, the Chiropractic Society of Wisconsin, is also skeptical. “We contend there is no public need or demand … to allow chiropractors to prescribe drugs,” said Dean Shepherd, the group’s president.
Opponents also pointed out that the changes could increase access to opioids at a time the state is trying to reduce abuse. “As you know, based on legislation passed in the last two sessions, we’re already dealing with an epidemic of opioid overuse,” Dexter said. “We don’t need new providers prescribing those medications.”
However, some practicing chiropractors like Jason Mackey, with Leutke Storm Mackey Chiropractic in Madison, argue that medical fields evolve: “We have always had change throughout the course of our professsion.” Mackey said there has been pushback with previous changes, like using X-ray or certain therapies and recommending vitamins.
END OF QUOTE
On this blog, we discussed the issue of chiropractic prescribing before. At the time, I argued against such a move and gave the following reasons:
- Patients might be put at risk by chiropractors who are less than competent in prescribing medicines.
- More unnecessary NAISDs would be prescribed.
- The vast majority of the drugs in question is already available OTC.
- Healthcare costs would increase.
- Prescribing rights would give more legitimacy to a profession that arguably does not deserve it.
- Chiropractors would then continue their lobby work and soon demand the prescription rights to be extended to other classes of drugs.
Considering the chiropractors’ arguments for prescribing rights stated in the above article, I see little reason to change my mind.
