politics
Online misinformation is disproportionality created and spread by people with extreme political attitudes, especially among the far-right. There is a debate in the literature about why people spread misinformation and what should be done about it. According to the purely cognitive account, people largely spread misinformation because they are lazy, not biased. According to a motivational account, people are also motivated to believe and spread misinformation for ideological and partisan reasons. To better understand the psychological and neurocognitive processes that underlie misinformation sharing among the far-right, an international team of researchers conducted a cross-cultural experiment with conservatives and far-right partisans in the Unites States and Spain (N = 1,609) and a neuroimaging study with far-right partisans in Spain (N = 36).
Far-right partisans in Spain and U.S. Republicans who highly identify with Trump were more likely to share misinformation than center-right voters and other Republicans, especially when the misinformation was related to sacred values (e.g., immigration). Sacred values predicted misinformation sharing above and beyond familiarity, attitude strength, and salience of the issue. Moreover, far-right partisans were unresponsive to fact-checking and accuracy nudges. At a neural level, this group showed increased activity in brain regions implicated in mentalizing and norm compliance in response to posts with sacred values.
The authors concluded that these results suggest that the two components of political devotion – identity fusion and sacred values – play a key role in misinformation sharing, highlighting the identity-affirming dimension of misinformation sharing. We discuss the need for motivational and identity-based interventions to help curb misinformation for high-risk partisan groups.
People who have followed the discussions on this blog closely could be forgiven in assuming that right-wing political devotion also plays an important role in spreading misinformation about healthcare (e.g. vaccination) and so-called alternative medicine (SCAM). It would be good, if someone could test this hypothesis more directly.
PS
Just as I had finished writing this post, I came across a quote given yesterday by Ben Habib on GBN:
“I’m very reluctant to put my destiny in the hands of scientists. You know, unbridled authority given to faux knowledge.”
QED
We discussed the 2015 Australian NHMRC report on homeopathy many times before, e.g.:
- Homeopathy: the 2015 NHMRC report and its criticism re-analysed
- HOMEOPATHY: the NHMRC report revisited
- Ombudsman investigates ‘flawed’ homeopathic study
- The final verdict on homeopathy: it’s a placebo
In a nutshell, the report was an hugely influential analysis of the effectiveness of homeopathy which came to squarely negative conclusions. Thus it was celebrated as a thorough and conclusive piece evidence demonstrating the madness of homeopathy. Unsurprisingly, homeopaths did not like it at all and produced various criticisms claiming that it was neither thorough nor conclusive.
Now the final evaluation of what has been going on was finally published (ISSUED BY THE COMMONWEALTH OMBUDSMAN, IAIN ANDERSON, ON 4 AUGUST 2023):
The Office of the Commonwealth Ombudsman (the Office) has finalised an investigation relating to the National Health and Medical Research Council’s (NHMRC) review of the evidence for the effectiveness of homeopathy, conducted between 2010 and 2015. We commenced this investigation in September 2017 in response to concerns raised with us about how the NHMRC review had proceeded.
The Office conducts its investigations in private, and the Ombudsman generally does not make a public statement in the absence of a formal report. In the circumstances of this matter, including that the then-Ombudsman released a public statement on 4 June 2021 which acknowledged the Office was investigating, we believe it is important to share publicly the information we can, now that the investigation is complete.
Our investigation was finalised in July 2023. We acknowledge the length of time the investigation has taken. This is in part due to the extensive efforts the Office made to source independent scientific expertise to advise us on some detailed and specific questions of scientific methodology that were raised with our Office, including some that were only brought to our attention as our investigation progressed. Despite our best efforts, it was not possible to engage an expert (or experts) to provide independent advice to our Office on this subject. In the absence of independent, expert scientific expertise we have not been able to conclusively determine those matters of scientific methodology. This did not prevent our Office from forming a view on other aspects of the matter.
Our investigation did not result in any adverse findings about the review or the NHMRC. When finalising investigations, we may offer comments and suggestions to an agency about areas for future improvement. In this instance, we offered comments and suggestions to the NHMRC about how it records and publicly explains decisions about its activities. The NHMRC also independently made several improvements to its processes during the course of our investigation.
________________
In essence, this means that the conclusions of the report stand:
Homeopathy should not be used to treat health conditions that are chronic, serious, or could become serious. People who choose homeopathy may put their health at risk if they reject or delay treatments for which there is good evidence for safety and effectiveness. People who are considering whether to use homeopathy should first get advice from a registered health practitioner. Those who use homeopathy should tell their health practitioner and should keep taking any prescribed treatments.
Thus the matter is closed – that is closed for rational thinkers. For irrationalists, the matter will no doubt continue to be a stone of contention. No, homeopath will be able to accept these conclusions simply because a member of a cult ceases to be a cultist once he/she accepts the criticism agaist the cult.
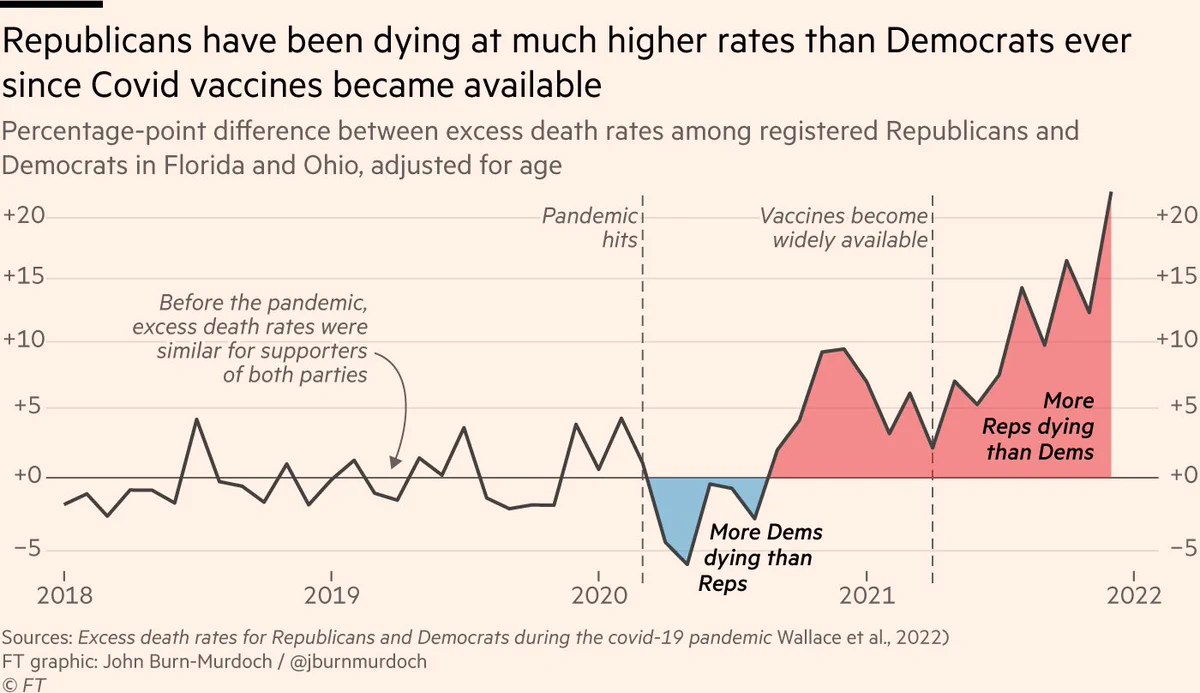
There is evidence that, in the US, Republican-leaning counties have had higher COVID-19 death rates than Democratic-leaning counties and similar evidence of an association between political party affiliation and attitudes regarding COVID-19 vaccination. This investigation assessed political party affiliation and mortality rates for individuals during the initial 22 months of the COVID-19 pandemic.
A cross-sectional comparison of excess mortality between registered Republican and Democratic voters between March 2020 and December 2021 adjusted for age and state of voter registration was conducted. Voter and mortality data from Florida and Ohio in 2017 linked to mortality records for January 1, 2018, to December 31, 2021, were used in data analysis. The main outcome measure was the excess weekly death rates during the COVID-19 pandemic adjusted for age, county, party affiliation, and seasonality.
Between January 1, 2018, and December 31, 2021, there were 538 159 individuals in Ohio and Florida who died at the age of 25 years or older in the study sample. The median age at death was 78 years (IQR, 71-89 years). Overall, the excess death rate for Republican voters was 2.8 percentage points, or 15%, higher than the excess death rate for Democratic voters (95% prediction interval [PI], 1.6-3.7 percentage points). After May 1, 2021, when vaccines were available to all adults, the excess death rate gap between Republican and Democratic voters widened from −0.9 percentage points (95% PI, −2.5 to 0.3 percentage points) to 7.7 percentage points (95% PI, 6.0-9.3 percentage points) in the adjusted analysis; the excess death rate among Republican voters was 43% higher than the excess death rate among Democratic voters. The gap in excess death rates between Republican and Democratic voters was larger in counties with lower vaccination rates and was primarily noted in voters residing in Ohio.
The authors concluded that, in this cross-sectional study, an association was observed between political party affiliation and excess deaths in Ohio and Florida after COVID-19 vaccines were available to all adults. These findings suggest that differences in vaccination attitudes and reported uptake between Republican and Democratic voters may have been factors in the severity and trajectory of the pandemic in the US.
In light of what has been discussed repeatedly, these findings are in my view most impressive and seem to speak for themselves. The authors are nevertheless prudent and stress that their study has several limitations which mean that we ought to interpret their results with caution.
- First, there are plausible alternative explanations for the difference in excess death rates by political party affiliation beyond the explanatory role of vaccines discussed herein.
- Second, the mortality data, although detailed and recent, only included approximately 83.5% of deaths in the US and did not include the cause of death. Although overall excess death patterns in our data are similar to those in other reliable sources, such as the Centers for Disease Control and Prevention National Center for Health Statistics data, it is possible that the deaths that our study data did not include may disproportionately occur among individuals registered with a particular political party, potentially biasing our results. In addition, the completeness of the mortality data may vary across states or time, potentially biasing our estimates of excess death rates.
- Third, all excess death models rely on fundamentally untestable assumptions to construct the baseline number of deaths one would expect in the absence of the COVID-19 pandemic.
- Fourth, because no information on individual vaccination status was available, analyses of the association between vaccination rates and excess deaths relied on county-level vaccination rates.
- Fifth, the study was based on data from 2 states with readily obtainable historical voter registration information (Florida and Ohio); hence, the results may not generalize to other states.
We have discussed the currently fashionable herbal remedy, ‘kratom‘, before:
Inadequate regulation of Kratom supplements put consumers at risk
News about Kratom: the herb was recently (semi-)legalized in Thailand
Kratom: a ‘herbal drug’ with the potental to do more harm than good
A quick recap:
Kratom is made of the leaves of Mitragyna speciosa, a tree endogenous to parts of Southeast Asia. It has been used traditionally for its stimulant, mood-elevating, and analgesic effects. The plant’s active constituents, mitragynine and 7-hydroxymitragynine, have been shown to modulate opioid receptors, acting as partial agonists at mu-opioid receptors and competitive antagonists at kappa- and delta-opioid receptors. Both alkaloids are G protein-biased agonists of the mu-opioid receptor and therefore, may induce less respiratory depression than classical opioid agonists. The Mitragyna alkaloids also appear to exert diverse activities at other brain receptors (including adrenergic, serotonergic, and dopaminergic receptors), which may explain the complex pharmacological profile of raw kratom extracts. By the early 2000s, kratom was increasingly used in the US as a substitute for prescription and illicit opioids for managing pain and opioid withdrawal by people seeking abstinence from opioids. There are numerous assessments where people have been unable to stop using kratom and withdrawal signs and symptoms are problematic. Kratom does not appear in normal drug screens and, when taken with other substances of abuse, may not be recognized.
Now it has been reported that the family of a Florida woman who died in 2021 after ingesting kratom has been awarded more than $11m from a distributor of the herbal extract. “There is of course no amount of money that will make up for the pain and suffering that Ms Talavera’s children are enduring because of their mother’s death,” Middlebrooks wrote in court records addressing the sanction against Kratom Distro. “The law nonetheless recognizes that the defendant must pay something, however inadequate.”
The US Drug Enforcement Agency in 2016 had imposed its strictest restrictions on kratom, which is made from the leaves of an evergreen tree and is often used by people to self-treat pain, anxiety, depression, and opioid addiction as well as withdrawal. There was an intense, immediate public backlash to that approach, however, and it prompted the DEA to rescind its prohibition of kratom, which is sold in stores and online.
The US Food and Drug Administration nonetheless has warned consumers over possible safety and addiction risks associated with kratom, and it has spoken in favor of more research aimed at gaining a better understanding of “the substance and its components”.
Friends of Talavera, a resident of the Florida community of Boynton Beach, introduced her to kratom years before her death. Her family said she regarded it as a safe, natural supplement and had taken some after buying it online from the Kratom Distro when her partner and the father of her youngest child – Biagio Vultaggio – found her unconscious in the living room on 20 June 2021. The 39-year-old Talavera was face down on the ground next to an open bag of a kratom derivative marketed as a “space dust”, her family has said. Vultaggio called paramedics, and they took Talavera to a hospital where she was pronounced dead. An autopsy later listed Talavera’s cause of death as acute intoxication from mitragynine, the main kratom component. The local coroner wrote in a report that “at high concentrations, mitragynine produces opioid-like effects, such as respiratory failure”.
________________________
Kratom Disro claims that 
Product Consistency
- Our kratom powder is sourced directly from Indonesia monthly. Your order was literally on a farm in Indonesia two months ago. No old powder.
- Our kratom extracts are produced in the US by a licensed chemist and a professionally trained staff.
- We only use delicious flavors and quality ingredients.
Complete Transparency
- Every batch of products we receive is lab tested and will not ship out without meeting our meticulous quality standards.
- Current labs – We will never show you an out-of-date lab with our products.
- Guaranteed purity levels and free of all toxins.
Get It When You Want It
- Many orders shipped same day.
- USPS shipping on all orders under 6 pounds.
- Larger orders can ship USPS Priority for a small additional charge.
_________________________________
Back to the above lawsuit:
One of the attorneys for Talavera’s family, Tamara Williams, said in a statement that the judgment won by her clients “should be a wakeup call to the kratom industry”. Williams’s law firm had also recently won a $2.5m jury verdict against a kratom manufacturer in Washington state after a separate lawsuit alleging wrongful death. A colleague of Williams called on government officials to take steps “to protect other families from having to deal with unnecessary kratom overdose deaths”.
Sobrenix (Kudzu, Milk Thistle, B Vitamins & More) is “designed to reduce alcohol cravings and help you detoxify your body so you can successfully manage alcohol consumption. Even better, taken before drinking, Sobrenix’s ingredients help you stop before you’ve had too much. DETOXIFY YOUR BODY with a powerful formula that combines herbs and nutrients that support liver health, curb cravings, and help you wake up without a nasty hangover. Sobrenix kick-starts the detoxification process with essential herbs like Milk Thistle and Chanca Piedra. Additionally, the formula contains the critical B-Vitamins that alcohol washes away so you can wake up happy and healthy again!”
Yes, you suspected correctly: this is pure BS!
Not only that but the Federal Trade Commission is taking action under the FTC Act and the Opioid Addiction Recovery Fraud Prevention Act of 2018 (OARFPA) against the makers of Sobrenix. According to the FTC’s complaint, the makers, a company, Rejuvica, and its owners, Kyle Armstrong and Kyle Dilger, made numerous unsubstantiated and false claims about Sobrenix and used paid endorsers in deceptively formatted advertising. The defendants also used bogus review sites to deceive consumers about their products.
As a result of the FTC’s suit, the defendants have agreed to a proposed court order that would permanently ban them from making any unsubstantiated claims about healthcare products or services, as well as require them to pay $650,000 to the FTC to be used for providing refunds to consumers.
“We will not tire in our pursuit of those who prey on individuals struggling with alcohol or other substance use disorders,” said Samuel Levine, Director of the Bureau of Consumer Protection. “This case evidences the breadth of the FTC’s authority to pursue such wrongdoing under both the FTC Act and OARFPA.”
The FTC charges that the defendants marketed Sobrenix with messages like:
- “STRUGGLING TO CONTROL YOUR ALCOHOL CONSUMPTION? Sobrenix is designed to reduce alcohol cravings and help you detoxify your body so you can successfully manage alcohol consumption. Even better, taken before drinking, Sobrenix’s ingredients help you stop before you’ve had too much.”
The FTC charges that Rejuvica and its owners lacked adequate evidence to support these claims. The complaint charges that Rejuvica, Armstrong, and Dilger violated both the FTC Act and OARFPA. The proposed order contains a total monetary judgment of $3,247,737, which is partially suspended based on the defendants’ inability to pay the full amount. The defendants will be required to pay $650,000 to the FTC to be used to refund consumers. If the defendants are found to have lied to the FTC about their financial status, the full judgment will be immediately due.
______________________________
A few short comments might be in order:
- Regulators have the duty to protect consumers from false health claims.
- It is commendable that some authorities sometimes do their duty and go after some of the people responsible for making false claims related to dietary supplements.
- Such actions should, however, occur MUCH more often.
- They ought to happen also in countries other than the US.
- Similar actions should be initiated against ALL false claims made for healthcare products and services.
- This means that all practitioners of so-called alternative medicine (SCAM) would need to review their advertising, websites, etc., and erase therapeutic claims that are not supported by evidence.
- This would unquestionably amount to an enormously valuable service to public health.
- Most countries already have legislation that would make such steps possible; my question, therefore, is this:
WHY ARE CONSUMERS NOT ADEQUATELY PROTECTED BY THEIR NATIONAL REGULATORS FROM CHARLATANS WHO SELL INEFFECTIVE AND OFTEN DANGEROUS SCAMs AT HIGH COSTS?
The website of the World Federation of Chiropractic (WFC) points out that public health is defined by the WHO as follows:
“Activities to strengthen public health capacities and service aim to provide conditions under which people can maintain to be healthy, improve their health and wellbeing, or prevent the deterioration of their health. Public health focuses on the entire spectrum of health and wellbeing, not only the eradication of particular diseases.”
The WFC then continues stating this:
As primary contact health professionals, chiropractors can play an important role as public health advocates. This can range from providing support and advice on health matters such as physical activity, diet, and fitness as well as lifestyle choices such as injury prevention and avoiding tobacco use. Chiropractors can also play a role in counselling patients and communities on the benefits of public health measures, especially as this relates to immediate health needs of each region.
I think that this might merit a few comments.
- Physical activity is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Diet is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Fitness is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Lifestyle choice is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Injury prevention is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Avoiding tobacco use is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Counseling is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
So, what is the real contribution of chiropractors to public health?
- Chiropractors tend to advise their clients against vaccinations.
- Some mislead the public by claiming they boost immunity and prevent serious infections.
- Many undermine evidence-based medicine by promoting obsolete myths such as ‘the innate’ or subluxations.
- Many sell supplements that could interact with prescription drugs.
- Many make bogus health claims for profit.
I would therefore argue that, on balance, the contribution of chiropractors to public health might be considerable …
sadly, however, it goes in the wrong direction.
As the organizer of several demos in the area of Linz, Austria, a ‘corona activist’ and ‘Holocaust denier’ had repeatedly made headlines over the past two years. Now the 39-year-old Austrian man is in the headlines yet again.
It has been reported that, on the evening of July 23, he was stopped by the police for a routine traffic control. His three children, aged 15, 11, and 5, were also in the car. “I know I’m wanted. I don’t have a driver’s license and I have a dead body in the trunk,” he said as he got out of the car. As the officers soon realized, he was only partly joking. A legal case for Holocaust denial was pending against the man who had not appeared at his main hearing last August, so a search was underway for him.
When police officers checked the car, they made the horrifying discovery. In the trunk was a woman’s body, wrapped in sheets. The dead woman turned out to be the wife, aged 38, of the driver. According to preliminary findings, she had died 4 hours earlier. Apparently, she had suffered from incurable cancer, and the police suspect that the illness had not been treated – her husband did not just not believe in vaccinations but disliked all drugs.
The husband, who already had several previous convictions, claimed that he was on his way to bury his wife somewhere “in nature”. The 39-year-old man was arrested and is now in pre-trial detention – though not for the incident with his wife’s body, but for Holocaust denial. He is said to have compared the Corona measures to the Holocaust, and the arrest order was issued because he failed to appear for his trial.
_________________________
One does not need to be a clairvoyant to predict that this remarkable man will come up with more surprises. I wonder what he might think of next.
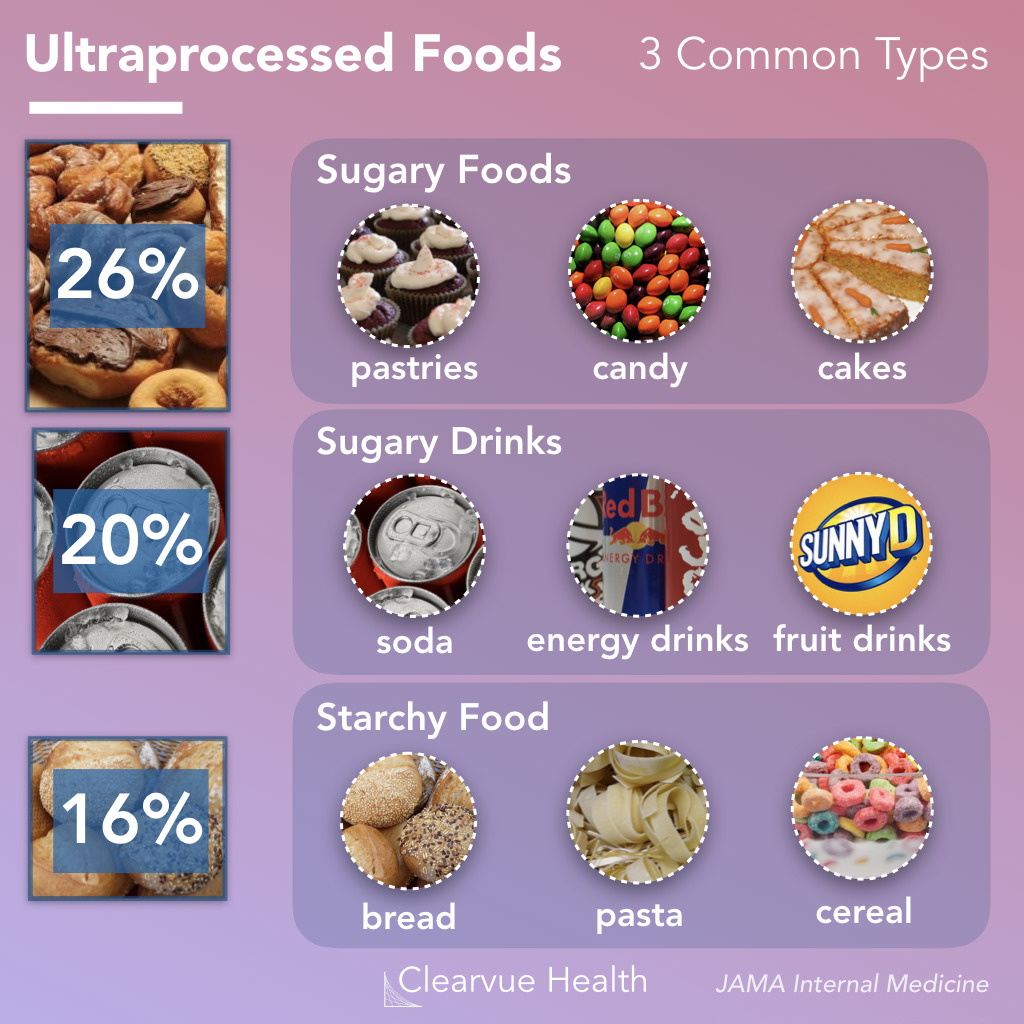
Like ultra-processed food (UPF) itself, the subject of UPF is everywhere – radio, TV, Twitter, you name it, the topic crops up. I too could not resist writing a post on it a few months ago. And now I am publishing another one but one in a slightly more irritated mood.
Why do these endless discussions on UPF irritate me?
To start with, there is no uniform definition of UPF, and many commentators seem more than a little confused about what UPF actually is. One definition holds that Ultra-processed foods are foods that have been altered to include fats, starches, sugars, salts and hydrogenated oils extracted from other foods. They contain ingredients, additives, and preservatives that are not normally used in home cooking. It seems obvious that discussions on UPF without a clear and understandable definition of the term are merely generating confusion in the general public.
But there are, of course, lists of UPF that might render the subject a bit clearer. The trouble, however, is that these lists reveal disagreement among each other. Thus they are prone to generate even more confusion.
Next, there is the evidence – and there is lots of it. It suggests that the regular consumption of UPF is bad for virtually every aspect of health. And if there is no evidence that it is detrimental for a given condition, it probably is merely because nobody has yet bothered to do the analyses. The trouble is, however, that all the relevant research comes from either basic science or epidemiology. This means that causality is unproven.
A further problem is that even the experts don’t know what the alleged causal factors in UPF are.
- Is it the processing?
- The additives?
- The sugar?
- The fats?
- If so, which fats exactly?
- Is it perhaps a complex inter-play of some of these factors?
If we want to make progress, we need to know! If not, we cannot possibly begin to avoid the health-threatening effects of UPF.
The final and arguably biggest problem is that UPF is everywhere. Nobody living in an industrialized country and earning a regular living can avoid consuming UPF. This means, I fear, that all the current hype about UPF is not just irritating but possibly counter-productive.
Imagine an average person trying to make sense of these discussions. She would soon give up and conclude that all these ‘clever’ experts know nothing at all. Her foremost concern is to make ends meet. In the end, she will carry on as before. Alternatively, she might even conclude that, as the even experts do not make sense, UPF cannot be all that bad after all.
After reading about and listening to the arguments around UPF, I ask myself this: would it not be more productive to apply more common sense and focus on a few nutritional messages that are 1) solidly based on evidence and 2) an average person can actually follow?
We have discussed dental amalgam and its risks to human health before. Finally, there is new legislation in sight. The European Commission has revised the EU Mercury Regulation to protect EU citizens and the environment from toxic mercury. Among other things, this will completely ban the use of dental amalgam, for which 40 tons of mercury are currently consumed annually in the EU. The revised mercury ordinance provides for the following:
– No more use of dental amalgam from January 1, 2025; viable mercury-free alternatives are available.
– Ban on the manufacture and export of dental amalgam from the EU from January 1, 2025;
– Ban on the manufacture and export of six mercury-containing lamps from January 1, 2026 and January 1, 2028 (depending on lamp type).
The delegated act adopted under the Mercury Regulation transposes into EU law the decisions taken at the fourth Conference of the Parties (2022) to the Minamata Convention by introducing a ban on the production, import, and export of eight additional mercury-containing products, including mercury-containing lamps and non-electrical equipment.
The Minamata Convention is the main international legal framework for the protection of human health and the environment from anthropogenic emissions and releases of mercury to air, water, and soil. Like the Mercury Regulation, it addresses the entire life cycle of mercury, from primary mercury mining to mercury waste management.
The revised Mercury Regulation must now be approved by the European Parliament and the Council under the ordinary legislative procedure. The delegated act will be sent to the European Parliament and the Council for consideration.
Mercury is a highly toxic chemical that poses a threat to both human health and the environment. When released into the environment, it enters the food chain where it accumulates (mainly in fish). High mercury exposure can damage the brain, lungs, kidneys, and immune system.
Historically, mercury has been used in a wide range of applications, including gold mining, batteries, fluorescent tubes, thermometers, and barometers. Over the last twenty years, the EU has developed a comprehensive body of legislation, in particular the Mercury Regulation, which protects human health and the environment from anthropogenic emissions and releases of mercury, taking into account the entire life cycle of mercury from primary mercury mining to final disposal of mercury waste. It also includes measures on trade in mercury-containing products and mercury pollution.
The Minamata Convention entered into force on August 16, 2017, and has so far been ratified by the European Union and 143 countries, including all EU Member States. The fifth session of the Conference of the Parties to the Minamata Convention on Mercury (COP-5) will be held in Geneva, Switzerland, from October 30 to November 3, 2023.
_____________________________
I don’t usually find reading medical papers scary. An article in the prestigious journal ‘Nature’ is the exception. Here is its abstract:
Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. Estimated numbers vary but the assumption is that, of all those who had COVID-19 globally, at least 10% have long COVID. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new health-care challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein–Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. Thus, the current picture is one of convergence towards a map of an immunopathogenic aetiology of long COVID, though as yet with insufficient data for a mechanistic synthesis or to fully inform therapeutic pathways.
The paper ends with this gloomy statement: “The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID. The biggest unknowns remain the joined-up scheme of its pathogenesis and thus the best candidate therapeutics to be trialled in randomized controlled trials, along with a better understanding of the kinetics of recovery and the factors influencing this. Some countries have invested in first-round funding for the pilot investigations. From the above, far more will be needed.”
In the context of this blog, we must, of course, ask: HAS SO-CALLED ALTERNATIVE MEDICINE (SCAM) SOMETHING TO OFFER?
I’m afraid that the short answer to this question is No!
However, one does not need to be a clairvoyant to predict that lots of therapeutic claims followed by plenty of methodologically weak (to put it politely) research will emerge from SCAM. Already some time ago, this homeopath indicated, that SCAM providers should see COVID as an opportunity: For homeopathy, shunned during its 200 years of existence by conventional medicine, this outbreak is a key opportunity to show potentially the contribution it can make in treating COVID-19 patients.
We should not hold our breath to see the emergence of convincing evidence, but we must be prepared to warn the public from getting exploited by charlatans.