politics
This analysis was aimed at quantifying how many studies registered on the Open Science Framework (OSF) up to November 2017 are performed but not shared after at least 4 years. Examining a sample of 315 registrations, of which 169 were research studies, the researchers found that 104 (62%) were published. They estimated that 5550 out of 9544 (58%) registered studies on the OSF are published.
Researchers use registries to make unpublished studies public, and the OSF policy to open registrations after a four-year embargo substantially increases the number of studies that become known to the scientific community. In responses to emails asking researchers why studies remained unpublished logistical issues (e.g., lack of time, researchers changing jobs) were the most common cause, followed by null results, and rejections during peer review.
The authors concluded that their study shows that a substantial amount of studies researchers perform remain unpublished.
I find this truly shocking!
Researchers are able to do research only because they receive financial and other support from elsewhere. Therefore they have an ethical obligation to publish it. The reasons frequently given for not publishing research are nothing well and truly invalid:
- Lack of time is a mere excuse; if researchers had the time to get the grants, permissions, etc. they simply must have the time to finish the job properly.
- Researchers changing jobs is an equally flawed excuse; if someone changes position, he/she is obliged to finish the job they were doing. A surgeon can also not leave mid-surgery because he has a better offer.
- ‘Null results’ is even worse as a reason. Null results are just as important as positive findings – occasionally they are even more important. If researchers fail to realize this, they simply disqualify themselves as researchers.
- ‘Rejections during peer review’ is complete nonsense. Everyone who submits papers for publication gets rejected once in a while. In this case, one learns from the peer-review comments, improves the paper in question, and re-submits it to another journal.
I have seen many studies of so-called alternative medicine (SCAM) that, for this or that reason, never were published. And I feel strongly that this is a serious violation of research ethics – so much so that I would ban researchers who are guilty of this crime from conducting research in the future. I also feel that, in order to receive the necessary support (financial and other), researchers should sign that they will publish their findings within a given time after finishing their study. Failing to comply could then incur a penalty such as paying back part of the funds wasted. I think such measures would very quickly clear up the current intolerable situation.
The General Chiropractic Council (GCC) “regulates chiropractors in the UK to ensure the safety of patients undergoing chiropractic treatment”. One might have assumed that they thus fulfill the important role of controlling the profession. Yet, one would have assumed wrongly. Instead of controlling, the GCC usually prefers promoting the profession. Their recent Chiropractic Patient Satisfaction and Experience is a good example. Let me show you several important sections of this document:
The outcomes reported here highlight two key findings:
• Overwhelmingly, chiropractic patients report high levels of satisfaction and positive experiences with their care. This was true both in the literature that examined international patient cohorts as well as the specific data collected from UK based chiropractic patients.
• A strong therapeutic relationship and good communication between patient and chiropractor underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based chiropractic patients.
Conclusion
This report shows that both existing literature and de novo data collection from patients receiving chiropractic care in the UK highlight excellent perceived experience and high satisfaction with such care.
Factors such as therapeutic alliance and communication are strongly associated with these positive perceptions by patients although other factors such as treatment beliefs were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of care, both in terms of clinical outcomes and patient experience, chiropractors should be explicitly skilled at curating excellent therapeutic alliances and communication with patients.
• Such skills and competences within chiropractic care delivery should receive higher visibility within the chiropractic profession generally and more specifically through advocacy within leading institutions and core emphasis within chiropractic curricula.
__________________________
By changing a few words, I have adapted the above excerpts to become a Customer Satisfaction and Experience Report of a fictitious hamburger joint published by the Hamburger General Council (HGC) of Great Britain which regulates hamburger joints in the UK to ensure the safety of consumers undergoing hamburger nutrition:
The outcomes reported here highlight two key findings:
• Overwhelmingly, customers report high levels of satisfaction and positive experiences with their restaurant. This was true both in the literature that examined international consumer cohorts as well as the specific data collected from UK based customers.
• A strong professional relationship and good communication between customer and service personell underpins high satisfaction scores and a positive experience. This was confirmed both in the international literature and through both quantitative and qualitative analysis of specific data collected from UK based hamburger consumers.
Conclusion
This report shows that both existing literature and de novo data collection from consumers eating hamburgers in the UK highlight excellent perceived experience and high satisfaction with such service.
Factors such as personal alliance and communication are strongly associated with these positive perceptions by consumers although other factors such as appetite were also significantly associated with satisfaction scores.
Recommendations
• To offer the highest quality of service, both in terms of profit and patient experience, hamburger vendors should be explicitly skilled at curating excellent professional alliances and communication with customers.
• Such skills and competences within hamburger delivery should receive higher visibility within the gastronomic trade generally and more specifically through advocacy within leading institutions and core emphasis within servers’ curricula.
___________________________
If you get the impression that I am taking the Mickey of the GCC, you are not mistaken. Yet, this post also has slightly more serious purposes. I wanted to 1) show how, in the chiropractic profession, pure BS is often disguised as research, and 2) question whether the GCC is fit for purpose.
On a more constructive note: there are many open questions that urgently need addressing in the realm of chiropractic (e.g. do chiropractors more good than harm?). I, therefore, suggest that the GCC stops publishing idiotic promotional documents disguised as research and gets on with its responsibilities.
Previous research revealed that cognitive abilities are negatively related to right-wing and prejudiced attitudes. No study has, however, investigated if emotional abilities also show such a relationship, although this can be expected based on both classic and recent literature. The aim of the present study was 2-fold:
(a) to investigate the relationship between emotional abilities and right-wing and prejudiced attitudes, and
(b) to pit the effects of emotional and cognitive abilities on these attitudes against each other.
Results from 2 adult samples (n = 409 and 574) in which abilities scores were collected in individual testing sessions, revealed that emotional abilities are significantly and negatively related to social-cultural and economic-hierarchical right-wing attitudes, as well as to blatant ethnic prejudice. These relationships were as strong as those found for cognitive abilities. For economic-hierarchical right-wing attitudes, emotional abilities were even the only significant correlate.
The authors concluded that the study of emotional abilities has the potential to significantly advance our understanding of right-wing and prejudiced attitudes.
__________
The researchers found that individuals with weaker emotional abilities — particularly emotional understanding and management — tended to score higher on a measure of right-wing authoritarianism and social dominance orientation. Right-wing authoritarianism is a personality trait that describes the tendency to submit to political authority and be hostile towards other groups, while social dominance orientation is a measure of a person’s preference for inequality among social groups.
The results of this study were univocal. People who endorse authority and strong leaders and who do not mind inequality — the two basic dimensions underlying right-wing political ideology — show lower levels of emotional abilities,” said Van Hiel, the lead author of the study. “Those with lower emotional and cognitive abilities were also more likely to agree with blatantly prejudiced statements such as “The White race is superior to all other races.”
Of course, the study only collected correlational data, preventing inferences of causality from being made. “Caution should be exercised in the interpretation of such results,” Van Hiel said. “One cannot discredit any ideology on the basis of such results as those presently obtained. Only in a distant future, we will be able to look back upon our times, and then we can maybe judge which ideologies were the best. Cognitively and emotionally smart people can make wrong decisions as well. The results have been obtained in one particular context. Would similar results be obtained in other contexts besides in a Western country with a long-standing stable democracy? Whether these tendencies are universal, or limited to particular contexts, is very intriguing.”
Numerous qualitative studies and a few quantitative studies have linked vaccine hesitancy or refusal with the belief in the efficacy of so-called alternative medicine (SCAM). Yet, large-scale data on this topic are scarce. In this study, the French researchers investigated the factors associated with the coverage rates of seven childhood vaccines or vaccine groups in the ninety-six metropolitan French departments. One of the factors investigated was the local interest in SCAM. In order to assess this interest, they built an Alternative Medicine Index based on departmental internet searches regarding SCAM—internet searches being a reliable indicator of the public’s actual interest in a given topic. They then conducted multiple regression analyses, which showed that this Index is a significant explanatory factor for the departmental variance in vaccination coverage rates, exceeding in importance the effect of other relevant local sociodemographic factors.
A further recent study from France adds to the picture. It presents the results of a survey conducted in July 2021 among a representative sample of the French mainland adult population (n = 3087). Using cluster analysis, the researchers identified five profiles of SCAM attitudes and found that even among the most pro-SCAM group, very few respondents disagreed with the idea that SCAM should only be used as a complement to conventional medicine. They then compared these SCAM attitudes to vaccine attitudes. Attitudes to SCAM had a distinct impact as well as a combined effect on attitudes to different vaccines and vaccines in general. They found that:
- attitudes to SCAM provide a very limited explanation of vaccine hesitancy;
- among the hesitant, pro-SCAM attitudes are often combined with other traits associated with vaccine hesitancy such as distrust of health agencies, radical political preferences, and low income.
Both SCAM endorsement and vaccine hesitancy are more prevalent among the socially disadvantaged. Drawing on these results, the researchers argue that, to better understand the relationship between SCAM and vaccine hesitancy, it is necessary to look at how both can reflect a lack of access and recourse to mainstream medicine and distrust of public institutions.
 The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- Sorry, I was wrong about homeopathy and vaccination
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
What seems fairly clear to me is that a cross-correlation exists: an attitude against modern medicine and the ‘scientific establishment’ determines both the enthusiasm for SCAM and the aversion to vaccination. What is, however, far from clear to me is what we could do about it.
Yes, better education seems important – and that’s precisely what I aim at achieving with this blog. Sadly, judging from some of the comments we receive, it does not seem crowned with much success.
Any other ideas?
“The decline of homeopathy, the ‘medicine’ that doesn’t cure anything” is the title of a remarkable article in EL PAIS of which I take the liberty of showing you a few key passages:
In the more than 200 years that have passed since its invention, no one has been able to prove that homeopathy is actually capable of curing anything with its alleged medicines that have no active ingredients…
…EL PAÍS reached out to some of its main promoters, such as the pharmaceutical company Boiron, leader in the sector; the Spanish Association of Homeopathy Pharmacists and the Spanish Society of Homeopathic Doctors. In the absence of a response from all three, the explanations are given by experts who are more critical of the discipline.
Many people who used to consume homeopathy were not even aware that this was the case. Fernando Frías, one of the activists who worked to undermine the discipline’s remaining prestige, recalls that people did not believe them when they were told that compounds with diluted Berlin Wall were sold to overcome the feelings of oppression and anxiety. This was actually commercialized under the premise that “like cures like”: if the Berlin Wall oppressed, a piece of it diluted in water should remedy it. “Many were under the impression that it was just a natural therapy and that we were making things up to attack it,” says Frías…
… There has been a lot of debate about how to regulate an alleged drug whose only effect is, in truth, the placebo effect. In 2001, the European Parliament issued a directive that covered its use in countries with a homeopathic tradition; sources explain that this happened due to the pressure exerted by both the industries and the governments of countries where pseudoscience is deep-rooted, such as France (where Boiron is headquartered) or Germany, where its consumption is much higher than in others, such as Spain.
“Having regard to the particular characteristics of these homeopathic medicinal products, such as the very low level of active principles they contain and the difficulty of applying to them the conventional statistical methods relating to clinical trials, it is desirable to provide a special, simplified registration procedure for those homeopathic medicinal products which are placed on the market without therapeutic indications in a pharmaceutical form and dosage which do not present a risk for the patient,” states the directive.
In its more than two centuries of history, this is not the first time that homeopathy loses ground. Still, Frías warns, it cannot be ruled out that at some point something will come up that will make it fashionable again. “Look at the example of chemtrails [the condensation trails left by airplanes that some conspiracy theorists believe are a way of poisoning the population from the air]. It seemed that no one remembered them anymore, but now they’re back,” he says. Frías cites the astrophysicist and disseminator Javier Armentia, who states that beliefs are like a rubber duck: no matter how much they sink, they always resurface. “Especially if there is money behind,” he adds.
______________________
As reported previously, homeopathy and other forms of so-called alternative medicine (SCAM) have come under fire in Spain. In 2017, ‘HOMEOPATHY PLUS‘ reported that “in a reversal of the 2015 Royal Legislative Decree, the Minister of Health has withdrawn homeopathic remedies and outlawed the practice in Spain’s national health services.” In 2018, more than 400 people signed an open letter triggered by the case of a cancer patient who died after preferring homeopathy to regular treatment. “Let’s be clear: pseudoscience kills,” begins the letter. Since then, the struggle of Spanish rational thinkers to stop misleading information about SCAM in general and homeopathy, in particular, has only intensified.
Spain is thus joining other European countries in opposing misinformation about homeopathy. Contrary to what some have claimed (for instance, in the comments section of this blog), most of the opponents do not want to restrict the public’s choice. People who wish to use homeopathy should be able to do so (but should pay for it themselves). However, the choice must be based on evidence-based information.
On this blog, we have some people who continue to promote conspiracy theories about Covid and Covid vaccinations. It is, therefore, time, I feel, to present them with some solid evidence on the subject (even though it means departing from our usual focus on SCAM).
This Cochrane review assessed the efficacy and safety of COVID‐19 vaccines (as a full primary vaccination series or a booster dose) against SARS‐CoV‐2. An impressive team of investigators searched the Cochrane COVID‐19 Study Register and the COVID‐19 L·OVE platform (last search date 5 November 2021). They also searched the WHO International Clinical Trials Registry Platform, regulatory agency websites, and Retraction Watch. They included randomized controlled trials (RCTs) comparing COVID‐19 vaccines to placebo, no vaccine, other active vaccines, or other vaccine schedules.
A total of 41 RCTs could be included and analyzed assessing 12 different vaccines, including homologous and heterologous vaccine schedules and the effect of booster doses. Thirty‐two RCTs were multicentre and five were multinational. The sample sizes of RCTs were 60 to 44,325 participants. Participants were aged: 18 years or older in 36 RCTs; 12 years or older in one RCT; 12 to 17 years in two RCTs; and three to 17 years in two RCTs. Twenty‐nine RCTs provided results for individuals aged over 60 years, and three RCTs included immunocompromised patients. No trials included pregnant women. Sixteen RCTs had two‐month follow-ups or less, 20 RCTs had two to six months, and five RCTs had greater than six to 12 months or less. Eighteen reports were based on preplanned interim analyses. The overall risk of bias was low for all outcomes in eight RCTs, while 33 had concerns for at least one outcome. 343 registered RCTs with results not yet available were identified.The evidence for mortality was generally sparse and of low or very low certainty for all WHO‐approved vaccines, except AD26.COV2.S (Janssen), which probably reduces the risk of all‐cause mortality (risk ratio (RR) 0.25, 95% CI 0.09 to 0.67; 1 RCT, 43,783 participants; high‐certainty evidence).High‐certainty evidence was found that BNT162b2 (BioNtech/Fosun Pharma/Pfizer), mRNA‐1273 (ModernaTx), ChAdOx1 (Oxford/AstraZeneca), Ad26.COV2.S, BBIBP‐CorV (Sinopharm‐Beijing), and BBV152 (Bharat Biotect) reduce the incidence of symptomatic COVID‐19 compared to placebo (vaccine efficacy (VE): BNT162b2: 97.84%, 95% CI 44.25% to 99.92%; 2 RCTs, 44,077 participants; mRNA‐1273: 93.20%, 95% CI 91.06% to 94.83%; 2 RCTs, 31,632 participants; ChAdOx1: 70.23%, 95% CI 62.10% to 76.62%; 2 RCTs, 43,390 participants; Ad26.COV2.S: 66.90%, 95% CI 59.10% to 73.40%; 1 RCT, 39,058 participants; BBIBP‐CorV: 78.10%, 95% CI 64.80% to 86.30%; 1 RCT, 25,463 participants; BBV152: 77.80%, 95% CI 65.20% to 86.40%; 1 RCT, 16,973 participants).Moderate‐certainty evidence was found that NVX‐CoV2373 (Novavax) probably reduces the incidence of symptomatic COVID‐19 compared to placebo (VE 82.91%, 95% CI 50.49% to 94.10%; 3 RCTs, 42,175 participants).There is low‐certainty evidence for CoronaVac (Sinovac) for this outcome (VE 69.81%, 95% CI 12.27% to 89.61%; 2 RCTs, 19,852 participants).High‐certainty evidence was found that BNT162b2, mRNA‐1273, Ad26.COV2.S, and BBV152 result in a large reduction in the incidence of severe or critical disease due to COVID‐19 compared to placebo (VE: BNT162b2: 95.70%, 95% CI 73.90% to 99.90%; 1 RCT, 46,077 participants; mRNA‐1273: 98.20%, 95% CI 92.80% to 99.60%; 1 RCT, 28,451 participants; AD26.COV2.S: 76.30%, 95% CI 57.90% to 87.50%; 1 RCT, 39,058 participants; BBV152: 93.40%, 95% CI 57.10% to 99.80%; 1 RCT, 16,976 participants).
Moderate‐certainty evidence was found that NVX‐CoV2373 probably reduces the incidence of severe or critical COVID‐19 (VE 100.00%, 95% CI 86.99% to 100.00%; 1 RCT, 25,452 participants).
Two trials reported high efficacy of CoronaVac for severe or critical disease with wide CIs, but these results could not be pooled.
mRNA‐1273, ChAdOx1 (Oxford‐AstraZeneca)/SII‐ChAdOx1 (Serum Institute of India), Ad26.COV2.S, and BBV152 probably result in little or no difference in serious adverse events (SAEs) compared to placebo (RR: mRNA‐1273: 0.92, 95% CI 0.78 to 1.08; 2 RCTs, 34,072 participants; ChAdOx1/SII‐ChAdOx1: 0.88, 95% CI 0.72 to 1.07; 7 RCTs, 58,182 participants; Ad26.COV2.S: 0.92, 95% CI 0.69 to 1.22; 1 RCT, 43,783 participants); BBV152: 0.65, 95% CI 0.43 to 0.97; 1 RCT, 25,928 participants). In each of these, the likely absolute difference in effects was fewer than 5/1000 participants.
Evidence for SAEs is uncertain for BNT162b2, CoronaVac, BBIBP‐CorV, and NVX‐CoV2373 compared to placebo (RR: BNT162b2: 1.30, 95% CI 0.55 to 3.07; 2 RCTs, 46,107 participants; CoronaVac: 0.97, 95% CI 0.62 to 1.51; 4 RCTs, 23,139 participants; BBIBP‐CorV: 0.76, 95% CI 0.54 to 1.06; 1 RCT, 26,924 participants; NVX‐CoV2373: 0.92, 95% CI 0.74 to 1.14; 4 RCTs, 38,802 participants).
The authors’ conclusions were as follows: Compared to placebo, most vaccines reduce, or likely reduce, the proportion of participants with confirmed symptomatic COVID‐19, and for some, there is high‐certainty evidence that they reduce severe or critical disease. There is probably little or no difference between most vaccines and placebo for serious adverse events. Over 300 registered RCTs are evaluating the efficacy of COVID‐19 vaccines, and this review is updated regularly on the COVID‐NMA platform (covid-nma.com).
_____________________
As some conspiratorial loons will undoubtedly claim that this review is deeply biased; it might be relevant to add the conflicts of interest of its authors:
- Carolina Graña: none known.
- Lina Ghosn: none known.
- Theodoros Evrenoglou: none known.
- Alexander Jarde: none known.
- Silvia Minozzi: no relevant interests; Joint Co‐ordinating Editor and Method editor of the Drugs and Alcohol Group.
- Hanna Bergman: Cochrane Response – consultant; WHO – grant/contract (Cochrane Response was commissioned by the WHO to perform review tasks that contribute to this publication).
- Brian Buckley: none known.
- Katrin Probyn: Cochrane Response – consultant; WHO – consultant (Cochrane Response was commissioned to perform review tasks that contribute to this publication).
- Gemma Villanueva: Cochrane Response – employment (Cochrane Response has been commissioned by WHO to perform parts of this systematic review).
- Nicholas Henschke: Cochrane Response – consultant; WHO – consultant (Cochrane Response was commissioned by the WHO to perform review tasks that contributed to this publication).
- Hillary Bonnet: none known.
- Rouba Assi: none known.
- Sonia Menon: P95 – consultant.
- Melanie Marti: no relevant interests; Medical Officer at WHO.
- Declan Devane: Health Research Board (HRB) – grant/contract; registered nurse and registered midwife but no longer in clinical practice; Editor, Cochrane Pregnancy and Childbirth Group.
- Patrick Mallon: AstraZeneca – Advisory Board; spoken of vaccine effectiveness to media (print, online, and live); works as a consultant in a hospital that provides vaccinations; employed by St Vincent’s University Hospital.
- Jean‐Daniel Lelievre: no relevant interests; published numerous interviews in the national press on the subject of COVID vaccination; Head of the Department of Infectious Diseases and Clinical Immunology CHU Henri Mondor APHP, Créteil; WHO (IVRI‐AC): expert Vaccelarate (European project on COVID19 Vaccine): head of WP; involved with COVICOMPARE P et M Studies (APHP, INSERM) (public fundings).
- Lisa Askie: no relevant interests; Co‐convenor, Cochrane Prospective Meta‐analysis Methods Group.
- Tamara Kredo: no relevant interests; Medical Officer in an Infectious Diseases Clinic at Tygerberg Hospital, Stellenbosch University.
- Gabriel Ferrand: none known.
- Mauricia Davidson: none known.
- Carolina Riveros: no relevant interests; works as an epidemiologist.
- David Tovey: no relevant interests; Emeritus Editor in Chief, Feedback Editors for 2 Cochrane review groups.
- Joerg J Meerpohl: no relevant interests; member of the German Standing Vaccination Committee (STIKO).
- Giacomo Grasselli: Pfizer – speaking engagement.
- Gabriel Rada: none known.
- Asbjørn Hróbjartsson: no relevant interests; Cochrane Methodology Review Group Editor.
- Philippe Ravaud: no relevant interests; involved with Mariette CORIMUNO‐19 Collaborative 2021, the Ministry of Health, Programme Hospitalier de Recherche Clinique, Foundation for Medical Research, and AP‐HP Foundation.
- Anna Chaimani: none known.
- Isabelle Boutron: no relevant interests; member of Cochrane Editorial Board.
___________________________
And as some might say this analysis is not new, here are two further papers just out:
Objectives To determine the association between covid-19 vaccination types and doses with adverse outcomes of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection during the periods of delta (B.1.617.2) and omicron (B.1.1.529) variant predominance.
Design Retrospective cohort.
Setting US Veterans Affairs healthcare system.
Participants Adults (≥18 years) who are affiliated to Veterans Affairs with a first documented SARS-CoV-2 infection during the periods of delta (1 July-30 November 2021) or omicron (1 January-30 June 2022) variant predominance. The combined cohorts had a mean age of 59.4 (standard deviation 16.3) and 87% were male.
Interventions Covid-19 vaccination with mRNA vaccines (BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna)) and adenovirus vector vaccine (Ad26.COV2.S (Janssen/Johnson & Johnson)).
Main outcome measures Stay in hospital, intensive care unit admission, use of ventilation, and mortality measured 30 days after a positive test result for SARS-CoV-2.
Results In the delta period, 95 336 patients had infections with 47.6% having at least one vaccine dose, compared with 184 653 patients in the omicron period, with 72.6% vaccinated. After adjustment for patient demographic and clinical characteristics, in the delta period, two doses of the mRNA vaccines were associated with lower odds of hospital admission (adjusted odds ratio 0.41 (95% confidence interval 0.39 to 0.43)), intensive care unit admission (0.33 (0.31 to 0.36)), ventilation (0.27 (0.24 to 0.30)), and death (0.21 (0.19 to 0.23)), compared with no vaccination. In the omicron period, receipt of two mRNA doses were associated with lower odds of hospital admission (0.60 (0.57 to 0.63)), intensive care unit admission (0.57 (0.53 to 0.62)), ventilation (0.59 (0.51 to 0.67)), and death (0.43 (0.39 to 0.48)). Additionally, a third mRNA dose was associated with lower odds of all outcomes compared with two doses: hospital admission (0.65 (0.63 to 0.69)), intensive care unit admission (0.65 (0.59 to 0.70)), ventilation (0.70 (0.61 to 0.80)), and death (0.51 (0.46 to 0.57)). The Ad26.COV2.S vaccination was associated with better outcomes relative to no vaccination, but higher odds of hospital stay and intensive care unit admission than with two mRNA doses. BNT162b2 was generally associated with worse outcomes than mRNA-1273 (adjusted odds ratios between 0.97 and 1.42).
Conclusions In veterans with recent healthcare use and high occurrence of multimorbidity, vaccination was robustly associated with lower odds of 30 day morbidity and mortality compared with no vaccination among patients infected with covid-19. The vaccination type and number of doses had a significant association with outcomes.
SECOND EXAMPLE Long COVID, or complications arising from COVID-19 weeks after infection, has become a central concern for public health experts. The United States National Institutes of Health founded the RECOVER initiative to better understand long COVID. We used electronic health records available through the National COVID Cohort Collaborative to characterize the association between SARS-CoV-2 vaccination and long COVID diagnosis. Among patients with a COVID-19 infection between August 1, 2021 and January 31, 2022, we defined two cohorts using distinct definitions of long COVID—a clinical diagnosis (n = 47,404) or a previously described computational phenotype (n = 198,514)—to compare unvaccinated individuals to those with a complete vaccine series prior to infection. Evidence of long COVID was monitored through June or July of 2022, depending on patients’ data availability. We found that vaccination was consistently associated with lower odds and rates of long COVID clinical diagnosis and high-confidence computationally derived diagnosis after adjusting for sex, demographics, and medical history.
_______________________________________
There are, of course, many more articles on the subject for anyone keen to see the evidence. Sadly, I have little hope that the COVID loons will be convinced by any of them. Yet, I thought I should give it nevertheless a try.
The well-known Dr. Chris van Tulleken recently joined forces with Professor Michael Heinrich and Dr. Anthony Booker from the University College London School of Pharmacy to test a range of herbal products on sale in the UK. They bought over 70 herbal products from various high street stores and internet retailers. Some of the products were ‘THR’ (traditional herbal registration) herbal medicines, and some were marketed as food supplements. They then analyzed their chemistry to see whether each one really contained what the label says. The three popular herbal remedies we tested were:-
- Milk thistle (Silybum marianum),
- Ginkgo (Ginkgo biloba),
- Evening primrose (Oenothera).
The team at UCL used two different methods of analysis to verify the identity of these herbal products and extracts. High-performance thin-layer chromatography (HPTLC) is a sophisticated technique for the analysis of herbal products and is one of the most commonly used methods in the industry. HPTLC analysis creates a chemical fingerprint of the product which the researchers can then compare to an accepted reference standard for the herb. They look for a broad spectrum of ‘marker compounds’ these are the pharmacologically active and/or chemical constituents within a plant that can be used to verify its potency or identity. For complex samples or where additional confirmation is required, researchers often turn to ¹H nuclear magnetic resonance spectroscopy (¹H-NMR) which allows individual samples to be compared in detail against other samples or to the whole group.
In every THR product tested, the product contained what was claimed on the label. However, the food supplements showed a wide range of quality.
- Of the food supplement products labeled as Ginkgo, 8 out of 30 (27%) contained little or no ginkgo extract.
- 36% of the food supplement milk thistle products contained no detectable milk thistle. Although this is quite a small sample size it is still a startling result. Furthermore, in one case of milk thistle, unidentified adulterants suspected to be synthetic compounds were present in place of milk thistle.
- All of the evening primrose food products we tested did contain what the packet claimed.
The researchers concluded that their investigation shows that a regulatory system for herbal products, like the THR scheme, ensures that people have access to safe herbal medicine products. So, if you are considering buying herbal products then do look out for the THR mark– otherwise, you might not just be wasting your money, you might be consuming other, potentially dangerous, ingredients.
_______________________________
This is an interesting investigation. The researchers should be commended for it! However, I disagree with some of their conclusions. Here is why:
- The investigation merely tested the quality of the products and NOT THEIR SAFETY! To claim that the THR ensures access to safe herbal medicines is incorrect. A product might be of adequate quality but can still be unsafe. The THR only implies safety because the herbal has been used for years without problems being noted. This is not the same as ensuring that it is safe. A direct test of safety is usually not available.
- The recommendation to buy a product with a THR mark is also somewhat misleading. It implies that these products are effective. I fail to see convincing evidence that either MILK THISTLE, GINKGO, or EVENING PRIMROSE are effective for any disease or condition. Thus the responsible recommendation should, in my view, be to NOT buy them regardless of whether they are of good quality or not.
‘Spagyric’ is a so-called alternative medicine (SCAM) based on the alchemy of Paracelsus (1493-1541). Paracelsus borrowed the term from “separate” (spao) and “combine” (ageiro) to indicate that spagyric preparations are based on the “separation”, “extraction” and “recombination” of the active ingredients of a substance. Plant, mineral as well as animal source materials are used.
The production of spagyric remedies is based on a complex process of maceration and fermentation of a plant extract in alcohol. It takes place in dark, thick-walled glass flasks that are hermetically sealed and kept at a controlled temperature of 37 °C for 28 days. The tincture thus obtained is then decanted and the drug residue is removed from the solution, completely dried, and burned to ash to recover the inorganic components of the plant material. The ash is subsequently dissolved in the alcoholic solution of maceration, and the finished spagyric preparation is left for 12 days before use.
Spagyric is not the most popular of all SCAMs but it certainly does have a significant following. One enthusiast claims that “spagyric essences work on a vibrational level in their action upon the emotional/mind and physical spheres and can be employed in numerous situations. Most people seek help to relieve physical symptoms. Even so, it is often necessary to address the emotional and psychological aspects which may predispose the illness or imbalance. In an era where many people are experiencing life-changing events, the ability to transition smoothly is essential for well-being and vitality. Guidance and help are required to maintain homeostasis. These medicines can help the patient to understand the root cause of their illness and learn to regain control of their lives. Some medicine systems appear to be less effective than in previous times. It has been suggested that the energetic frequency of both the earth and human organism are changing. Therefore these systems may no longer be a vibrational match for the changing frequencies. Spagyric Medicine is designed to ‘tune in with’ these current frequencies. Research suggests that the Spagyric essences may instigate improved health by energetically influencing DNA.”
After reading such weird statements, I ask myself, is there any evidence that spagyric remedies work? In my search for robust studies, I was unsuccessful. There does not seem to be a single controlled study on the subject. However, there are fragmentary reports of a study initiated and conducted by a now largely unknown healer named Karl Hann von Weyhern.
Von Weyhern (1882 – 1954) had taken a few semesters of pharmacy and medicine in Freiburg but remained without a degree. In 1930, he became a member of the NSDAP (Hitler’s Nazi party) and in 1940 he joined the SS. Around 1935, he settled in Munich as a non-medical practitioner (Heilpraktiker), and Heinrich Himmler who has a soft spot for SCAM enlisted as one of his patients. By then von Weyhern had by then made a steep career in the Nazi hierarchy, and he managed to convince Himmler that his spagyric remedies could cure tuberculosis, which was still rampant at the time. They decided to carry out experiments in this regard in the Dachau concentration camp.
Thus, von Weyhern was allowed to test spagyric remedies on forcibly recruited concentration camp prisoners. These experiments lasted for about one year and included around 150 patients who, according to von Weyhern’s iridology diagnosis, suffered from tuberculosis. Half of them were treated with spagyric remedies and the others with conventional treatments. At the end of the experiment, 27 persons were reportedly released into everyday concentration camp life as ‘fit for work’. How many of the 150 prisoners lost their lives due to these experiments is not known. Von Weyhern never filed a final report. It is to be feared that the death toll was considerable. [1]
After the war, von Weyhern denied belonging to the SS, claimed that he had ‘sacrificed himself’ for his patients in the concentration camp, merely had to pay a fine, and was ‘denazified’ in 1948. Subsequently, he resumed his work as a ‘Heilpraktiker’ in Olching, a village near Dachau. [1]
Of course, these infamous experiments cannot be blamed on spagyric medicine. Yet, I feel they are nevertheless important, not least because they seem to reveal the only thing remotely resembling something like evidence.
[1] Die Ärzte der Nazi-Führer: Karrieren und Netzwerke : Mathias Schmidt (Hg.), Dominik Groß (Hg.), Jens Westemeier (Hg.): Amazon.de: BooksA ‘manifesto’ is not something that I come across often in my area of research, i.e. so-called alternative medicine (SCAM). This one is in German, I, therefore, translated it for you:
Manifesto for healthy medicine
With the Manifesto for healthy medicine, we, the citizens and patients alliance weil’s hilft! (‘BECAUSE IT HELPS’) demand a fundamental change in our healthcare system, towards a diverse medicine that focuses on people and health. Be part of it! Sign the manifesto and become part of the movement.
It’s of paramount importance, the Manifesto for healthy medicine. About the way we live. It’s about our health. It’s about you and it’s about me.
We want our healthcare system to actually focus on health.
We want a medicine that doesn’t ask what’s missing, but what is possible.
We want a medicine that cares about people, that takes care, gets to the bottom of things, and uses innovative technologies to do so.
We want more bio, so that the chemistry is right, and we want naturopathic procedures and naturally effective medicines to be recognized, promoted, and researched further.
We want research that creates knowledge because, in addition to studies, it also takes into account the experience of physicians and the needs of patients.
We want carers and doctors to be able to work in a way that is good for their patients and for themselves.
We want people from all healthcare professions to work together as equals.
We want a medicine that creates awareness for a good and healthy life because climate protection also begins in one’s own body.
We want an integrative medicine that puts people at the center and self-evidently combines conventional and natural healing methods.
And we want this medicine to be accessible and affordable for everyone.
We fight for a healthy medicine of the future.
Be part of it!
(sorry, if some of it might sound badly translated but the German original is in parts pure gibberish)
_____________________
Who writes such tosh composed of every thinkable platitude and then pompously calls it a MANIFESTO?
BECAUSE IT HELPS! (weil’s hilft!) is a citizens’ movement that demands a change in the health care system – towards the needs and preferences of patients, towards a holistic view of people, and a focus on health instead of disease. The sensible combination of natural medicine and conventional medicine, an integrative medicine, makes an indispensable contribution to this. This is because it relies fully on the patients and involves them as active partners in the treatment. Modern medicine of the future, therefore, needs the equal cooperation of natural medicine and conventional medicine – in the everyday life of physicians and patients, in the reimbursement by the health insurance companies as well as in research and teaching.
On the information platform www.weils-hilft.de weil’s hilft! informs about current developments in integrative medicine, provides background information, and publishes a podcast once a month. The movement is also active on social media at www.facebook.com/weilshilft and www.instagram.com/weilshilft.
weil’s hilft! is supported by the health and patient organizations GESUNDHEIT AKTIV, KNEIPP-BUND, and NATUR UND MEDIZIN. Together, the alliance represents the interests of more than 220,000 people.
_______________________
One could easily disclose the funny side of this, the utter stupidity of the arguments, the platitudes, fallacies, misunderstandings, ignorance, etc. Yes, that would hardly be difficult. But it would ignore how worrying this and similar movements are. They systematically misinform consumers with the sole aim of persuading them that the integration of unproven or disproven treatments into medical routine is in their interest. Yet, if we only scratch the surface of their arguments, we realize that it is exclusively in the interest of those who profit from this type of misinformation.
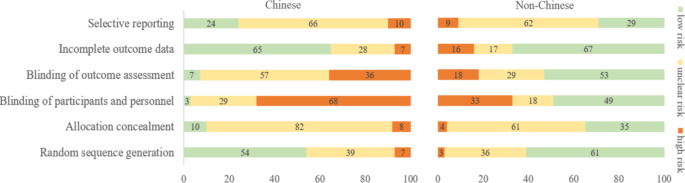
There are debates in acupuncture-related systematic reviews and meta-analyses on whether searching Chinese databases to get more Chinese-language studies may increase the risk of bias and overestimate the effect size, and whether the treatment effects of acupuncture differ between Chinese and non-Chinese populations.
For this meta-epidemiological study, a team of investigators searched the Cochrane Library from its inception until December 2021, and identified systematic reviews and meta-analyses with acupuncture as one of the interventions. Paired reviewers independently screened the reviews and extracted the information. They repeated the meta-analysis of the selected outcomes to separately pool the results of Chinese- and non-Chinese-language acupuncture studies and presented the pooled estimates as odds ratios (OR) with 95% confidence interval (CI). They calculated the Ratio of ORs (ROR) by dividing the OR of the Chinese-language trials by the OR of the non-Chinese-language trials, and the ROR by dividing the OR of trials addressing Chinese population by the OR of trials addressing non-Chinese population. The researchers thus explored whether the impact of a high risk of bias on the effect size differed between studies published in Chinese- and in non-Chinese-language, and whether the treatment effects of acupuncture differed between Chinese and non-Chinese populations.
The researchers identified 84 Cochrane acupuncture reviews involving 33 Cochrane groups, of which 31 reviews (37%) searched Chinese databases. Searching versus not searching Chinese databases significantly increased the contribution of Chinese-language literature both to the total number of included trials (54% vs. 15%) and the sample size (40% vs. 15%). When compared with non-Chinese-language trials, Chinese-language trials were associated with a larger effect size (pooled ROR 0.51, 95% CI 0.29 to 0.91). The researchers also observed a higher risk of bias in Chinese-language trials in blinding of participants and personnel (97% vs. 51%) and blinding of outcome assessment (93% vs. 47%). The higher risk of bias was associated with a larger effect estimate in both Chinese language (allocation concealment: high/unclear risk vs. low risk, ROR 0.43, 95% CI 0.21 to 0.87) and non-Chinese-language studies (blinding of participants and personnel: high/unclear risk vs. low risk, ROR 0.41, 95% CI 0.23 to 0.74). However, the team found no evidence that the higher risk of bias would increase the effect size of acupuncture in Chinese-language studies more often than in non-Chinese-language studies (the confidence intervals of all ROR in the high-risk group included 1, Table 3). The researchers further found acupuncture appeared to be more effective in Chinese than in non-Chinese populations.
The authors concluded that the findings of this study suggest the higher risk of bias may lead to an overestimation of the treatment effects of acupuncture but would not increase the treatment effects in Chinese-language studies more often than in other language studies. The difference in treatment effects of acupuncture was probably associated with differences in population characteristics.
The authors discuss that, although searching Chinese databases can substantially increase the number of eligible studies and sample size in acupuncture reviews, the potentially higher risk of bias is an argument that needs to be considered in the inclusion of Chinese-language studies. Patients, investigators, and guideline panels should be cautious when adopting evidence from acupuncture reviews where studies with a high risk of bias contributed with a high weight to the meta-analysis.
The authors observed larger treatment effects of acupuncture in Chinese-language studies than in studies published in other languages. Although the treatment effects of acupuncture tended to be greater in studies with a high risk of bias, this potential overestimation did not differ between studies published in Chinese and in other languages. In other words, the larger treatment effects in Chinese-language studies cannot be explained by a high risk of bias. Furthermore, our study found acupuncture to be more effective in Chinese populations than in other populations, which could at least partly explain the larger treatment effects observed in Chinese-language studies.
I feel that this analysis obfuscates more than it clarifies. As we have discussed often here, acupuncture studies by Chinese researchers (regardless of what language they are published in) hardly ever report negative results, and their findings are often fabricated. It, therefore, is not surprising that their effect sizes are larger than those of other trials.
The only sensible conclusion from this messy and regrettable situation, in my view, is to be very cautious and exclude them from systematic reviews.