bias
Today, you cannot read a newspaper or listen to the radio without learning that there has been a significant, sensational, momentous, unprecedented, etc. breakthrough in the treatment of Alzheimer’s disease. The reason for all this excitement (or is it hype?) is this study just out in the NEJM:
BACKGROUND
The accumulation of soluble and insoluble aggregated amyloid-beta (Aβ) may initiate or potentiate pathologic processes in Alzheimer’s disease. Lecanemab, a humanized IgG1 monoclonal antibody that binds with high affinity to Aβ soluble protofibrils, is being tested in persons with early Alzheimer’s disease.
METHODS
We conducted an 18-month, multicenter, double-blind, phase 3 trial involving persons 50 to 90 years of age with early Alzheimer’s disease (mild cognitive impairment or mild dementia due to Alzheimer’s disease) with evidence of amyloid on positron-emission tomography (PET) or by cerebrospinal fluid testing. Participants were randomly assigned in a 1:1 ratio to receive intravenous lecanemab (10 mg per kilogram of body weight every 2 weeks) or placebo. The primary end point was the change from baseline at 18 months in the score on the Clinical Dementia Rating–Sum of Boxes (CDR-SB; range, 0 to 18, with higher scores indicating greater impairment). Key secondary end points were the change in amyloid burden on PET, the score on the 14-item cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-cog14; range, 0 to 90; higher scores indicate greater impairment), the Alzheimer’s Disease Composite Score (ADCOMS; range, 0 to 1.97; higher scores indicate greater impairment), and the score on the Alzheimer’s Disease Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS-MCI-ADL; range, 0 to 53; lower scores indicate greater impairment).
RESULTS
A total of 1795 participants were enrolled, with 898 assigned to receive lecanemab and 897 to receive placebo. The mean CDR-SB score at baseline was approximately 3.2 in both groups. The adjusted least-squares mean change from baseline at 18 months was 1.21 with lecanemab and 1.66 with placebo (difference, −0.45; 95% confidence interval [CI], −0.67 to −0.23; P<0.001). In a substudy involving 698 participants, there were greater reductions in brain amyloid burden with lecanemab than with placebo (difference, −59.1 centiloids; 95% CI, −62.6 to −55.6). Other mean differences between the two groups in the change from baseline favoring lecanemab were as follows: for the ADAS-cog14 score, −1.44 (95% CI, −2.27 to −0.61; P<0.001); for the ADCOMS, −0.050 (95% CI, −0.074 to −0.027; P<0.001); and for the ADCS-MCI-ADL score, 2.0 (95% CI, 1.2 to 2.8; P<0.001). Lecanemab resulted in infusion-related reactions in 26.4% of the participants and amyloid-related imaging abnormalities with edema or effusions in 12.6%.
CONCLUSIONS
Lecanemab reduced markers of amyloid in early Alzheimer’s disease and resulted in moderately less decline on measures of cognition and function than placebo at 18 months but was associated with adverse events. Longer trials are warranted to determine the efficacy and safety of lecanemab in early Alzheimer’s disease. (Funded by Eisai and Biogen; Clarity AD ClinicalTrials.gov number, NCT03887455. opens in new tab.)
It’s a good study, and I (like everyone else) hope that it will mean tangible progress in the management of that devastating disease. Most media outlets are announcing the news with the claim that it is the FIRST TIME that any treatment has been shown to delay the cognitive decline of Alzheimer’s disease patients.
But is this true?
I think not!
There have been several studies showing that the herbal remedy GINKGO BILOBA slows the Alzheimer-related decline. Here is the latest systematic review of the subject:
Background: Ginkgo biloba is a natural medicine used for cognitive impairment and Alzheimer’s disease. The objective of this review is to explore the effectiveness and safety of Ginkgo biloba in treating mild cognitive impairment and Alzheimer’s disease.
Methods: Electronic search was conducted from PubMed, Cochrane Library, and four major Chinese databases from their inception up to 1(st) December, 2014 for randomized clinical trials on Ginkgo biloba in treating mild cognitive impairment or Alzheimer’s disease. Meta-analyses were performed by RevMan 5.2 software.
Results: 21 trials with 2608 patients met the inclusion criteria. The general methodological quality of included trials was moderate to poor. Compared with conventional medicine alone, Ginkgo biboba in combination with conventional medicine was superior in improving Mini-Mental State Examination (MMSE) scores at 24 weeks for patients with Alzheimer’s disease (MD 2.39, 95% CI 1.28 to 3.50, P<0.0001) and mild cognitive impairment (MD 1.90, 95% CI 1.41 to 2.39, P<0.00001), and Activity of Daily Living (ADL) scores at 24 weeks for Alzheimer’s disease (MD -3.72, 95% CI -5.68 to -1.76, P=0.0002). When compared with placebo or conventional medicine in individual trials, Ginkgo biboba demonstrated similar but inconsistent findings. Adverse events were mild.
Conclusion: Ginkgo biloba is potentially beneficial for the improvement of cognitive function, activities of daily living, and global clinical assessment in patients with mild cognitive impairment or Alzheimer’s disease. However, due to limited sample size, inconsistent findings and methodological quality of included trials, more research are warranted to confirm the effectiveness and safety of ginkgo biloba in treating mild cognitive impairment and Alzheimer’s disease.
I know, the science is not nearly as good as that of the NEJM trial. I also know that the trial data for ginkgo biloba are not uniformly positive. And I know that, after several studies showed good results, later trials tended not to confirm them.
But this is what very often happens in clinical research: studies are initially promising, only to be disappointing as more studies emerge. I sincerely hope that this will not happen with the new drug ‘Lecanemab’ and that today’s excitement will not turn out to be hype.
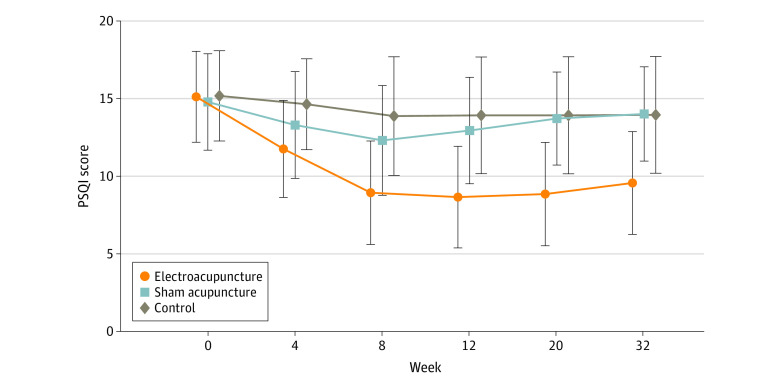
Electroacupuncture (EA) is often advocated for depression and sleep disorders but its efficacy remains uncertain. The aim of this study was, therefore, to “assess the efficacy and safety of EA as an alternative therapy in improving sleep quality and mental state for patients with insomnia and depression.”
A 32-week patient- and assessor-blinded, randomized, sham-controlled clinical trial (8-week intervention plus 24-week follow-up) was conducted from September 1, 2016, to July 30, 2019, at 3 tertiary hospitals in Shanghai, China. Patients were randomized to receive
- EA treatment and standard care,
- sham acupuncture (SA) treatment and standard care,
- standard care only as control.
Patients in the EA or SA groups received a 30-minute treatment 3 times per week (usually every other day except Sunday) for 8 consecutive weeks. All treatments were performed by licensed acupuncturists with at least 5 years of clinical experience. A total of 6 acupuncturists (2 at each center; including X.Y. and S.Z.) performed EA and SA, and they received standardized training on the intervention method before the trial. The regular acupuncture method was applied at the Baihui (GV20), Shenting (GV24), Yintang (GV29), Anmian (EX-HN22), Shenmen (HT7), Neiguan (PC6), and SanYinjiao (SP6) acupuncture points, with 0.25 × 25-mm and 0.30 × 40-mm real needles (Wuxi Jiajian Medical Device Co, Ltd), or 0.30 × 30-mm sham needles (Streitberger sham device [Asia-med GmbH]).
For patients in the EA group, rotating or lifting-thrusting manipulation was applied for deqi sensation after needle insertion. The 2 electrodes of the electrostimulator (CMNS6-1 [Wuxi Jiajian Medical Device Co, Ltd]) were connected to the needles at GV20 and GV29, delivering a continuous wave based on the patient’s tolerance. Patients in the SA group felt a pricking sensation when the blunt needle tip touched the skin, but without needle insertion. All indicators of the nearby electrostimulator were set to 0, with the light switched on. Standard care (also known as treatment as usual or routine care) was used in the control group. Patients receiving standard care were recommended by the researchers to get regular exercise, eat a healthy diet, and manage their stress level during the trial. They were asked to keep the regular administration of antidepressants, sedatives, or hypnotics as well. Psychiatrists in the Shanghai Mental Health Center (including X.L.) guided all patients’ standard care treatment and provided professional advice when a patient’s condition changed.
The primary outcome was change in Pittsburgh Sleep Quality Index (PSQI) from baseline to week 8. Secondary outcomes included PSQI at 12, 20, and 32 weeks of follow-up; sleep parameters recorded in actigraphy; Insomnia Severity Index; 17-item Hamilton Depression Rating Scale score; and Self-rating Anxiety Scale score.
Among the 270 patients (194 women [71.9%] and 76 men [28.1%]; mean [SD] age, 50.3 [14.2] years) included in the intention-to-treat analysis, 247 (91.5%) completed all outcome measurements at week 32, and 23 (8.5%) dropped out of the trial. The mean difference in PSQI from baseline to week 8 within the EA group was -6.2 (95% CI, -6.9 to -5.6). At week 8, the difference in PSQI score was -3.6 (95% CI, -4.4 to -2.8; P < .001) between the EA and SA groups and -5.1 (95% CI, -6.0 to -4.2; P < .001) between the EA and control groups. The efficacy of EA in treating insomnia was sustained during the 24-week postintervention follow-up. Significant improvement in the 17-item Hamilton Depression Rating Scale (-10.7 [95% CI, -11.8 to -9.7]), Insomnia Severity Index (-7.6 [95% CI, -8.5 to -6.7]), and Self-rating Anxiety Scale (-2.9 [95% CI, -4.1 to -1.7]) scores and the total sleep time recorded in the actigraphy (29.1 [95% CI, 21.5-36.7] minutes) was observed in the EA group during the 8-week intervention period (P < .001 for all). No between-group differences were found in the frequency of sleep awakenings. No serious adverse events were reported.
The result of the blinding assessment showed that 56 patients (62.2%) in the SA group guessed wrongly about their group assignment (Bang blinding index, −0.4 [95% CI, −0.6 to −0.3]), whereas 15 (16.7%) in the EA group also guessed wrongly (Bang blinding index, 0.5 [95% CI, 0.4-0.7]). This indicated a relatively higher degree of blinding in the SA group.
The authors concluded that, in this randomized clinical trial of EA treatment for insomnia in patients with depression, quality of sleep improved significantly in the EA group compared with the SA or control group at week 8 and was sustained at week 32.
This trial seems rigorous, it has a sizable sample size, uses a credible placebo procedure, and is reported in sufficient detail. Why then am I skeptical?
- Perhaps because we have often discussed how untrustworthy acupuncture studies from China are?
- Perhaps because I fail to see a plausible mechanism of action?
- Perhaps because the acupuncturists could not be blinded and thus might have influenced the outcome?
- Perhaps because the effects of sham acupuncture seem unreasonably small?
- Perhaps because I cannot be sure whether the acupuncture or the electrical current is supposed to have caused the effects?
- Perhaps because the authors of the study are from institutions such as the Shanghai Municipal Hospital of Traditional Chinese Medicine, the Department of Acupuncture and Moxibustion, Huadong Hospital, Fudan University, Shanghai,
- Perhaps because the results seem too good to be true?
If you have other and better reasons, I’d be most interested to hear them.
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
The AMA has recently published a short article that – even though not addressing so-called alternative medicine (SCAM) directly – has considerable relevance for the field:
It’s increasingly common for patients to encounter nonphysician practitioners as members of their health care teams. Meanwhile, ever more nonphysician practitioners have received advanced training resulting in a doctorate degree, such as the doctor of nursing practice.
To help patients keep pace with these changes, physicians should make new strides to clarify their roles and credentials vis-a-vis other members of the health care team and also promote collaboration among all health professionals, according to an AMA Council on Ethical and Judicial Affairs report that was adopted at the 2022 AMA Interim Meeting.
The core issue is that “the skill sets and experience of nonphysician practitioners are not the same as those of physicians.” Thus, when nonphysician practitioners identify themselves as “doctors”—consistent with the doctoral-level degrees they earned—“it may create confusion and be misleading to patients and other practitioners,” says the report.
In fact, surveys (PDF) performed as part of the AMA Truth in Advertising Campaign have found that while patients strongly support physician-led health care teams, many are confused about the level of education and training of health professionals—and the confusion isn’t limited to nonphysician practitioners who hold doctorates. For example, roughly one-fifth of respondents think psychiatrists are not physicians, while a similar number think nurse practitioners are physicians.
The AMA Code of Medical Ethics touches on this issue in an opinion on collaborative care, which provides guidance on the roles of physicians in team-based settings where a mix of health professionals provide care.
In SCAM, we have the problem that practitioners often call themselves doctors or physicians without having a medical degree. This confuses patients who might consult and trust these practitioners assuming they have studied medicine. We recently discussed the case of a naturopath who called himself a doctor and failed to diagnose a rectal tumor of his patient. Much more dramatic was the case of a UK-based chiropractor who called herself a doctor, thus attracting a patient suffering from complex health issues contraindicating spinal manipulations. She nonetheless manipulated his neck and promptly killed him.
I know that patients are being misled every day by SCAM practitioners (ab)using the ‘Dr.’ title. Therefore, the AMA reminder is an important, timely, and necessary lesson for SCAM. I feel that the professional organizations of SCAM providers should issue similar reminders to their members and make sure they behave appropriately.
Acupuncture is emerging as a potential therapy for relieving pain, but the effectiveness of acupuncture for relieving low back and/or pelvic pain (LBPP) during pregnancy remains controversial. This meta-analysis aimed to investigate the effects of acupuncture on pain, functional status, and quality of life for women with LBPP pain during pregnancy.
The authors included all RCTs evaluating the effects of acupuncture on LBPP during pregnancy. Data extraction and study quality assessments were independently performed by three reviewers. The mean differences (MDs) with 95% CIs for pooled data were calculated. The primary outcomes were pain, functional status, and quality of life. The secondary outcomes were overall effects (a questionnaire at a post-treatment visit within a week after the last treatment to determine the number of people who received good or excellent help), analgesic consumption, Apgar scores >7 at 5 min, adverse events, gestational age at birth, induction of labor and mode of birth.
Ten studies, reporting on a total of 1040 women, were included. Overall, acupuncture
- relieved pain during pregnancy (MD=1.70, 95% CI: (0.95 to 2.45), p<0.00001, I2=90%),
- improved functional status (MD=12.44, 95% CI: (3.32 to 21.55), p=0.007, I2=94%),
- improved quality of life (MD=−8.89, 95% CI: (−11.90 to –5.88), p<0.00001, I2 = 57%).
There was a significant difference in overall effects (OR=0.13, 95% CI: (0.07 to 0.23), p<0.00001, I2 = 7%). However, there was no significant difference in analgesic consumption during the study period (OR=2.49, 95% CI: (0.08 to 80.25), p=0.61, I2=61%) and Apgar scores of newborns (OR=1.02, 95% CI: (0.37 to 2.83), p=0.97, I2 = 0%). Preterm birth from acupuncture during the study period was reported in two studies. Although preterm contractions were reported in two studies, all infants were in good health at birth. In terms of gestational age at birth, induction of labor, and mode of birth, only one study reported the gestational age at birth (mean gestation 40 weeks).
The authors concluded that acupuncture significantly improved pain, functional status and quality of life in women with LBPP during the pregnancy. Additionally, acupuncture had no observable severe adverse influences on the newborns. More large-scale and well-designed RCTs are still needed to further confirm these results.
What should we make of this paper? 
In case you are in a hurry: NOT A LOT!
In case you need more, here are a few points:
- many trials were of poor quality;
- there was evidence of publication bias;
- there was considerable heterogeneity within the studies.
The most important issue is one studiously avoided in the paper: the treatment of the control groups. One has to dig deep into this paper to find that the control groups could be treated with “other treatments, no intervention, and placebo acupuncture”. Trials comparing acupuncture combined plus other treatments with other treatments were also considered to be eligible. In other words, the analyses included studies that compared acupuncture to no treatment at all as well as studies that followed the infamous ‘A+Bversus B’ design. Seven studies used no intervention or standard of care in the control group thus not controlling for placebo effects.
Nobody can thus be in the slightest surprised that the overall result of the meta-analysis was positive – false positive, that is! And the worst is that this glaring limitation was not discussed as a feature that prevents firm conclusions.
Dishonest researchers?
Biased reviewers?
Incompetent editors?
Truly unbelievable!!!
In consideration of these points, let me rephrase the conclusions:
The well-documented placebo (and other non-specific) effects of aacupuncture improved pain, functional status and quality of life in women with LBPP during the pregnancy. Unsurprisingly, acupuncture had no observable severe adverse influences on the newborns. More large-scale and well-designed RCTs are not needed to further confirm these results.
PS
I find it exasperating to see that more and more (formerly) reputable journals are misleading us with such rubbish!!!
It has been reported that a Vancouver naturopath has been fined and temporarily suspended after a patient complained he failed to notice a rectal tumor during four months of treatment for hemorrhoids.
Jordan Atkinson will have to pay $5,000 and lose his license for 16 days after signing a consent agreement with the College of Naturopathic Physicians of B.C., according to a public notice posted by the COLLEGE OF NATUROPATHIC PHYSICIANS OF BRITISH COLUMBIA.
A former patient had filed the complaint when another medical professional diagnosed a tumor on the rectum following “several appointments” with Atkinson for hemorrhoid treatment. “The patient complained that Dr. Atkinson failed to detect the tumor because he did not perform a competent examination,” the college notice says. ‘Doctor’ Atkinson disagreed with that allegation but admitted that he didn’t fully document his appointments with the patient.
The college’s inquiry committee, which investigates complaints, found that “Dr. Atkinson’s treatment of the patient fell short of the standard of practice required of a naturopathic doctor in these circumstances.” Atkinson who is also the subject of a lawsuit from a patient who alleges he seriously injured her while injecting Botox into her face at the base of her nose, has also agreed to a reprimand and “to make reasonable efforts when a language barrier exists to ensure that his patients understand the treatment plan and provide informed consent.” 
Personally, I find it hard to believe that any health professional can administer a prolonged treatment for hemorrhoids, while the patient is actually suffering from a rectal tumor which might well be malign. I find it even harder to believe that, after a complaint had been filed by a victim, the professional body of this professional suspends his license for just 16 days.
In my view, this suggests that this professional body (like so many in the realm of so-called alternative medicine (SCAM)) is not fit for purpose. That is to say, it does clearly not fulfill its main task adequately which is to protect the public from the malpractice of its members. Rather it seems to prioritize the interests of the member over those of the public. Yet, on its website the COLLEGE OF NATUROPATHIC PHYSICIANS OF BRITISH COLUMBIA state that “the College protects the public interest by ensuring that naturopathic physicians in British Columbia practice safely, ethically, and competently.” As so often in SCAM, what is being stated and what is being done differs dramatically.
At the heart of this and many similar cases, I fear, is that consumers find it difficult to differentiate between well-educated healthcare professionals and poorly trained charlatans. And who could blame them? Calling naturopaths ‘doctors’ cannot be helpful, particularly if the ‘Dr.-title’ is used without a clear qualification that the person who carries it has never seen the inside of a medical school; instead he has learned an abundance of nonsense taught by a quack institution.
In summary one is tempted to conclude that this case yet again confirms that naturopaths are medically incompetent graduates of schools of incompetence protected by organizations of incompetence.
Recently, I received an email with this ‘special offer’ for purchasing a book and was impressed – but not in a positive sense:
Dr Farokh’s commendable work at upto 22% off – Healing Cancer. For Limited time period only.
Healing Cancer: A Homoeopathic Approach
As a homeopath one should not deter oneself in dealing with any type of cases, be it cancer. But for executing that an ultimate guidance is needed. Cancer is so much prevalent and challenging medical problem of today that a trustworthy source of accurate information becomes pertinent and this work of Dr. Farokh Master immediately propels at the top of quality books for cancer. Based on Master’s 40 years of experience this book was written for students to understand the basis of oncology and for practitioners for brushing-up of their knowledge in this growing discipline. Author says that to get a grasp on cancer cases we should believe in the potential of the homeopathic treatment, that healing from cancer refers to internal process of becoming whole and feeling harmonious with yourself and your environment.To even start with handling the cases of cancer one should be aware of understanding of cancer, its cause, pathophysiology, different types, conventional treatment and their side effects, integrative medicines, social problems in the treatment, such topics are well casted by Volume 1 of the book.
Peak points of Volume 1- • A full chapter is dealing with Iscador, a relatively old method, very effective but unfortunately underemployed.• Published papers about Homeopathy in the treatment of cancer are presented before the last chapter which is on some of most used allopathic drugs in cancer with a focus on their side-effects. After the coverage of basic information on oncology in Volume 1 comes the Volume 2 which explores topics like understanding cancer from homoeopathic point of view, constitutional remedies, therapeutics of individual cancers, nutrition, general management.
Peak points of Volume 2-• A whole chapter on Cadmium salts and cancer.• 51 “lesser known remedies” are briefly quoted and their usefulness in different situations and types of cancer exposed.• A long chapter deals with the “Indian drugs”, it is important that these remedies are used mostly in tincture or low potencies, as herbal or Ayurvedic remedies or food supplements relieving the patients. • The choice and differentiation between the remedies is then helped by the “Repertory of Cancer”, very well compiled and a highly useful section. “Clinical tips from my practice” given as a sub-chapter. • It ends with recommendations on how to deal with radiation illness and the side-effects of conventional treatment, as well as the treatment of pain and help with palliative care.
For fighting and curing cancer and improving the quality and quantity of life of people, knowledge of Homeopathy, both philosophically and scientifically is needed which this work of art portrays delightfully.
About Book Author:
Dr. Farokh J. Master’s birth into homeopathy was in the year 1976, when he joined Bombay homeopathic medical college, after giving up his studies at the orthodox school of medicine. Dr Master was instrumental in starting homeopathic out-patient dept in many allopathic hospitals viz. Bombay Hospital, KEM Hospital & Ruby Hall, Pune. Besides his work as a senior Homeopath of the HHC, Dr. Farokh Master is teaching homeopathy (advanced level) at the Mumbai Homeopathic Medical College, part of Mumbai university. He is also teaching at other homeopathic colleges in India and abroad. He has given seminars in various countries like Austria, Australia, India, Japan etc. Dr Master has written more than 50 books like -The Homeopathic Dream Dictionary, Cross References of the Mind, Perceiving Rubrics of the Mind, The State of Mind affecting the Foetus, Tumors and Homeopathy, The Bedside Organon of Medicine, The proving of Mocassin Snake, Bungarus, etc. Dr. Master is the originator of many recent new approaches and insights in homoeopathy.
Some people claim that homeopaths are not dangerous and argue that their placebos cannot harm patients. I have long disagreed with this position. As homeopathy is not an effective therapy (it has no effects beyond placebo), its use simply means allowing diseases to remain untreated.
- If we are dealing with a common cold, this might be little more than a costly nuisance.
- If we are dealing with a chronic condition such as arthritis, it means causing unnecessary suffering.
- If we are dealing with life-threatening diseases like cancer, it means shortening the life of patients.
This is the politest way I can put it. There are of course other, less polite terms for ‘shortening a life’! Most of us shy away from using them in the context of homeopathy. In the case of the author of this book, we might make an exception. In my view, he is someone who is deluded to the point where he is ready to kill his patients with homeopathy.
PS
Iscador is not even a homeopathic remedy.
Prof. Harald Walach and his work have been regular topics on this blog (e.g. here, here, and here). Walach has served as the editor of Forschende Komplementärmedizin / Research in Complementary Medicine for 20 years and is now retiring from this post. On this occasion, he just published an EDITORIAL looking both back and ahead on research into so-called alternative medicine (SCAM). Here are the last paragraphs of his piece:
What lies in store? We do not know. “Hidden is the future before me, I am wondering what my destiny will bring,” sings Lensky in Tschaikowsky’s opera Eugen Onegin, and this is a good description of our current situation, not only in medicine, but also politically. If I have one wish for the future of CAM, for the future of our journal, then it is to keep the fire ablaze and uphold the hope of change that has been at the source of its founding and is still empowering many in the field. The field of medicine, but also the world, needs examples of visions and visionaries. The landscape will change. While the beginning of the field and the journal was a decidedly German-speaking, central European enterprise, we have now seen the extension of the field.
China has entered the scene with enormous manpower, a venerable tradition, and a huge amount of experience, research, and funding. Other countries, Iran for instance, are discovering the sources of traditional medical approaches. It might well be the case that those who forget that the world does not end at the rim of the Mediterranean and of the Atlantic will be left behind. It has always been a decisive element of CAM research that it bridged countries, nations, polities, and worldviews. The ISCMR, Consortium, and European Congress for Integrative Medicine (ECIM) conferences probably had as attendees more researchers from outside Europe and the US than from their host countries. Africa is only slowly beginning to enter the scene. The future will be less Euro- and Western-centric than the beginning of CAM, I am quite sure. The Western model of healthcare and economic growth through single pharmacological inventions is not sustainable worldwide and in the long run, apart from the fact that it is conceptually ill-founded. Thus, our hope very likely lies in broadening our view: thinking about other systems of medicine, other approaches, whole-systems thinking. This is actually very similar to our beginning. Every end is a beginning, every beginning is an end, Oscar Wilde used to say.
Apart from the abundant use of platitudes, there are several statements that might deserve a comment:
- The beginning of the field and the journal was a decidedly German-speaking, central European enterprise. Yes, the journal started as a predominantly German publication, yet the field was never mostly German/ central European. SCAM always included many modalities that originated from China, the US, and other non-European countries. Neither was the research into these areas ever dominated by German-speaking investigators.
- China has entered the scene with enormous manpower, a venerable tradition, and a huge amount of experience, research, and funding. This is true – but is it a good development? On this blog, I have often written about the fact that research from China is notoriously unreliable or even fabricated. As the quantity of such work is about to totally overwhelm SCAM research, this is a most concerning development, in my view.
- It has always been a decisive element of CAM research that it bridged countries, nations, polities, and worldviews. I would say that this is not something that characterizes SCAM research. It is a hallmark of any research. And considering my last point, it might soon no longer apply to SCAM. As we are being flooded with unreliable Chinese SCAM research, Chinese dominance might soon stifle criticism of SCAM.
- The Western model of healthcare and economic growth? As far as I can see, the model of economic growth is fast being adopted by non-Western counties.
So, what is the future of SCAM and SCAM research? Like Walach, I don’t know. But contrary to Walach, I hope for something entirely different. I hope that the stupidly short-sighted notion of two types of research and two types of healthcare can eventually be abandoned. In the end, there can only be one type of science – the one that understands itself as critically testing hypotheses by trying to prove them wrong – and only one type of medicine – the one that does more good than harm.
It has been reported that America’s Frontline Doctors (a right-wing organization that is associated with the ‘Tea Party’) is suing one of its founders in a battle for control over the controversial group, which gained national notoriety for spreading misinformation about COVID-19 treatments and vaccines during the pandemic.
The organization and its current board chairman have sued Simone Gold, MD, alleging that she misused the nonprofit organization’s funds to buy a $3.6 million Florida mansion, purchase a Mercedes-Benz and other luxury vehicles, and take trips on private planes.
The lawsuit, filed November 4 in federal court, comes just months after Gold was released from prison for her role in the January 6 US Capitol insurrection. Gold pleaded guilty to trespassing in the Capitol and was sentenced to 60 days in federal prison.
The group and the board chairman, Joseph Gilbert, claim that after her release from prison, Gold attempted to reassert control of the group, take over its website, and fraudulently represent herself as its director, according to the complaint. The complaint referred to Gold as a “rogue founder,” alleging that she spent almost $50,000 monthly on personal expenses using the organization’s credit cards.
Gold resigned from the group’s board in February ― before she pled guilty ― so that she could pursue her goal of opening health and wellness centers nationwide, according to the complaint. At that time, the board voted Gilbert to be its chairman and agreed to have Gilbert negotiate an agreement for Gold to serve as a consultant. Gold sought a “signing bonus” of $1.5 million, along with $50,000 to be paid monthly as a consulting fee, according to the complaint.
Another report has more details on Gold’s alleged wrong-doing: The complaint claims that in November 2021, Gold used “AFLDS charitable funds to purchase a $3.6 million home in Naples, Florida for her personal rent-free use, and at least three vehicles and has otherwise used AFLDS funds to resource her personal lifestyle and expenses since she formed AFLDS.” Plaintiffs also allege that Gold “currently lives in this home with John Strand, rent free.” Strand is a former underwear model and boyfriend of Gold’s who was arrested with her in connection with the January 6, 2021 insurrection in the U.S. Capitol. She moved with Strand to Florida this year from Los Angeles, where she had been an emergency room physician. Strand allegedly was paid $10,000 per month as an AFLDS employee and allegedly spent $15,000 to $17,000 a month using those credit cards. He was terminated from AFLDS in summer 2022, according to the complaint. In addition to purchasing the house with AFLDS funds, the complaint said Gold purchased a Mercedes Benz Sprinter van, a Hyundai Genesis, and a GMC Denali. After taking possession of the Naples home, she used AFLDS funds to pay a personal security officer $12,000, a personal housekeeper $5,600 a month, and charged “nearly $50,000 per month” to AFLDS credit cards.
I tried to find some information on th health and wellness centers that Simone Gold wanted or did open. Alas I was unsuccessful in my endeavor. However, I found an interesting passage she once wrote:
The World Health Organization, the FDA, the NIH, and the CDC are proven liars who have lost all credibility and common-sense, while jeopardizing YOUR health and safety. What disgusts me most is how their failed prescriptions have exposed the most vulnerable: our elderly and our children. The New York Times, CNN, NPR, and hundreds of other news outlets have censored the truth in order to preserve their power. Twitter, Facebook, Google/YouTube, Apple, and dozens of other Tech companies are throttling down content, suppressing information, and de-platforming those with whom they disagree.
I find it hard to find words for a comment – except perhaps this: maybe it is not such a bad thing when anti-vaxxers fight each other; it means they have less time, energy, and money to confuse the public with their lies.
A review conducted in 2015 reported community pharmacists are willing to adopt a professional role in counselling consumers about the appropriate and safe use of so-called alternative medicine (SCAM) but faced multiple barriers in doing so. This current review aimed to update and extend these findings, by identifying studies published since 2015 that reported on pharmacists across any setting.
Eligible studies published between January 01, 2016, and December 31, 2021, were identified across 6 databases (PubMed, Scopus, Web of Science, EMBASE, ScienceDirect and MEDLINE). A grounded theory approach was used to thematically synthesize the data extracted.
A total of 64studies representing pharmacists across 30 countries were included for review. The study designs varied and included:
- cross-sectional surveys (n = 36),
- qualitative studies (n = 14),
- pseudo-patient studies (n = 3).
Eight studies reported on practice and/or bioethical responsibilities and 19 studies documented factors that would enable pharmacists to fulfill these responsibilities, while 37 studies reported on both.
The authors concluded that these findings indicate research about pharmacists’ responsibilities associated with SCAM is evolving from gap analysis towards research that is proactive in advocating for change in multiple areas. These findings can be used to inform a consensus discussion among pharmacists and key stakeholders regarding a set of professional responsibilities that would serve in the development of: a clearly defined role and associated practice standards, and competency requirements that inform educational learning objectives for inclusion in undergraduate, post-graduate and continuing professional pharmacy education.
I am puzzled why so many researchers in this specific area seem to avoid clearer language plainly stating the essential, simple, and undeniable facts. I am equally puzzled why so few pharmacists speak out.
It is obvious that community pharmacists are firstly healthcare professionals and only secondly shopkeepers. As such, they have important professional and ethical duties. Foremost, they are obliged to inform their customers responsibly – and responsible means telling them about the evidence for or against the SCAM product they are about to purchase. This duty also entails that pharmacists must inform themselves about the best current evidence. In turn, this means they must stop tolerating the current plethora of under- or post-graduate SCAM courses that are not evidence-based.
As we have discussed ad nauseam on this blog, none of this is actually happening (except in very few laudable cases)!
By and large, pharmacists continue to go along with the double standards of a) evidence for conventional drugs and b) fairy tales for SCAM. In the interest of progress, patient safety, and public health, it is time that pharmacists wake up and remind themselves that they are not commercially orientated shopkeepers but ethical healthcare professionals.