Spinal manipulation has been associated with a wide range of serious complications. Usually, they occur after neck manipulations. Neurologists from Morocco just published a case-report of a patient suffering a subdural haematoma after lumbar spinal manipulation.
A previously healthy 23 years-old man was receiving spinal manipulation for chronic back pain by a physiotherapist when he experienced a knife-like low back pain and lower limbs radiculalgia. The manipulation consisted on high velocity pression in the lumbar region while the patient was in prone position. He woke up the next morning with a weakness of both lower limbs and sensation of bladder fullness.
On presentation to the emergency department, 24 hours after the manipulation, the neurological examination found a cauda equina syndrome with motor strength between 2/5 and 3/5 in the left lower limb, 4/5 in the right lower limb, an abolition of the patellar and Achilles reflexes, a saddle hypoesthesia and a tender bladder. The general examination was normal. Magnetic resonance imaging (MRI) of the lumbar spine was performed promptly and showed intradural collection extending from L2 to L3 level with signal intensity consistent with blood. There were no adjacent fractures, disc or ligament injuries. Routine blood investigations were normal.
The patient underwent an emergency operation via L2-L3 laminectomy. The epidural space had no obvious abnormalities but the dura mater was tense and bluish. After opening the dura, a compressive blood clot was removed completely. The origin of the bleeding could not be determined. At the end of the intervention, nerve roots appeared free with normal courses. Subsequently, the patient’s the motor function of lower limbs gradually returned. He was discharged without neurological deficits 6 days postoperatively. At 6-months’ follow-up, the neurological examination was totally normal.
___________________________________________________________
Subdural haematoma is a rare occurrence. As a complication after spinal manipulation, it seems to be ever rarer. Our case-series of serious adverse effects after chiropractic manipulation did include such a case, albeit not at the lumbar level (as far as I remember):
To obtain preliminary data on neurological complications of spinal manipulation in the UK all members of the Association of British Neurologists were asked to report cases referred to them of neurological complications occurring within 24 hours of cervical spine manipulation over a 12-month period. The response rate was 74%. 24 respondents reported at least one case each, contributing to a total of about 35 cases. These included 7 cases of stroke in brainstem territory (4 with confirmation of vertebral artery dissection), 2 cases of stroke in carotid territory and 1 case of acute subdural haematoma. There were 3 cases of myelopathy and 3 of cervical radiculopathy. Concern about neurological complications following cervical spine manipulation appears to be justified. A large long-term prospective study is required to determine the scale of the hazard.
The big problem with adverse events of this nature is that their true incidence is essentially unknown. The two cases of subdural haematoma mentioned above seem to be the only two reported in the medical literature. But, as there is no monitoring system, the true figure is anybody’s guess.
A pro-homeopathy site (to be taken with a pinch of salt) claims that today 300 homeopathic MDs belong to the “Unio Homoeopathica Belgica” and 4,000 MDs (about 10% of all doctors) are prescribing homeopathics at least occasionally.
One-fourth of the Belgian population uses homeopathy. As of 1998, only MDs can legally practice homeopathy. But now it seems that the free ride for Belgian homeopathy is coming to an end. Belgium has joined the long list of countries (e.g. UK, US, Spain, France, Sweden, Russia) where the usefulness of homeopathy is being questioned.
‘Test Achats’ is a Belgian not-for-profit organization which promotes consumer protection. It was founded in 1957 and publishes research in a subscription magazine. It has been reported that this organiation has issued a crushing report on homoeopathy, describing it as “unacceptable” that homeopathic remedies are allowed to be described by practitioners as medication.
Il est inacceptable que des médicaments homéopathiques et des médicaments traditionnels à base de plantes puissent être vendus en tant que “médicament” en pharmacie sans que leur efficacité n’ait été démontrée. Il en va de même pour un certain nombre de médicaments classiques et de médicaments ordinaires à base de plantes, pour lesquels nous avons également de gros doutes quant à leur efficacité et/ou leur sécurité. Le statut de “médicament” leur confère une aura de crédibilité qu’ils ne méritent absolument pas. Notre banque de données de médicaments met un terme à cette tromperie et distingue les médicaments utiles de ceux qui ne le sont pas…
Pour les 55 médicaments homéopathiques avec indication, ces pourcentages sont … 84 % à “utilité contestable” et 16 % “à déconseiller”.
‘Test-Achats’ describes homoeopathy as “quack medicine,” and states that “there are conditions where the patient really has no time to lose on products whose effectiveness has not been demonstrated. People who are suffering from very real heart and vascular conditions should immediately seek treatment by a doctor, and with truly effective medication.”
In the bizarre world of chiropractic, the war between vitalistic subluxationists and reformers has reached a new climax. The World Federation of Chiropractic (WFC) has just announced that its president, Laurie Tassell, has resigned. The move follows what the International Chiropractor’s Association (ICA) called a “blatant offensive behaviour on a public stage” that “speaks for itself” and “cannot be excused under any circumstances.” The ICA’s alleged an embarrassing display of unprofessional and disruptive behaviour of presenters and attendees at the WFC Conference in Berlin in March 2019. It involved attacks on subluxationist chiropractors and included the throwing of water bottles onto the stage and clapping and cheering as the management of subluxation was denigrated.
The ICA President, Stephen Welsh, subsequently demanded that:
- The current Chair of the WFC Research Council be immediately removed from his current position and denied future participation in any activities on behalf of the WFC.
- An additional member of the WFC Research Council be publicly reprimanded and sanctioned and prohibited from the opportunity to serve in any leadership role at the WFC for at least 5 years.
- The sponsoring organization that coordinated, reviewed and permitted the alleged questionable presentations be sanctioned for conduct not reflecting the professional, inclusive and collegial respect for the values embedded in the WFC Strategic Plan, Governing Documents and the WFC Official Policy Statements.
According to Welsh, and others who attended, the Chair of the WFC Research Council, Greg Kawchuk DC, Ph.D, compared bringing a child to a vitalistic chiropractor to bringing them to a Catholic priest at a children’s school.
The WFC has now announced the appointment of Vivian Kil DC as Interim President to take over from Tassel. Kil is a graduate of the AECC, full-time clinician and the owner of a multidisciplinary clinic in the Netherlands. Kil is an advocate for chiropractors as practitioners of so called “primary spine care”. She stated her vision as follows:
- That we will (the chiropractic profession) set aside our differences within the profession, unite as a profession, and agree that becoming the source of nonsurgical, nonpharmacological, primary, spine care expertise and management should be a primary common goal.
- That for us to do the necessary work to fulfill this role and do it with the entire profession, every chiropractor will be involved and not just a small active group of leaders.
- And finally, that we will become the source of nonsurgical, nonpharmacological, primary, spine care expertise and management worldwide.
In my view, the problem of the chiropractic profession is unsolvable. Giving up Palmer’s obsolete nonsense of vitalism, innate intelligence, subluxation etc. is an essential precondition for joining the 21st century. Yet, doing so would abandon any identity chiropractors will ever have and render them physiotherapists in all but name. Neither solution bodes well for the future of the profession.
Glucosamine supplements are often advocated for the treatment of osteoarthritis. But there is evidence that they might convey other benefits as well. This prospective observational study assessed the association of habitual glucosamine use with risk of cardiovascular disease (CVD) events. The UK Biobank data of 466 039 participants without CVD at baseline was used. They completed a questionnaire on supplement use, which included glucosamine. These participants were enrolled from 2006 to 2010 and were followed up to 2016. The main outcome measures were incident CVD events, including CVD death, coronary heart disease, and stroke.
During a median follow-up of seven years, there were 10 204 incident CVD events, 3060 CVD deaths, 5745 coronary heart disease events, and 3263 stroke events. After adjustment for age, sex, body mass index, race, lifestyle factors, dietary intakes, drug use, and other supplement use, glucosamine use was associated with a significantly lower risk of total CVD events (hazard ratio 0.85, 95% confidence interval 0.80 to 0.90), CVD death (0.78, 0.70 to 0.87), coronary heart disease (0.82, 0.76 to 0.88), and stroke (0.91, 0.83 to 1.00).
The authors concluded that habitual use of glucosamine supplement to relieve osteoarthritis pain might also be related to lower risks of CVD events.
This is an impressive study! It incorporates both a huge sample size and a long observation period. Moreover, the authors analysed the data expertly and interpreted their results with the necessary caution.
The association between glucosamine intake and CVD risk were independent of CVD risk factors, such as gender, age, income, body mass index, physical activity, healthy diet, alcohol intake, smoking status, diabetes, hypertension, high cholesterol, arthritis, drug use, and other supplement use. Moreover, the findings are in line with several previous studies that show inverse associations of glucosamine use with CVD risk and mortality. And finally, the authors discuss several biologically plausible mechanisms that could explain the observed findings.
Yet, it is conceivable that the association is not of a causal nature. There might be a host of confounders responsible for the finding. Therefore, before we now all rush to the next health-food store to buy glucosamine supplements – they are not all that cheap! – we should perhaps wait for further independent replications and research.
Homeopathy has had a long and profitable ride in France; nowhere else in Europe is it more popular, nowhere in Europe are the profit margins higher, and nowhere have I seen pharmacists pushing so hard to earn a few extra Euros on useless homeopathic remedies.
But, since a few months, sceptics have started to raise their voices and object to homeopathic reimbursement (currently at the rate of 30%) and to homeopathy in general.
- A group of doctors protested against homeopathy by publishing an open letter in ‘Le Figaro’.
- The French Academies of Medicine and Pharmacy published a report confirming the lack of evidence for homeopathy.
- The medical school in Lille suspended its degree in homeopathy.
The French health secretary, the oncologist Dr Agnès Buzyn, reacted wisely, in my view. She initially stated that the effect of homeopathy is ‘probably a placebo effect‘. Subsequently, she asked the regulator, La Haute Autorite de Sante (HAS), to look into the matter and prepare a full analysis of the evidence. This report has now been published.
An article in ‘FRANCE INFO’ reports that HAS found no good evidence in support of the ~ 1 200 homeopathic remedies currently on the French market. The document is currently being considered by Dr Buzyn who will announce her decision about reimbursement in June. It is considered to be highly likely that she will stop reimbursement.
If so, consumers will soon have to pay in full for homeopathic preparations out of their own pocket. In addition, they would have to pay the VAT, and it is foreseeable that this change would signal the end of the French consumers’ love affair with homeopathy. This development is bound to seriously hurt Boiron, the world’s largest producer of homeopathics. The firm has already announced that they suspended its trading on the stock market and is now arguing that the move would endanger its sizable workforce.
The question I now ask myself is whether Boiron is powerful enough to do something about all this. Personally, I have been impressed by the rational approach of Dr Buzyn. She will no doubt see through Boiron’s bogus argument of saving a form of obsolete quackery in the name of employment. Therefore, I expect that the days of homeopathy’s reimbursement in France are counted.
(For those who can read French, I add the original ‘ FRANCE INFO’ article below.)
_________________________________________________________________
Les granules homéopathiques offrent “un service médical rendu insuffisant” selon la HAS.
Avis définitif en juin
Cet avis avait été réclamé par la ministre de la Santé il y a plusieurs mois face à la montée de la polémique entre médecins pro et anti-homéopathie. 124 médecins avaient relancé le débat l’an dernier en qualifiant les homéopathes de “charlatans”.
Désormais, lors d’une phase contradictoire, les laboratoires vont pouvoir répondre à la HAS, qui rendra son avis définitif en juin. La ministre de la Santé, Agnès Buzyn, avait par le passé annoncé qu’elle se rangerait à cet avis.
1 000 emplois menacés, selon Boiron
Les pro-homéopathie eux, s’insurgent. Selon eux, les granules ne coûtent que 130 millions d’euros par an à la Sécurité sociale, contre 20 milliards pour les médicaments classiques. Et il existe d’après eux, au minimum, un effet placebo. Pour les laboratoires Boiron, leader mondial du secteur, si l’homéopathie n’est plus remboursée, ce sont 1 000 emplois qui sont directement menacés.
Par ailleurs, dans un communiqué commun, trois laboratoires (Boiron, Lehning et Weleda) s’émeuvent de découvrir à travers un média la teneur d’un avis d’une agence indépendante qui devait être tenu confidentiel. Les laboratoires Boiron précisent à franceinfo qu’ils n’ont pas encore reçu le projet d’avis de la Haute autorité de santé. Boiron, entreprise française cotée, annonce “suspendre” son cours de bourse.
The debate what might be the optimal treatment of back pain has been going on for many years. This new study provides important further insights.
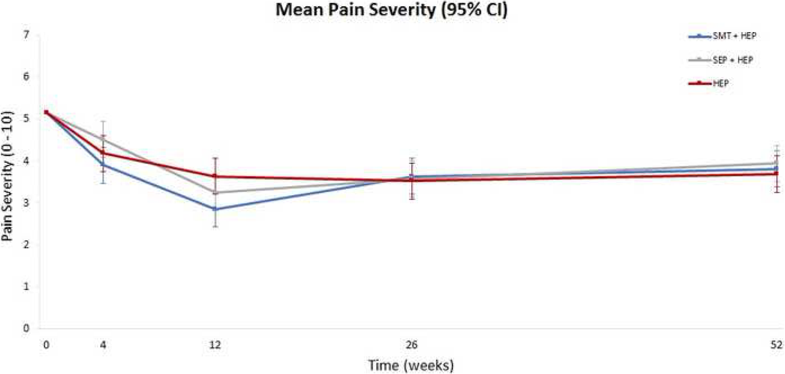
The RCT assessed the comparative effectiveness of adding spinal manipulative therapy (SMT) or supervised rehabilitative exercise to home exercise in adults 65 or older suffering from sub-acute or chronic low back pain (LBP). Treatments were provided over 12-weeks and self-report outcomes were collected at 4, 12, 26, and 52 weeks. The primary outcome was pain severity. Secondary outcomes included back disability, health status, medication use, satisfaction with care, and global improvement. Linear mixed models were used to analyse outcomes. The primary analysis included longitudinal outcomes in the short (week 4–12) and long-term (week 4–52). An omnibus test assessing differences across all groups over the year was used to control for multiplicity. Secondary analyses included outcomes at each time point and responder analyses. This study was funded by the US Department of Health and Human Services, Health Resources and Services Administration.
A total of 241 participants were randomized and 230 (95%) provided complete primary outcome data. The primary analysis showed group differences in pain over the one-year were small and not statistically significant. Pain severity was reduced by 30 to 40% after treatment in all 3 groups with the largest difference (eight percentage points) favouring SMT and home exercise over home exercise alone. Group differences at other time points ranged from 0 to 6 percentage points with no consistent pattern favouring one treatment. One-year post-treatment pain reductions diminished in all three groups. Secondary self-report outcomes followed a similar pattern with no important group differences, except satisfaction with care, where the two combination groups were consistently superior to home exercise alone.
The authors concluded that adding spinal manipulation or supervised rehabilitative exercise to home exercise alone does not appear to improve pain or disability in the short- or long-term for older adults with chronic low back pain, but did enhance satisfaction with care.
It is rare to find such a well designed, conducted and reported study in the realm of SCAM. Its results are clear and show that SMT offers no benefit over exercise in this LBP population. The better satisfaction rate with SMT is to be expected; it is probably due to the extra attention this option offers. The most recent systematic review addressing non-pharmacologic treatments for chronic LBP has found evidence of modest short-term improvements in function and/or pain for both exercise and SMT when compared to usual care, attention control, sham, or placebo, and no clear differences between exercise and SMT. In view of the facts that
- SMT might cause adverse effects,
- exercise is cheaper,
- exercise conveys benefits beyond back pain,
the new findings are a very clear verdict: exercise is preferable to SMT in the treatment of LBP.
Radix Salviae Miltiorrhizae (Danshen) is a herbal remedy that is part of many TCM herbal mixtures. Allegedly, Danshen has been used in clinical practice for over 2000 years.
But is it effective?
The aim of this systematic review was to evaluate the current available evidence of Danshen for the treatment of cancer. English and Chinese electronic databases were searched from PubMed, the Cochrane Library, EMBASE, and the China National Knowledge Infrastructure (CNKI), VIP database, Wanfang database until September 2018. The methodological quality of the included studies was evaluated by using the method of Cochrane system.
Thirteen RCTs with 1045 participants were identified. The studies investigated the lung cancer (n = 5), leukemia (n = 3), liver cancer (n = 3), breast or colon cancer (n = 1), and gastric cancer (n = 1). A total of 83 traditional Chinese medicines were used in all prescriptions and there were three different dosage forms. The meta-analysis suggested that Danshen formulae had a significant effect on RR (response rate) (OR 2.38, 95% CI 1.66-3.42), 1-year survival (OR 1.70 95% CI 1.22-2.36), 3-year survival (OR 2.78, 95% CI 1.62-4.78), and 5-year survival (OR 8.45, 95% CI 2.53-28.27).
The authors concluded that the current research results showed that Danshen formulae combined with chemotherapy for cancer treatment was better than conventional drug treatment plan alone.
I am getting a little tired of discussing systematic reviews of so-called alternative medicine (SCAM) that are little more than promotion, free of good science. But, because such articles do seriously endanger the life of many patients, I do nevertheless succumb occasionally. So here are a few points to explain why the conclusions of the Chinese authors are nonsense:
- Even though the authors claim the trials included in their review were of high quality, most were, in fact, flimsy.
- The trials used no less than 83 different herbal mixtures of dubious quality containing Danshen. It is therefore not possible to define which mixture worked and which did not.
- There is no detailed discussion of the adverse effects and no mention of possible herb-drug interactions.
- There seemed to be a sizable publication bias hidden in the data.
- All the eligible studies were conducted in China, and we know that such trials are unreliable to say the least.
- Only four articles were published in English which means those of us who cannot read Chinese are unable to check the correctness of the data extraction of the review authors.
I know it sounds terribly chauvinistic, but I do truly believe that we should simply ignore Chinese articles, if they have defects that set our alarm bells ringing – if not, we are likely to do a significant disservice to healthcare and progress.
One of the most difficult things in so-called alternative medicine (SCAM) can be having a productive discussion with patients about the subject, particularly if they are deeply pro-SCAM. The task can get more tricky, if a patient is suffering from a serious, potentially life-threatening condition. Arguably, the discussion would become even more difficult, if the SCAM in question is relatively harmless but supported only by scarce and flimsy evidence.
An example might be the case of a cancer patient who is fond of mindfulness cognitive therapy (MBCT), a class-based program designed to prevent relapse or recurrence of major depression. To contemplate such a situation, let’s consider the following hypothetical exchange between a patient (P) and her oncologist (O).
P: I often feel quite low, do you think I need some treatment for depression?
O: That depends on whether you are truly depressed or just a bit under the weather.
P: No, I am not clinically depressed; it’s just that I am worried and sometimes see everything in black.
O: I understand, that’s not an unusual thing in your situation.
P: Someone told me about MBCT, and I wonder what you think about it.
O: Yes, I happen to know about this approach, but I’m not sure it would help you.
P: Are you sure? A few years ago, I had some MBCT; it seemed to work and, at least, it cannot do any harm.
O: Yes, that’s true; MBCT is quite safe.
P: So, why are you against it?
O: I am not against it; I just doubt that it is the best treatment for you.
P: Why?
O: Because there is little evidence for it and even less for someone like you.
P: But I have seen some studies that seem to show it works.
O: I know, there have been trials but they are not very reliable.
P: But the therapy has not been shown to be ineffective, has it?
O: No, but the treatment is not really for your condition.
P: So, you admit that there is some positive evidence but you are still against it because of some technicalities with the science?
O: No, I am telling you that this treatment is not supported by good evidence.
P: And therefore you want me to continue to suffer from low mood? I don’t call that very compassionate!
O: I fully understand your situation, but we ought to find the best treatment for you, not just one that you happen to be fond of.
P: I don’t understand why you are against giving MBCT a try; it’s safe, as you say, and there is some evidence for it. And I have already had a good experience with it. Is that not enough?
O: My role as your doctor is to provide you with advice about which treatments are best in your particular situation. There are options that are much better than MBCT.
P: But if I want to try it?
O: If you want to try MBCT, I cannot prevent you from doing so. I am only trying to tell you about the evidence.
P: Fine, in this case, I will give it a go.
___________________________________________________
Clearly this discussion did not go all that well. It was meant to highlight the tension between the aspirations of a patient and the hope of a responsible clinician to inform his patient about the best available evidence. Often the evidence is not in favour of SCAM. Thus there is a gap that can be difficult to breach. (Instead of using MBCT, I could, of course, have used dozens of other SCAMs like homeopathy, chiropractic, Reiki, etc.)
The pro-SCAM patient thinks that, as she previously has had a good experience with SCAM, it must be fine; at the very minimum, it should be tried again, and she wants her doctor to agree. The responsible clinician thinks that he ought to recommend a therapy that is evidence-based. The patient feels that scientific evidence tells her nothing about her experience. The clinician insists that evidence matters. The patient finds the clinician lacks compassion. The clinician feels that the most compassionate and ethical strategy is to recommend the most effective therapy.
As the discussion goes on, the gap is not closing but seems to be widening.
What can be done about it?
I wish I knew the answer!
Do you?
Fibromyalgia (FM) is one of the most frequent generalized pain disorders. It accounts for a sizable proportion of healthcare costs. Despite extensive research, the etiology (the ‘root cause’) of FM remains unknown – except, of course, to SCAM practitioners!
Most types of SCAM are said to be effective for FM (while the evidence for such claims is less than solid).
And almost every one of them claims to treat the ‘root cause’ of the condition. Which must mean that they are able to tackle its etiology, usually some disturbance of the ‘vital force’ or ‘energy’ flow. To patients, this sadly sounds impressive.
But what, if the etiology of FM is something entirely different?
New research shows that most (if not all) patients with FM belong to a distinct population that can be segregated from a control group by their glycated haemoglobin A1c (HbA1c) levels, a surrogate marker of insulin resistance (IR). This was demonstrated by analysing the data after introducing an age stratification correction into a linear regression model. This strategy showed highly significant differences between FM patients and control subjects (p < 0.0001 and p = 0.0002, for two separate control populations, respectively).
A subgroup of FM patients meeting criteria for pre-diabetes or diabetes (patients with HbA1c values of 5.7% or greater) who had undergone treatment with metformin showed dramatic improvements of their widespread myofascial pain. This was shown comparing pre and post-treatment numerical pain rating scale (NPRS). Response to metformin plus standard treatment (ST) was followed by complete resolution of the pain (report of 0 of 10 in the NPRS) in 8 of 16 patients who had been treated with metformin (50%), a degree of improvement never observed before in such a large proportion of FM patients subjected to any available treatment. In contrast, patients treated with ST alone improved, but complete resolution of pain was generally not observed. Interestingly, some patients responded only to metformin and not to ST with NSRIs or membrane stabilizing agents. Importantly, there was a long-term retention of the analgesic effect of metformin.
The authors concluded that these findings suggest a pathogenetic relationship between FM and IR, which may lead to a radical paradigm shift in the management of this disorder.
From my perspective, these findings also suggest that all the many SCAMs allegedly claiming to tackle the ‘root cause’ of FM have been barking up the wrong tree. In fact, all these claims of SCAM practitioners about treating the ‘root causes’ can easily be disclosed as a simple (and sadly effective) marketing gimmick. Six years ago, I even challenged the world of SCAM to name a single treatment that treats the ‘root cause’ of any disease. As yet, nobody has come forward with a convincing suggestion.
‘Rationable’ has recently published a remarkable article on homeopathy. Its author starts admitting that for most of my life, I have taken it for granted that homoeopathy worked. I didn’t know how or why, I just knew that my parents and most other people swore by it, so there had to be something to it. I was treated with homoeopathy several times. In one case, it actually made things worse. The homoeopathic doctor responded with, “Things sometimes have to get worse before they get better.” I have to admit, as much as I wasn’t impressed with that answer, I liked the taste of the medicines. Always sugary and sweet or even with that little bit of alcohol. What more does a kid need in his life than to eat something sugary sweet for medicine!
The article is lengthy but well worth reading. I take the liberty of merely quoting its conclusion:
Here I am, a decade later, seeing homoeopathy from a completely different perspective than what I used to. It’s probably one of the most profound discoveries in my life and has been one of the factors that have led me to question everything, including, most importantly, myself.
Now, homoeopathy has become one of the most studied fields in the world, with an impenetrable mountain of evidence that has piled up against its claims. These studies have been done by many independent teams and analysed and reviewed by some of the most reliable scientific organisations in the world. There’s just no denying it. There is no evidence for it working…ever. Why? Because it’s just water. And if it’s brought into contact with sugar, it somehow transfers its memories to it. The more I think about it, the more implausible it sounds.
And it’s not just me. Many governmental bodies like UK’s National Health Service (NHS), The American Medical Association, the FASEB and National Health and Medical Research Council of Australia, have stated that there is no evidence to support the use of homoeopathic treatments. Even representatives of the WHO have said that homoeopathic remedies should not be used to treat tuberculosis or diarrhoea.
So, what do you think? Is it worth your time and money to buy water and sugar pills that have shown no evidence of working, or would you instead go to a regular doctor and get real medication that has a good chance of treating you? I, for one, will be going to the latter.
TL;DR
As promised, here’s the short version of this topic:
Homoeopathy is an ancient practice created in the 1700s as a counter treatment to bloodletting and other rather horrific medical practices
Homoeopathy is a process of diluting a small amount substance in more water than the whole earth can contain to treat your ailment
There has been no evidence to show that it works any better than a placebo, even after hundreds of clinical trials have been conducted.
Dig Deeper
https://www.theguardian.com/science/blog/2012/apr/03/homeopathy-why-i-changed-my-mind
https://skeptoid.com/blog/2011/09/18/homeopathy-a-drop-in-10-billion-oceans/
https://nccih.nih.gov/health/homeopathy
https://www.livescience.com/31977-homeopathy.html
https://www.nhs.uk/conditions/homeopathy/
___________________________________________________
I am always delighted to see how individuals who start thinking critically can change things for themselves and others. The evidence suggests that people who are strong on either intelligence or critical thinking experience fewer negative events, but critical thinkers tend to do better. I hope that, one day, all readers of this blog manage to benefit from the great potential of critical thinking.