musculoskeletal problems
There is widespread agreement amongst clinicians that people with non-specific low back pain (NSLBP) comprise a heterogeneous group and that their management should be individually tailored. One treatment known by its tailored design is the McKenzie method (e.g. an individualized program of exercises based on clinical clues observed during assessment) used mostly but not exclusively by physiotherapists.
A recent Cochrane review evaluated the effectiveness of the McKenzie method in people with (sub)acute non-specific low back pain. Randomized clinical trials (RCTs) investigating the effectiveness of the McKenzie method in adults with (sub)acute (less than 12 weeks) NSLBP.
Five RCTs were included with a total of 563 participants recruited from primary or tertiary care. Three trials were conducted in the USA, one in Australia, and one in Scotland. Three trials received financial support from non-commercial funders and two did not provide information on funding sources. All trials were at high risk of performance and detection bias. None of the included trials measured adverse events.
McKenzie method versus minimal intervention (educational booklet; McKenzie method as a supplement to other intervention – main comparison) There is low-certainty evidence that the McKenzie method may result in a slight reduction in pain in the short term (MD -7.3, 95% CI -12.0 to -2.56; 2 trials, 377 participants) but not in the intermediate term (MD -5.0, 95% CI -14.3 to 4.3; 1 trial, 180 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -2.5, 95% CI -7.5 to 2.0; 2 trials, 328 participants) nor in the intermediate term (MD -0.9, 95% CI -7.3 to 5.6; 1 trial, 180 participants).
McKenzie method versus manual therapy There is low-certainty evidence that the McKenzie method may not reduce pain in the short term (MD -8.7, 95% CI -27.4 to 10.0; 3 trials, 298 participants) and may result in a slight increase in pain in the intermediate term (MD 7.0, 95% CI 0.7 to 13.3; 1 trial, 235 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -5.0, 95% CI -15.0 to 5.0; 3 trials, 298 participants) nor in the intermediate term (MD 4.3, 95% CI -0.7 to 9.3; 1 trial, 235 participants).
McKenzie method versus other interventions (massage and advice) There is very low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD 4.0, 95% CI -15.4 to 23.4; 1 trial, 30 participants) nor in the intermediate term (MD 10.0, 95% CI -8.9 to 28.9; 1 trial, 30 participants).
The authors concluded that, based on low- to very low-certainty evidence, the treatment effects for pain and disability found in our review were not clinically important. Thus, we can conclude that the McKenzie method is not an effective treatment for (sub)acute NSLBP.
The hallmark of the McKenzie method for back pain involves the identification and classification of nonspecific spinal pain into homogenous subgroups. These subgroups are based on the similar responses of a patient’s symptoms when subjected to mechanical forces. The subgroups include postural syndrome, dysfunction syndrome, derangement syndrome, or “other,” with treatment plans directed to each subgroup. The McKenzie method emphasizes the centralization phenomenon in the assessment and treatment of spinal pain, in which pain originating from the spine refers distally, and through targeted repetitive movements the pain migrates back toward the spine. The clinician will then use the information obtained from this assessment to prescribe specific exercises and advise on which postures to adopt or avoid. Through an individualized treatment program, the patient will perform specific exercises at home approximately ten times per day, as opposed to 1 or 2 physical therapy visits per week. According to the McKenzie method, if there is no restoration of normal function, tissue healing will not occur, and the problem will persist.
Classification:
The postural syndrome is pain caused by mechanical deformation of soft tissue or vasculature arising from prolonged postural stresses. These may affect the joint surfaces, muscles, or tendons, and can occur in sitting, standing, or lying. Pain may be reproducible when such individuals maintain positions or postures for sustained periods. Repeated movements should not affect symptoms, and relief of pain typically occurs immediately following the correction of abnormal posture.
The dysfunction syndrome is pain caused by the mechanical deformation of structurally impaired soft tissue; this may be due to traumatic, inflammatory, or degenerative processes, causing tissue contraction, scarring, adhesion, or adaptive shortening. The hallmark is a loss of movement and pain at the end range of motion. Dysfunction has subsyndromes based upon the end-range direction that elicits this pain: flexion, extension, side-glide, multidirectional, adherent nerve root, and nerve root entrapment subsyndromes. Successful treatment focuses on patient education and mobilization exercises that focus on the direction of the dysfunction/direction of pain. The goal is on tissue remodeling which can be a prolonged process.
The derangement syndrome is the most commonly encountered pain syndrome, reported in one study to have a prevalence as high as 78% of patients classified by the McKenzie method. It is caused by an internal dislocation of articular tissue, causing a disturbance in the normal position of affected joint surfaces, deforming the capsule, and periarticular supportive ligaments. This derangement will both generate pain and obstruct movement in the direction of the displacement. There are seven different subsyndromes which are classified by the location of pain and the presence, or absence, of deformities. Pain is typically elicited by provocative assessment movements, such as flexion or extension of the spine. The centralization and peripheralization of symptoms can only occur in the derangement syndrome. Thus the treatment for derangement syndrome focuses on repeated movement in a single direction that causes a gradual reduction in pain. Studies have shown approximately anywhere between 58% to 91% prevalence of centralization of lower back pain. Studies have also shown that between 67% to 85% of centralizers displayed the directional preference for a spinal extension. This preference may partially explain why the McKenzie method has become synonymous with spinal extension exercises. However, care must be taken to accurately diagnose the direction of pain, as one randomized controlled study has shown that giving the ‘wrong’ direction of exercises can actually lead to poorer outcomes.
Other or Nonmechanical syndrome refers to any symptom that does not fit in with the other mechanical syndromes, but exhibits signs and symptoms of other known pathology; Some of these examples include spinal stenosis, sacroiliac disorders, hip disorders, zygapophyseal disorders, post-surgical complications, low back pain secondary to pregnancy, spondylolysis, and spondylolisthesis.
CONCLUSION:
“Internationally researched” and found to be ineffective!
I have seen some daft meta-analyses in my time – this one, however, takes the biscuit. Here is its unaltered abstract:
Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
___________________________
This meta-analysis has too many serious flaws to mention. Let me therefore just focus on the main two:
- Craniosacral Therapy is not an MBMBT.
- Craniosacral Therapy is not effective for NLBP. The false positive result was generated on the basis of 4 studies. All of them have serious methodological problems that prevent an overall positive conclusion about the effectiveness of this treatment. In case you don’t believe me, here are the 4 abstracts:
1) Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
2) Background: Craniosacral therapy (CST) and sensorimotor training (SMT) are two recommended interventions for nonspecific chronic low back pain (NCLBP). This study compares the effects of CST and SMT on pain, functional disability, depression and quality of life in patients with NCLBP.
Methodology: A total of 31 patients with NCLBP were randomly assigned to the CST group (n=16) and SMT (n=15). The study patients received 10 sessions of interventions during 5 weeks. Visual analogue scale (VAS), Oswestry disability index (ODI), Beck depression inventory-II (BDI-II), and Short Form-36 (SF-36) questionnaires were used at baseline (before the treatment), after the treatment, and 2 months after the last intervention session. Results were compared and analyzed statistically.
Results: Both groups showed significant improvement from baseline to after treatment (p < 0.05). In the CST group, this improvement continued during the follow-up period in all outcomes (p < 0.05), except role emotional domain of SF-36. In the SMT group, VAS, ODI and BDI-II increased during follow-up. Also, all domains of SF-36 decreased over this period. Results of group analysis indicate a significant difference between groups at the end of treatment phase (p < 0.05), except social functioning.
Conclusions: Results of our research confirm that 10 sessions of craniosacral therapy (CST) or sensorimotor training (SMT) can significantly control pain, disability, depression, and quality of life in patients with NCLBP; but the efficacy of CST is significantly better than SMT.
3) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
4) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
_______________________________
I REST MY CASE
This study allegedly evaluated the efficacy of osteopathic manipulative therapy (OMT) compared to that of the Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) for patients with chronic LBP.
It included 68 participants of both genders, aged 30 to 60, with chronic LBP. Participants were randomly assigned to one of two parallel groups, each with 34 members. The OMT group received, as a direct technique, a high-velocity/low-amplitude (HVLA) impulse, and as indirect techniques, strain counterstrain (SCS), myofascial release (MFR), and visceral mobilization therapy (VMT). The KEOMT group received lumbar segmental traction and lumbar segmental mobilization-flexion and gliding therapy grade 3. The participants in both groups received 10 treatments, two per week for five weeks. The primary outcome was pain severity, using a numeric pain rating scale (NPRS). The secondary outcome was the measurement of functional disability, using the Oswestry Disability Index (ODI).
The OMT and KEOMT both decreased pain and disability; however, the changes on the NPRS and ODI postintervention were statistically greater for the OMT group compared to the KEOMT group (P < .05).
The authors concluded that the OMT was better at reducing pain and improving quality of life. It reduced functional disability more than KEOMT in patients with chronic LBP.
The Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) concept is a treatment and training system based upon a comprehensive biomechanical evaluation of the arthro-neuro-muscular system and an individual’s functional abilities. This system of diagnosis and patient management applies to both patients with acute, subacute and chronic conditions of the spine and extremities and to athletes seeking to improve performance. It offers a reliable and practical approach that focuses on optimal physical health and function.
Has the KEOMT concept been tested and shown to be effective for LBP?
No!
So, what we have here is an equivalence trial of two manual techniques. As such it is FAR too small to yield a meaningful result. If the findings were meaningful, would they show that OMT is effective?
No!
As we have no proof that KEOMT does not impede recovery from LBP, the result could merely be due to the fact that OMT does not influence the natural history of LBP, while KEOMT has a detrimental effect.
Last question: which journal publishes such rubbish?
Ahh, it’s the remarkable Alternative therapies in health and medicine. That explains a lot!
An explanatory sequential mixed methods study with three separate phases was conducted in Danish patients with lumbar radiculopathy receiving a standardized chiropractic care package (SCCP). Lumbar radiculopathy is pain and other neurological symptoms caused by the pinching of nerve roots where they leave your spinal cord in the lumbar region. 
Phase one of the study was a quantitative analysis based on a survey in a prospective cohort of patients with lumbar radiculopathy in an SCCP from 2018 to 2020. Patients rated their satisfaction with the examination, information, treatment effect, and overall management of their problem on a 0–10 scale. In phase two, six semi-structured interviews conducted in 2021 were used to gain further explanatory insights into the findings from phase one. Data were analyzed using systematic text condensation. In phase three, the quantitative and qualitative data were merged in a narrative joint display to obtain a deeper understanding of the overall results.
Here I am only interested in the patients’ perception of the treatment effect. Of 303 eligible patients, 238 responded to the survey. Of these, 50% were very satisfied with the treatment effect.
The authors stated that patients in their study expected a rapid and persistent decrease in symptoms, which, unfortunately, does not match the prognosis of lumbar radiculopathy. Although the prognosis is considered good, the improvement happens gradually and often with fluctuating pain patterns, and it is not unusual to have milder symptoms for three months or longer.
So, only half of the patients who had chosen to consult chiropractors for their lumbar radiculopathy were very satisfied with the treatment results. In most patients, the symptoms decreased only gradually often with fluctuating pain patterns, and the authors comment that symptoms frequently last for three months or longer with a SCCP.
Impressive?
Might I point out that what is being described here looks to me very much like the natural history of lumbar radiculopathy? About 90% of patients with back pain caused by disc herniation see improvements within three months without therapy. Are the authors aware that their observational study is in accordance with the notion that the SCCP does nothing or very little to help patients suffering from lumbar radiculopathy?
This meta-analysis aimed “to provide better evidence of the efficacy of manual therapy (MT) on adolescent idiopathic scoliosis (AIS)”. 
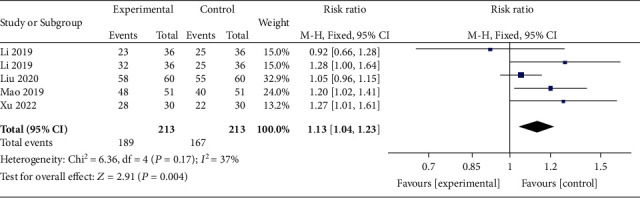
All RCTs of MT for the management of patients with AIS were included in the present study. The treatment difference between the experimental and control group was mainly MT. The outcomes consisted of the total effective rate, the Cobb angle, and Scoliosis Research Society-22 (SRS-22) questionnaire score. Electronic database searches were conducted from database inception to July 2022, including the Cochrane Library, PubMed, Web of Science, Embase, Wanfang Data, CNKI, and VIP. The pooled data were analyzed using RevMan 5.4 software.
Four RCTs with 213 patients in the experimental groups were finally included. There are 2 studies of standalone MT in the experimental group and 3 studies of MT with identical conservative treatments in the control group. Three trials reported the total effective rate and a statistically significant difference was found (P = 0.004). Three trials reported Cobb angle; a statistical difference was found (P = 0.01). Then, sensitivity analysis showed that there was a significant difference in the additional MT subgroup (P < 0.00001) while not in the standalone MT subgroup (P = 0.41). Three trials reported SRS-22 scores (P = 0.55) without significant differences.
The authors concluded that there is insufficient data to determine the effectiveness of spinal manipulation limited by the very low quality of included studies. High-quality studies with appropriate design and follow-up periods are warranted to determine if MT may be beneficial as an adjunct therapy for AIS. Currently, there is no evidence to support spinal manipulation. 
The treatment of idiopathic scoliosis depends on the age, curve size, and progression of the condition. Therapeutic options include observation, bracing, physiotherapy, and surgery. They do NOT include MT because it is neither a plausible nor effective solution to this problem. It follows that further studies are not warranted and should be discouraged.
And, even if you disagree with me here and feel that further studies might be justified, let me remind you that proper research is never aimed at providing better evidence that a therapy works (as the authors of this odd paper seem to think); it must be aimed at testing whether it is effective!
This review investigated the characteristics, hotspots, and frontiers of global scientific output in acupuncture research for chronic pain over the past decade. the authors retrieved publications on acupuncture for chronic pain published from 2011 to 2022 from the Science Citation Index Expanded (SCI-expanded) of the Web of Science Core Collection (WoSCC). The co-occurrence relationships of journals/countries/institutions/authors/keywords were performed using VOSviewer V6.1.2, and CiteSpace V1.6.18 analyzed the clustering and burst analysis of keywords and co-cited references.
A total of 1616 articles were retrieved. The results showed that:
- the number of annual publications on acupuncture for chronic pain has increased over time;
- the main types of literature are original articles (1091 articles, 67.5 %) and review articles (351 articles, 21.7 %);
- China had the most publications (598 articles, 37 %), with Beijing University of Traditional Chinese Medicine (93 articles, 5.8 %);
- Evidence-based Complementary and Alternative Medicine ranked first (169 articles, 10.45 %) as the most prolific affiliate and journal, respectively;
- Liang FR was the most productive author (43 articles);
- the article published by Vickers Andrew J in 2012 had the highest number of citations (625 citations).
Recently, “acupuncture” and “pain” appeared most frequently. The hot topics in acupuncture for chronic pain based on keywords clustering analysis were experimental design, hot diseases, interventions, and mechanism studies. According to burst analysis, the main research frontiers were functional connectivity (FC), depression, and risk.
The authors concluded that this study provides an in-depth perspective on acupuncture for chronic pain studies, revealing pivotal points, research hotspots, and research trends. Valuable ideas are provided for future research activities.
I might disagree with the authors’ conclusion and would argue that they have demonstrated that:
- the acupuncture literature is dominated by China, which is concerning because we know that 1) these studies are of poor quality, 2) never report negative findings, and 3) are often fabricated;
- the articles tend to be published in journals that are more than a little suspect.
As we have seen recently, the reliable evidence that acupuncture remains effective is wafer-thin. Therefore, I feel that we are currently being misled by a flurry of rubbish publications that have one main aim: to distract from the fact that acupuncture might be nonsense.
The McTimoney College of Chiropractic just announced that it has established a new four-year program in veterinary chiropractic for college students:
It means that those without a prior degree can undertake the training and education necessary to enter this coveted career. To date, animal chiropractors were required to have a prior qualification in human chiropractic or a degree in the relevant sciences.
Applications for the new program are being accepted from September 2023. Students will attend Abingdon-based University, Oxford, and a variety of practical locations, enabling the development of academic knowledge and the application of practical skills together . Modules include anatomy and physiology, veterinary science, practice and professionalism, and clinical skills, with a research dissertation running over the four-year course.
University director Christina Cunliffe said the new program was an exciting step in the development of chiropractic care for animals.
“Building on our decades of experience graduating confident, competent, and highly-skilled animal chiropractors, now is the time to open up this exciting career opportunity to college students.”
For the past 50 years, McTimoney College of Chiropractic has been training and educating human chiropractors to the highest regulatory standards. Over the past 20 years, animal chiropractic has developed to meet the requirements for this gentle, holistic treatment in the veterinary world.
Prospective students are invited to a Open House at McTimoney College of Chiropractic in Abingdon on February 16.
McTimoney Chiropractic for Animals identifies areas of stiffness, asymmetry, and poor range of motion within the skeletal system, particularly the spine and pelvis. This affects the muscles that surround these structures, as well as the nerve impulses that pass from the central nervous system to the periphery of the body. The adjustments are very light and fast, stimulating an instant response in the affected soft tissues and joints, promoting relaxation of muscle spasms, improving nerve function, and helping the skeletal structure regain better symmetry and movement again.
In many cases, animals suffer from underlying conditions such as arthritic changes or degenerative diseases that force them to compensate in their posture and movement in an attempt to remain comfortable. However, these offsets become increasingly entrenched and can be painful or uncomfortable, requiring chiropractic care to provide some relief. In other cases, the animals are working hard or competing and as such accumulate tension and asymmetries due to the demands of their work. Once again, chiropractic care helps relieve pain and promote performance, whether it’s faster speeds over hurdles for racehorses and events, better jumping style in showjumpers, or more extravagant movements for dressage stars.
Two recent graduates of the school’s Master of Animal Handling (Chiropractic) program did not hesitate to recommend the university. Natalie McQuiggan said that she had wanted to do McTimoney Chiropractic from a very young age, “but the process of doing it always seemed really daunting.
“But from the start, the staff and teachers were lovely and welcoming, and queries were answered promptly. I have really enjoyed my two years in the Master of Animal Handling (Chiropractic) program and would recommend anyone thinking of doing it to just do it.”
Pollyanna Fitzgerald said the university offered a supportive and welcoming learning environment, allowing her to grow and develop as a student and future professional. “There is always someone to talk to and offer encouragement when needed. As a student I have learned a lot and have been encouraged to believe in myself and it has been a wonderful place to learn.”
A free webinar, McTimoney’s Animal Chiropractic as a Careeron January 24 at 7:30 p.m. (GMT), is open to those who wish to learn more about the McTimoney technique and its application, and the training paths available to those interested in becoming a McTimoney Animal Chiropractor.
________________________
I think this announcement is puzzling on several levels:
- I was unable to find an ‘Abingdon-based University, Oxford’; could it be this institution that is a college and not a university?
- Christina Cunliffe seems to be (or has been?) affiliated with the McTimoney College of Chiropractic which is a bit odd, in my opinion.
- The college does not have ‘decades of experience’; it was founded only in 2001.
- Most importantly, I am unable to find a jot of good evidence that veterinary chiropractic is effective for any condition (see also here, here, and here). In case anyone is aware of any, please let me know. I’d be delighted to revise my judgment.
If I am right, the new course could be a fine example of quackademia where students are ripped off and taught to later rip off the owners of animals after the academically trained quacks have mistreated them.
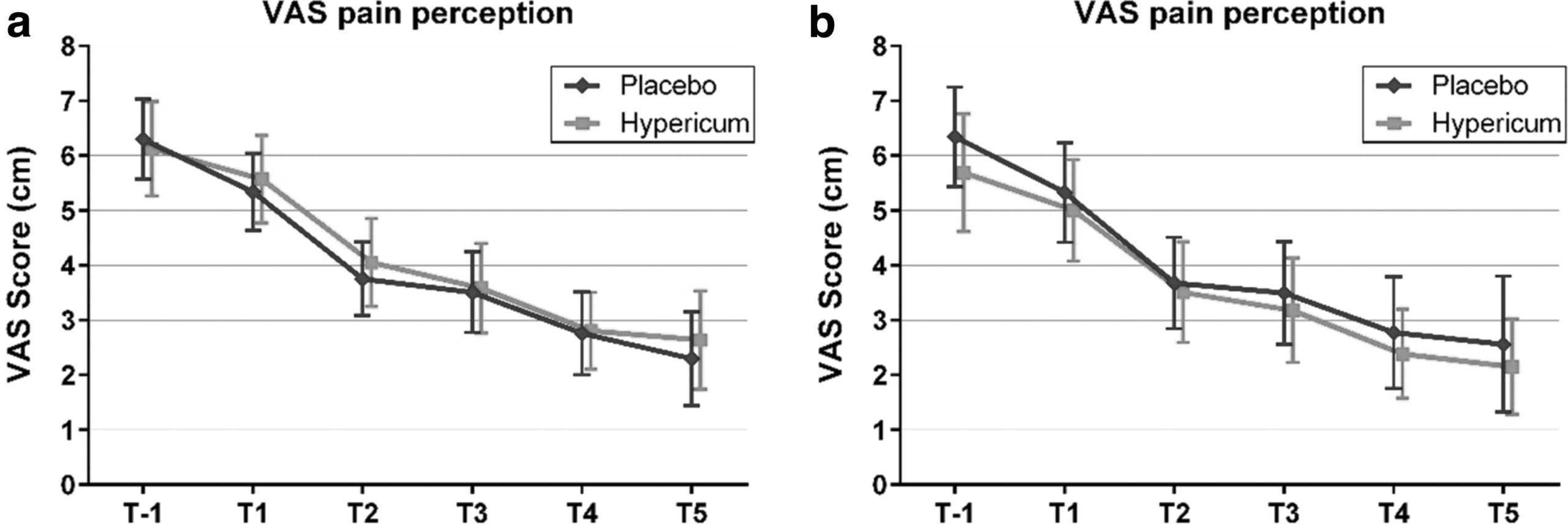
Hypericum perforatum (St John’s wort) is often recommended as a remedy to relieve pain caused by nerve damage. This trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo.
The study was designed as a randomized double-blind, monocentric, placebo-controlled clinical trial with inpatients undergoing surgery for lumbar sequestrectomy. Homeopathic treatment was compared to placebo, both in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The results show that the change in pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
For a number of reasons, this is a remarkably mysterious and quite hilarious study:
- Hypericum is recommended as an analgesic for neuropathic pain.
- According to the ‘like cures like’ axiom of homeopathy, it therefore must increase pain in such situations.
- Yet, the authors of this trial mounted an RCT to see whether it reduces pain.
- Thus they either do not understand homeopathy or wanted to sabotage it.
- As they are well-known pro-homeopathy researchers affiliated with a university that promotes homeopathy (Witten/Herdecke University, Herdecke, Germany), both explanations are highly implausible.
- The facts that the paper was published in a pro-SCAM journal (J Integr Complement Med), and the study was sponsored by the largest German firm of homeopathics (Deutsche Homoeopathische Union) renders all this even more puzzling.
- However, these biases do explain that the authors do their very best to mislead us by including some unwarranted ‘positive’ findings in their overall conclusions.
In the end, none of this matters, because the results of the study reveal that firstly the homeopathic ‘law of similars’ is nonsense, and secondly one homeopathic placebo (i.e. Hypericum C200) produces exactly the same outcomes as another, non-homeopathic placebo.
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
The aim of this evaluator-blinded randomized clinical trial was to determine if manual therapy added to a therapeutic exercise program produced greater improvements than a sham manual therapy added to the same exercise program in patients with non-specific shoulder pain. 
Forty-five subjects were randomly allocated into one of three groups:
- manual therapy (glenohumeral mobilization technique and rib-cage technique);
- thoracic sham manual therapy (glenohumeral mobilization technique and rib-cage sham technique);
- sham manual therapy (sham glenohumeral mobilization technique and rib-cage sham technique).
All groups also received a therapeutic exercise program. Pain intensity, disability, and pain-free active shoulder range of motion were measured post-treatment and at 4-week and 12-week follow-ups. Mixed-model analyses of variance and post hoc pairwise comparisons with Bonferroni corrections were constructed for the analysis of the outcome measures.
All groups reported improved pain intensity, disability, and pain-free active shoulder range of motion. However, there were no between-group differences in these outcome measures.
The authors concluded that the addition of the manual therapy techniques applied in the present study to a therapeutic exercise protocol did not seem to add benefits to the management of subjects with non-specific shoulder pain.
What does that mean?
I think it means that the improvements observed in this study were due to 1) exercise and 2) a range of non-specific effects, and that they were not due to the manual techniques tested.
I cannot say that I find this enormously surprising. But I would also find it unsurprising if fans of these methods would claim that the results show that the physios applied the techniques not correctly.
In any case, I feel this is an interesting study, not least because of its use of sham therapy. But I somehow doubt that the patients were unable to distinguish sham from verum. If so, the study was not patient-blind which obviously is difficult to achieve with manual treatments.