integrative medicine
I have been informed by the publisher, that my book has been published yesterday. This is about two months earlier than it was announced on Amazon. It is in German – yes, I have started writing in German again. But not to worry, I translated the preface for you:
Anyone who falls ill in Germany and therefore needs professional assistance has the choice, either to consult a doctor or a non-medical practitioner (Heilpraktiker).
– The doctor has studied and is licensed to practice medicine; the Heilpraktiker is state-recognized and has passed an official medical examination.
– The doctor is usually in a hurry, while the Heilpraktiker takes his time and empathizes with his patient.
– The doctor usually prescribes a drug burdened with side effects, while the Heilpraktiker prefers the gentle methods of alternative medicine.
So who should the sick person turn to? Heilpraktiker or doctor? Many people are confused by the existence of these parallel medical worlds. Quite a few finally decide in favor of the supposedly natural, empathetic, time-tested medicine of the Heilpraktiker. The state recognition gives them the necessary confidence to be in good hands there. The far-reaching freedoms the Heilpraktiker has by law, as well as the coverage of costs by many health insurances, are conducive to further strengthening this trust. “We Heilpraktiker are recognized and respected in politics and society,” writes Elvira Bierbach self-confidently, the publisher of a standard textbook for Heilpraktiker.
The first consultation of our model patient with the Heilpraktiker of his choice is promising. The Heilpraktiker responds to the patient with understanding, usually takes a whole hour for the initial consultation, gives explanations that seem plausible, is determined to get to the root of the problem, promises to stimulate the patient’s self-healing powers naturally, and invokes a colossal body of experience. It almost seems as if our patient’s decision to consult a Heilpraktiker was correct.
However, I have quite significant reservations about this. Heilpraktiker are perhaps recognized in politics and society, but from a medical, scientific, or ethical perspective, they are highly problematic. In this book, I will show in detail and with facts why.
The claim of government recognition undoubtedly gives the appearance that Heilpraktiker are adequately trained and medically competent. In reality, there is no regulated training, and the competence is not high. The official medical examination, which all Heilpraktiker must pass is nothing more than a test to ensure that there is no danger to the general public. The ideas of many Heilpraktiker regarding the function of the human body are often in stark contradiction with the known facts. The majority of Heilpraktiker-typical diagnostics is pure nonsense. The conditions that they diagnose are often based on little more than naive wishful thinking. The treatments that Heilpraktiker use are either disproven or not proven to be effective.
There is no question in my mind that Heilpraktiker are a danger to anyone who is seriously ill. And even if Heilpraktiker do not cause obvious harm, they almost never offer what is optimally possible. In my opinion, patients have the right to receive the most effective treatment for their condition. Consumers should not be misled about health-related issues. Only those who are well-informed will make the right decisions about their health.
My book provides this information in plain language and without mincing words. It is intended to save you from a dangerous misconception of the Heilpraktiker profession. Medical parallel worlds with the radically divergent quality standard – doctor/Heilpraktiker – are not in the interest of the patient and are simply unacceptable for an enlightened society.
I have grumbled about prevalence surveys in so-called alternative medicine (SCAM) before, I know. But, as the problem continues to get on my nerves – I estimate that there are about 10 times more surveys in SCAM than in any other field – allow me to do it again. The subject appeared on my screen in the form of a recent article from a minor, not Medline-listed journal. The paper is entitled:
Investigation of Complementary and Alternative Medicine Use in Turkish Patients with Epilepsy
This type of prevalence survey is typical of its genre and stands for hundreds – thousands even – like it. Its findings reveal a high prevalence of use. From that result, enthusiasts tend to draw stereotypical conclusions, namely that we need more research and that we ought to consider the integration of SCAM into routine care.
WHAT A WASTE OF TIME AND EFFORT!
Who really needs to know how many epilepsy patients in Turkey use SCAM?
Nobody!
You disagree?
Fine, then tell me: why Turkey and why epilepsy? If such information were important (and the methodology of the survey were perfect [which it hardly ever is]), then we surely need it for all diseases. How many different diseases are there? Let’s make it easy and say 1000. This means we need 1000 surveys to obtain a valuable picture of SCAM use in Turkey.
And if this sort of information is relevant in Turkey, we need to have it also for all other major countries. How many major countries exist? Let’s make it simple again and say 500. This means that we need 500 x 1000 or 500 000 surveys to generate a meaningful picture of SCAM use.
Since SCAM use changes quickly, we require these articles to be updated regularly; let’s say every 3 years. That means we require half a million surveys every 3 years.
What for?
What would it tell us?
What would we conclude from this enormous body of research?
Yes, of course, we would conclude that we need more research and we ought to consider the integration of SCAM into routine care!
My point is that if we truly need more research, why not get on with it? Why not finally forget about such useless surveys and do the science? Why not determine which SCAM works for what condition and at what risks? And, in case the findings turn out to be positive [but only then], let’s talk about integration into routine care. To put it even blunter:
The survey mania in SCAM prevents progress.
A recent article in ‘The Lancet Regional Health‘ emphasized the “need for reimagining India’s health system and the importance of an inclusive approach for Universal Health Coverage” by employing traditional medicine, including homeopathy. This prompted a response by Siddhesh Zadey that I consider worthy of reproducing here in abbreviated form:
… Since the first trial conducted in 1835 that questioned homeopathy’s efficacy, multiple randomized controlled trials (RCTs) and other studies compiled in several systematic reviews and meta-analyses have shown that there is no reliable and clinically significant effect of non-individualized or individualized homeopathic treatments across disease conditions ranging from irritable bowel syndrome in adults to acute respiratory tract infections in children when compared to placebo or other treatments. Even reviews that support homeopathy’s efficacy consistently caution about low quality of evidence and raise questions on its clinical use. The most recent analysis of reporting bias in homeopathic trials depicted problematic trial conduction practices that further obscure reliability and validity of evidence. Homeopathic treatments have also been linked to aggravations and non-fatal and fatal adverse events.
The Lancet has previously published on another kind of harm that uptake of homeopathy encourages in India: delay to evidence-based clinical care that can lead to fatality. Authors have pointed out that evidence for some of the alternative systems of medicine may not come from RCTs. I agree that more appropriate study designs and analytical techniques are needed for carefully studying individualized treatment paradigms. However, the need for agreement on some consistent form of evidence synthesis and empirical testing across diverse disciplines cannot be discounted. Several other disciplines including psychology, economics, community health, implementation science, and public policy have adopted RCTs and related study designs and have passed the empirical tests of efficacy. Moreover, the ideas around mechanism of action in case of homeopathy still remain controversial and lack evidence after over a century. On the contrary, biochemical, molecular, and physiological mechanistic evidence supporting allopathic treatments has grown abundantly in the same period.
Owing to lack of evidence on its efficacy and safety, the World Health Organization had previously warned against the use of homeopathic treatments for severe diseases. Additionally, multiple countries, including Germany where the practice originated, have initiated mechanisms that discourage uptake of homeopathy while others are considering banning it. Homeopathy doesn’t work, could be harmful, and is not a part of Indian traditional medicine. While we should welcome pluralistic approaches towards UHC, we need to drop homeopathy.
(for references, see original text)
___________________
Yes, in the name of progress and in the interest of patients, “we need to drop homeopathy” (not just in India but everywhere). I quite agree!
This systematic review and meta-analysis aimed to evaluate the effectiveness and safety of Chinese herbal medicine (CHM) combined with Western medicine (WM) in comparison with WM in reducing systolic and diastolic blood pressure for patients with primary hypertension (PHTN).
Various literature searches located a total of 29 studies that included 2623 patients. The results showed that the clinical effectiveness in the treatment of hypertension with CHM+WM was considerably higher than that with WM alone, clinical effective (RR 1.23, 95% CI [1.17, 1.30], P < 0.00001), and markedly effective (ME) in the patients (RR 1.66, 95% CI [1.52, 1.80], and P < 0.00001). Random effect in SBP (MD 7.91 mmHg,[6.00, 983], P < 0.00001) and DBP (MD 5.46 mmHg, [3.88, 6.43], P < 0.00001), a subgroup analysis was carried out based on the type of intervention, duration of treatment, and CHM formulas that showed significance. Furthermore, no severe side effects were reported, and no patients stopped treatment or withdrawal due to any severe adverse events.
The authors concluded that compared to WM alone, the therapeutic effectiveness of CHM combined with WM is significantly improved in the treatment of hypertension. Additionally, CHM with WM may safely and efficiently lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) in individuals with PHTN. However, rigorous randomized controlled trials with a large sample, high quality, long duration of treatment, and follow-up are recommended to strengthen this clinical evidence.
The authors can boast of an impressive list of affiliations:
- 1Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China; School of Pharmacy, Lebanese International University, 18644, Sana’a, Yemen.
- 2Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 3Key Laboratory of Chinese Materia Medica, Ministry of Education of Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 4Department of Urology, Affiliated Hospital of Qingdao Binhai University, Qingdao, Shandong, China.
- 5Department of Respiratory Diseases, Shandong Second Provincial General Hospital, Shandong University, Shandong, China.
- 6Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China. Electronic address: [email protected].
Impressive in the sense of being impressively prone to bias, particularly knowing that ~80% of Chinese research findings have been shown to be fabricated and considering that Chinese authors as good as never publish anything negative about TCM.
But perhaps you still believe that the results reported here are 100% true? In this case, I might even agree with you. The reason is that the authors demonstrate in exemplary fashion what I have been saying so often before:
Blood pressure is one of the many endpoints that are highly prone to placebo effects. Therefore, even the addition of an ineffective CHM to WM would lower blood pressure more effectively than WM alone.
But there is a third way of explaining the findings of this review: some herbal remedies might actually have a hypotensive effect. The trouble is that this review does come not even close to telling us which.
About 3 years ago, I reported that the Bavarian government had decided to fund research into the question of whether the use of homeopathy would reduce the use of antibiotics (an idea that also King Charles fancies). With the help of some friends, I found further details of the project. Here are some of them:
The study on individualized homeopathic treatment to reduce the need for antibiotics in patients with recurrent urinary tract infections is a randomized, placebo-controlled, multicenter, double-blind trial. Frequent urinary tract infections (more than two infections within six months or more than three infections within twelve months) occur in up to three percent of all women during their lifetime and represent a high risk for increased antibiotic use in this population.
The current guidelines therefore also provide for therapeutic approaches without antibiotic administration under close monitoring. The approach to be investigated in the study is the administration of a homeopathic medicine individually selected for the patient for prophylaxis. The number of urinary tract infections and the need for antibiotics will be recorded and evaluated at the end of the trial period, around mid to late 2023.
The aim of the study is to find out whether patients taking homeopathics need antibiotics for the treatment of urinary tract infections less often compared to the placebo group. This could lead to a reduction in the use of antibiotics for recurrent urinary tract infections.
Project participants: Technical University of Munich, Klinikum Rechts der Isar
Project funding: 709,480.75 Euros
Project duration: January 1, 2021 to December 31, 2023
____________________
This sketch is of course not enough for providing a full evaluation of the study concept (if someone has more details, I’d be interested to learn more). From the little information given above, I feel that:
- the design of the trial might be quite rigorous,
- a fairly large sample will be required to have enough power,
- the closing date of 31/12/2023 seems optimistic (but this obviously depends on the number of centers cooperating),
- I, therefore, predict that we will have to wait a long time for the results (the pandemic and other obstacles will have delayed recruitment),
- the costs of the trial are already substantial and might increase due to delays etc.
My main criticism of the study is that:
- I see no rationale for doing such a trial,
- there is no evidence to suggest that homeopathy might prevent recurrent urinary tract infections,
- there is compelling evidence that homeopathic remedies are placebos,
- the study thus compares one placebo with another placebo (in fact, it is a classic example of what my late friend Harriet Hall would have called TOOTH FAIRY SCIENCE),
- therefore, its results will show no difference between the 2 groups (provided the trial was conducted without bias),
- if that is true, enthusiastic homeopaths will claim that the homeopathic verum was inadequate (e.g. because the homeopaths prescribing the verum did not or could not do their job properly),
- when that happens, they will therefore not stop claiming that homeopathy can reduce the over-prescribing of antibiotics;
- that means we will be exactly where we were before the trial.
In other words, the study will turn out to be a waste of 709,480.75 Euros. To express it as I did in my previous post: the Bavarian government has gone barmy!
In this study, the impact of a multimodal integrative oncology pre- and intraoperative intervention on pain and anxiety among patients undergoing gynecological oncology surgery was explored.
Study participants were randomized into three groups:
- Group A received preoperative touch/relaxation techniques, followed by intraoperative acupuncture, plus standard care;
- Group B received preoperative touch/relaxation only, plus standard care;
- Group C (the control group) received standard care.
Pain and anxiety were scored before and after surgery using the Measure Yourself Concerns and Wellbeing (MYCAW) and Quality of Recovery (QOR-15) questionnaires, using Part B of the QOR to assess pain, anxiety, and other quality-of-life parameters.
A total of 99 patients participated in the study: 45 in Group A, 25 in Group B, and 29 in Group C. The three groups had similar baseline demographic and surgery-related characteristics. Postoperative QOR-Part B scores were significantly higher in the treatment groups (A and B) when compared with controls (p = .005), including for severe pain (p = .011) and anxiety (p = .007). Between-group improvement for severe pain was observed in Group A compared with controls (p = .011). Within-group improvement for QOR depression subscales was observed in only the intervention groups (p <0.0001). Compared with Group B, Group A had better improvement of MYCAW-reported concerns (p = .025).
The authors concluded that a preoperative touch/relaxation intervention may significantly reduce postoperative anxiety, possibly depression, in patients undergoing gynecological oncology surgery. The addition of intraoperative acupuncture significantly reduced severe pain when compared with controls. Further research is needed to confirm these findings and better understand the impact of intraoperative acupuncture on postoperative pain.
Regular readers of my blog know only too well what I am going to say about this study.
Imagine you have a basket full of apples and your friend has the same plus a basket full of pears. Who do you think has more fruit?
Dumb question, you say?
Correct!
Just as dumb, it seems, as this study: therapy A and therapy B will always generate better outcomes than therapy B alone. But that does not mean that therapy A per se is effective. Because therapy A generates a placebo effect, it might just be that it has no effect beyond placebo. And that acupuncture can generate placebo effects has been known for a very long time; to verify this we need no RCT.
As I have so often pointed out, the A+B versus B study design never generates a negative finding.
This is, I fear, precisely the reason why this design is so popular in so-called alternative medicine (SCAM)! It enables promoters of SCAM (who are not as dumb as the studies they conduct) to pretend they are scientists testing their therapies in rigorous RCTs.
The most disappointing thing about all this is perhaps that more and more top journals play along with this scheme to mislead the public!
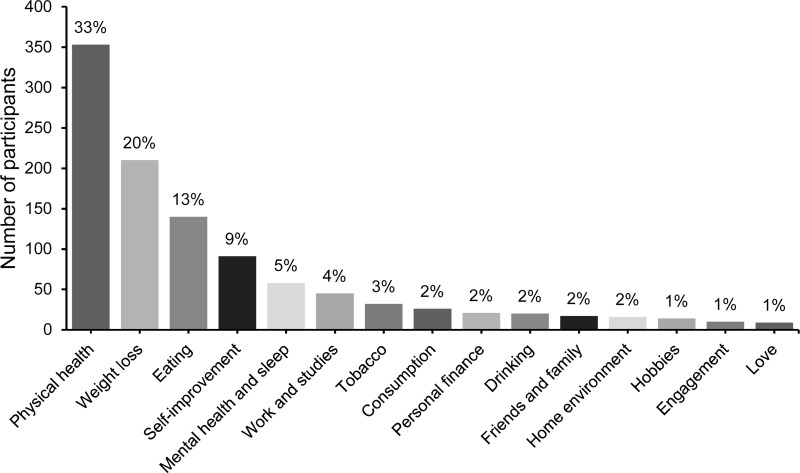
In 2020, a Swedish team published a study investigating what resolutions people make when they are free to formulate them, whether different resolutions reach differing success rates, and whether it is possible to increase the likelihood of a resolution’s success by administering information and exercises on effective goal setting. Participants (N = 1066) from the general public were randomized into three groups:
- active control,
- some support,
- and extended support.
The most popular resolutions regarded physical health, weight loss, and eating habits. At a one-year follow-up, 55% of responders considered themselves successful in sustaining their resolutions. Participants with approach-oriented goals were significantly more successful than those with avoidance-oriented goals (58.9% vs. 47.1%). The group that received some support was exclusively and significantly more successful compared to the other two.
The authors concluded that New Year’s resolutions can have lasting effects, even at a one-year follow-up.
This is a truly interesting study generating a lot of truly boring resolutions.
Boring is, however, something that we must avoid on this blog. In an attempt of doing just this, I decided to lodge my tongue in my cheek and formulate my very own resolutions for 2023 in relation to so-called alternative medicine (SCAM) and this blog. I shall:
- Never again call a comment or a commentator idiotic.
- Never state that chiropractors, homeopaths, osteopaths, naturopaths, or other SCAM practitioners are unethical charlatans.
- Never claim that subluxations, meridians, vital forces, etc. are pure fantasy.
- Never suggest that the assumptions of homeopathy fly in the face of science.
- Never imply that holism, integrative medicine, etc. are just sales gimmicks for crooks to boost their businesses.
- Never again demonstrate that a study is fraudulent just because its findings are too good to be true.
- Never again utter a critical word about our SCAM-loving sovereign, King Charles.
In case you are puzzled by my resolutions, please consider this: contrary to the above-cited evidence, it has been shown that only 12% of people who make new year’s resolutions will actually keep them. And this brings me to my last (and only realistic) resolution for 2023:
8. I shall not feel tempted to adhere to my New Year’s resolutions.
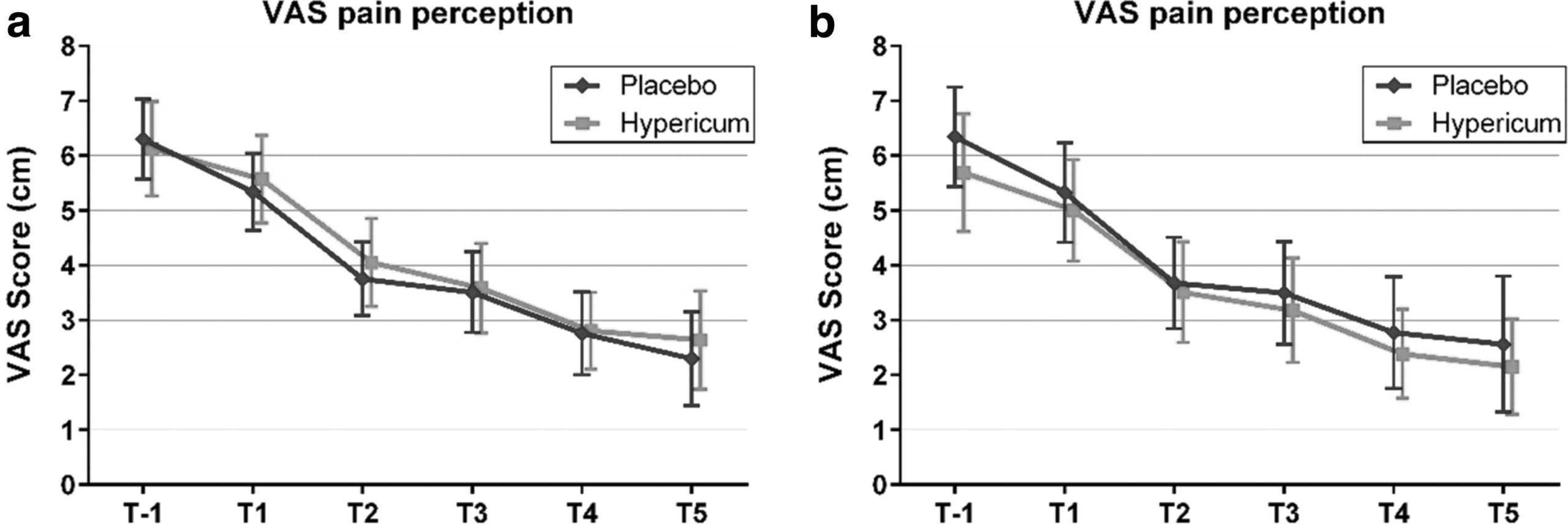
Hypericum perforatum (St John’s wort) is often recommended as a remedy to relieve pain caused by nerve damage. This trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo.
The study was designed as a randomized double-blind, monocentric, placebo-controlled clinical trial with inpatients undergoing surgery for lumbar sequestrectomy. Homeopathic treatment was compared to placebo, both in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The results show that the change in pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
For a number of reasons, this is a remarkably mysterious and quite hilarious study:
- Hypericum is recommended as an analgesic for neuropathic pain.
- According to the ‘like cures like’ axiom of homeopathy, it therefore must increase pain in such situations.
- Yet, the authors of this trial mounted an RCT to see whether it reduces pain.
- Thus they either do not understand homeopathy or wanted to sabotage it.
- As they are well-known pro-homeopathy researchers affiliated with a university that promotes homeopathy (Witten/Herdecke University, Herdecke, Germany), both explanations are highly implausible.
- The facts that the paper was published in a pro-SCAM journal (J Integr Complement Med), and the study was sponsored by the largest German firm of homeopathics (Deutsche Homoeopathische Union) renders all this even more puzzling.
- However, these biases do explain that the authors do their very best to mislead us by including some unwarranted ‘positive’ findings in their overall conclusions.
In the end, none of this matters, because the results of the study reveal that firstly the homeopathic ‘law of similars’ is nonsense, and secondly one homeopathic placebo (i.e. Hypericum C200) produces exactly the same outcomes as another, non-homeopathic placebo.
Our ‘Memorandum Integrative Medicine‘ seems to be causing ripples. A German website that claims to aim at informing consumers objectively posted a rebuttal. Here is my translation (together with comments by myself inserted via reference numbers in brackets and added below):
With drastic words and narrow-mindedness bordering on ideology (1), the Münster Circle, an association of opponents to complementary therapies such as homeopathy (2), takes issue with the treatment concept of integrative medicine in a memorandum (3). By integrative medicine physicians understand the combination of doctor-led medicine and doctor-led complementary medicine to a meaningful total concept with the goal of reducing side effects and to treating patients individually and optimally (4). Integrative medicine focuses primarily on chronic diseases, where conventional acute medicine often reaches its limits (5)In the memorandum of the Münsteraner Kreis, general practitioner Dr. Claudia Novak criticizes integrative medicine as “guru-like self-dramatization” (6) by physicians and therapists, which undermines evidence-based medicine and leads to a deterioration in patient care. She is joined by Prof. Dr. Edzard Ernst, Professor Emeritus of Alternative Medicine, who has changed from Paul to Saul with regard to homeopathy (7) and is leading a veritable media campaign against proponents of treatment procedures that have not been able to prove their evidence in randomized placebo-controlled studies (8). The professor ignores the fact that this involves a large number of drugs that are used as a matter of course in everyday medicine (9) – for example, beta-blockers or other cardiological drugs (10). “Like the devil fears the holy water” (11), the Münsteraner Kreis seems to fear the concept of integrative medicine (12). The vehemence coupled with fear with which they warn against the treatment concept makes one sit up and take notice (13). “As an experienced gynecologist who has successfully worked with biological medicine as an adjunct in his practice for decades, I can only shake my head at such narrow-mindedness”, points out Fred-Holger Ludwig, MD (14). Science does not set limits for itself, but the plurality of methods is immanent (15). “Why doesn’t Prof. Ernst actually give up his professorial title for alternative medicine? That would have to be the logical consequence of its overloud criticism of established treatment concepts from homeopathy to to integrative medicine”, questions Dr. Ludwig (16).
The concept of integrative medicine is about infiltrating alternative procedures into medicine, claim the critics of the concept, without mentioning that many naturopathic procedures have been used for centuries with good results (17) and that healthcare research gives them top marks (18). “Incidentally, the scientists among the representatives of the Münster Circle should know that it is difficult to capture individualized treatment concepts with the standardized procedures of randomized, placebo-controlled studies (19). Anyone who declares the highest level of evidence to be the criterion for approval makes medicine impossible and deprives patients in oncology or with rare diseases, for example, of chances of successful treatment (20). Even there, drugs are used that cannot be based on high evidence, tested in placebo-controlled studies, because the number of cases is too low (21),” notes Dr. Ludwig .
- Ideology? Evidence is not ideology, in my view.
- We are an association of multidisciplinary experts advocating a level playing field with sound evidence in all areas of healthcare.
- The actual memorandum is not linked in this text; does the author not want his readers to form the own opinion?
- In our memorandum, we offer various definitions of integrative medicine (IM), none of which is remotely similar to this one.
- No, IM is usually being promoted in a much wider sense.
- This term does not appear in our memorandum.
- I am not aware that I changed from Paul to Saul with regard to homeopathy; I know that I was led mostly by the evidence.
- I feel flattered but don’t think that my humble work is a ‘media campaign’.
- True, I do not pretend to understand all areas of medicine and tend to be silent in the ones that I lack up-to-date expertise.
- Is he really saying that beta-blockers are not evidence-based?
- The holy water comparison from a homeopath, who arguably makes a living from dishing out ‘holy water’, made me laugh!
- It is most revealing, I think, that he thinks our motivation is fear.
- Splendid!
- FHL is the author of the article, and it is thus charmingly naive that he cites himself in this way
- I somehow doubt that he understands what he is expressing here.
- I find this rather a bizarre idea but I’ll think about it.
- Argumentum ad traditionem.
- Those that get ‘top marks’ belong to evidence-based medicine and not to IM.
- Here the author reveals that he does not understand the RCT methodology and even fails to know the trial evidence on homeopathy – RCTs of individualised homeopathy are possible and have been published (e.g. this one).
- If he really believes this, I fear for his patients.
- Pity that he does not provide an example.
To understand FHL better, it is worth knowing that he claims to treat cancer patients with conventional and homeopathic medicine. He states that this approach reduces side effects – without providing evidence, of course.
Altogether, FHL does not dispute a single fact or argument from our memorandum. In fact, I get the impression that he never actually read it. To me, it feels as though he merely read an article ABOUT the document. In any case, his critique is revealing and important, in my view. It demonstrates that there are no good arguments to defend IM.
So, thank you FHL!
The American Heart Association has issued a statement outlining research on so-called alternative medicine (SCAM) for heart failure. They found some SCAMs that work, some that don’t work, and some that are harmful.
Alternative therapies that may benefit people with heart failure include:
- Omega-3 polyunsaturated fatty acids (PUFA, fish oil) have the strongest evidence among complementary and alternative agents for clinical benefit in people with heart failure and may be used safely, in moderation, in consultation with their health care team. Omega-3 PUFA is associated with a lower risk of developing heart failure and, for those who already have heart failure, improvements in the heart’s pumping ability. There appears to be a dose-related increase in atrial fibrillation (an irregular heart rhythm), so doses of 4 grams or more should be avoided.
- Yoga and Tai Chi, in addition to standard treatment, may help improve exercise tolerance and quality of life and decrease blood pressure.
Meanwhile, some therapies were found to have harmful effects, such as interactions with common heart failure medications and changes in heart contraction, blood pressure, electrolytes and fluid levels:
- While low blood levels of vitamin D are associated with worse heart failure outcomes, supplementation hasn’t shown benefit and may be harmful when taken with heart failure medications such as digoxin, calcium channel blockers and diuretics.
- The herbal supplement blue cohosh, from the root of a flowering plant found in hardwood forests, might cause a fast heart rate called tachycardia, high blood pressure, chest pain and may increase blood glucose. It may also decrease the effect of medications taken to treat high blood pressure and Type 2 diabetes.
- Lily of the valley, the root, stems and flower of which are used in supplements, has long been used in mild heart failure because it contains active chemicals similar to, but less potent than, the heart failure medicine digoxin. It may be harmful when taken with digoxin by causing very low potassium levels, a condition known as hypokalemia. Lily of the valley also may cause irregular heartbeat, confusion and tiredness.
Other therapies have been shown as ineffective based on current data, or have mixed findings, highlighting the importance of patients having a discussion with a health care professional about any non-prescribed treatments:
- Routine thiamine supplementation isn’t shown to be effective for heart failure treatment unless someone has this specific nutrient deficiency.
- Research on alcohol varies, with some data showing that drinking low-to-moderate amounts (1 to 2 drinks per day) is associated with preventing heart failure, while habitual drinking or intake of higher amounts is toxic to the heart muscle and known to contribute to heart failure.
- There are mixed findings about vitamin E. It may have some benefit in reducing the risk of heart failure with preserved ejection fraction, a type of heart failure in which the left ventricle is unable to properly fill with blood between heartbeats. However, it has also been associated with an increased risk of hospitalization in people with heart failure.
- Co-Q10, or coenzyme Q10, is an antioxidant found in small amounts in organ meats, oily fish and soybean oil, and commonly taken as a dietary supplement. Small studies show it may help improve heart failure class, symptoms and quality of life, however, it may interact with blood pressure lowering and anti-clotting medicines. Larger trials are needed to better understand its effects.
- Hawthorn, a flowering shrub, has been shown in some studies to increase exercise tolerance and improve heart failure symptoms such as fatigue. Yet it also has the potential to worsen heart failure, and there is conflicting research about whether it interacts with digoxin.
“Overall, more quality research and well-powered randomized controlled trials are needed to better understand the risks and benefits of complementary and alternative medicine therapies for people with heart failure,” said Chow. “This scientific statement provides critical information to health care professionals who treat people with heart failure and may be used as a resource for consumers about the potential benefit and harm associated with complementary and alternative medicine products.”
____________________
No doubt, this assessment is a laudable attempt to inform patients responsibly. Personally, I am always a bit skeptical about such broad statements. SCAM encompasses some 400 different therapies, and I doubt that these can all be assessed in one single overview.
It is not difficult to find SCAMs that seem to have not been considered. Take this systematic review, for instance. It included 24 RCTs (n = 1314 participants) of 9 different mind-body interventions (MBI) types: Tai Chi (n = 7), yoga (n = 4), relaxation (n = 4), meditation (n = 2), acupuncture (n = 2), biofeedback (n = 2), stress management (n = 1), Pilates (n = 1), and reflexology (n = 1). Most (n = 22, 95.8%) reported small-to-moderate improvements in quality of life (14/14 studies), exercise capacity (8/9 studies), depression (5/5 studies), anxiety and fatigue (4/4 studies), blood pressure (3/5 studies), heart rate (5/6 studies), heart rate variability (7/9 studies), and B-type natriuretic peptide (3/4 studies). Studies ranged from 4 minutes to 26 weeks and group sizes ranged from 8 to 65 patients per study arm.
The authors concluded that, although wide variability exists in the types and delivery, RCTs of MBIs have demonstrated small-to-moderate positive effects on HF patients’ objective and subjective outcomes. Future research should examine the mechanisms by which different MBIs exert their effects.
Or take this systematic review of 38 RCTs of oral TCM remedies. The majority of the included trials were assessed to be of high clinical heterogeneity and poor methodological quality. The main results of the meta-analysis showed improvement in total MLHFQ score when oral Chinese herbal medicine plus conventional medical treatment (CMT) compared with CMT with or without placebo [MD = -5.71 (-7.07, -4.36), p < 0.01].
The authors concluded that there is some encouraging evidence of oral Chinese herbal medicine combined with CMT for the improvement of QoL in CHF patients. However, the evidence remains weak due to the small sample size, high clinical heterogeneity, and poor methodological quality of the included trials. Further, large sample size and well-designed trials are needed.
Don’t get me wrong: I am not saying that TCM remedies are a viable option – in fact, I very much doubt it – but I am saying that attempts to provide comprehensive overviews of all SCAMs are problematic, and that incomplete overviews are just that: incomplete.