cupping
Cupping is a from of so-called alternative medicine (SCAM) that has featured already many times on this blog, e.g.:
- Wet cupping in the management of cervical spondylosis? No!
- The effectiveness of cupping therapy for low back pain
- Cupping: “the propagation of ancient, scientifically unsound techniques that may cause more harm than benefit”
- Cupping therapy for non-specific chronic low back pain
- Cupping for Olympic swimmers. Or: why breaking your shoulder is not necessarily good for writing a successful book
- Wet cupping and dry humour
- Cupping for athletes: rubbish trials, rubbish review, rubbish journal
- The future of cupping: it’s bright, profitable and vacuous
Now a new and interesting paper has been published on the subject
This review aimed to investigate the effectiveness of cupping therapy on low back pain (LBP). Medline, Embase, Scopus and WANFANG databases were searched for relevant cupping RCTs on low back pain articles up to 2023. A complementary search was manually made on 27 September for update screening. Full-text English and Chinese articles on all ethnic adults with LBP of cupping management were included in this study. Studies looking at acute low back pain only were excluded. Two independent reviewers screened and extracted data, with any disagreement resolved through consensus by a third reviewer. The methodological quality of the included studies was evaluated independently by two reviewers using an adapted tool. Change-from-baseline outcomes were treated as continuous variables and calculated according to the Cochrane Handbook. Data were extracted and pooled into the meta-analysis by Review Manager software (version 5.4, Nordic Cochrane Centre).
Eleven trials involving 921 participants were included (6 on dry and 5 on wet cupping). Five studies were assessed as being at low risk of bias, and six studies were of acceptable quality. High-quality evidence demonstrated cupping significantly improves pain at 2-8 weeks endpoint intervention (d=1.09, 95% CI: [0.35-1.83], p = 0.004). There was no continuous pain improvement observed at one month (d=0.11, 95% CI: [-1.02-1.23], p = 0.85) and 3-6 months (d=0.39, 95% CI: [-0.09-0.87], p = 0.11). Dry cupping did not improve pain (d=1.06, 95% CI: [-0.34, 2.45], p = 0.14) compared with wet cupping (d=1.5, 95% CI: [0.39-2.6], p = 0.008) at the endpoint intervention. There was no evidence indicating the association between pain reduction and different types of cupping (p = 0.2). Moderate- to low-quality evidence showed that cupping did not reduce chronic low back pain (d=0.74, 95% CI: [-0.67-2.15], p = 0.30) and non-specific chronic low back pain (d=0.27, 95% CI: [-1.69-2.24], p = 0.78) at the endpoint intervention. Cupping on acupoints showed a significant improvement in pain (d=1.29, 95% CI: [0.63-1.94], p < 0.01) compared with the lower back area (d=0.35, 95% CI: [-0.29-0.99], p = 0.29). A potential association between pain reduction and different cupping locations (p = 0.05) was found. Meta-analysis showed a significant effect on pain improvement compared to medication therapy (n = 8; d=1.8 [95% CI: 1.22 – 2.39], p < 0.001) and usual care (n = 5; d=1.07 [95% CI: 0.21- 1.93], p = 0.01). Two studies demonstrated that cupping significantly mediated sensory and emotional pain immediately, after 24 h, and 2 weeks post-intervention (d= 5.49, 95% CI [4.13-6.84], p < 0.001). Moderate evidence suggested that cupping improved disability at the 1-6 months follow-up (d=0.67, 95% CI: [0.06-1.28], p = 0.03). There was no immediate effect observed at the 2-8 weeks endpoint (d=0.40, 95% CI: [-0.51-1.30], p = 0.39). A high degree of heterogeneity was noted in the subgroup analysis (I2 >50%).
The authors concluded that high- to moderate-quality evidence indicates that cupping significantly improves pain and disability. The effectiveness of cupping for LBP varies based on treatment durations, cupping types, treatment locations, and LBP classifications. Cupping demonstrated a superior and sustained effect on pain reduction compared with medication and usual care. The notable heterogeneity among studies raises concerns about the certainty of these findings. Further research should be designed with a standardized cupping manipulation that specifies treatment sessions, frequency, cupping types, and treatment locations. The actual therapeutic effects of cupping could be confirmed by using objective pain assessments. Studies with at least six- to twelve-month follow-ups are needed to investigate the long-term efficacy of cupping in managing LBP.
A crucial point here is that only 3 of the included studies were ‘patient-blind’, i.e. tried to control for placebo effects by using a sham procedure:
- The first of these used leaking vaccum cups that failed to create sucction. This would therefore not have resulted in the typical circular hematoma. In other words, patients were easily de-blinded.
- The second trial compared two different wet cupping techniques which involved different procedures. This would have been easily identifiable by the patients. In other words, patients were easily de-blinded.
- The third (which showed no effectiveness of cupping) supposedly patient-blind study used a similar method as the first. In other words, patients were easily de-blinded.
In addition, we ought to remember that in no study was it possible to blind the therapists. Thus there is a danger of verbal or non-verbal communications impacting on the outcomes.
In my view, it follows that the effectiveness of cupping is far lass certain than the authors of this paper try to make us believe.
When I still worked as a clinician, I have looked after athletes long enough to know that they go for everything that promises to improve their performance. It is thus hardly surprising that Olympians would try all sorts of so-called alternative medicine (SCAM) regardless of whether the therapy is supported by evidence or not. Skeptics are tempted to dismiss all of SCAM for improving fitness. But is that fair? Is it true that no evidence evists for any of them?
The short answer to this question is NO.
Here I have looked at some of the possibilities and show you some of the Medline-listed papers that seem to support SCAM as a means of improving fitness:
Acupuncture
Ashwagandha
Balneology
Cupping
Ginkgo biloba
Ice
Kinesiology tape
Massage guns
Percussion massage
Sports massage
Tai massage
Vibrational massage
Yoga
Please do not mistake this for anything resembling a systematic review of the evidence; it is merely a list to give you a flavour of what is out there. And please don’t assume that the list is complete; I am sure that there is much more.
Looking at the articles that I found, one could get the impression that there is plenty of good evidence to support SCAM for improving fitness. This, however, would be wrong. The evidence for almost every of the above listed therapies is flimsy to say the least. But – as I stated already at the beginning – in my experience, this will not stop athletes to use them.
Cervical spondylosis is a chronic degenerative process of the cervical spine characterized by pain in neck, degenerative changes in intervertebral disc and osteophyte formation. The present study was aimed at evaluating the effect of wet cupping (Ḥijāma Bish Sharṭ) in the pain management of cervical spondylosis.
This Open, randomized, clinical study was conducted on 44 patients.
- Subjects in the test group (n = 22) received a series of three-staged wet cupping treatment, performed on 0, 7th and 14th day.
- Subjects in the control group (n = 22) received 12 sittings of Transcutaneous Electrical Nerve Stimulation (TENS): 6 sittings per week for two weeks.
The outcomes were assessed with the help of VAS, Neck Disability Index (NDI) and Cervical range of motion.
Intra group comparison in test group from baseline to 21st day were found highly significant (p < 0.001) in terms of VAS, NDI, Flexion, Extension and Left rotation score. While in Right rotation, Left rotation and Left lateral flexion score were found moderately significant (p < 0.01). Statistically significant difference was observed between two groups at 21st day in VAS scale, NDI, and Cervical range of motion score (p < 0.001).
The authors concluded that Ḥijāma Bish Sharṭ was found better in the management of pain due to cervical spondylosis than TENS. It can be concluded that Ḥijāma Bish Sharṭ may a better option for the pain management of cervical spondylosis.
Wet cupping is the use of a vacuum cup applied to the skin which has previously been lacerated. It draws blood and can thus be seen as a form of blood letting. It has been used in various cultures for the treatment of joint pain and many other conditions since antiquity.
The authors point out that, in Unani medicine, it is believed to reduce pain and other symptoms by diverting and evacuating the causative pathological humours (akhlāṭ-e-fasida). Galen (Jalinoos) mentioned wet cupping as a very useful modality in evacuating the thick humours (akhlāṭ-e-Ghaleez) (Nafeesi, 1954; Qamri, 2008). Wet cupping works on the principle of diversion and evacuation of morbid matter (imala wa tanqiya-i-mawād-i-fasida). It opens the pores of the skin, enhances the blood circulation, nourishes the affected area with fresh blood, improves the eliminative function and facilitates the evacuation of morbid matter from the body.
There are several studies of wet cupping, most of which are as flawed as the one above. This new trial has several limitations, e.g.:
- It makes no attempt to control for placebo effects which could well be more prominent for wet cupping than for TENS.
- It did not inhibit the influence of verbal or non-verbal communications between therapists and patients which are likely to influence the results.
- The sample size is far too small, particularly as the study was designed as an equivalence study.
But some might say that my arguments a petty and argue that, regardless of a flimsy study, wet cupping is still worth a try. I would disagree – not because of the flaws of this study, nor the implausibility of the long-obsolete assumptions that underpin the therapy, but because wet cupping is associaated with infections of the skin lacerations which occasionally can be serious.
This systematic review aimed to investigate the effectiveness of cupping therapy on low back pain (LBP). Medline, Embase, Scopus and WANFANG databases were searched for relevant cupping RCTs on low back pain articles up to 2023. A complementary search was manually made on 27 September for update screening. Full-text English and Chinese articles on all ethnic adults with LBP of cupping management were included. Studies looking at acute low back pain only were excluded. Two independent reviewers screened and extracted data, with any disagreement resolved through consensus by a third reviewer. The methodological quality of the included studies was evaluated independently by two reviewers using an adapted tool. Change-from-baseline outcomes were treated as continuous variables and calculated according to the Cochrane Handbook. Data were extracted and pooled into the meta-analysis by Review Manager software (version 5.4, Nordic Cochrane Centre).
Eleven trials involving 921 participants were included. Five studies were assessed as being at low risk of bias, and six studies were of acceptable quality. The findings reveal:
- High-quality evidence demonstrated cupping significantly improves pain at 2-8 weeks endpoint intervention (d=1.09, 95% CI: [0.35-1.83], p=0.004).
- There was no continuous pain improvement observed at one month (d=0.11, 95% CI: [-1.02-1.23], p=0.85) and 3-6 months (d=0.39, 95% CI: [-0.09-0.87], p=0.11).
- Dry cupping did not improve pain (d=1.06, 95% CI: [-0.34, 2.45], p=0.14) compared with wet cupping (d=1.5, 95% CI: [0.39-2.6], p=0.008) at the endpoint intervention.
- There was no evidence indicating the association between pain reduction and different types of cupping (p=0.2).
- Moderate- to low-quality evidence showed that cupping did not reduce chronic low back pain (d=0.74, 95% CI: [-0.67-2.15], p=0.30) and non-specific chronic low back pain (d=0.27, 95% CI: [-1.69-2.24], p=0.78) at the endpoint intervention.
- Cupping on acupoints showed a significant improvement in pain (d=1.29, 95% CI: [0.63-1.94], p<0.01) compared with the lower back area (d=0.35, 95% CI: [-0.29-0.99], p=0.29).
- A potential association between pain reduction and different cupping locations (p=0.05) was found.
- Meta-analysis showed a significant effect on pain improvement compared to medication therapy (n=8; d=1.8 [95% CI: 1.22 – 2.39], p<0.001) and usual care (n=5; d=1.07 [95% CI: 0.21- 1.93], p=0.01).
- Two studies demonstrated that cupping significantly mediated sensory and emotional pain immediately, after 24 hours, and 2 weeks post-intervention (d= 5.49, 95% CI [4.13-6.84], p<0.001).
- Moderate evidence suggested that cupping improved disability at the 1-6 months follow-up (d=0.67, 95% CI: [0.06-1.28], p=0.03).
- There was no immediate effect observed at the 2-8 weeks endpoint (d=0.40, 95% CI: [-0.51-1.30], p=0.39).
- A high degree of heterogeneity was noted in the subgroup analysis (I2 >50%).
The authors concluded that high- to moderate-quality evidence indicates that cupping significantly improves pain and disability. The effectiveness of cupping for LBP varies based on treatment durations, cupping types, treatment locations, and LBP classifications. Cupping demonstrated a superior and sustained effect on pain reduction compared with medication and usual care. The notable heterogeneity among studies raises concerns about the certainty of these findings. Further research should be designed with a standardized cupping manipulation that specifies treatment sessions, frequency, cupping types, and treatment locations. The real therapeutic effects of cupping could be confirmed using a sham device or objective outcome measurements. Studies with at least six- to twelve-month follow-ups are needed to investigate the long-term efficacy of cupping in managing LBP.
Confused?
No need, it’s really quite simple: cupping can, according to this review, be shown to have some short-lasting effect, provided the study is flawed and does not control for placebo effects.
Surprised?
No need! There is hardly a form of so-called alternative medicine (SCAM) that does not have a similarly small effect of back pain, if tested in equally dodgy studies. This is particularly true for those treatments that can act as a theatrical placebo, e.g. acupuncture or chiropractic.
So, should a back pain sufferer try cupping?
If he/she insists, why not? But please don’t use wet cupping (which can do quite a bit of harm). Dry cupping (without injuring the skin) is arguably better (less risk, less expense, possibility of home treatment by your partner) than chiropractic, osteopathy, acupuncture, or many other SCAMs.
My conclusions – as mentioned many times previously – are as follows:
- Most SCAMs help a little with back pain (and similar conditions) because they can have a powerful placebo effect.
- Conventional medicine is also not convincingly effective for back pain.
- If you insist on SCAM, it is best to use one that is relatively harmless and inexpensive.
We have often discussed cupping on this blog, e.g.:
- The ‘WORST PAPER OF 2022 COMPETITION’ entry No 6: “The efficacy and safety of dry cupping in cervical spondylosis with optimization of cup application time – A randomized clinical trial”
- Cupping therapy for non-specific chronic low back pain
- Cupping for Olympic swimmers. Or: why breaking your shoulder is not necessarily good for writing a successful book
- Infant receiving cupping treatment prompts outrage
Yes, generally speaking I have been critical about cupping – not because I don’t like it (I even used the treatment as a young clinician many years ago) but because the evidence tells me to. I was glad to see that the authors of a recent article entitled “Utility of Cupping Therapy in Substance Use Disorder: A Novel Approach or a Bizarre Treatment?” offer even more outspoken words about the therapy. Here are their conclusions:
Established treatment modalities for substance use disorder and its withdrawal symptoms include pharmacotherapy and psychotherapy, but their utilization by the general population remains unsatisfactory. Taboos regarding mental health services and concerns about confidentiality are massive obstacles for patients seeking psychiatric help, and alternative forms of medicine may seem more approachable, even with the associated risks. As displayed in this case, cupping therapy is a traditional therapy with no role in treating polyaddiction and withdrawal symptoms, but it unnecessarily exposes individuals to really uncomfortable and often concealed complications such as bruising, and skin and blood infections, especially when carried out by untrained, incompetent individuals. While one can explore these options in addition to seeking professional mental health care, it is imperative to spread awareness about the roles, scientific soundness, and adverse effects of these alternative health practices. The health promotion and education sectors need reforms to educate the general population, especially the rural population in India, about the dangers of iatrogenesis caused by non-evidence-backed treatments. There needs to be an extensive advertisement of only the most effective and scientific treatment options provided by medical professionals, and the risks of overlooking them in favor of traditional cures propagated by unqualified individuals. With all the scientific advancements in the 21st century ranging from artificial intelligence in healthcare, and robotic surgeries, to extensive clinical trials for novel anti-cancer drugs, we cannot allow the propagation of ancient, scientifically unsound techniques that may cause more harm than benefit to patients.
Why, I am sure you ask yourself, are they so critical? The reason lies in the case they report in the same paper:
A 30-year-old man presented to the psychiatric outpatient department with complaints of nervousness, anxiety, a sense of impending doom, irritability, anger outbursts, headache, and reduced sleep and appetite for the last five days. The patient had a history of daily consumption of 5-10 mg of alprazolam tablets, 200-250 mg of codeine syrup, and about five packets of chewable tobacco over the last seven years; this was a pattern of polyaddiction to a benzodiazepine, opiate, and nicotine. The patient had no history of fever, confusion, or hallucinations. On eliciting the past history, the patient revealed that he went to an alternative medicine practitioner after his family persuaded him to seek help for his substance use disorder. After ceasing the consumption of all three substances for three days, he started developing the symptoms with which he presented to our hospital. He was hesitant to talk about his substance use disorder to medical professionals and concerned about confidentiality, and, hence, went to an alternative medicine practitioner whom he deemed approachable. There he was given wet cupping therapy on the head for four days, which involved the use of rubber pumps to create a suction inside the cups placed on his head. After three to five minutes, the cups were removed and small incisions were made on the cupping sites, following which a second suction caused the oozing out of blood from the incision sites on the scalp (Figure 1). But, this did not improve his symptoms, and hence, he stopped going there two days before coming to our tertiary care hospital.
On examination, the patient had a pulse rate of 76 beats per minute, blood pressure of 128/78 mm Hg, and respiratory rate of 22 per minute. He was well-oriented to time, place, and person. Systemic examination of the cardiovascular system was unremarkable. He denied any other substance use. The skin over his head had distinct cupping marks but no signs of infection or active bleeding, which are some common complications after cupping therapy (Figure 2). On assessment, the patient had a Clinical Opiate Withdrawal Scale (COWS) score of 13 and a Clinical Institute Withdrawal Assessment (CIWA) scale score of 26.
Later, the patient was admitted to the psychiatric ward to manage the withdrawal symptoms, where we initiated pharmacotherapy. Tablet diazepam (20 mg/day), sodium valproate (800 mg/day), tramadol (200 mg/day), thiamine (300 mg/day), paracetamol (500 mg/day) and intravenous fluids were given to the patient. We counseled the patient regarding substance abuse, its harmful effects, and de-addiction. The patient’s symptoms started to improve, and we continued the treatment for four days and discharged him with a COWS score of 4 and a CIWA score of 2. We intended to reassess him after 14 days, but we lost him to follow-up.
I like skeptics; they have taught me a lot, and I am thankful for it.
At the same time, they occasionally irritate me when they comment on so-called alternative medicine (SCAM).
Why? Because, when they comment on SCAM, they are not rarely wrong or at least not quite correct.
I am referring to the typical scenario where a skeptic discusses a form of SCAM and explains that there is no evidence on it. Such statements are almost invariably false. There is evidence on almost all forms of SCAM; it may not be positive but it exists. To make statements to the contrary is demonstrably wrong.
Let’s assume that a skeptic discusses CUPPING (I am referring to an actual video that I recently watched). He explains its history, how it’s done, that there is no plausible mode of action, and that there is NO evidence on it.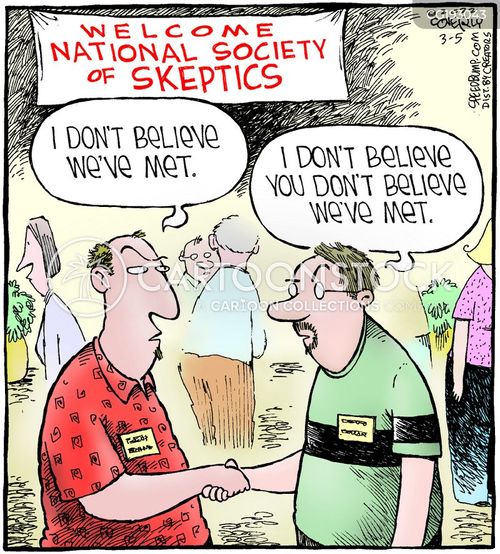
This is not correct!
In fact, there is a substantial body of evidence in terms of clinical trials and even systematic reviews (if you search this blog, you will find quite a bit; if you go on Medline, you’ll find even more). And there is some evidence about cupping’s possible mode of action.
Don’t get me wrong:
- I am not a fan of cupping,
- in fact, cupping is merely an example – I could have chosen almost any other SCAM,
- I am certainly not defending therapists who practice cupping,
- the evidence is far from convincing.
All that I am trying to say is this:
When you comment on a SCAM (or anything else), it is worth checking the evidence. More often than not, you will then find that there is quite a lot of evidence. You might conclude that:
- the evidence is poor quality,
- the evidence is negative,
- the evidence is suspect,
- etc., etc.
So, please comment accordingly. Just saying THERE IS NO EVIDENCE is not just wrong, it is irritating, because it gives the SCAM promoters the occasion to rightly point out that skeptics are just badly informed. And that surely is worth preventing!
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. You will ask what is there to win in this competition? I agree: a competition without a prize is no fun. Therefore, I suggest offering the winner (that is the author of the winning paper) one of my books that best fits his/her subject. I am sure this will over-joy him or her. And how do we identify the winner? I suggest that I continue blogging about nominated papers (I hope to identify about 10 in total), and towards the end of the year, I let my readers decide democratically.
In this spirit of democratic voting, let me suggest to you ENTRY No 6:
This study was to ascertain the efficacy of dry cupping therapy (DCT) and optimal cup application time duration for cervical spondylosis (CS). It was designed as a randomized clinical trial involving 45 participants with clinically diagnosed CS. The eligible subjects were randomly allocated into three groups, each having 15 participants. Each of the three groups, i.e., A, B, and C, received DCT daily for 15 days for 8 min, 10 min, and 12 min, respectively. All the participants were evaluated at the baseline, 7th, and 15th day of the trial using the neck disability index (NDI) as well as the visual analog scale (VAS).
The baseline means ± SD of NDI and VAS scores were significantly reduced in all three groups at the end of the trial. Although all three groups were statistically equal in terms of NDI, group C demonstrated greater efficacy in terms of VAS.
The authors concluded that the per-protocol analysis showed that dry cupping effectively alleviated neck pain across all treatment groups. Although this effect on neck disability index was statistically equal in all three groups, the 12-min protocol was more successful in reducing pain.
Who would design such a study and why?
- The authors claim they wanted to ascertain the efficacy of DCT. A trial is for testing, not ascertaining. And this study does certainly not test for efficacy.
- The groups were too small to generate a meaningful result of what, in fact, was an equivalence study.
- Intra-group changes in symptoms between baseline and time points during treatment are irrelevant in a controlled trial.
- The slightly better results of group C are most likely due to chance or non-specific effects (a longer application of a placebo would generate better outcomes that a shorter one).
- The study participants had cervical spondylosis, yet the conclusion is about neck pain. The two are not identical.
- The title of the paper promises that we learn something about the safety of DCT. Sadly, a trial with just 45 patients has no chance in hell to pick up adverse effects in a reliable way.
- As there is no control group, the study cannot tell us anything about possible specific effects of DCT.
The authors of the study have impressive affiliations:
- Department of Ilaj bil Tadbir, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
- Department of Ilaj bil Tadbir, National Institute of Unani Medicine, Bengaluru, India.
- Department of Moalajat, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
I would have hoped that researchers from national institutions and medical colleges should be able to design a trial that has at least a small chance to produce a meaningful finding. As it turns out, my hope was badly disappointed.
Cupping is a so-called alternative medicine (SCAM) that has been around for millennia in many cultures. We have discussed it repeatedly on this blog (see, for instance, here, here, and here). This new study tested the effects of dry cupping on pain intensity, physical function, functional mobility, trunk range of motion, perceived overall effect, quality of life, psychological symptoms, and medication use in individuals with chronic non-specific low back pain.
Ninety participants with chronic non-specific low back pain were randomized. The experimental group (n = 45) received dry cupping therapy, with cups bilaterally positioned parallel to the L1 to L5 vertebrae. The control group (n = 45) received sham cupping therapy. The interventions were applied once a week for 8 weeks.
Participants were assessed before and after the first treatment session, and after 4 and 8 weeks of intervention. The primary outcome was pain intensity, measured with the numerical pain scale at rest, during fast walking, and during trunk flexion. Secondary outcomes were physical function, functional mobility, trunk range of motion, perceived overall effect, quality of life, psychological symptoms, and medication use.
On a 0-to-10 scale, the between-group difference in pain severity at rest was negligible: MD 0.0 (95% CI -0.9 to 1.0) immediately after the first treatment, 0.4 (95% CI -0.5 to 1.5) at 4 weeks and 0.6 (95% CI -0.4 to 1.6) at 8 weeks. Similar negligible effects were observed on pain severity during fast walking or trunk flexion. Negligible effects were also found on physical function, functional mobility, and perceived overall effect, where mean estimates and their confidence intervals all excluded worthwhile effects. No worthwhile benefits could be confirmed for any of the remaining secondary outcomes.
The authors concluded that dry cupping therapy was not superior to sham cupping for improving pain, physical function, mobility, quality of life, psychological symptoms or medication use in people with non-specific chronic low back pain.
These results will not surprise many of us; they certainly don’t baffle me. What I found interesting in this paper was the concept of sham cupping therapy. How did they do it? Here is their explanation:
For the experimental group, a manual suction pump and four acrylic cups size one (internal diameter = 4.5 cm) were used for the interventions. The cups were applied to the lower back, parallel to L1 to L5 vertebrae, with a 3-cm distance between them, bilaterally. The dry cupping application consisted of a negative pressure of 300 millibars (two suctions in the manual suction pump) sustained for 10 minutes once a week for 8 weeks.
In the control group, the exact same procedures were used except that the cups were prepared with small holes < 2 mm in diameter to release the negative pressure in approximately 3 seconds. Double-sided adhesive tape was applied to the border of the cups in order to keep them in contact with the participants’ skin.
So, sham-controlled trials of cupping are doable. Future trialists might now consider the inclusion of testing the success of patient-blinding when conducting trials of cupping therapy.
Bloodletting therapy (BLT) has been widely used for centuries until it was discovered that it is not merely useless for almost all diseases but also potentially harmful. Yet in so-called alternative medicine (SCAM) BLT is still sometimes employed, for instance, to relieve acute gouty arthritis (AGA). This systematic review aimed to evaluate the feasibility and safety of BLT in treating AGA.
Seven databases were searched from the date of establishment to July 31, 2020, irrespective of the publication source and language. BLT included fire needle, syringe, three-edged needle, and bloodletting followed by cupping. The included articles were evaluated for bias risk by using the Cochrane risk of bias assessment tool.
Twelve studies involving 894 participants were included in the final analysis. A meta-analysis suggested that BLT was highly effective in relieving pain (MD = -1.13, 95% CI [-1.60, -0.66], P < 0.00001), with marked alterations in the total effective (RR = 1.09, 95% [1.05, 1.14], P < 0.0001) and curative rates (RR = 1.37, 95%CI [1.17, 1.59], P < 0.0001). In addition, BLT could dramatically reduce serum C-reactive protein (CRP) level (MD = -3.64, 95%CI [-6.72, -0.55], P = 0.02). Both BLT and Western medicine (WM) produced comparable decreases in uric acid (MD = -18.72, 95%CI [-38.24, 0.81], P = 0.06) and erythrocyte sedimentation rate (ESR) levels (MD = -3.01, 95%CI [-6.89, 0.86], P = 0.13). Lastly, we demonstrated that BLT was safer than WM in treating AGA (RR = 0.36, 95%CI [0.13, 0.97], P = 0.04).
The authors concluded that BLT is effective in alleviating pain and decreasing CRP level in AGA patients with a lower risk of evoking adverse reactions.
This conclusion is optimistic, to say the least. There are several reasons for this statement:
- All the primary studies came from China (and we have often discussed that such trials need to be taken with a pinch of salt).
- All the studies had major methodological flaws.
- There was considerable heterogeneity between the studies.
- The treatments employed were very different from study to study.
- Half of all studies failed to mention adverse effects and thus violate medical ethics.
Since Gwyneth Paltrow, as well as US Olympic swimmers, were publicly sporting their cupping marks, cupping has repeatedly occupied the pages of this blog. Now, cupping is in the news yet again. It has been reported that an image of a self-proclaimed ‘cupping’ expert performing treatment on a newborn baby has caused a major outcry. The photo shows a three-month-old baby’s skin on its back being sucked into a cup with the skin deformed and bright red.

The man, known as Mustafa, who refers to himself as an ‘expert’ at a ’cupping centre’ in the city of Istanbul, recently shared the images on social media where he was apparently treating the baby for ‘gas’. “We provide cupping for everyone from three-month-old babies to 70-year-olds. We do it since it is an Islamic tradition and we believe that everyone should take part in it,“ Mustafa said. “I am not a swindler. I do not demand money from people. They give as much as they choose.”
Child and adolescent psychiatrist associate, Dr Veysi Ceri, slammed the parents who allowed the procedure to be performed on their children. “Children cannot be left at the mercy of their parents,” Dr Ceri said. “Cupping is something that is not based on scientific evidence and children are physically harmed from it.”
On social media, people expressed their fury, labelling the practice as “questionable”. One commenter wrote: “Are these people crazy? They don’t read or learn anything.” But there were also those who shared their positive experiences. “I congratulate the family who had cupping performed on their baby,” one person wrote. “I also do cupping regularly and I haven’t had a headache in years. I do not take any medicine either. It is also beneficial for children to have cupping.“
___________________________
So, is there any reliable evidence about dry cupping for children?
Is it demonstrably effective for any paediatric condition?
Is it harmful?
Believe it or not, there has been at least one clinical trial of dry cupping as a treatment of constipation in children:
One hundred and twenty children (4-18 years old) diagnosed as functional constipation according to ROME III criteria were assigned to receive a traditional dry cupping protocol on the abdominal wall for 8 minutes every other day or standard laxative therapy (Polyethylene glycol (PEG) 40% solution without electrolyte), 0.4 g/kg once daily) for 4 weeks, in an open label randomized controlled clinical trial using a parallel design with a 1:1 allocation ratio. Patients were evaluated prior to and following 2, 4, 8 and 12 weeks of the intervention commencement in terms of the ROME III criteria for functional constipation.
Results: There were no significant differences between the two arms regarding demographic and clinical basic characteristics. After two weeks of the intervention, there was a significant better result in most of the items of ROME III criteria of patients in PEG group. In contrast, after four weeks of the intervention, the result was significantly better in the cupping group. There was no significant difference in the number of patients with constipation after 4 and 8 weeks of the follow-up period.
Conclusion: This study showed that dry cupping of the abdominal wall, as a traditional manipulative therapy, can be as effective as standard laxative therapy in children with functional constipation.
This study is squarely negative, yet the conclusions are clearly positive. I have stopped being amazed by such contradictions. After all, we are dealing with so-called alternative medicine (SCAM)!
For what it’s worth, here is our 2011 overview of all systematic reviews of cupping:
Several systematic reviews (SRs) have assessed the effectiveness of cupping for a range of conditions. Our aim was to provide a critical evaluation and summary of these data. Electronic searches were conducted to locate all SRs concerning cupping for any condition. Data were extracted by two authors according to predefined criteria. Five SRs met our inclusion criteria, which related to the following conditions: pain conditions, stroke rehabilitation, hypertension, and herpes zoster. The numbers of studies included in each SR were small. Relatively clear evidence emerged only for one indication, that cupping may be effective for reducing pain. Based on evidence from the currently available SRs, the effectiveness of cupping has been demonstrated only as a treatment for pain, and even for this indication doubts remain.
And here is our 2011 SR of cupping as a treatment of pain:
The objective of this study was to assess the evidence for or against the effectiveness of cupping as a treatment option for pain. Fourteen databases were searched. Randomized clinical trials (RCTs) testing cupping in patients with pain of any origin were considered. Trials using cupping with or without drawing blood were included, while trials comparing cupping with other treatments of unproven efficacy were excluded. Trials with cupping as concomitant treatment together with other treatments of unproven efficacy were excluded. Trials were also excluded if pain was not a central symptom of the condition. The selection of studies, data extraction and validation were performed independently by three reviewers. Seven RCTs met all the inclusion criteria. Two RCTs suggested significant pain reduction for cupping in low back pain compared with usual care (P < .01) and analgesia (P < .001). Another two RCTs also showed positive effects of cupping in cancer pain (P < .05) and trigeminal neuralgia (P < .01) compared with anticancer drugs and analgesics, respectively. Two RCTs reported favorable effects of cupping on pain in brachialgia compared with usual care (P = .03) or heat pad (P < .001). The other RCT failed to show superior effects of cupping on pain in herpes zoster compared with anti-viral medication (P = .065). Currently there are few RCTs testing the effectiveness of cupping in the management of pain. Most of the existing trials are of poor quality. Therefore, more rigorous studies are required before the effectiveness of cupping for the treatment of pain can be determined.
The included trials frequently were silent about adverse effects. Others reported no adverse effects and one mentioned three cases of vaso-vagal shock. None of the studies was on children.
So, here are my answers to the questions above:
- Is there any reliable evidence about dry cupping for children? No
- Is it demonstrably effective for any paediatric condition? No
- Is it harmful? Probably not that much (other than undermining common sense and rationality).


