critical thinking
Yesterday I received an electronic Christmas card from two homeopathic institutions called ‘Homeopathic Associates and The Homeopathic College’. It read: WISHING YOU THE BEST OF HEALTH AND HAPPINESS FOR THE NEW YEAR!
Naturally I was puzzled, particularly since I had no recollection of ever having been in contact with them. The card was signed by Manfred Mueller, MA, DHM, RSHom(NA), CCH, and I decided to find out more about this man. It turns out that Manfred Mueller developed The Mueller Method or “Extra-Strength Homeopathy” to meet today’s complex chronic conditions, drug induced disorders, vaccine injuries, toxic overload, radiation-induced health problems, cancers, etc.
Now, this sounds interesting, I thought, and read on. Just a few clicks further, Mueller offers his wisdom on homeopathic cancer treatments in a lengthy article entitled ‘Is Homeopathy an Effective Cancer Treatment?‘
According to Mueller, the answer to his question is a clear yes. I will spare you the torture of reading the entire paper (if you have masochistic tendencies, you can read it via the link I provided above); instead, I will just copy Mueller’s conclusion:
START OF QUAOTE
Laboratory studies in vitro and in vivo show that homeopathic drugs, in addition to having the capacity to reduce the size of tumors and to induce apoptosis, can induce protective and restorative effects. Additionally homeopathic treatment has shown effects when used as a complementary therapy for the effects of conventional cancer treatment. This confirms observations from our own clinical experience as well as that of others that when suitable remedies are selected according to individual indications as well as according to pathology and to cell-line indications and administered in the appropriate doses according to the standard principles of homeopathic posology, homeopathic treatment of cancer can be a highly effective therapy for all kinds of cancers and leukemia as well as for the harmful side effects of conventional treatment. More research is needed to corroborate these clinical observations.
Homeopathy over almost two decades of its existence has developed more than four hundred remedies for cancer treatment. Only a small fraction have been subjected to scientific study so far. More homeopathic remedies need to be studied to establish if they have any significant action in cancer. Undoubtedly the next big step in homeopathic cancer research must be multiple comprehensive double-blinded, placebo-controlled, randomized clinical trials. To assess the effect of homeopathic treatment in clinical settings, volunteer adult patients who prefer to try homeopathic treatment instead of conventional therapy could be recruited, especially in cases for which no conventional therapy has been shown to be effective.
Many of the researchers conducting studies — cited here but not discussed — on the growing interest in homeopathic cancer treatment have observed that patients are driving the demand for access to homeopathic and other alternative modes of cancer treatment. So long as existing cancer treatment is fraught with danger and low efficacy, it is urgent that the research on and the provision of quality homeopathic cancer treatment be made available for those who wish to try it.
END OF QUOTE
Amazing! What could be more wrong than this?
But it’s the season of joy and love; so, let’s not go into the embarrassing details of this article. Instead, I feel like returning the curtesy of Mr Mueller’s Christmas card. Therefore, I have decided to post this open ‘Christmas card’ to him:
Dear Mr Mueller,
thank you for your card, the good wishes, and the links you provided to your websites, articles, etc. I only read the one on cancer but was impressed. It is remarkably misguided, unethical and dangerous. Crucially, it has the potential to shorten the lives of many desperate patients. I therefore urge you to desist making your opinions public or from applying them in your clinical practice. I say this not merely because I am concerned about the patients that have the misfortune to fall into your hands, but also to prevent you from getting into trouble for immoral, unethical or unlawful behaviour.
In this spirit, I wish you happiness for the New Year.
Edzard Ernst
The fact that much of chiropractic might be bogus has frequently been discussed on this blog. A recent press-release provided me with more evidence for this notion. It proudly announced a new book entitled “Beyond the Back: The Chiropractic Alternative For Conditions Beyond Back Pain”
The text claimed that shortly after the launch, the book hit #1 on the Amazon.com best seller list out of all Chiropractor books and also reached #1 for the category of Holistic Medicine.
 When I checked (22/12/2016), I was not able to confirm this statement: #47 in Kindle Store > Kindle eBooks > Medical eBooks > Alternative & Holistic > Holistic Medicine, #58 in Books > Medical Books > Allied Health Professions > Chiropractic. But let’s not be petty; let’s rather see what the book has to offer.
When I checked (22/12/2016), I was not able to confirm this statement: #47 in Kindle Store > Kindle eBooks > Medical eBooks > Alternative & Holistic > Holistic Medicine, #58 in Books > Medical Books > Allied Health Professions > Chiropractic. But let’s not be petty; let’s rather see what the book has to offer.
‘Beyond the Back’ focuses on how Chiropractic care can do so much more than just alleviate back pain, the press-release says. From avoiding knee surgery to resolving athletic injuries, chiropractic care allegedly is a 100% natural health solution for a wide variety of conditions… In fact, in some cases, chiropractors can help their patients get off medications entirely and even avoid surgery, the press-release continues.
In the book itself, the authors claim that chiropractic is effective for a multitude of conditions, including asthma and colic (in fact, the authors try to give the impression that chiropractic is a veritable panacea), and that there is sound evidence for all these indications from hundreds, if not thousands of studies. The authors make it very clear – even on the book cover – that chiropractic is not an adjunct to conventional healthcare but an alternative to it; an idea, of course, that goes back to the founding fathers of chiropractic. As if this were not enough, the book also promotes diagnostic techniques such as applied kinesiology.
Some commentators on this blog have argued that the chiropractic profession is in the midst of giving up much of the nonsense upon it was originally based and to which it has clung on for more than hundred years. This book, written by 9 US authors of the new generation of chiropractors, seems to demonstrate the opposite.
On Amazon, the book currently has one single customer review: Value information and an easy read! I am a strong believer of chiropractic and this makes it easy for me to share this info with my friends !
This comment is apt because it makes clear that chiropractic is a belief system. We must not expect rational thoughts or facts from what, in effect, is a religion for many. I can understand this in a way: belief can be a cosy shelter from the truth; it does not require much thinking; it hardly needs any learning, no changing of minds, etc. However, belief can never be a basis for good healthcare. In my view, ‘Beyond The Back’ provides a perfect example of that.
This meta-analysis was performed “to ascertain the effectiveness of oral aloe vera consumption on the reduction of fasting blood glucose (FBG) and hemoglobin A1c (HbA1c).”
PubMed, CINAHL, Natural Medicines Comprehensive Database, and Natural Standard databases were searched. The searches were limited to clinical trials or observational studies conducted in humans and published in English. Studies of aloe vera’s effect on FBG, HbA1c, homeostasis model assessment-estimated insulin resistance (HOMA-IR), fasting serum insulin, fructosamine, and oral glucose tolerance test (OGTT) in prediabetic and diabetic populations were examined.
Nine studies were included in the FBG parameter (n = 283); 5 of these studies included HbA1c data (n = 89). Aloe vera decreased FBG by 46.6 mg/dL (p < 0.0001) and HbA1c by 1.05% (p = 0.004). Significant reductions of both endpoints were maintained in all subgroup analyses. Additionally, the data suggested that patients with an FBG ≥200 mg/dL may see a greater benefit. A mean FBG reduction of 109.9 mg/dL was observed in this population (p ≤ 0.0001). There was evidence of publication bias with FBG but not with HbA1c.
The authors concluded that the results of this meta-analysis support the use of oral aloe vera for significantly reducing both FBG (46.6 mg/dL) and HbA1c (1.05%) in prediabetic and diabetic patients. However, given the current overall quality and relative scarcity of data, further clinical studies that are more robust and better controlled are warranted to confirm and further explore these findings.
Oh no, the results do not support the use of aloe vera at all!!
Why?
Because this ‘meta-analysis’ is of unacceptably poor quality. Here are just some of the flaws that render it totally useless, particularly for issuing advice such as above:
- The authors included uncontrolled observational studies which make no attempt to control for non-specific effects.
- In several studies, the use of concomitant anti-diabetic medications was allowed; therefore it is not possible to establish cause and effect by aloe vera.
- The search strategy was woefully inadequate; for instance non-English publications were not considered.
- There was no assessment of the scientific rigor of the included studies; this totally invalidates the reliably of the conclusions.
- The included studies used preparations of widely different aloe vera preparations, and there is no way of knowing the does of the active ingredients.
Diabetes is a serious condition that affects millions worldwide. If some of these patients are sufficiently gullible to follow the conclusions of this paper, they might be dead within a matter of days. This makes this article one of the most dangerous papers that I have seen in the ‘peer-reviewed’ literature of alternative medicine.
Who publishes such utter and irresponsible rubbish?
You may well ask.
The journal has been discussed on this blog before for the junk that regularly appears in its pages, and so has its editor in chief. The authors (and the reviewers) are not known to me, but one thing is for sure: they don’t know the first thing about conducting a decent systematic review/meta-analysis.
The boom of alternative medicine in the US – and consequently in the rest of the developed world – is intimately connected with a NHI centre now called NCCIH (National Center for Complementary and Integrative Health). It was founded in the early 1990s because some politicians were bent on promoting quackery. Initially the institution had modest funding but, after more political interference, it had ample cash to pursue all sorts of activities, including sponsoring research into alternative therapies at US universities. A most interesting video summarising the history of the NCCIH can be seen here.
No other institution in the world had more funds for research into alternative medicine than the NCCIH, and it soon became the envy of alt med researchers globally. I have been invited by the NCCHI on several occasions and invariably was impressed by their apparent affluence. While we Europeans usually had to do our research on a shoe-string, our American colleagues seemed to be ‘rolling in it’.
I was often far less impressed with the research they sponsored. Not only it was invariably eye-wateringly expensive, but also its quality seemed often dismal. Sometimes, I even got the impression that research was used as a means of mainstreaming quackery for the unsuspecting American – and consequently world-wide – public.
An example of this mainstreaming is an article in JAMA published yesterday. Here is a short but telling excerpt:
Researchers led by Richard L. Nahin, PhD, MPH, lead epidemiologist at the NIH’s National Center for Complementary and Integrative Health (NCCIH), examined efficacy and safety evidence in 105 randomized controlled trials (RCTs) conducted between January 1966 and March 2016. The review—geared toward primary care physicians as part of the journal’s Symposium on Pain Medicine—focused on popular complementary approaches to common pain conditions.
Unlike a typical systematic review that assigns quality values to the studies, the investigators conducted a narrative review, in which they simply looked at the number of positive and negative trials. “If there were more positives than negatives then we generally felt the approach had some value,” Nahin explained. “If there were more negatives, we generally felt the approach had less value.” Trials that were conducted outside of the United States were excluded from the review.
Based on a “preponderance” of positive vs negative trials, complementary approaches that may offer pain relief include acupuncture and yoga for back pain; acupuncture and tai chi for osteoarthritis of the knee; massage therapy for neck pain; and relaxation techniques for severe headaches and migraine. Several other techniques had weaker evidence, according to the qualitative assessments, for specific pain conditions (see “Selected Complementary Health Approaches for Pain”). The treatments were generally safe, with no serious adverse events reported.
To me, this looks that NCCIH has now managed to persuade even the editors of JAMA to white-wash their dodgy science. The review referred to here is a paper we discussed some time ago on this blog. I then stated about it the following:
Reading the article carefully, it is impossible not to get troubled. Here are a few points that concern me most:
- the safety of a therapy cannot be evaluated on the basis of data from RCTs (particularly as it has been shown repeatedly that trials of alternative therapies often fail to report adverse effects); much larger samples are needed for that; any statements about safety in the aims of the paper are therefore misplaced;
- the authors talk about efficacy but seem to mean effectiveness;
- the authors only included RCTs from the US which must result in a skewed and incomplete picture;
- the article is from the National Center for Complementary and Integrative Health which is part of the NIH but which has been criticised repeatedly for being biased in favour of alternative medicine;
- not all of the authors seem to be NIH staff, and I cannot find a declaration of conflicts of interest;
- the discussion of the paper totally lacks any critical thinking;
- there is no assessment of the quality of the trials included in this review.
My last point is by far the most important. A summary of this nature that fails to take into account the numerous limitations of the primary data is, I think, as good as worthless. As I know most of the RCTs included in the analyses, I predict that the overall picture generated by this review would have changed substantially, if the risks of bias in the primary studies had been accounted for.
I find it puzzling that the ‘lead epidemiologist at the NIH’s National Center for Complementary and Integrative Health’ would publish such dubious research. Why does he do it? If you have watched the video mentioned above, you are inclined to think that it might be because of political interference.
However, I suggest another, in a way much more damming reason or contributing factor: the NCCIH has so long indulged in such poor science that even its top people have forgotten what good science looks like. I know this is a bold hypothesis; so, let me try to support it with some data.
Several years ago, my team together with several other researches have looked at the NCCIH-sponsored research systematically according to 4 different subject areas. Here are the conclusions of our articles reporting the findings:
ACUPUNCTURE
Seven RCTs had a low risk of bias. Numerous methodological shortcomings were identified. Many NCCAM-funded RCTs of acupuncture have important limitations. These findings might improve future studies of acupuncture and could be considered in the ongoing debate regarding NCCAM-funding. [Focus on Alternative and Complementary Therapies Volume 17(1) March 2012 15–21]
HERBAL MEDICINE
This independent assessment revealed a plethora of serious concerns related to NCCAM studies of herbal medicine. [Perfusion 2011; 24: 89-102]
ENERGY MEDICINE
In conclusion, the NCCAM-funded RCTs of energy medicine are prime examples of misguided investments into research. In our opinion, NCCAM should not be funding poor-quality studies of implausible practices. The impact of any future studies of energy medicine would be negligible or even detrimental. [Focus on Alternative and Complementary Therapies Volume 16(2) June 2011 106–109 ]
CHIROPRACTIC
In conclusion, our review demonstrates that several RCTs of chiropractic have been funded by the NCCAM. It raises numerous concerns in relation to these studies; in particular, it suggests that many of these studies are seriously flawed. [https://www.ncbi.nlm.nih.gov/pubmed/21207089]
I think I can rest my case and urge you to watch the video mentioned above.
Alternative medicine suffers from what might be called ‘survey overload’: there are far too much such investigations and most of them are of deplorably poor quality producing nothing of value except some promotion for alternative medicine. Yet, every now and then, one finds a paper that is worth reading, and I am happy to say that this survey (even though it has several methodological shortcomings) belongs in this category.
This cross-sectional assessment of the views of general practitioners towards chiropractors and osteopaths was funded by the Department of Chiropractic at Macquarie University. It was designed as a quantitative descriptive study using an anonymous online survey that included closed and open-ended questions with opportunities provided for free text. The target population was Australian general practitioners. Inclusion criteria included current medical registration, membership of the Royal Australian College of General Practitioners and currently practicing as a general practitioner in Australia. The data being reported here were collected between May and December, 2014.
There were 630 respondents to the online survey during this period representing a response rate of 2.6 %. Results were not uniform for the two professions. More general practitioners believed chiropractic education was not evidence-based compared to osteopathic education (70 % and 50 % respectively), while the scope of practice was viewed as similar for both professions. A majority of general practitioners had never referred a patient to either profession (chiropractic: 60 %; osteopathy: 66 %) and indicated that they would not want to co-manage patients with either profession. Approximately two-thirds of general practitioners were not interested in learning more about their education (chiropractors: 68 %; osteopaths: 63 %).
The authors concluded that this study provides an indication of the current views of Australian general practitioners towards chiropractors and osteopaths. The findings suggest that attitudes may have become less favourable with a growing intolerance towards both professions. If confirmed, this has the potential to impact health service provision. The results from this cross-sectional study suggest that obtaining representative general practitioner views using online surveys is difficult and another approach is needed to supplement or replace the current recruitment strategy.
The authors do not speculate on the reasons why the attitudes of general practitioners towards chiropractic and osteopathy might have become more critical. Therefore I decided to offer a few possibilities here. The more negative views could be due to:
- better education of general practitioners,
- tightening of healthcare budgets,
- recent ‘bad press’ and loss of reputation (for instance, the BCA’s libel action against Simon Singh),
- the work of sceptics in informing the public about the numerous bogus claims made by osteopaths and chiropractors,
- the plethora of overtly bogus claims which nevertheless continue to be made by these practitioners on a daily basis,
- a more general realisation that these therapies can cause very serious harm,
- a mixture of the above factors.
Whatever the reasons are, the finding that there now seems to be a growing scepticism (in Australia, but hopefully elsewhere as well) about the value of chiropractic and osteopathy is something that cheers me up no end.
Yes, this post might come as a surprise to some.
And no, I am not changing sides in the debate in the debate about homeopathy.
But I have long felt that, when sceptics criticise homeopathy, they often wrong-foot themselves by using arguments which are not entirely correct.
Here I want to list seven of them (more details can be found here):
Homeopathy is one single, well-defined entity
During the last 200 years, many different variations of Hahnemann’s classical homeopathy have emerged, for instance clinical homeopathy, complex homeopathy and isopathy. Strictly speaking, they should be differentiated, and it is not correct to generalise across all of them.
In the 200-years’ history of homeopathy, homeopaths have done no good at all
Hahnemann and his followers can be credited with considerable achievements. Foremost, they realised that, 200 years ago, most of the conventional treatments in common use were not just useless but often outright dangerous. Their criticism of ‘heroic medicine’ helped to initiate crucial reforms and to improve health care for the benefit of millions.
No theories to explain how homeopathy might work have ever been put forward
There are several theories which might go some way in explaining how homeopathy works. But all of them are currently just theories, and none provides a full explanation as to the mechanism of action of highly diluted remedies. Yet, to claim that homeopathy is totally implausible might be a counter-productive exaggeration.
There is nothing in it
Many sceptics claim that homeopathic remedies are devoid of active ingredients. Yet, not all homeopathic remedies are highly diluted; some can contain pharmacologically active compounds for affecting human health. These preparations cannot therefore be classified as implausible.
There is no credible evidence at all that might support homeopathy
Several well-conducted clinical studies of homeopathy with positive results have been published. It is therefore not true to claim that there is no good trial evidence at all to support homeopathy. The much better point sceptics should make is that the totality of the reliable evidence fails to show that highly dilute homeopathic remedies are more effective than placebos.
Homeopaths aim at deceiving their patients because they have nothing to offer to them
It would be wrong to claim that all homeopaths aim at deceiving their patients, and it would be misleading to say that homeopaths have nothing to offer to their patients. Many patients of homeopaths primarily treasure the long, compassionate consultations that homeopaths have with their patients and see the homeopathic remedy as secondary. Seen from this perspective, homeopaths do offer something that many patients value highly.
Patients who use homeopathy must be stupid
It would be arrogant, insulting and counter-productive to claim that everyone who uses homeopathy is stupid. Patients consult homeopaths mostly because they have needs which are not met by conventional medicine but which they feel taken care of by homeopathy. Seen from this perspective, the current popularity of homeopathy in some countries is a poignant criticism of conventional medicine. To dismiss it a stupidity means missing a chance to learn an important lesson and to improve mainstream health care.
I know, my stance here can easily get misunderstood (see for instance some of the comments here). But please don’t get me wrong, I am not saying that homeopathy is a useful therapy, nor am I suggesting that we should not criticise it or stop public funding for it. All that I am trying to convey here is this: when we criticise homeopathy, we ought to make sure our arguments are factually correct – if not, we only give ammunition to our opponents.
In a nutshell: I don’t wish to undermine our arguments, but want them to be more effective.
The Scotsman reported that David Tredinnick, the somewhat feeble-minded Tory MP for Bosworth, has been at it again. Apparently he said that many of his constituents are only alive today because they have been treated with alternative medicine.
Tredennick recently urged ministers to spend more NHS money on alternative therapies such as homeopathy and acupuncture to treat patients. It seems to me that, for him and other quackery promoters, evidence and science are issues beyond comprehension. Mr Tredinnick also disclosed the fact that he received acupuncture at a Chinese medical clinic just before the Commons debate on cancer strategy – a regular treatment he credits with keeping him healthy.
Tredennick told his fellow MPs: “I was talking there to practitioners about what they are able to do for cancer patients, and there is actually a very long list of types of cancer that can be treated using traditional Chinese herbal medicine.“ One, cervical cancer, two, non-Hodkins lymphoma, three, HIV, four, colon cancer, five… six, breast cancer, seven, prostate cancer. And so the list goes on. “I have in my constituency several constituents who I believe are alive today because they have used Chinese medicine.“ And the reason for that is what it does is it strengthens your system, and it strengthens the immune system, and it is very effective after cancer treatment. It deals with particular symptoms.”
This is by no means the first outburst of quackery-promotion by the Right Honourable Gentleman. I have a whole selection of quotes from him which I sometimes use for amusing my audience during public lectures. Because amusing he is; Tredennick seems to be utterly devoid of rational thought when it comes to the subject of alternative medicine, and often his statements make for comedy gold. This time, however, he might be sailing closer to the wind than he perhaps realizes: Under English law, it is an offence to claim that any treatment can cure cancer, I believe.
We all had to learn to laugh about unethical and dangerous nonsense the ‘Tredennicks of this world’ regularly claim about alternative medicine. Laughing is the only solution for coping with such idiocy, I am afrid. If we don’t laugh, we have to consider taking it seriously – and this is a truly frightening prospect, particularly considering that this guy actually sits in parliament and has the power to influence our lives.
This randomized, double-blind study evaluated the efficacy of a homeopathic treatment in preventing excessive weight gain during pregnancy in overweight or obese women who were suspected of having a common mental disorder. For the homeopathic group (n=62), 9 homeopathic remedies were pre-selected: (1) Pulsatilla nigricans, (2) Sepia succus, (3) Lycopodium clavatum, (4) sulphur, (5) Lachesis trigonocephalus, (6) Nux vomica, (7) Calcarea carbonica, (8) phosphorus; and (9) Conium maculatum. From those 9 drugs, one was prioritized for administration for each participant. After the first appointment, a re-selection or selection of a new, more appropriate drug occurred, using the list of preselected drugs. The dosage was 6 drops orally 2 ×/day, in the morning and at night, on 4 consecutive days each week, with an interval of 3 d between doses, up until the next appointment medical appointment. The control group (n=72) took placebos. Both groups also received a diet orientation.
Weight change during pregnancy was defined as the difference between the body mass index (BMI) at the initial evaluation and that recorded at the final evaluation, adjusted for 40 weeks of gestation. In addition, the APGAR index in the newborn (a measure of the health of the baby) was evaluated. The mean variation between baseline BMI and BMI at week 40 of gestation was +4.95 kg/m2 in the control group and +5.05 kg/m2 in the homeopathy group. The difference between the two groups was not significant. APGAR 10 at 5 min (59.6% in the homeopathy group and 36.4% in the control group) was statistically significant (P = .016).
The authors concluded that homeopathy does not appear to prevent excessive body mass gain in pregnant women who are overweight or obese and suspected of having a common mental disorder. Homeopathy did not change the APGAR score to modified clinical attention at delivery room. However, the evidence observed at APGAR 10 at minute 5 suggests that homeopathy had a modulating effect on the vitality of newborns, warranting further studies designed to investigate it.
I have seen many odd studies in my time, but this must be one of the oddest?
- What is the rationale for assuming that homeopathy might affect body weight?
- Why take pregnant women with a weight problem who were suspected of having a common mental disorder?
- Why try to turn a clearly negative result into a finding that is (at least partly) positive?
The last point seems the most important one to me. The primary outcome measure of this study (weight gain) was clearly defined and was not affected by the therapy. Yet the authors feel it justified to add to their conclusions that homeopathy had a modulating effect on the vitality of newborns (almost certainly nothing but a chance finding).
Are they for real?
I suppose they are: they are real pseudo-scientific promoters of quackery!
Meniscus-injuries are common and there is no consensus as to how best treat them. Physiotherapists tend to advocate exercise, while surgeons tend to advise surgery.
Of course, exercise is not a typical alternative therapy but, as many alternative practitioners might disagree with this statement because they regularly recommend it to their patients, it makes sense to cover it on this blog. So, is exercise better than surgery for meniscus-problems?
The aim of this recent Norwegian study aimed to shed some light on this question. Specifically wanted to determine whether exercise therapy is superior to arthroscopic partial meniscectomy for knee function in patients with degenerative meniscal tears.
A total of 140 adults with degenerative medial meniscal tear verified by magnetic resonance imaging were randomised to either receiving 12 week supervised exercise therapy alone, or arthroscopic partial meniscectomy alone. Intention to treat analysis of between group difference in change in knee injury and osteoarthritis outcome score (KOOS4), defined a priori as the mean score for four of five KOOS subscale scores (pain, other symptoms, function in sport and recreation, and knee related quality of life) from baseline to two-year follow-up and change in thigh muscle strength from baseline to three months.
The results showed no clinically relevant difference between the two groups in change in KOOS4 at two years (0.9 points, 95% confidence interval −4.3 to 6.1; P=0.72). At three months, muscle strength had improved in the exercise group (P≤0.004). No serious adverse events occurred in either group during the two-year follow-up. 19% of the participants allocated to exercise therapy crossed over to surgery during the two-year follow-up, with no additional benefit.
The authors concluded that the observed difference in treatment effect was minute after two years of follow-up, and the trial’s inferential uncertainty was sufficiently small to exclude clinically relevant differences. Exercise therapy showed positive effects over surgery in improving thigh muscle strength, at least in the short-term. Our results should encourage clinicians and middle-aged patients with degenerative meniscal tear and no definitive radiographic evidence of osteoarthritis to consider supervised exercise therapy as a treatment option.
As I stated above, I mention this trial because exercise might be considered by some as an alternative therapy. The main reason for including it is, however, that it is in many ways an exemplary good study from which researchers in alternative medicine could learn.
Like so many alternative therapies, exercise is a treatment for which placebo-controlled studies are difficult, if not impossible. But that does not mean that rigorous tests of its value are impossible. The present study shows the way how it can be done.
Meaningful clinical research is no rocket science; it merely needs well-trained scientists who are willing to test the (rather than promote) their hypotheses. Sadly such individuals are as rare as gold dust in the realm of alternative medicine.
WARNING: THIS POST IS NOT ABOUT ALTERNATIVE MEDICINE
My first ever scientific paper, a spin-off from my MD thesis, was published exactly 40 years ago. Since then, I have written many more articles. Readers of this blog might think that they are all on alternative medicine, but that is not the case. My most cited paper is (I think) one which combined my research in haemorheology with that in epidemiology. Yet, I would not consider it to be my most important article.
So, what is my most important publication?
It is one that relates to the history of medicine.
How come?
In 1990, I was appointed as chair of Rehabilitation Medicine at the University of Vienna. On the occasion of the official opening of the new 2000-bed university hospital in Vienna, I was asked to say a few words and thought that a review of the history of my department might be a fitting subject. But I was wrong. What I discovered while researching it turned out to be totally unfitting for the event; in fact, it contributed to my decision to leave Vienna in 1993. I did, however, summarize my findings in an article – and it is this paper that I consider my most important publication. Here is its abstract:
Misguided by the notion that the decline of the German race would be prevented by purifying “Aryan blood” and eliminating foreign, particularly Jewish, influences, the Nazis evicted all Jews from universities within their growing empire during the Third Reich. The Medical Faculty of Vienna suffered more than any other European faculty from “race hygiene.” Within weeks of the Nazi annexation of Austria in 1938, 153 of the Faculty’s 197 members were dismissed. By far the most frequent reason for dismissal was Jewish origin. Most victims managed to emigrate, many died in concentration camps, and others committed suicide. The “cleansing” process encountered little resistance, and the vacant posts were quickly filled with persons known not for their medical expertise but for their political trustworthiness. It was in this climate that medical atrocities could be committed. After the collapse of the Third Reich, most members of the Faculty were burdened with a Nazi past. Most remained in office, and those who had to leave were reinstituted swiftly. The Jews evicted in 1938 were discouraged from returning. These events have significantly–and with long-lasting effects–damaged the quality of a once-leading medical school. This story needs to be told to honor its victims and to fortify us so that history does not repeat itself.
As I pointed out in my memoir, it “was not published until 1995, by which time I was no longer at the University of Vienna but had left Austria and gone joyfully back to the U.K. to take up my post at the University of Exeter. When the paper was published, it had a considerable impact and important consequences. On the one hand, I received a torrent of hate-mail and threats, and was even accused by the more sensationalistic elements of the Austrian press of having stolen considerable amounts of money from my department at the University of Vienna – an entirely fabricated story, of course, and so ridiculous that I couldn’t even take it seriously enough to instigate legal action.”
So, what else happened as a consequence of the paper?
The answer is ‘lots’.
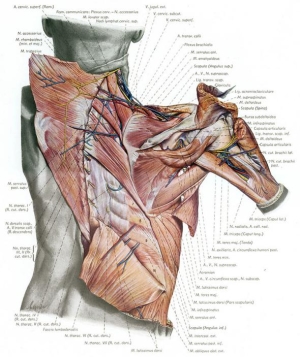
The Nazi-dean of the medical faculty in 1938, Eduard Pernkopf, became the author of one of the world’s best anatomical atlas. Here is a short excerpt from a website on Pernkopf and his work which outlines some of the consequences of my paper:
START OF QUOTE
Following Dr. Edzard Ernst’s, revelations in the Annals of Internal Medicine (1995) about the source of Pernkopf’s “models,” Yad Vashem (the Holocaust Authority in Israel) requested that the Universities of Vienna and Insbruck conduct an independent inquiry to determine who the subjects in Pernkopf’s Atlas were and how they died. The request from Yad Vashem was initially denied; but the issue did not end. The following year, a letter by Dr. Seidelman and Dr. Howard Israel, an oral surgeon at Columbia University published in JAMA (November, 1996) in which they stated: “The abuses of medicine perpetrated during the Hitler regime pervaded the entire medical profession of the Third Reich including the academic elite. One legacy of the tragic era endures today through the continued publication of a critically acclaimed atlas, Pernkopf Anatomy…” Their letter prompted a report by the New York Times (1996).
In 1997, Alfred Ebenbauer, the rector of the University of Vienna, wrote to JAMA indicating that an investigation had been initiated and that preliminary findings indicated that the anatomy department had indeed, routinely received corpses of executed persons, among them renowned dissidents, and “brain preparations derived from children under the euthanasia program in psychiatric institutes were still stored there…” For the first time, he acknowledged publicly systematic suppression and even denial of the university’s Nazi past and its failure to conduct relevant investigations. Ebenbauer explained that this attitude had changed because of ‘‘increasing pressure from abroad’’ and a new political atmosphere in Austria (Ethics and Access…Pernkopf atlas, Bulletin of the Medical Library Association 2001; Hildebrandt, 2006).
 The final report of University of Vienna investigation found that at least 1,377 bodies of executed victims (guillotined or shot by the Gestapo at a rifle range); about 7,000 bodies of fetuses and children; and “8 victims of Jewish origin” had been received by the Anatomy Institute. A statement for users of Pernkop’s Atlas sent out by the U of V to all libraries states: “it is therefore within the individual user’s ethical responsibility to decide whether and in which way he wishes to use this book.” (Hildebrandt, 2006). Hildebrandt states: “the influx of bodies from executions increased so much during the NS [Nazi] regime that the rooms of the anatomy institute were sometimes overfilled and executions had to be postponed because of this.” However, she notes that the true numbers are not known because of incomplete documentation.
The final report of University of Vienna investigation found that at least 1,377 bodies of executed victims (guillotined or shot by the Gestapo at a rifle range); about 7,000 bodies of fetuses and children; and “8 victims of Jewish origin” had been received by the Anatomy Institute. A statement for users of Pernkop’s Atlas sent out by the U of V to all libraries states: “it is therefore within the individual user’s ethical responsibility to decide whether and in which way he wishes to use this book.” (Hildebrandt, 2006). Hildebrandt states: “the influx of bodies from executions increased so much during the NS [Nazi] regime that the rooms of the anatomy institute were sometimes overfilled and executions had to be postponed because of this.” However, she notes that the true numbers are not known because of incomplete documentation.
Howard M. Spiro, M.D., director of Yale’s Program for Humanities in Medicine and professor of internal medicine, was among the noted speakers at the convocation in Vienna marking (1998) the 60th anniversary of the dismissal of Jewish faculty members from the Vienna Medical School. In his address The Silence of Words, Dr. Spiro said, “the things that we avoid and don’t talk about are the matters that mean the most to us. The shame that has no vent in words makes other organs weep.” Dr. Spiro acknowledged that current officials of the University of Vienna are attempting to recover information that has either been hidden or destroyed and trying to locate former faculty who were interned and exiled. “There is a new generation that has taken over, and they are not afraid to look into these atrocities.”
It is now understood that many of the incredibly detailed illustrations in Pernkopf’s atlas depicted the bodies of victims of Nazi terror.
END OF QUOTE
Why do I bring this up again today?
For two reasons: firstly, I have been invited to give two lecture about these events in recent weeks. Secondly and much more importantly, we seem to live in times when the threat of fascism in several countries has again become worrisomely acute, and I think reminding people of my conclusion drawn in 1995 might not be a bad idea:
This story needs to be told to honor its victims and to fortify us so that history does not repeat itself.
