Monthly Archives: August 2019
Yes, I have just published another book! It is entitled ALTERNATIVE MEDICINE, A CRITICAL ASSESSMENT OF 150 MODALITIES.
And yes, I would like you to read it! (You don’t need to buy it, go to your library and ask them to order it.)
Therefore, allow me to try and whet your appetite by simply copying the preface of my book here:

In their famous editorial of 1998, Angell and Kassirer concluded that “It is time for the scientific community to stop giving alternative medicine a free ride. There cannot be two kinds of medicine — conventional and alternative. There is only medicine that has been adequately tested and medicine that has not, medicine that works and medicine that may or may not work. Once a treatment has been tested rigorously, it no longer matters whether it was considered alternative at the outset. If it is found to be reasonably safe and effective, it will be accepted. But assertions, speculation, and testimonials do not substitute for evidence. Alternative treatments should be subjected to scientific testing no less rigorous than that required for conventional treatments.”[1]
Twenty years later, alternative medicine remains popular and assertions, speculation, and testimonials still substitute for evidence. We are still being inundated with misleading advice, biased opinions, uncritical evaluations, commercially-driven promotion and often even fraudulently wrong conclusions. Consequently, consumers find it hard to access reliable data. As a result, they often make misguided, sometimes even dangerously wrong decisions.
I have researched alternative medicine for more than 25 years. Through this work, I have gathered a wealth of knowledge, facts and experience. In this book, I have summarised the essentials into an easily accessible text. My book offers an introduction into the most important issues around alternative medicine as well as a concise, evidence-based analysis of 150 alternative therapies and diagnostic techniques.
Such information is surely a good thing, but it should nevertheless come with a warning: it may not please everybody! If you are a believer in alternative medicine who does not care about the facts, or an enthusiast for whom alternative medicine has become some sort of a religion, or a person who thinks that science is less important than anecdote, you better return this book to its shelf; reading it will only disquiet you.
If, however, you are looking for the facts about alternative medicine, trust in science, prefer critical assessment to commercial promotion, it might well be a book for you.
I hope that you belong to the latter group and trust it will help you making the right therapeutic decisions for yourself and your family.
[1] http://www.kitsrus.com/pdf/nejm_998.pdf
PS
If you want to publish a book review, please contact me and I will see that you get a free e-book.
According to the European Committee of Homeopathy, the Committee on Health and Consumer Affairs of the Spanish Parliament unanimously adopted a bill in 2009 that recognises homeopathy as a medical act. It urged the government to “take the measures necessary for the exercise of homeopathy exclusively by graduates in medicine and surgery.” On 17 December 2009, the Consejo General de Colegios Oficiales de Médicos (Spanish Medical Council) adopted a resolution that recognised the practice of homeopathy as a medical act.
One decade later, the wind seems to have changed. As reported previously (see here and here), there are now several Spanish initiatives to minimise the damage bogus therapies like homeopathy do to public health. A recent article reported that the Spanish health ministry has been campaigning for a change in the EU law that classifies homeopathic products as medicines. The European Commission seems to be open to the idea.
The criticism of homeopathy in Spain was triggered at least in part by reports of people refusing or abandoning regular treatment in favour of homeopathic products to treat serious diseases like cancer. One of them was Rosa Morillo, who died of breast cancer in 2017, after she refused chemotherapy and sought homeopathic treatments instead, according to El País.
“The problem is the damage that can be done by opting for an alternative therapy that has not demonstrated scientific evidence,” Carcedo, the Sanish health minister, said. She raised the issue again in bilateral talks at the most recent EU health ministers’ meeting in Luxembourg in June. “What we can do is keep up the pressure, because the change in the directive must be done at a European level,” she told El País.
The 2001 EU directive on the code for human medicines states that “homeopathic medicinal products” are eligible for a simplified registration procedure if they are administered orally or externally, have no specific therapeutic indication on their packaging; and are sufficiently diluted to guarantee their safety. Homeopathic products with a specific therapeutic indication, meanwhile, have to get a marketing authorization following the same rules as regular medicines, including providing proof of efficacy.
The envisaged change in EU law would be most welcome, in my view. It would:
- abolish the current double standards,
- end the misleading messages to consumers,
- align the law with the current best evidence,
- abolish the unfair commercial advantage of homeopathy producers,
- align the law with ethical imperatives,
- make a positive contribution to public health,
- increase trust in EU drug regulation.
But we should not be over-optimistic either. The European homeopathy lobby is powerful and is fighting with its back to the wall.
And what can we do to help? Perhaps writing to your MEP in support of the Spanish initiative might be a good idea?
Japanese neurosurgeons reported the case of A 55-year-old man who presented with progressive pain and expanding swelling in his right neck. He had no history of trauma or infectious disease. The patient had undergone chiropractic manipulations once in a month and the last manipulation was done one day before the admission to hospital.
On examination by laryngeal endoscopy, a swelling was found on the posterior wall of the pharynx on the right side. The right piriform fossa was invisible. CT revealed hematoma in the posterior wall of the right oropharynx compressing the airway tract. Aneurysm-like enhanced lesion was also seen near the right common carotid artery. Ultrasound imaging revealed a fistula of approximately 1.2 mm at the posterior wall of the external carotid artery and inflow image of blood to the aneurysm of a diameter of approximately 12 mm. No dissection or stenosis of the artery was found. Jet inflow of blood into the aneurysm was confirmed by angiography. T1-weighted MR imaging revealed presence of hematoma on the posterior wall of the pharynx and the aneurysm was recognized by gadolinium-enhancement.
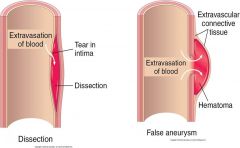
The neurosurgeons performed an emergency operation to remove the aneurysm while preserving the patency of the external carotid artery. The pin-hole fistula was sutured and the wall of the aneurysm was removed. Histopathological assessment of the tissue revealed a pseudoaneurysm (also called a false aneurism), a collection of blood that forms between the two outer layers of an artery.
The patient was discharged after 12 days without a neurological deficit. Progressively growing aneurysm of the external carotid artery is caused by various factors and early intervention is recommended. Although, currently, intravascular surgery is commonly indicated, direct surgery is also feasible and has advantages with regard to pathological diagnosis and complete repair of the parent artery.
The relationship between the pseudoaneurysm and the chiropractic manipulations seems unclear. The way I see it, there are the following three possibilities:
- The manipulations have causally contributed to the pseudo-aneurysm.
- They have exacerbated the condition and/or its symptoms.
- They are unrelated to the condition.
If someone is able to read the Japanese full text of this paper, please let us know what the neurosurgeons thought about this.
The Society of Homeopaths (SoH) is the professional organisation of UK lay homeopaths (those with no medical training). The SoH has recently published a membership survey. Here are some of its findings:
- 89% of all respondents are female,
- 70% are between the ages of 35 and 64.
- 91% of respondents are currently in practice.
- 87% are RSHoms.
- The majority has been in practice for an average of 11 – 15 years.
- 64% identified their main place of work as their home.
- 51% work within a multidisciplinary clinic.
- 43% work in a beauty clinic.
- 85% offer either telephone or video call consultations.
- Just under 50% see 5 or fewer patients each week.
- 38% are satisfied with the number of patients they are seeing.
- 80% felt confident or very confident about their future.
- 65% feel supported by the SoH.
 What can we conclude from these data?
What can we conclude from these data?
Nothing!
Why?
Because this truly homeopathic survey is based on exactly 132 responses which equates to 14% of all SoH members.
If, however, we were able to conclude anything at all, it would be that the amateur researchers at the SoH cause Hahnemann to turn in his grave. Offering telephone/video consultations and working in a beauty salon would probably have annoyed the old man. But what would have definitely made him jump with fury in his Paris grave is a stupid survey like this one.
Guest post by Toby Katz
Who am I?
I’m a final-year graduate medic (also hold an Economics degree) studying at St George’s University. I founded the Integrative Medicine Society at the university, with the aim of hosting talks on evidence-based CAM. My interest in evidence-based CAM arose as many of my family members have benefitted from different CAM interventions (mostly due to chronic MSk pain), where conventional interventions (physiotherapy and chronic pain teams) have failed to resolve their issues.
When it comes to the CAM debate, I see myself as a centrist. I am both a CAM apologist and sceptic and in recent years I have looked to educate myself around this subject. I have read Ernst’s Desktop Guide to CAM and Moral Maze books, spoken to Professor Colquhoun and most recently I undertook the Foundation Course in CAM run by the College of Medicine. My review of the course follows.
Overall, there’s a lot to learn from both sides of the debate and the debate continues due to systematic issues in the UK. Ad hominem attacks don’t help anyone, but conversation can. I hope I can converse with many of you in the future.
The Foundation Course
Two days of fast-paced talks on Integrative/Complementary and Alternative Medicine. The topics included: Resilience, nutritional therapy, medical acupuncture, MSk methods for non-osteopaths, homeopathy, herbs and spices, imagery and relaxation, cancer, hypnotherapy and social prescribing.
The speakers included: Professor David Peters, Dr Catherine Zollman (Medical Director for Penny Brohn), Heather Richards (Nutritional Therapist), Dr Elizabeth Thompson (GP and homeopath), Trevor Hoskisson (Hypnotherapist), Dr Mike Cummings (BMAS), Simon Mills (Medical Herbalist) – at least two of these are already in the infamous Alt Med Hall of Fame!
Initial feelings
My initial feelings upon hearing the talks were that most of these individuals are inherently good people, who want the best outcomes for their patients. Their aim is to operate in the areas of medicine where conventional medicine doesn’t hold the answers – chronic pain, idiopathic headache, IBS etc. But there were also people who were advocating the use of unproven alternative therapies.
These were some of my thoughts I jotted down during the two days:
Professor Peters – Constantly speaking in generalisations. Uses historic references, romantic and philosophical language to entice listeners but generally has little point to what he says. Suffers from tangential thinking. Loses track of his own point. Very Freudian-like thinking (everyone has gone through childhood trauma according to him).
Dr Catherine Zollman – Brilliant. Absolutely brilliant. The doctor I resonate most closely with out of everyone speaking. Promoting the holistic management of a cancer diagnosis; integrating (not undermining) conventional medicine with complementary ways of dealing with the stress surrounding the diagnosis and much more. Works for a non-for-profit organisation. She has many years of oncology experience and strives to create a patient-centred approach to management.
Dr Mike Cummings – promoting medical acupuncture mainly for myofascial pain syndrome. I volunteered to receive acupuncture in my shoulder (have had post-op muscular pain since April). He dry-needled one of my trigger points and it helped, for a few days – this is better than anything a physio has done for me so far. I don’t know why dry-needling isn’t taught at medical school to help with myofascial pain syndrome.
Dr Elizabeth Thompson – Very respectable but I do feel the homeopathy ship has well and truly sailed. Provided ‘evidence’ on how ‘succussion’ changes the make-up of water molecules. Though Dr Thompson is medically trained, there are many non-medical homeopaths who promote things such as homeoprophylaxis and anti-vaccine views and I’m more worried about these such homeopaths. I do respect Dr Thompson and believe her when she says she has helped many patients. Whether this is due to placebo or the get-better-anyway effect I don’t know.
What they were promoting
On reflection, it’s clear that there was a real mix in promoting evidence-based therapies and eyebrow-raising alternatives – this is often difficult for those with an untrained eye to spot the difference. There was a general air of distrust with modern science and EBM floating around the room at all times. Sure, there are things wrong with it, but I think it’s done us pretty well over the last few decades!
I irritated a few speakers when I asked about the evidence behind their claims!
What to take away
There were many GPs present, who stated they’re often in a difficult position in the current system of healthcare we have in the UK. Around half of all consultations are MSk based, many of which are associated with chronic, muscular pain. The WHO analgesic pathway does little for these patients (unless you want to knock them for six with oxycodone) and physiotherapists struggle to make a real difference in a 30-minute appointment. The truth is, we are not providing GPs with the right toolkit to cope with these “difficult” patients.
Going forward
– Get a copy of Ernst et al.’s Desktop Guide for CAM
– Release more formal guidelines using this book as a base for any positive evidence
– Engage in conversation with those from both sides. We have a lot to learn from one another
– SCRAP the forms of CAM that have no plausibility
Food for thought
– If a patient’s pain improves after a session of acupuncture and not from physiotherapy, does it fit with a utilitarian ethical model to deny this person access to acupuncture if EBM shows acupuncture has rates similar to placebo?
– Chronic myofascial pain syndrome. Can we manage it better in primary care? Why not teach dry needling to healthcare professionals? (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4107879/ – Desai et al suggest it works)
– What is the alternative for no CAM for many patients who suffer? If patient’s choice is reduced, does that not reduce their autonomy?
If anyone wishes to contact me, you can at [email protected]
- the availability (numbers and where they are practising),
- quality (education and licensing),
- accessibility (entry and reimbursement),
- acceptability (scope of practice and legal rights).
An electronic survey was issued to contact persons of constituent member associations of the World Federation of Chiropractic (WFC). In addition, data were collected from government websites, personal communication and internet searches. Data were analysed using descriptive statistics.
Information was available from 90 countries in which at least one chiropractor was present. The total number of chiropractors worldwide was 103,469. The number of chiropractors per country ranged from 1 to 77,000. Chiropractic education was offered in 48 institutions in 19 countries. Direct access to chiropractic services was available in 81 (90%) countries, and services were partially or fully covered by government and/or private health schemes in 46 (51.1%) countries. The practice of chiropractic was legally recognized in 68 (75.6%) of the 90 countries. It was explicitly illegal in 12 (13.3%) countries. The scope of chiropractic practice was governed by legislation or regulation in 26 (28.9%) countries and the professional title protected by legislation in 39 (43.3%). In 43 (47.8%) countries, chiropractors were permitted to own, operate, or prescribe x-rays, in 22 (24.4%) countries they were lawfully permitted to prescribe advanced imaging (MRI or CT), and in 34 (38.8%) countries owning, operating or prescribing diagnostic ultrasound was permitted. Full or limited rights to the prescription of pharmaceutical medication were permitted in 9 (10%) countries, and authorization of sick leave was permitted in 20 (22.2%) countries. The care of children was subject to specific regulations and/or statutory restrictions in 57 (63.3%) countries.
The authors concluded as follows: We have provided information about the global chiropractic workforce. The profession is represented in 90 countries, but the distribution of chiropractors and chiropractic educational institutions, and governing legislations and regulations largely favour high-income countries. There is a large under-representation in low- and middle-income countries in terms of provision of services, education and legislative and regulatory frameworks, and the available data from these countries are limited.
The countries where chiropractic is explicitly illegal are the following:
- Egypt
- Argentina
- Columbia
- Austria,
- Estonia,
- Greece,
- Hungary,
- Lebanon,
- Republic of Korea,
- Taiwan,
- Turkey.
- Ukraine.
Forty-two countries (61.8%) have regulations and/or rules under the legislation to provide for registration or licensure of chiropractors. Chiropractors may be available in 90 countries, but 50% percent of these have 10 or fewer chiropractors. Importantly, the care of children is under regulation or restrictions in most countries.
- The World Federation of Chiropractic takes 3 years to publish data which, by then, are of course out-dated.
- In most countries, the chiropractic care for children is restricted.
- In many countries chiropractic is illegal.
- In many countries, there are only very few or no chiropractors at all.
- There are about 4 times more physiotherapists than chiropractors.
- In 9 countries, chiropractors have the right to prescribe medicines.
Much of the data revealed in this survey suggests to me that the world can do without chiropractors.
