prevention
Massage is frequently used for recovery and increased performance. This review, aimed to search and systemize current literature findings relating to massages’ effects on sports and exercise performance concerning its effects on motor abilities and neurophysiological and psychological mechanisms.
One hundred and fourteen articles were included. The data revealed that massages, in general, do not affect motor abilities, except flexibility. However, several studies demonstrated that positive muscle force and strength changed 48 h after the massage was given. Concerning neurophysiological parameters, massage did not change blood lactate clearance, muscle blood flow, muscle temperature, or activation. However, many studies indicated a reduction of pain and delayed onset muscle soreness, which are probably correlated with the reduction of the level of creatine kinase enzyme and psychological mechanisms. In addition, massage treatment led to a decrease in depression, stress, anxiety, and the perception of fatigue and an increase in mood, relaxation, and the perception of recovery.
The authors concluded that the direct usage of massages just for gaining results in sport and exercise performance seems questionable. However, it is indirectly connected to performance as an important tool when an athlete should stay focused and relaxed during competition or training and recover after them.
The evidence about the value of massage therapy is limited through the mostly poor quality of the primary studies. Unfortunately, the review authors did not bother to address this issue. Another recent and in my opinion more rigorous review identified 29 eligible studies recruiting 1012 participants, representing the largest examination of the effects of massage. Its authors found no evidence that massage improves measures of strength, jump, sprint, endurance, or fatigue, but massage was associated with small but statistically significant improvements in flexibility and DOMS. Massage therapy has the additional advantage that it is agreeable and nearly free of adverse effects. So, on balance, I think massage therapy might be worth considering for athletes.
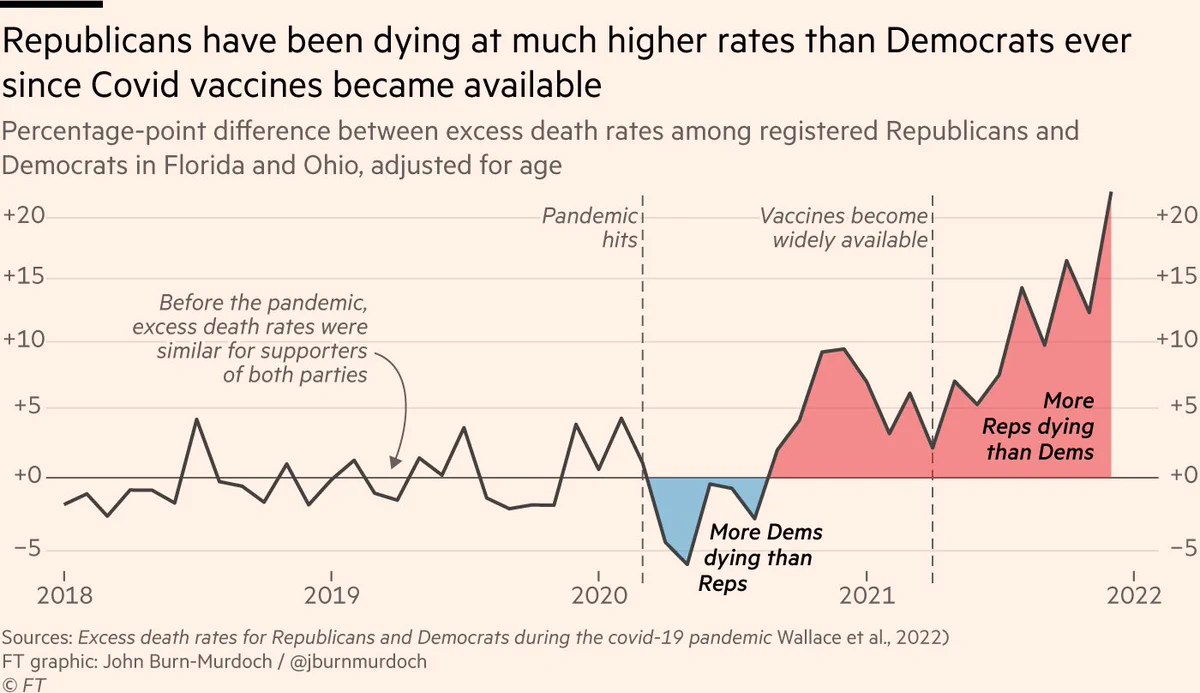
There is evidence that, in the US, Republican-leaning counties have had higher COVID-19 death rates than Democratic-leaning counties and similar evidence of an association between political party affiliation and attitudes regarding COVID-19 vaccination. This investigation assessed political party affiliation and mortality rates for individuals during the initial 22 months of the COVID-19 pandemic.
A cross-sectional comparison of excess mortality between registered Republican and Democratic voters between March 2020 and December 2021 adjusted for age and state of voter registration was conducted. Voter and mortality data from Florida and Ohio in 2017 linked to mortality records for January 1, 2018, to December 31, 2021, were used in data analysis. The main outcome measure was the excess weekly death rates during the COVID-19 pandemic adjusted for age, county, party affiliation, and seasonality.
Between January 1, 2018, and December 31, 2021, there were 538 159 individuals in Ohio and Florida who died at the age of 25 years or older in the study sample. The median age at death was 78 years (IQR, 71-89 years). Overall, the excess death rate for Republican voters was 2.8 percentage points, or 15%, higher than the excess death rate for Democratic voters (95% prediction interval [PI], 1.6-3.7 percentage points). After May 1, 2021, when vaccines were available to all adults, the excess death rate gap between Republican and Democratic voters widened from −0.9 percentage points (95% PI, −2.5 to 0.3 percentage points) to 7.7 percentage points (95% PI, 6.0-9.3 percentage points) in the adjusted analysis; the excess death rate among Republican voters was 43% higher than the excess death rate among Democratic voters. The gap in excess death rates between Republican and Democratic voters was larger in counties with lower vaccination rates and was primarily noted in voters residing in Ohio.
The authors concluded that, in this cross-sectional study, an association was observed between political party affiliation and excess deaths in Ohio and Florida after COVID-19 vaccines were available to all adults. These findings suggest that differences in vaccination attitudes and reported uptake between Republican and Democratic voters may have been factors in the severity and trajectory of the pandemic in the US.
In light of what has been discussed repeatedly, these findings are in my view most impressive and seem to speak for themselves. The authors are nevertheless prudent and stress that their study has several limitations which mean that we ought to interpret their results with caution.
- First, there are plausible alternative explanations for the difference in excess death rates by political party affiliation beyond the explanatory role of vaccines discussed herein.
- Second, the mortality data, although detailed and recent, only included approximately 83.5% of deaths in the US and did not include the cause of death. Although overall excess death patterns in our data are similar to those in other reliable sources, such as the Centers for Disease Control and Prevention National Center for Health Statistics data, it is possible that the deaths that our study data did not include may disproportionately occur among individuals registered with a particular political party, potentially biasing our results. In addition, the completeness of the mortality data may vary across states or time, potentially biasing our estimates of excess death rates.
- Third, all excess death models rely on fundamentally untestable assumptions to construct the baseline number of deaths one would expect in the absence of the COVID-19 pandemic.
- Fourth, because no information on individual vaccination status was available, analyses of the association between vaccination rates and excess deaths relied on county-level vaccination rates.
- Fifth, the study was based on data from 2 states with readily obtainable historical voter registration information (Florida and Ohio); hence, the results may not generalize to other states.
The World Federation of Chiropractic (WFC) has recently launched a new Global Patient Safety (GPS) initiative:
Unanimously approved by the WFC Board at its May meeting, the project will be overseen by the Research Committee and involve the establishment of an expert task force. Planned projects will include a scoping review, identification of best practices in incident reporting and learning, risk management in chiropractic practice and knowledge translation activities.
In recent years, patient safety has increasingly been in the spotlight as health systems strive to reduce unnecessary incidents and iatrogenic injury.
“With adverse events having the potential to impact trust and confidence in the chiropractic profession, it is important that we do as much as possible to inform ourselves in relation to the risks and benefits of chiropractic treatments and related activities,” said Prof. Richard Brown DC, LL.M, WFC Secretary- General.
“While we know that serious adverse events are rare, patients with multiple co-morbidities and known risk factors require special attention. The WFC GPS Task Force will highlight key areas of patient safety to support chiropractors, build and strengthen the existing safety culture and help to meet the expectations of patients and the public.”
Chiropractors use a package of interventions in their treatment of patients, including hands-on care, adjunct therapies, health promotion, advice and exercise prescription. The process of shared decision-making involves consideration by the chiropractor of the suitability and safety of each intervention. In addition to direct patient care, chiropractors also have a duty to consider the safety of their offices and clinics.
A WHO resolution on patient safety, passed in 2019 at the World Health Assembly, made a commitment to take global action in tackling avoidable harm.
Its subsequent publication, Global Action on Patient Safety, set out goals and targets to reduce morbidity from healthcare related incidents.
Chair of the Task Force and Research Committee vice-chair, Dr Katie Pohlman DC, PhD, said: “With the current global focus on patient safety, I’m proud to be leading this WFC Task Force, which will support the chiropractic profession but, most importantly, work to minimize adverse events and protect patients.
“The creation of an open, transparent culture of patient safety is key to maintaining trust and credibility. The Task Force is looking forward to adding to the body of knowledge and advancing safe, evidence-based, people-centered practice.”
The WFC GPS Task Force will report to Research Committee Chair, Assoc. Prof Sidney Rubinstein. It will include members of the existing Research Committee as well as external experts.
____________________________
At first, most people will think: WHAT A GOOD IDEA!
After a bit of reflection, however, some might ponder: WHY ONLY NOW AND NOT DECADES AGO?
And after reading the above text carefully, skeptics might feel that the exercise can already be classified as a PR gimmick that will not generate the needed information:
- The WFC has yet again failed to establish a monitoring system of adverse effects; without it ‘patient safety’ is not achievable.
- They claim that “we know that serious adverse events are rare”. How do they know this? And if they already are convinced of this, the new task force is bound to be a pure ‘white wash’.
- They think an “existing safety culture” exists in chiropractic. This is wishful thinking and far from reality.
- They speak of the “expectations of patients and the public” but ignore the need for a monitoring system accessible to the public.
As we have recently discussed diet and its effects on health, it seems reasonable to ask whether there is a diet that is demonstrably healthy. A recent investigation attempted to answer this question.
This study was aimed at developing a healthy diet score that is associated with health outcomes and is globally applicable. It used data from the Prospective Urban Rural Epidemiology (PURE) study and tried to replicate it in five independent studies on a total of 245 000 people from 80 countries.
A healthy diet score was developed on the basis of the data from 147 642 people from the general population, from 21 countries in the PURE study. The consistency of the associations of the score with events was examined in five large independent studies from 70 countries.
The healthy diet score was developed based on six foods each of which has been associated with a significantly lower risk of mortality [i.e. fruit, vegetables, nuts, legumes, fish, and dairy (mainly whole-fat); range of scores, 0–6]. The main outcome measures were all-cause mortality and major cardiovascular events [cardiovascular disease (CVD)].
During a median follow-up of 9.3 years in PURE, compared with a diet score of ≤1 point, a diet score of ≥5 points was associated with a lower risk of:
- mortality [hazard ratio (HR) 0.70; 95% confidence interval (CI) 0.63–0.77)],
- CVD (HR 0.82; 0.75–0.91),
- myocardial infarction (HR 0.86; 0.75–0.99),
- stroke (HR 0.81; 0.71–0.93).
In three independent studies with vascular patients, similar results were found, with a higher diet score being associated with lower mortality (HR 0.73; 0.66–0.81), CVD (HR 0.79; 0.72–0.87), myocardial infarction (HR 0.85; 0.71–0.99), and a non-statistically significant lower risk of stroke (HR 0.87; 0.73–1.03). Additionally, in two case-control studies, a higher diet score was associated with lower first myocardial infarction [odds ratio (OR) 0.72; 0.65–0.80] and stroke (OR 0.57; 0.50–0.65). A higher diet score was associated with a significantly lower risk of death or CVD in regions with lower than with higher gross national incomes (P for heterogeneity <0.0001). The PURE score showed slightly stronger associations with death or CVD than several other common diet scores (P < 0.001 for each comparison).

The authors concluded that consumption of a diet comprised of higher amounts of fruits, vegetables, nuts, legumes, and a moderate amount of fish and whole-fat dairy is associated with a lower risk of CVD and mortality in all world regions, but especially in countries with lower income where consumption of these natural foods is low. Similar associations were found with the inclusion of meat or whole grain consumption in the diet score (in the ranges common in the six studies that we included). Our findings indicate that the risks of deaths and vascular events in adults globally are higher with inadequate intake of protective foods.
The authors rightly stress that their analyses have a number of limitations:
First, diet (as in most large epidemiologic studies) was self-reported and variations in reporting might lead to random errors that could dilute real associations between diet scores and clinical outcomes. Therefore, the beneficial effects of a healthier diet may be larger than estimated.
Second, the researchers did not examine the role of individual types of fruits and vegetables as components in the diet score, since the power to detect associations of the different types of fruits and vegetables vs. CVD or mortality is low (i.e. given that the number of events per type of fruit and vegetable was relatively low). Recent evidence suggests that bioactive compounds and, in particular, polyphenols which are found in certain fruit or vegetables (e.g. berries, spinach, and beans) may be especially protective against CVD.
Third, in observational studies, the possibility of residual confounding from unquantified or imprecise measurement of covariates cannot be ruled out—especially given that the differences in risk of clinical events are modest (∼10%–20% relative differences). Ideally, large randomized trials would be needed to clarify the clinical impact on events of a policy of proposing a dietary pattern in populations.
Fourth, the use of the median intake of each food component as a cut-off in the scoring scheme for each diet may not reflect the full range of consumption or provide a meaningful indicator of consumption associated with the disease. However, the use of quintiles instead of medians within each study or within each region yielded the same results indicating the robustness of our findings.
Fifth, the level of intake to meet the cut-off threshold for each food group in the diet score may differ between countries. However, in sensitivity analyses where region-specific median cut-offs were used to classify participants on each component of the diet score, the results were similar to using the overall cohort median of each food component. Further, with unprocessed red meat and whole grains included or excluded from the diet score in these sensitivity analyses, the results were again similar.
Sixth, misclassification of exposures cannot be ruled out as repeat measures of diet were not available in all studies. However, the ORIGIN study, in which repeat diet assessments at 2 years were conducted, showed similar results based on the first vs. second diet assessments. This indicates that misclassification of dietary intake during follow-up was not undermining the findings.
Seventh, one unique aspect of the study is the focus on only protective foods, i.e. a dietary pattern score that highlights what is missing from the food supply, especially in poorer world regions, but this does not negate the importance of limiting the consumption of harmful foods such as highly processed foods. While the PURE diet score had significantly stronger associations with events than other diet scores, the HRs were only slightly larger for PURE than for most other diet scores. However, the Planetary score was the least predictive of events. The analyses provide empirical evidence that all diet scores (other than the Planetary diet score) are of value to predicting death or CVD globally and in all regions of the world.
So, what should we, according to these findings, be looking for and how much of it should we consume? Here is the table that should answer these questions:
| Fruits and vegetables | 4 to 5 servings daily | 1 medium apple, banana, pear; 1 cup leafy vegs; 1/2 cup other vegs |
| Legumes | 3 to 4 servings weekly | 1/2 cup beans or lentils |
| Nuts | 7 servings weekly | 1 oz., tree nuts or peanuts |
| Fish | 2 to 3 servings weekly | 3 oz. cooked (pack of cards size) |
| Dairy | 14 servings weekly | 1 cup milk or yogurt; 1 ½ oz cheese |
| Whole grainsc | Moderate amounts (e.g. 1 serving daily) can be part of a healthy diet | 1 slice (40 g) bread; ½ medium (40 g) flatbread; ½ cup (75–120 g) cooked rice, barley, buckwheat, semolina, polenta, bulgur, or quinoa |
| Unprocessed meatsc | Moderate amounts (e.g. 1 serving daily) can be part of a healthy diet | 3 oz. cooked red meat or poultry |
Sobrenix (Kudzu, Milk Thistle, B Vitamins & More) is “designed to reduce alcohol cravings and help you detoxify your body so you can successfully manage alcohol consumption. Even better, taken before drinking, Sobrenix’s ingredients help you stop before you’ve had too much. DETOXIFY YOUR BODY with a powerful formula that combines herbs and nutrients that support liver health, curb cravings, and help you wake up without a nasty hangover. Sobrenix kick-starts the detoxification process with essential herbs like Milk Thistle and Chanca Piedra. Additionally, the formula contains the critical B-Vitamins that alcohol washes away so you can wake up happy and healthy again!”
Yes, you suspected correctly: this is pure BS!
Not only that but the Federal Trade Commission is taking action under the FTC Act and the Opioid Addiction Recovery Fraud Prevention Act of 2018 (OARFPA) against the makers of Sobrenix. According to the FTC’s complaint, the makers, a company, Rejuvica, and its owners, Kyle Armstrong and Kyle Dilger, made numerous unsubstantiated and false claims about Sobrenix and used paid endorsers in deceptively formatted advertising. The defendants also used bogus review sites to deceive consumers about their products.
As a result of the FTC’s suit, the defendants have agreed to a proposed court order that would permanently ban them from making any unsubstantiated claims about healthcare products or services, as well as require them to pay $650,000 to the FTC to be used for providing refunds to consumers.
“We will not tire in our pursuit of those who prey on individuals struggling with alcohol or other substance use disorders,” said Samuel Levine, Director of the Bureau of Consumer Protection. “This case evidences the breadth of the FTC’s authority to pursue such wrongdoing under both the FTC Act and OARFPA.”
The FTC charges that the defendants marketed Sobrenix with messages like:
- “STRUGGLING TO CONTROL YOUR ALCOHOL CONSUMPTION? Sobrenix is designed to reduce alcohol cravings and help you detoxify your body so you can successfully manage alcohol consumption. Even better, taken before drinking, Sobrenix’s ingredients help you stop before you’ve had too much.”
The FTC charges that Rejuvica and its owners lacked adequate evidence to support these claims. The complaint charges that Rejuvica, Armstrong, and Dilger violated both the FTC Act and OARFPA. The proposed order contains a total monetary judgment of $3,247,737, which is partially suspended based on the defendants’ inability to pay the full amount. The defendants will be required to pay $650,000 to the FTC to be used to refund consumers. If the defendants are found to have lied to the FTC about their financial status, the full judgment will be immediately due.
______________________________
A few short comments might be in order:
- Regulators have the duty to protect consumers from false health claims.
- It is commendable that some authorities sometimes do their duty and go after some of the people responsible for making false claims related to dietary supplements.
- Such actions should, however, occur MUCH more often.
- They ought to happen also in countries other than the US.
- Similar actions should be initiated against ALL false claims made for healthcare products and services.
- This means that all practitioners of so-called alternative medicine (SCAM) would need to review their advertising, websites, etc., and erase therapeutic claims that are not supported by evidence.
- This would unquestionably amount to an enormously valuable service to public health.
- Most countries already have legislation that would make such steps possible; my question, therefore, is this:
WHY ARE CONSUMERS NOT ADEQUATELY PROTECTED BY THEIR NATIONAL REGULATORS FROM CHARLATANS WHO SELL INEFFECTIVE AND OFTEN DANGEROUS SCAMs AT HIGH COSTS?
The website of the World Federation of Chiropractic (WFC) points out that public health is defined by the WHO as follows:
“Activities to strengthen public health capacities and service aim to provide conditions under which people can maintain to be healthy, improve their health and wellbeing, or prevent the deterioration of their health. Public health focuses on the entire spectrum of health and wellbeing, not only the eradication of particular diseases.”
The WFC then continues stating this:
As primary contact health professionals, chiropractors can play an important role as public health advocates. This can range from providing support and advice on health matters such as physical activity, diet, and fitness as well as lifestyle choices such as injury prevention and avoiding tobacco use. Chiropractors can also play a role in counselling patients and communities on the benefits of public health measures, especially as this relates to immediate health needs of each region.
I think that this might merit a few comments.
- Physical activity is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Diet is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Fitness is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Lifestyle choice is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Injury prevention is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Avoiding tobacco use is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Counseling is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
So, what is the real contribution of chiropractors to public health?
- Chiropractors tend to advise their clients against vaccinations.
- Some mislead the public by claiming they boost immunity and prevent serious infections.
- Many undermine evidence-based medicine by promoting obsolete myths such as ‘the innate’ or subluxations.
- Many sell supplements that could interact with prescription drugs.
- Many make bogus health claims for profit.
I would therefore argue that, on balance, the contribution of chiropractors to public health might be considerable …
sadly, however, it goes in the wrong direction.
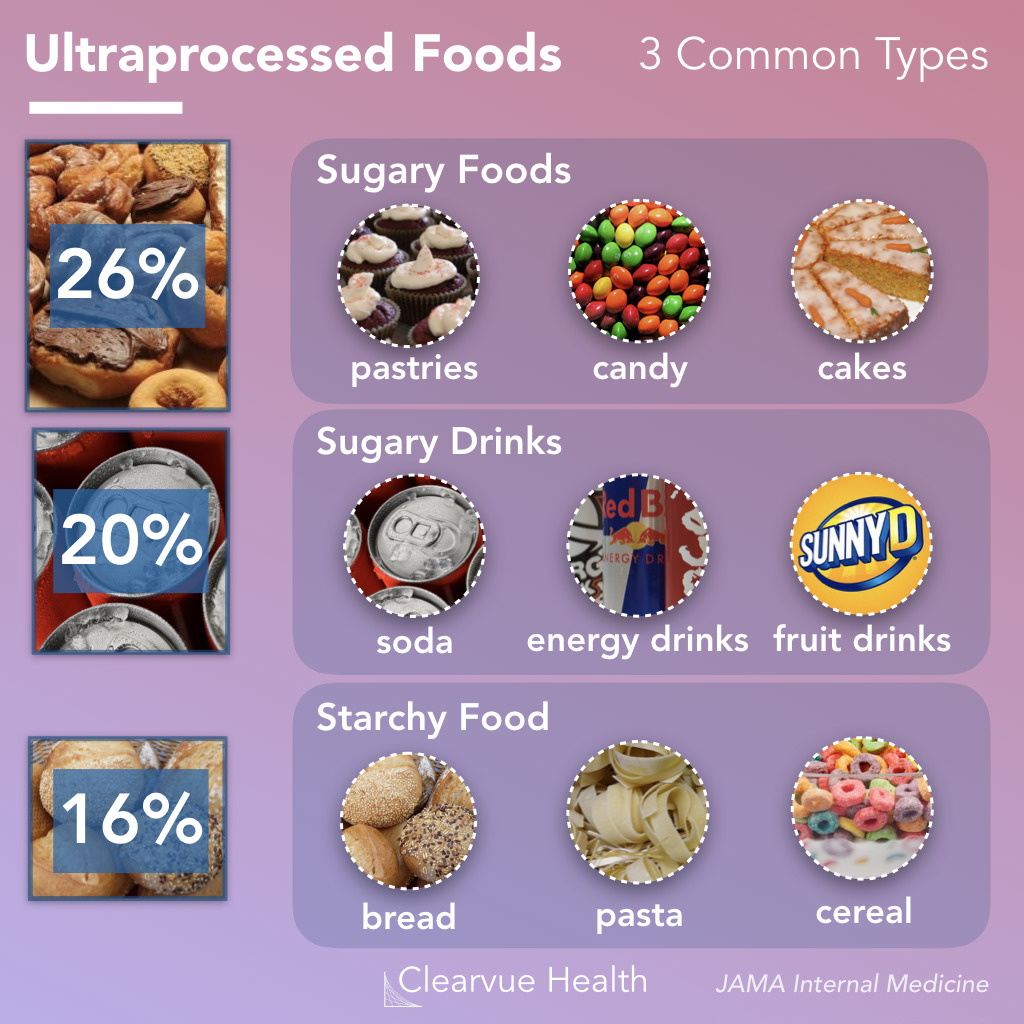
Like ultra-processed food (UPF) itself, the subject of UPF is everywhere – radio, TV, Twitter, you name it, the topic crops up. I too could not resist writing a post on it a few months ago. And now I am publishing another one but one in a slightly more irritated mood.
Why do these endless discussions on UPF irritate me?
To start with, there is no uniform definition of UPF, and many commentators seem more than a little confused about what UPF actually is. One definition holds that Ultra-processed foods are foods that have been altered to include fats, starches, sugars, salts and hydrogenated oils extracted from other foods. They contain ingredients, additives, and preservatives that are not normally used in home cooking. It seems obvious that discussions on UPF without a clear and understandable definition of the term are merely generating confusion in the general public.
But there are, of course, lists of UPF that might render the subject a bit clearer. The trouble, however, is that these lists reveal disagreement among each other. Thus they are prone to generate even more confusion.
Next, there is the evidence – and there is lots of it. It suggests that the regular consumption of UPF is bad for virtually every aspect of health. And if there is no evidence that it is detrimental for a given condition, it probably is merely because nobody has yet bothered to do the analyses. The trouble is, however, that all the relevant research comes from either basic science or epidemiology. This means that causality is unproven.
A further problem is that even the experts don’t know what the alleged causal factors in UPF are.
- Is it the processing?
- The additives?
- The sugar?
- The fats?
- If so, which fats exactly?
- Is it perhaps a complex inter-play of some of these factors?
If we want to make progress, we need to know! If not, we cannot possibly begin to avoid the health-threatening effects of UPF.
The final and arguably biggest problem is that UPF is everywhere. Nobody living in an industrialized country and earning a regular living can avoid consuming UPF. This means, I fear, that all the current hype about UPF is not just irritating but possibly counter-productive.
Imagine an average person trying to make sense of these discussions. She would soon give up and conclude that all these ‘clever’ experts know nothing at all. Her foremost concern is to make ends meet. In the end, she will carry on as before. Alternatively, she might even conclude that, as the even experts do not make sense, UPF cannot be all that bad after all.
After reading about and listening to the arguments around UPF, I ask myself this: would it not be more productive to apply more common sense and focus on a few nutritional messages that are 1) solidly based on evidence and 2) an average person can actually follow?
We have discussed dental amalgam and its risks to human health before. Finally, there is new legislation in sight. The European Commission has revised the EU Mercury Regulation to protect EU citizens and the environment from toxic mercury. Among other things, this will completely ban the use of dental amalgam, for which 40 tons of mercury are currently consumed annually in the EU. The revised mercury ordinance provides for the following:
– No more use of dental amalgam from January 1, 2025; viable mercury-free alternatives are available.
– Ban on the manufacture and export of dental amalgam from the EU from January 1, 2025;
– Ban on the manufacture and export of six mercury-containing lamps from January 1, 2026 and January 1, 2028 (depending on lamp type).
The delegated act adopted under the Mercury Regulation transposes into EU law the decisions taken at the fourth Conference of the Parties (2022) to the Minamata Convention by introducing a ban on the production, import, and export of eight additional mercury-containing products, including mercury-containing lamps and non-electrical equipment.
The Minamata Convention is the main international legal framework for the protection of human health and the environment from anthropogenic emissions and releases of mercury to air, water, and soil. Like the Mercury Regulation, it addresses the entire life cycle of mercury, from primary mercury mining to mercury waste management.
The revised Mercury Regulation must now be approved by the European Parliament and the Council under the ordinary legislative procedure. The delegated act will be sent to the European Parliament and the Council for consideration.
Mercury is a highly toxic chemical that poses a threat to both human health and the environment. When released into the environment, it enters the food chain where it accumulates (mainly in fish). High mercury exposure can damage the brain, lungs, kidneys, and immune system.
Historically, mercury has been used in a wide range of applications, including gold mining, batteries, fluorescent tubes, thermometers, and barometers. Over the last twenty years, the EU has developed a comprehensive body of legislation, in particular the Mercury Regulation, which protects human health and the environment from anthropogenic emissions and releases of mercury, taking into account the entire life cycle of mercury from primary mercury mining to final disposal of mercury waste. It also includes measures on trade in mercury-containing products and mercury pollution.
The Minamata Convention entered into force on August 16, 2017, and has so far been ratified by the European Union and 143 countries, including all EU Member States. The fifth session of the Conference of the Parties to the Minamata Convention on Mercury (COP-5) will be held in Geneva, Switzerland, from October 30 to November 3, 2023.
_____________________________
I don’t usually find reading medical papers scary. An article in the prestigious journal ‘Nature’ is the exception. Here is its abstract:
Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. Estimated numbers vary but the assumption is that, of all those who had COVID-19 globally, at least 10% have long COVID. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new health-care challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein–Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. Thus, the current picture is one of convergence towards a map of an immunopathogenic aetiology of long COVID, though as yet with insufficient data for a mechanistic synthesis or to fully inform therapeutic pathways.
The paper ends with this gloomy statement: “The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID. The biggest unknowns remain the joined-up scheme of its pathogenesis and thus the best candidate therapeutics to be trialled in randomized controlled trials, along with a better understanding of the kinetics of recovery and the factors influencing this. Some countries have invested in first-round funding for the pilot investigations. From the above, far more will be needed.”
In the context of this blog, we must, of course, ask: HAS SO-CALLED ALTERNATIVE MEDICINE (SCAM) SOMETHING TO OFFER?
I’m afraid that the short answer to this question is No!
However, one does not need to be a clairvoyant to predict that lots of therapeutic claims followed by plenty of methodologically weak (to put it politely) research will emerge from SCAM. Already some time ago, this homeopath indicated, that SCAM providers should see COVID as an opportunity: For homeopathy, shunned during its 200 years of existence by conventional medicine, this outbreak is a key opportunity to show potentially the contribution it can make in treating COVID-19 patients.
We should not hold our breath to see the emergence of convincing evidence, but we must be prepared to warn the public from getting exploited by charlatans.
In the UK – this post is mainly for UK readers – journalists and opinion leaders are currently falling over themselves reporting about a major breakthrough: an Alzheimer’s drug has been shown to slow the disease by around 36%. “After 20 years with no new Alzheimer’s disease drugs in the UK, we now have two potential new drugs in 12 just months,” wrote Dr Richard Oakley, associate director at the Alzheimer’s Society. And the Daily Mail headlined: “New drug which claims to slow mental decline caused by Alzheimer’s by 36% could spell ‘the beginning of the end’ for the degenerative brain disease”.
That’s excellent news!
Many people will have made a sigh of relief!
So, why does it make me angry?
Once we listen to the news more closely we learn that:
- the drug only works for patients who are diagnosed early;
- for an early diagnosis, we need a PET scan;
- the UK hardly has any PET scanners, in fact, we have the lowest number among developed countries;
- these scanners are very expensive;
- the costs for the new drug are as yet unknown but will also be high.
Collectively these facts mean that we have a major advance in healthcare that could help many patients. At the same time, we all know that this is mere theory and that the practice will be very different.
Why?
- Because the NHS has been run down and is on its knees.
- Because our government will again say that they have invested xy millions into this area.
- The statement might be true or not, but in any case, the funds will be far too little.
- The UK has become a country where some patients suffering from severe toothache currently resort to pulling out their own teeth at home with pairs of pliers.
- In the foreseeable future, the NHS will not be allocated the money to invest in sufficient numbers of PET scans (not to mention the funds to buy the new and expensive drug).
In other words, the UK celebrates yet another medical advance raising many people’s expectations, while everyone in the know is well aware of the fact that the UK public will not benefit from it.
Does that not make you angry too?