bogus claims
The ‘International Chiropractors Association’ (ICA) has just issued a statement entitled “International Chiropractors Association Affirms Policy on Health Freedom“. On the background of the fact that US President Biden, issued a series of Executive Orders related to mandating federal employees and federal contractors to receive the COVID-19 vaccine, the ICA try to explain their position regarding vaccinations. Here are a few passages from this statement:
…In a world of public health that promotes evidence-based decision making, we see the importance of natural immunity being ignored and replaced with a totalitarian approach of compulsory vaccination. At a time when the Surgeon General says misinformation has become an urgent threat to public health, misinformation is now being used in an attempt to discredit the chiropractic profession, the International Chiropractors Association, and all chiropractic patients who desire to focus on improving health naturally. After enduring 18 months of shutdowns, lockdowns, flattening the curve, masking, limitations of speech on social media; and a cancel culture environment that threatens the basic freedoms our country was founded upon in 1776, ICA will not compromise on the importance of protecting health freedom…
The ICA Policy on Immunization and Vaccination has remained unchanged for almost 50 years and clearly states:
“The International Chiropractors Association recognizes that the use of vaccines is not without risk and questions the wisdom of mass vaccination programs. Chiropractic principles favor the enhancement of natural immunity over artificial immunization.
The ICA supports each individual’s right to select his or her own health care and to be made aware of the possible adverse effects of vaccines upon a human body. In accordance with such principles and based upon the individual’s right to freedom of choice, the ICA is opposed to compulsory programs which infringe upon such rights.
The International Chiropractors Association is supportive of a conscience clause or waiver in compulsory vaccination laws, providing an elective course of action for all regarding immunization, thereby allowing patients freedom of choice in matters affecting their bodies and health.”
The International Chiropractors Association maintains that all healthcare interventions, including the chiropractic adjustment, are associated with some level of risk and that every individual is entitled to be informed of those risks, no matter how insignificant. All individuals must retain the freedom to accept or reject any healthcare product, procedure, or medication including vaccinations. The International Chiropractors Association therefore strongly opposes the use of medical mandates that violate personal sovereignty, violate the principles of informed consent, and constrain the rights of patients to make their own health care choices…
The ICA encourages the recognition that natural efforts to enhance the innate immune system ability to adapt to novel viruses are grounded in science and rejects the notion that the patients’ freedom to rely on naturally acquired immunity is not based upon unscientific beliefs.
The ICA rejects the premise that the chiropractic profession’s long history of promoting health freedom and supporting conscientious exemptions is based upon unscientific or non-mainstream beliefs…
I find this statement clear as mud and have the following questions:
- Do the ICA recommend vaccinations?
- In particular, do they encourage their members to get vaccinated with the COVID-19 vaccines?
- Do they advise to recommend COVID-19 vaccinations to their patients?
- Or do they think that natural immunity is preferable and advise their members and patients accordingly?
- Do they believe that spinal manipulation enhances natural immunity?
- Do they think that spinal manipulations are an effective alternative to COVID-19 vaccinations?
- Do they believe that scientific evidence trumps dogma or vice versa?
- Which of the two should, according to their conviction, must influence the decision-making processes in healthcare?
- If the ICA object to misinformation about COVID, why do they not stop their members from promoting it?
- What makes them think that information about the possible adverse effects of vaccines upon a human body is unavailable?
- If the ICA recognizes the risks of spinal manipulation, why do they not inform the public about them regularly and objectively?
- If the ICA knows about the importance of informed consent, why do not all of their members adhere to it?
- And finally, why do the ICA insist on the term ‘international’ in the name of their organization, if they purely deal with the US situation?
I do not expect the ICA to give me the answers to these questions. But perhaps their Wiki page goes some way towards answering some of them: “… The ICA supports the efforts of the National Vaccine Information Center (NVIC).[13] The NVIC is known for promoting false and misleading information about vaccines, in particular the discredited claim that vaccines cause autism.
The ICA’s annual conferences have featured anti-vaccination propaganda. In 2018 Guest Speaker Beau Pierce (Pierce co-produced a series entitled Vaccines Revealed) hosted a session entitled Vaccines Revealed.,[14] and Jeff Hays, known for producing the anti-Vaccine propaganda Vaccines Revealed, was invited to host a session the 2017 ICA Council on Chiropractic Pediatrics Annual Conference. In 2016 the widely discredited anti-vaccination propaganda film VAXXED was shown at a conference sponsored by the ICA’s Council on Chiropractic Pediatrics …”
SAY NO MORE!
Therapeutic touch (TT) is a form of paranormal or energy healing developed by Dora Kunz (1904-1999), a psychic and alternative practitioner, in collaboration with Dolores Krieger, a professor of nursing. TT is popular and practised predominantly by US nurses; it is currently being taught in more than 80 colleges and universities in the U.S., and in more than seventy countries. According to one TT-organisation, TT is a holistic, evidence-based therapy that incorporates the intentional and compassionate use of universal energy to promote balance and well-being. It is a consciously directed process of energy exchange during which the practitioner uses the hands as a focus to facilitate the process.
The question is: does TT work beyond a placebo effect?
This review synthesized recent (January 2009–June 2020) investigations on the effectiveness and safety of therapeutic touch (TT) as a therapy in clinical health applications. A rapid evidence assessment (REA) approach was used to review recent TT research adopting PRISMA 2009 guidelines. CINAHL, PubMed, MEDLINE, Cochrane databases, Web of Science, PsychINFO, and Google Scholar were screened between January 2009-March 2020 for studies exploring TT therapies as an intervention. The main outcome measures were for pain, anxiety, sleep, nausea, and functional improvement.
Twenty-one studies covering a range of clinical issues were identified, including 15 randomized controlled trials, four quasi-experimental studies, one chart review study, and one mixed-methods study including 1,302 patients. Eighteen of the studies reported positive outcomes. Only four exhibited a low risk of bias. All others had serious methodological flaws, bias issues, were statistically underpowered, and scored as low-quality studies. Over 70% of the included studies scored the lowest score possible on the GSRS weight of evidence scale. No high-quality evidence was found for any of the benefits claimed.
The authors drew the following conclusions:
After 45 years of study, scientific evidence of the value of TT as a complementary intervention in the management of any condition still remains immature and inconclusive:
- Given the mixed result, lack of replication, overall research quality and significant issues of bias identified, there currently exists no good quality evidence that supports the implementation of TT as an evidence‐based clinical intervention in any context.
- Research over the past decade exhibits the same issues as earlier work, with highly diverse poor quality unreplicated studies mainly published in alternative health media.
- As the nature of human biofield energy remains undemonstrated, and that no quality scientific work has established any clinically significant effect, more plausible explanations of the reported benefits are from wishful thinking and use of an elaborate theatrical placebo.
TT turns out to be a prime example of a so-called alternative medicine (SCAM) that enthusiastic amateurs, who wanted to prove TT’s effectiveness, have submitted to multiple trials. Thus the literature is littered with positive but unreliable studies. This phenomenon can create the impression – particularly to TT fans – that the treatment works.
This course of events shows in an exemplary fashion that research is not always something that creates progress. In fact, poor research often has the opposite effect. Eventually, a proper scientific analysis is required to put the record straight (the findings of which enthusiasts are unlikely to accept).
In view of all this, and considering the utter implausibility of TT, it seems an unethical waste of resources to continue researching the subject. Similarly, continuing to use TT in clinical settings is unethical and potentially dangerous.
This article from AP News caught my attention. Here it is (I haven’t changed a word):
The flashy postcard, covered with images of syringes, beckoned people to attend Vax-Con ’21 to learn “the uncensored truth” about COVID-19 vaccines.
Participants traveled from around the country to a Wisconsin Dells resort for a sold-out convention that was, in fact, a sea of misinformation and conspiracy theories about vaccines and the pandemic. The featured speaker was the anti-vaccine activist who appeared in the 2020 movie “Plandemic,” which pushed false COVID-19 stories into the mainstream. One session after another discussed bogus claims about the health dangers of mask wearing and vaccines.
The convention was organized by members of a profession that has become a major purveyor of vaccine misinformation during the pandemic: chiropractors.
At a time when the surgeon general says misinformation has become an urgent threat to public health, an investigation by The Associated Press found a vocal and influential group of chiropractors has been capitalizing on the pandemic by sowing fear and mistrust of vaccines.
They have touted their supplements as alternatives to vaccines, written doctor’s notes to allow patients to get out of mask and immunization mandates, donated large sums of money to anti-vaccine organizations and sold anti-vaccine ads on Facebook and Instagram, the AP discovered. One chiropractor gave thousands of dollars to a Super PAC that hosted an anti-vaccine, pro-Donald Trump rally near the U.S. Capitol on Jan. 6.
They have also been the leading force behind anti-vaccine events like the one in Wisconsin, where hundreds of chiropractors from across the U.S. shelled out $299 or more to attend. The AP found chiropractors were allowed to earn continuing education credits to maintain their licenses in at least 10 states.
On this blog, I have often discussed that chiropractors tend to be anti-vax. It all goes back to their founding father, DD Palmer, who famously wrote:
- Vaccination and inoculation are pathological; chiropractic is physiological,
- and who in 1894, published his views on smallpox vaccination: ‘…the monstrous delusion … fastened on us by the medical profession, enforced by the state boards, and supported by the mass of unthinking people …’
- and who stated in 1896 that keeping tissue healthy is therefore the best prevention against infections; and this is best achieved by magnetic healing.
But that’s long ago! We are not like that anymore! … say the chiros of today.
Do you believe them?
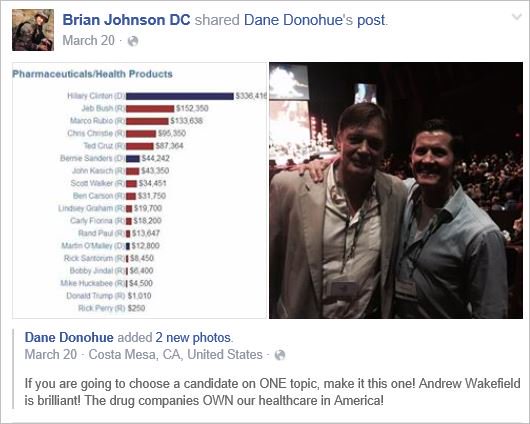
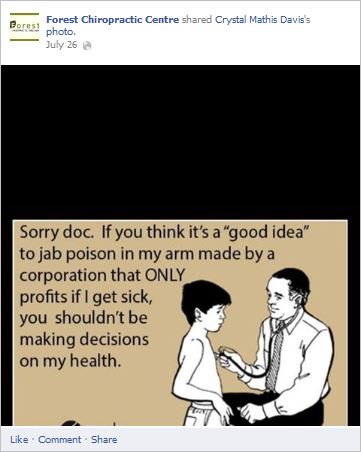
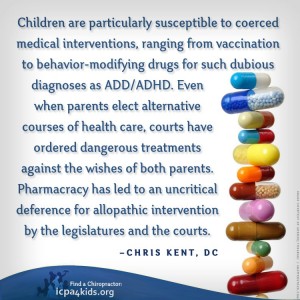
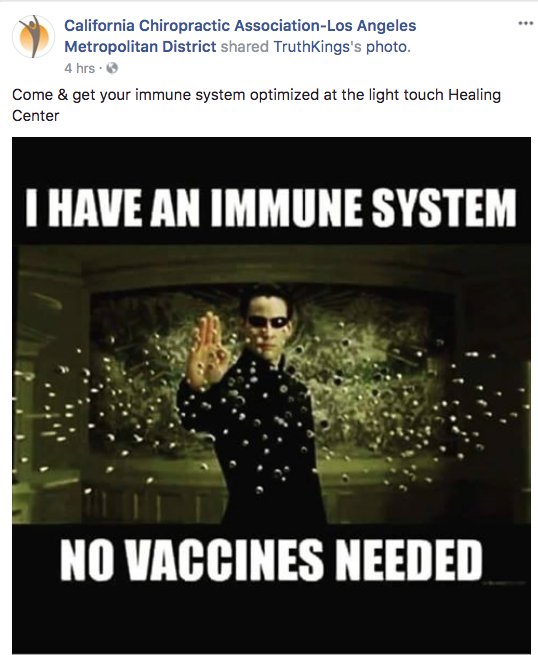
If so, you might want to read this article by Jann Bellamy. Or alternatively, just look at some of my finds from the Internet:
Practitioners of so-called alternative medicine (SCAM) regularly claim with great pride that they treat the ROOT CAUSES of disease. The claim has at least 4 effects:
- It distracts from the true causes of disease which are often multifactorial.
- It attracts customers to SCAM.
- It implies that conventional medicine is at best symptomatic and thus far inferior to SCAM.
- It encourages the patients of SCAM practitioners to turn their backs on mainstream healthcare.
The notion that SCAM practitioners treat the root causes is based on the practitioners’ understanding of etiology:
- If a traditional acupuncturist, for instance, becomes convinced that all disease is the expression of an imbalance of life-forces, and that needling acupuncture points will re-balance these forces thus restoring health, he must automatically assume that he is treating the root causes of any condition.
- If a chiropractor believes that all diseases are due to ‘subluxations’ of the spine, it must seem logical to him that spinal ‘adjustment’ is synonymous with treating the root cause of whatever complaint his patient is suffering from.
- If a Bowen therapist is convinced that “the Bowen Technique aims to balance the whole person, not just the symptoms“, he is bound to be equally sure that the root cause of “practically any problem can potentially be addressed” by this intervention.
- If a homeopath is convinced that all illness stems from a weakness of the ‘vital force’ and that only homeopathic remedies can revitalize it, they are likely to believe that their remedies tackle the root cause of all diseases.
- Etc., etc.
So, are SCAM practitioners correct when they claim to treat the root causes of disease?
When a root cause has been eliminated, the disease has been eliminated by its root. Treating a root cause, therefore, means that the disease is permanently cured. The above question can therefore be re-phrased as follows:
Is there any SCAM that cures any disease permanently?
I think the answer is NO. (At least, I know none. I would, however, be most grateful if someone could name one together with the evidence)
Even demonstrably effective forms of SCAM are effective only in terms of alleviating the symptoms. The one with the best evidence is probably St John’s wort. It works fine for mild to moderate depression. Yet, it does not cure depression: if we discontinue the treatment, the depression is likely to return.
And what about conventional medicine? Does it offer any permanent cures?
I have been searching and have to admit that I cannot find many either. Here is my list so far of diseases that are potentially curable (meaning they are unlikely to come back once the treatment has stopped and excluding disease prevention) with conventional medicine – and again, I would be really grateful if readers could add to my preliminary list:
- Acute emergencies, like anaphylaxis, cardiac arrest, etc.
- Bacterial infections (well most of them)
- Cancer (some), like Hodgkin lymphoma
- Malnutrition like beriberi of iron-deficiency anemia
- Phobias (some)
- Fungal infections (some)
- Poisonings (some)
- Many surgical indications such as appendicitis, gall stones, carpal tunnel syndrome, etc.
Not a long list, I admit (but better than nothing!) – so, please help me to prolong it by adding diseases that I did not mention.
THANKS
I was surprised to discover that there is an entire website by a homeopath. He used to comment regularly on my blog but eventually got banned (I think). Now that chap writes pages and pages explaining that my criticisms of homeopathy are all wrong and that I actually haven’t got a clue. This seems to suggest that his homeopathy is not very effective for anger control. The texts are so intensely funny that I took the liberty of copying a short passage for you (without altering a single word).
Here we go:
When I started this blog in 2013, it was aimed to rebut Professor Edzard Ernst’s scientific examination and critique of homeopathy.
After 7 years of engaging with his posts, I realised that he does not have a clue about homeopathy due to rejecting the central tenet of homeopathy that disorder of the vital force leads to disease and, over time, to incurable medical conditions.
This blog aims to dispel false notions about the philosophy and practice of homeopathy and I recommend that the widely used clinical approach to homeopathy is discarded and replaced with spiritual/dynamic approach to homeopathy that is aligned with the principles set out in Hahnemann’s Organon of Medicine.
Dr. Edzard Ernst has, for more than two decades, engaged in a comical and polemical critique of what he considers to be ‘homeopathy’:
- He does not hold a recognized qualification in homeopathy.
- His understanding of homeopathy has, from the very outset, been below par: See my post ‘Arnica’.
- He associated Bach Flower Remedies with ‘homeopathy’ because both use potentised substances.
- He included Berlin Wall remedy in his new book, a remedy that he referred to as homeopathy’s finest in one of his blogs. Berlin Wall originated in the imagination of Colin Griffith (‘New Materia Medica’: isn’t that hilarious?) and it is not listed in the official Homeopathic Pharmacopeia.
- He continues to write blogs about homeopathic treatment of certain clinical conditions and his study of the ‘adjunctive treatment’ of asthma with homeopathy is in opposition to Hahnemann’s instruction that no other medicines should be used during homeopathic treatment.
- He seems to be unable to understand that homeopathy does not treat medical conditions, and that for classical homeopathy, as set out by Kent, most ‘medical conditions’ are beyond the curable stage of homeopathic treatment.
- He seems not even to know in detail Hahnemann’s works: The Organon, Chronic Diseases, and Materia Medica Pura. Evidence of this is that, in 7 years, I never read a post that was written by him that engaged in a critique of these works.
- He writes silly blogs about Boris Johnson almost being a homeopath.
- He has, on last count, six pages of blogs written in derision and criticism of HRH Prince of Wales.
- In discussion, he even asks the question: ‘are you speaking out of your arse?’
- He did a bit of reading on the Russia collusion investigation that he seemed to think was negative against President Trump and worried that the Donald might start world war 3.
- He rated himself as the world’s number one researcher in SCAM (so called alternative medicine of which homeopathy is one of the major forms of treatment).
I rate him as the world’s number one clown-critic of homeopathy.
Before Dr. Ernst started his journey to become the world eminent critic of homeopathy (and every other alternative health modality), he could have done two things:
- Undertaken a meticulous study of the works by Samuel Hahnemann and James Tyler Kent in order to gain an understanding of what Homeopathy is. I have yet to read a post by Edzard Ernst that provides a critique of the original works on homeopathy by the founders of homeopathy. Instead, he seems to have preferred to bypass the tedious work of reading texts and substituted his own interpretation of homeopathy in his critical reviews of ‘homeopathy’.
In Dr. Ernst’s view, the central tenet of homeopathy that there is a ‘vital force’ (living intelligence) in the human body must be rejected because it is an ‘outdated’ concept of ‘vitalism’. It seems to me, from my reading of his posts, that he considers atheism and materialist epistemology to be self-evident and idealist epistemology to be obviously deluded. Edzard Ernst is obviously not the philosophical type because if he was then he would have realised that his rejection of the ‘principle of vitalism’ automatically invalidates homeopathy as a credible subject of scientific investigation. Why did he waste so much time studying something that is evidently nonsense?
- Before embarking on expensive and time consuming trials and meta analyses of homeopathy, Dr. Ernst ought to have first sought to find independently verified scientific evidence of homeopathic cures of non self-resolving clinical conditions and illnesses documented in clinical practice and publications. As far as I am aware, there is no hard medical scientific evidence that homeopathy cures any non self-resolving clinical conditions and illnesses and so how sensible was it that numerous researchers conducted RCTs over several decades to test whether or not homeopathy is an effective treatment for medical conditions?
END OF QUOTE
There is more, much more – and it’s all as hilarious as the above. So, whenever you are having a bad day and feeling a bit low, please read it. It is certain to cheer you up.
The global market for dietary supplements has grown continuously during the past years. In 2019, it amounted to around US$ 353 billion. The pandemic led to a further significant boost in sales. Evidently, many consumers listened to the sly promotion by the supplement industry. Thus they began to be convinced that supplements might stimulate their immune system and thus protect them against COVID-19 infections.
During the pre-pandemic years, the US sales figures had typically increased by about 5% year on year. In 2020, the increase amounted to a staggering 44 % (US$435 million) during the six weeks preceding April 5th, 2020 relative to the same period in 2019. The demand for multivitamins in the US reached a peak in March 2020 when sales figures had risen by 51.2 %. Total sales of vitamins and other supplements amounted to almost 120 million units for that period alone. In the UK, vitamin sales increased by 63 % and, in France, sales grew by around 40–60 % in March 2020 compared to the same period of the previous year.
Vis a vis such impressive sales figures, one should ask whether dietary supplements really do produce the benefit that consumers hope for. More precisely, is there any sound evidence that these supplements protect us from getting infected by COVID-19? In an attempt to answer this question, I conducted several Medline searches. Here are the conclusions of the relevant clinical trials and systematic reviews that I thus found:
- KSK (a polyherbal formulation from India’s Siddha system of medicine) significantly reduced SARS-CoV-2 viral load among asymptomatic COVID-19 cases and did not record any adverse effect, indicating the use of KSK in the strategy against COVID-19. Larger, multi-centric trials can strengthen the current findings.
- There is currently insufficient evidence to determine the benefits and harms of vitamin D supplementation as a treatment of COVID-19.
- Herbal supplements may help patients with COVID-19, zinc sulfate is likely to shorten the duration of olfactory dysfunction. DS therapy and herbal medicine appear to be safe and effective adjuvant therapies for patients with COVID-19. These results must be interpreted with caution due to the overall low quality of the included trials. More well-designed RCTs are needed in the future.
- No significant difference with vitamin-D supplementation on major health related outcomes in COVID-19.
- there is not enough evidence on the association between individual zinc status and COVID-19 infections and mortality.
- Omega-3 supplementation improved the levels of several parameters of respiratory and renal function in critically ill patients with COVID-19.
- A 5000 IU daily oral vitamin D3 supplementation for 2 weeks reduces the time to recovery for cough and gustatory sensory loss among patients with sub-optimal vitamin D status and mild to moderate COVID-19 symptoms. The use of 5000 IU vitamin D3 as an adjuvant therapy for COVID-19 patients with suboptimal vitamin D status, even for a short duration, is recommended.
- In this 2-sample MR study, we did not observe evidence to support an association between 25OHD levels and COVID-19 susceptibility, severity, or hospitalization. Hence, vitamin D supplementation as a means of protecting against worsened COVID-19 outcomes is not supported by genetic evidence.
- These antiviral and immune-modulating activities and their ability to stimulate interferon production recommend the use of probiotics as an adjunctive therapy to prevent COVID-19. Based on this extensive review of RCTs we suggest that probiotics are a rational complementary treatment for RTI diseases and a viable option to support faster recovery.
- In this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
- These findings neither support nor refute the claim that 3M3F alters the severity of COVID-19 or alleviates symptoms. More rigorous studies are required to properly ascertain the potential role of Chinese Herbal Medicine in COVID-19.
- NSO (Nigella sativa oil) supplementation was associated with faster recovery of symptoms than usual care alone for patients with mild COVID-19 infection. These potential therapeutic benefits require further exploration with placebo-controlled, double-blinded studies.
- The clinical application of LQ (Lianhua Qingwen Granules or Capsules ) on the treatment of COVID-19 has significant efficacy in improving clinical symptoms and reducing the rate of clinical change to severe or critical condition. Nevertheless, due to the limited quantity and quality of the included studies, more and higher quality trials with more observational indicators are expected to be published.
- The study identified some important potential traditional Indian medicinal herbs such as Ocimum tenuiflorum, Tinospora cordifolia, Achyranthes bidentata, Cinnamomum cassia, Cydonia oblonga, Embelin ribes, Justicia adhatoda, Momordica charantia, Withania somnifera, Zingiber officinale, Camphor, and Kabusura kudineer, which could be used in therapeutic strategies against SARS-CoV-2 infection.
- Shenhuang Granule is a promising integrative therapy for severe and critical COVID-19.
- Low-certainty or very low-certainty evidence demonstrated that oral CPM (Chinese patent medicine) may have add-on potential therapeutic effects for patients with non-serious COVID-19. These findings need to be further confirmed by well-designed clinical trials with adequate sample sizes.
- XYP (Xiyanping) injection is safe and effective in improving the recovery of patients with mild to moderate COVID-19. However, further studies are warranted to evaluate the efficacy of XYP in an expanded cohort comprising COVID-19 patients at different disease stages.
- Our meta-analysis of RCTs indicated that LH (Lianhuaqingwen) in combination with usual treatment may improve the clinical efficacy in patients with mild or moderate COVID-19 without increasing adverse events. However, given the limitations and poor quality of included trials in this study, further large-sample RCTs or high-quality real-world studies are needed to confirm our conclusions.
- Reduning injection might be effective and safe in patients with symptomatic COVID-19.
- In light of the safety and effectiveness profiles, LH (Lianhuaqingwen) capsules could be considered to ameliorate clinical symptoms of Covid-19.
- QPT (Qingfei Paidu Tang) was associated with a substantially lower risk of in-hospital mortality, without extra risk of acute liver injury or acute kidney injury among patients hospitalized with COVID-19.
- This community-based RCT found that the use of a herbal medicine therapy (Jinhaoartemisia antipyretic granules and Huoxiangzhengqi oral liquids) could significantly reduce the risks of the common cold among community-dwelling residents, suggesting that herbal medicine may be a useful approach for public health intervention to minimize preventable morbidity during COVID-19 outbreak.
- Based on unresolved controversies and inconclusive findings, it could be said that generally, a single and specific therapeutics to COVID-19 is still a mirage.
- Keguan-1-based integrative therapy was safe and superior to the standard therapy in suppressing the development of ARDS in COVID-19 patients.
Confused?
Me too!
Does the evidence justify the boom in sales of dietary supplements?
More specifically, is there good evidence that the products the US supplement industry is selling protect us against COVID-19 infections?
No, I don’t think so.
So, what precisely is behind the recent sales boom?
It surely is the claim that supplements protect us from Covid-19 which is being promoted in many different ways by the industry. In other words, we are being taken for a (very expensive) ride.
Exploring preventive therapeutic measures has been among the biggest challenges during the coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A team of Indian and US researchers explored the feasibility and methods of recruitment, retention, and potential signal of efficacy, of selected homeopathic medicines as a preventive measure for developing COVID-19 in a multi-group study.
A six-group, randomized, double-blind, placebo-controlled prophylaxis study was conducted in a COVID-19 exposed population in a quarantine facility in Mumbai, India. Each group received one of the following:
- Arsenicum album 30c,
- Bryonia alba 30c,
- Arsenicum album 30c, Bryonia alba 30c, Gelsemium sempervirens 30c, and Influenzinum 30c
- coronavirus nosode CVN01 30c,
- Camphora 1M,
- placebo.
Six pills twice a day were administered for 3 days. The primary outcome measure used was testing recruitment and retention in this quarantined setting. Secondary outcomes were numbers testing positive for COVID-19 after developing symptoms of illness, the number of subjects hospitalized, and days to recovery.
Good rates of recruitment and retention were achieved. Of 4,497 quarantined individuals, 2,343 sought enrollment, with 2,294 enrolled and 2,233 completing the trial (49.7% recruitment, 97.3% retention). Subjects who were randomized to either Bryonia alba (group 2) or to the CVN01 nosode (group 4) signaled a numerically lower incidence of laboratory-confirmed COVID-19 and a shorter period of illness, with evidence of fewer hospitalizations than those taking placebo. The three other groups did not show signals of efficacy.
The authors concluded that this pilot study supports the feasibility of a larger randomized, double-blind, placebo-controlled trial. Bryonia alba 30c and CVN01 30c should both be explored in disease prevention or shortening the course of disease symptomatology in a COVID-19-exposed population.
Signals of efficacy?
Are they kidding us?
The results failed to be statistically significant!
Hence the conclusions should be rewritten as follows:
This pilot study supports the feasibility of a larger trial in India where people have been told by an irresponsible government to believe in homeopathy. None of the 5 homeopathic treatments generated encouraging findings and none should be explored further. Studies of this nature must be discouraged firstly because homeopaths would not accept the findings of a trial of non-individualized homeopathy, and secondly because such trials will further confuse the public who might think that homeopathy is worth trying.
Traditional European Medicine (TEM) is an increasingly popular yet ill-defined term. Like Traditional Chinese Medicine (TCM), it encompasses all the traditional therapies from the respective region. One website describes it with this very odd graph:
On Medline, I found only very few papers on TEM. One article reported about a congress based on the concept of TEM but confusingly called it ‘European Traditional Medicine (ETM). Here are a few excerpts:
… the aim of this congress is to explore and survey, very old and modern traditional based therapies and treatments curing the principles of scientific medicine (1). Discussions of the links between ETM and other traditional medicines therefore are mandatory, particularly when considering the importance of traditionally based therapies that are still a source of primary health care to about 70 percent of the world’s population. Connections between traditional medicine and human health have been addressed and commented upon by many national and international political and sanitary bodies because: a) the good health of populations requires enlightened management of our social resources, economic relations, and of the natural world, and b) that many of today’s public-health issues have their roots in lack of scientifically sustainable holistic approach to the patient c) many socioeconomic inequalities and irrational consumption patterns that jeopardize the future economic sustainability of health.
In the same context the conventional biomedical approach to health is based on methods of diagnosing and treating specific pathologies: one pathogen = one disease, an approach that does not take into account connections between diseases, humanity, and some psychological aspects of suffering, and other socioeconomic factors such as poverty and education, and even the connections between disease and the environment in which sick people lives (2,3).
Other authors, like the one on this website, are much more concrete. Again, a few excerpts must suffice:
Bloodletting
When bloodletting according to Hildegard von Bingen max. 150 ml of blood taken. It is one of the most valuable and fastest detoxification options in TEM. In some people, no blood comes, because the body has no need to excrete something. For others, the doctor may say a lot about human health after the blood has been left for about 2 hours. If the serum is yellowish or whitish, this indicates excess fats. If certain threads form, they are signs of inflammation. Then the doctor gives recommendations for certain herbs and applications.
Wraps and packs
Whether neck wrap or hay flower sack. In TEM, there are many natural remedies made from natural materials (clay, pots) and herbs that support the body’s self-healing powers.
Wyda instead of yoga
Wyda is a holistic philosophy that is about getting in touch with yourself. In doing so, one can relax through flowing exercises and energy sounds, strengthen one’s mind or stimulate the metabolism. The exercises are similar in some ways to yoga. Here you can learn more about European yoga!
Which archetype are you?
In Traditional European Medicine (TEM), the archetype of a human is first determined so that the TEM doctor can coordinate the treatments. There are 4 temperatures:
Sanguine: He is active, open-hearted, energetic and mostly optimistic and cheerful. He is not resentful and does what he enjoys.
Suitable use: cool applications such as chest and liver wrap, whole body rubbings with grape seed and lemon balm oils.
Abandonment: too much sweet and fat, animal foods, sweet alcohol.
Choleric: He has a hot temper, shows leadership qualities, is prone to hyperbole, emotional and outbursts of anger, is extroverted, but often uncontrolled. Suitable application: cooling and calming applications. Massages with thistle, almond and lavender oils.
Avoidance of: too much animal protein, alcohol, hot spices and fatty foods.
Phlegmatic: enjoyment is important to him. He is reliable, can accomplish things, but seldom initiate. To get going causes him problems when he “runs”, then persistently and with energy.
Suitable application: warming and drying applications, warm chest wraps. Abdominal massages with camelina oil, marigold ointment.
Abandonment: too much sweets, milk, whole grains, tropical fruits, pork, too many carbohydrates.
Melancholic: He is an admonisher and a thinker, appreciates beauty and intelligence, is more introverted. He tends to ponder and pessimism, struggling for an activity.
Suitable use: warm applications such as warm chest wraps and liver wrap. Clay in water in the morning relieves gastrointestinal discomfort. Massages with strengthening cedar nut oil.
No: Frozen food, raw food, hard to digest, too much salt and sugar.
Yes, much of this is dangerous nostalgic nonsense that would lead us straight back into the dark ages.
Do we need more of this in so-called alternative medicine (SCAM)?
Definitely not!
TCM was created by Mao as a substitute for real medicine, at a time when China was desperately short of medicine. The creators of TEM have no such reason or motivation. So, why do they do it?
Search me!
I have repeatedly likened so-called alternative medicine (SCAM) to a cult – not a religious cult, of course, but to a ‘health cult’. A health cult is defined as a system for the cure of disease based on dogma set forth by its promulgator. So, are you a member of a health cult?
In case you are a proponent of SCAM, you might be in danger. Here are a few questions you should ask yourself:
- Is your SCAM based on dogma, such as ‘LIKE CURES LIKE’ or ‘SUBLUXATIONS ARE THE CAUSE OF DISEASE?
- Does the cult demand you accept its dogma or doctrine as truth?
- Is it set forth by a single guru or promulgator?
- Is your SCAM supposed to cure all ills?
- Is belief used by proponents of your SCAM as a substitute for evidence?
- Does the SCAM determine your diet and/or lifestyle?
- Does the SCAM exploit you financially?
- Does your SCAM impose rigid rules and regulations?
- Does your SCAM practice deception?
- Does your SCAM have its own sources of information/propaganda?
- Does your SCAM cultivate its own lingo?
- Does your SCAM discourage or inhibit critical thinking?
- Are questions about the values of your SCAM discouraged or forbidden?
- Do the proponents of your SCAM reduce complexities into platitudinous buzz words?
- Do they assume that health problems are the result of not adhering to the dogma?
- Does your SCAM instill fear into members who consider leaving?
- Do the proponents of your SCAM depict conventional medicine as ineffective or harmful?
- Are you asked to recruit new members to your SCAM?
Please try to answer these questions honestly and self-critically.
If more than a handful turn out to be positive, you have, in my view, a reason to be concerned. In this case, I would recommend you go to a library and start reading a few books that provide critical analyses of SCAM.
I was alerted to an interesting article about homeopathy in Switzerland. Its author points out that homeopathy is paid for by health insurance in Switzerland because of anything remotely related to evidence but because of a referendum in 2009. At the time, one of the arguments of the proponents was that health care costs would tend to decrease if more so-called alternative medicine (SCAM) would be paid for by the public purse. This is what Jacques de Haller, the president of the medical association, claimed: because SCAM is comparatively cheap and helps to prevent more expensive consultations, the total cost of health care would decrease.
This rather naive assumption was also one made in 2005 by the ‘Smallwood-Report’, commissioned by Charles and paid for by Dame Shirley Porter, specifically to inform health ministers. It stated that up to 480 million pounds could be saved if one in 10 family doctors offered homeopathy as an alternative to standard drugs. Savings of up to 3.5 billion pounds could be achieved by offering spinal manipulation rather than drugs to people with back pain. (Because I had commented on this report, Prince Charles’ first private secretary asked the vice-chancellor of Exeter University, Steve Smith, to investigate. Even though I was found to be not guilty of any wrongdoing, specifically of violating confidentiality, all local support stopped which led to my decision to retire early.)
In Switzerland, the assumption that SCAM saves money was refuted in 2019 by the Swiss health insurance association Santésuisse in a proper cost analysis. According to this analysis, doctors who also prescribed homeopathy caused 22% more costs per patient than those practicing conventional medicine. As it turned out, SCAM would be charged in addition to existing conventional medical services. Consequently, from a point of view of health economics, SCAM should not be called “alternative”, but rather “additive”, Santésuisse wrote at the time.
More evidence comes from a German study (authored by proponents of homeopathy!) that confirms these findings. Integrated care contracts for homeopathy by German health insurers were shown to result in higher costs across all diagnoses.
The recognition that homeopathy lacks sound evidence has already led to an end of reimbursement in the UK and France. Both in Germany and Switzerland, strong pro-homeopathy lobbies have so far succeeded in preventing similar actions. Yet, there is no doubt that, in these and other countries, the writing is on the wall.