Some time ago, I published ‘The 10 commandments of quackery’. Since then, I discovered that there are several errors that occur with such regularity in the comment section of this blog as well as in most other discussions about so-called alternative medicine (SCAM), that – in the hope to improve the logical reasoning of my readers (and often times my own) – it seems timely to publish the
10 ‘commandments’ of rational thought
- Thou shalt not confuse popularity of a therapy with its efficacy or safety (appeal to popularity).
- Thou shalt not assume that the test of time is a valid substitute for evidence (appeal to tradition).
- Thou shalt not believe that natural therapies are necessarily harmless (appeal to nature).
- Thou shalt not think that those who question your claim need to prove that you are wrong (reversal of the burden of proof).
- Thou shalt not assume that a therapy administered before a symptomatic improvement was necessarily the cause of that outcome (post hoc ergo propter hoc).
- Thou shalt not suppose that, because you do not know or understand an issue, it cannot be true (appeal to ignorance).
- Thou shalt not misrepresent your opponent’s position in order to make it easier for you to defeat it (straw man fallacy).
- Thou shalt not argue that, because others do wrong, you are permitted to do the same (tu quoque fallacy).
- Thou shalt not assume that your argument is correct because some authority agrees with you (appeal to authority).
- Thou shalt not attack your opponents instead of their arguments (ad hominem).
Yes, I know, one could add a lot more. But these 10 ‘commandments’ relate to the errors in rational thought that I feel would, if taken on board, be most useful in our discussions about SCAM.
A substantial proportion of consumers now use healthcare options known as so-called alternative medicine (SCAM). But why? This study aimed to understand the processes and decisional pathways through which chronic illness patients choose treatments outside of regular allopathic medicine.
It employed Charmaz’s constructivist grounded theory methods to collect and analyze data. Using theoretical sampling, 21 individuals suffering from chronic illness and who had used SCAM treatments participated in face-to-face in-depth interviews conducted in Miami/USA.
Seven overarching themes emerged from the data to describe how and why people with chronic illness choose SCAM treatments:
- influences,
- desperation,
- being averse to allopathic medicine and allopathic medical practice,
- curiosity and chance,
- ease of access,
- institutional help,
- trial and error.
The author concluded that in selecting treatment options that include SCAM, individuals draw on their social, economic, and biographical situations. Though exploratory, this study sheds light on some of the less examined reasons for SCAM use.
There already is a plethora of research on the reasons why people elect to try SCAM. Our own systematic review of 2011 was, in my view, more informative. Here is the abstract:
The aim of this review is to summarize the published evidence regarding the expectations of so-called alternative medicine (SCAM) users. We conducted electronic searches in MEDLINE and a hand search of our own files. Seventy-three articles met our inclusion criteria. A wide range of expectations emerged. In order of prevalence, they included:
- hope to influence the natural history of the disease;
- disease prevention and health/general well-being promotion;
- fewer side effects;
- being in control over one’s health;
- symptom relief;
- boosting the immune system;
- emotional support;
- holistic care;
- improving quality of life;
- relief of side effects of conventional medicine;
- good therapeutic relationship;
- obtaining information;
- coping better with illness;
- supporting the natural healing process;
- availability of treatment.
It is concluded that the expectations of SCAM users are currently not rigorously investigated. Future studies should have a clear focus on specific aspects of this broad question.
As our conclusion stated, the issue is too broad to be easily researchable. The question might need to be narrowed down. And even then, I ask myself, what might such investigations, even if done well, amount to? In what way would the results of such studies benefit anyone? How would they improve the healthcare of the future?
Perhaps someone can help me by suggesting some answers to these questions?
In staunch defiance of the evidence and common sense, Prince Charles has long defended homeopathy. Apparently, he not only uses it himself but also employs it for his animals. Claiming that his cattle don’t know about placebo effects, he seems convinced it works better than a placebo. Homeopaths are naturally delighted to have his royal support, not least the ones from India where homeopathy has been hugely popular for many years.
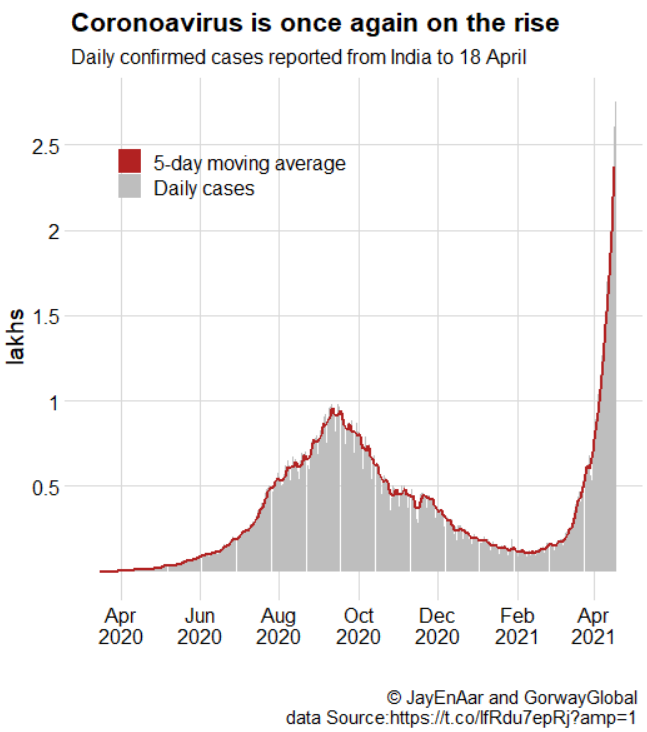
From the beginning of the pandemic, many Indian enthusiasts have claimed that homeopathy can effectively prevent and treat COVID-19 infections. In parts of India, homeopathy was thus employed on a population basis in an attempt to prevent the spread of the disease. There were voices that warned of a disaster but the Indian enthusiasm for homeopathy as an effective anti-COVID-19 therapy won the day.
When Prince Charles fell ill with COVID-19, Indian officials did not hesitate to claim that his quick recovery was due to the homeopathic treatment he had received. Charles’ officials denied this but in India, the story was reported widely and lent crucial support to the myth that homeopathy would provide a solution to the pandemic. Subsequently, Indian officials began to rely even more on the alleged power of homeopathy.
Today, the consequences of these actions are becoming tragically visible: With more than 15 million confirmed cases, India is experiencing a catastrophic tsunami of COVID-19 infections. Its healthcare system is close to collapse, and the high prevalence of the virus provides dangerously fertile grounds for the development of mutants. One does not need to be a clairvoyant to predict that, in turn, these will cause problems on a global basis.
Why am I telling you all this?
I think this depressing sequence of events shows in exemplary fashion what damage ill-informed VIP support for an ineffective therapy can do. Many people tend to feel that Charles’ passion for homeopathy might perhaps be laughable but is essentially harmless. I beg to differ. I am not saying that Charles instructed Indian officials to employ homeopathy the way they did. I am even emphasizing that Charles’ officials denied that homeopathy had anything to do with his speedy recovery after his illness. But I am saying that Charles’ life-long promotion of homeopathy combined with his quick recovery motivated Indian officials, even more, to ignore the evidence and decide to heavily rely on homeopathy.
This decision has cost uncounted lives and will cause many more in the near future. I submit that the seemingly harmless promotion of unproven or disproven treatments such as homeopathy can be a deadly dangerous game indeed.
In Germany, homeopathy had a free ride for a very long time. In recent years, however, several doctors, pharmacists, scientists, etc. have started opposing the fact that the public has to pay for ineffective treatments such as homeopathics. As a consequence, homeopaths have begun to fight back. The weapons they chose are often not the most subtle. Now they seem to have reached a new low; the Board of the German Central Association of Homeopathic Physicians (DZVhÄ) has sent an open letter to the Board of the German Society of Internal Medicine (DGIM) and to the participating colleagues of the 127th Congress of the DGIM from April 17 – 20, 2021 in an attempt to stop an invited lecture of a critic of homeopathy.
Here is my translation of the letter:
Dear colleagues on the board of the DGIM,
We were very surprised to read that an ENT colleague will speak on homeopathy at the 127th Congress of Internal Medicine. Dr. Lübbers is known up and down the country as a media-active campaigner against homeopathy. His “awakening experience” he had, according to his own account, when he had to fish homeopathic pills out of the ear of a child with otitis, since then he is engaged – no: not for better education, in the mentioned case of the parents or other users – against the method homeopathy (which was certainly not “guilty” of the improper application!).
It has surely not escaped you that in all media again and again only a small handful of self-proclaimed “experts” – all from the clique of the skeptic movement! – are heard on the subject of homeopathy. A single (!) fighter against homeopathy is a physician who completed her training in homeopathy and practices for a time as a homeopath. All the others come from non-medical and other occupational groups. In contrast, there are several thousand medical colleagues throughout Germany who stand on the ground of evidence-based medicine, have learned conventional medicine, implement it in their practices, and have completed a recognized continuing education program in homeopathy.
In the German Central Association of Homeopathic Physicians – the oldest medical professional association in Germany – 146 qualified internists are currently registered as members, in addition to numerous other medical specialists, all of whom are actively practicing medicine.
Question: Why does the German Society for Internal Medicine invite an ENT specialist, of all people, who lectures on homeopathy without any expertise of his own? Why not at least a specialist colleague in internal medicine? Or even a colleague who could report on the subject from her own scientific or practical experience? For example, on the topic of “hyperaldosteronism,” would you also invite a urologist or orthodontist? And if so, why?
Dear Board of Directors of the DGIM: As an honorary board member of the German Central Association of Homeopathic Physicians e.V.. (DZVhÄ) – and a specialist in internal medicine – I am quite sure that we could immediately name several colleagues with sufficient expertise as homeopathically trained and experienced internists, if you are really interested in a solid and correct discourse on the subject of homeopathy. Under the above-mentioned circumstances, there is, of course, rather the suspicion that it should not be about, but rather exclusively against homeopathy.
If it is planned for a later congress, e.g. in 2022, to deal again with the topic of homeopathy in a truly professionally well-founded and possibly even more balanced form: please contact us at any time! As medical colleagues, we are very interested in a fair and unprejudiced professional discourse.
Yours sincerely
Dr. med. Ulf Riker, Internist – Homeopathy – Naturopathy
2nd chairman DZVhÄ / 1st chairman LV Bayern
________________
What are Riker and the DZVhÄ trying to say with this ill-advised, convoluted, and poorly written letter?
Let me try to put his points a little clearer:
- They are upset that the congress of internists invited a non-homeopath to give a lecture about homeopathy.
- The person in question, Dr. Lübbers, is an ENT specialist and, like all other German critics of homeopathy (apart from one, Dr. Grams), does not understand homeopathy.
- There are thousands of physicians who do understand it and are fully trained in homeopathy.
- They would therefore do a much better job in providing a lecture.
- So, would the German internists please invite homeopaths for their future meetings?
And what is Riker trying to achieve?
- It seems quite clear that he aims to prevent criticism of homeopathy.
- He wishes to replace it with pro-homeopathy propaganda.
- Essentially he wants to stifle free speech, it seems to me.
To reach these aims, he does not hesitate to embarrass himself by sending and making publicly available a very stupid letter. He also behaves in a most unprofessional fashion and does not mind putting a few untruths on paper.
Having said that, I will admit that they are in good company. Hahnemann was by all accounts a most intolerant and cantankerous chap himself. And during the last 200 years, his followers have given ample evidence that critical thinking has remained an alien concept for them. Consequently, such behavior seems not that unusual for German defenders of homeopathy. In recent times they have:
- Made the results of the largest investigation into homeopathy disappear because its results were devastatingly negative.
- Went to Liberia to cure Ebola with homeopathy.
- Published lots of untruths and exaggerations.
- Hired a journalist to systematically defame me and other critics.
- Likened critics to Roland Freisler, the infamous judge of the Nazi era.
- Threatened critics with legal action.
- Started a media campaign to promote homeopathy.
- Published libelous statements about me.
Quite a track record, wouldn’t you agree?
But, I think, attempting to suppress free speech beats it all and must be a new low in the history of homeopathy.
Energy healing is an umbrella term for a range of paranormal healing practices. Their common denominator is the belief in a mystical ‘energy’ that can be used for therapeutic purposes. Forms of energy healing have existed in many ancient cultures. The ‘New Age’ movement has brought about a revival of these ideas, and today energy healing systems are amongst the most popular alternative therapies in the US as well as in many other countries.
Energy healing relies on the esoteric belief in some form of ‘energy’ which is distinct from the concept of energy understood in physics and refers to some life force such as chi in Traditional Chinese Medicine, or prana in Ayurvedic medicine. Some proponents employ terminology from quantum physics and other ‘cutting-edge’ science to give their treatments a scientific flair which, upon closer scrutiny, turns out to be but a veneer of pseudo-science. The ‘energy’ that energy healers refer to is not measurable and lacks biological plausibility.
The purpose of this study was to evaluate the effects of energy healing (EH) therapy prior to and following posterior surgical correction for adolescent idiopathic scoliosis (AIS) compared to controls.
Patients were prospectively randomized to one of two groups: standard operative care for surgery (controls) vs. standard care with the addition of three EH sessions. The outcomes included visual analog scales (VAS) for pain and anxiety (0-10), days until conversion to oral pain medication, and length of hospital stay. For the experimental group, VAS was assessed pre- and post-EH session.
Fifty patients were enrolled-28 controls and 22 EH patients. The controls had a median of 12 levels fused vs. 11 in the EH group (p = 0.04). Pre-operative thoracic and lumbar curve magnitudes were similar (p > 0.05). Overall VAS pain scores increased from pre- to post-operative (p < 0.001), whereas the VAS anxiety scores decreased immediately post-operative (p < 0.001). The control and pre-EH assessments were statistically similar. Significant decreases in VAS pain and anxiety scores from pre to post-EH assessments were noted for the EH group. Both groups transitioned to oral pain medication a median of 2 days post-operative (p = 0.11). The median days to discharge were four in the controls and three in the EH group (p = 0.07).
The authors concluded that EH therapy resulted in a decrease in patient’s pre-operative anxiety. Offering this CAM modality may enhance the wellbeing of the patient and their overall recovery when undergoing posterior surgical correction for AIS.
I am getting tired of explaining that this trial design tells us as good as nothing about the effects of the tested therapy per se. As we have discussed ad nauseam on this blog, A+B is always more than B alone. Such trials appear to be rigorous and fool many people, but they are unable to control for context effects, like placebo or attention. Therefore, I need to re-write the conclusions:
The placebo effect and the extra attention associated with EH therapy resulted in a decrease in patients’ pre-operative anxiety. EH itself is most likely bar any effect. Further studies in this area are not required.
Absurd claims about spinal manipulative therapy (SMT) improving immune function have increased substantially during the COVID-19 pandemic. Is there any basis at all for such notions?
The objective of this systematic review was to identify, appraise, and synthesize the scientific literature on the efficacy and effectiveness of SMT in preventing the development of infectious disease or improving disease-specific outcomes in patients with infectious disease and to examine the association between SMT and selected immunological, endocrine, and other physiological biomarkers.
A literature search of MEDLINE, the Cumulative Index to Nursing and Allied Health Literature, the Index to Chiropractic Literature, the Cochrane Central Register of Controlled Trials, and Embase was conducted. Randomized clinical trials and cohort studies were included. Eligible studies were critically appraised, and evidence with high and acceptable quality was synthesized using the Synthesis Without Meta-Analysis guideline.
A total of 2593 records were retrieved; after exclusions, 50 full-text articles were screened, and 16 articles reporting the findings of 13 studies comprising 795 participants were critically appraised. No clinical studies were located that investigated the efficacy or effectiveness of SMT in preventing the development of infectious disease or improving disease-specific outcomes among patients with infectious disease. Eight articles reporting the results of 6 high- and acceptable-quality RCTs comprising 529 participants investigated the effect of SMT on biomarkers. Spinal manipulative therapy was not associated with changes in lymphocyte levels or physiological markers among patients with low back pain or participants who were asymptomatic compared with sham manipulation, a lecture series, and venipuncture control groups. Spinal manipulative therapy was associated with short-term changes in selected immunological biomarkers among asymptomatic participants compared with sham manipulation, a lecture series, and venipuncture control groups.
The authors concluded that no clinical evidence was found to support or refute claims that SMT was efficacious or effective in changing immune system outcomes. Although there were limited preliminary data from basic scientific studies suggesting that SMT may be associated with short-term changes in immunological and endocrine biomarkers, the clinical relevance of these findings is unknown. Given the lack of evidence that SMT is associated with the prevention of infectious diseases or improvements in immune function, further studies should be completed before claims of efficacy or effectiveness are made.
I fully agree with the data as summarised in this paper. Yet, I find the conclusions a bit odd. The authors of this paper are chiropractors who declare the following conflicts of interest: Dr Côté reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Research Foundation, travel expenses from the World Federation of Chiropractic, and personal fees from the Canadian Chiropractic Protective Association outside the submitted work. Dr Cancelliere reported receiving grants from the Canadian Chiropractic Research Foundation outside the submitted work. Dr Mior reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Association and the Ontario Chiropractic Association outside the submitted work. Dr Hogg-Johnson reported receiving grants from the College of Chiropractors of British Columbia during the conduct of the study and grants from the Canadian Chiropractic Research Foundation outside the submitted work. No other disclosures were reported. The research was supported by funding from the College of Chiropractors of British Columbia to Ontario Tech University, the Canada Research Chairs program (Dr Côté), and the Canadian Chiropractic Research Foundation (Dr Cancelliere).
Would authors independent of chiropractic influence have drawn the same conclusions? I doubt it! While I do appreciate that chiropractors published these negative findings prominently, I feel the conclusions could easily be put much clearer:
There is no clinical evidence to support claims that SMT is efficacious or effective in changing immune system outcomes. Further studies in this area are not warranted.
Battlefield Acupuncture (BFA) – I presume the name comes from the fact that it is so simple, it could even be used under combat situations – is a form of ear acupuncture developed 20 years ago by Dr Richard Niemtzow. BFA employs gold semipermanent needles that are placed at up to 5 specific sites in one or both ears. The BFA needles are small conical darts that pierce the outer ear in designated locations and remain in place until they fall out typically within 3–4 days.
The US Defense and Veterans Center for Integrative Pain Management and the Veterans Health Administration National Pain Management Program Office recently completed a 3-year acupuncture education and training program, which deployed certified BFA trainers for the Department of Defense and Veterans Administration medical centers. Over 2800 practitioners were thus trained to provide BFA. The total costs amounted to $ 5.4 million.
This clearly begs the question:
DOES IT WORK?
This review aims to investigate the effects and safety of BFA in adults with pain. Electronic databases were searched for randomized controlled trials (RCTs) published in English evaluating efficacy and safety of BFA in adults with pain, from database inception to September 6, 2019. The primary outcome was pain intensity change, and the secondary outcome was safety. Nine RCTs were included in this review, and five trials involving 344 participants were analyzed quantitatively. Compared with no intervention, usual care, sham BFA, and delayed BFA interventions, BFA had no significant improvement in the pain intensity felt by adults suffering from pain. Few adverse effects (AEs) were reported with BFA therapy, but they were mild and transitory.
The authors of this review concluded that BFA is a safe, rapid, and easily learned acupuncture technique, mainly used in acute pain management, but no significant efficacy was found in adult individuals with pain, compared with the control groups. Given the poor methodological quality of the included studies, high-quality RCTs with rigorous evaluation methods are needed in the future.
And here are my comments:
- SAFE? Impossible to tell on the basis of 344 patients.
- RAPID? True, but meaningless, as it does not work.
- EASILY LEARNT? True, it’s simple and seems ever so stupid.
- NO SIGNIFICANT EFFICACY? That I can easily believe.
I am amazed that anyone would fall for an idea as naive as BFA. That it should be the US military is simply hilarious, in my view. I am furthermore baffled that anyone recommends more study of such monumental nonsense.
Why, oh why?
Acupuncture is far-fetched (to put it mildly). Ear acupuncture is positively ridiculous. BFA seems beyond ridiculous and must be the biggest military hoax since general Grigory Aleksandrovich Potemkin painted façades to fool Catherine the Great into thinking that an area was far richer than it truly was.
Low back pain must be one of the most frequent reasons for patients to seek out some so-called alternative medicine (SCAM). It would therefore be important that the information they get is sound. But is it?
The present study sought to assess the quality of web-based consumer health information available at the intersection of LBP and CAM. The investigators searched Google using six unique search terms across four English-speaking countries. Eligible websites contained consumer health information in the context of CAM for LBP. They used the DISCERN instrument, which consists of a standardized scoring system with a Likert scale from one to five across 16 questions, to conduct a quality assessment of websites.
Across 480 websites identified, 32 were deemed eligible and assessed using the DISCERN instrument. The mean overall rating across all websites 3.47 (SD = 0.70); Summed DISCERN scores across all websites ranged from 25.5-68.0, with a mean of 53.25 (SD = 10.41); the mean overall rating across all websites 3.47 (SD = 0.70). Most websites reported the benefits of numerous CAM treatment options and provided relevant information for the target audience clearly, but did not adequately report the risks or adverse side-effects adequately.
The authors concluded that despite some high-quality resources identified, our findings highlight the varying quality of consumer health information available online at the intersection of LBP and CAM. Healthcare providers should be involved in the guidance of patients’ online information-seeking.
In the past, I have conducted several similar surveys, for instance, this one:
Background: Low back pain (LBP) is expected to globally affect up to 80% of individuals at some point during their lifetime. While conventional LBP therapies are effective, they may result in adverse side-effects. It is thus common for patients to seek information about complementary and alternative medicine (CAM) online to either supplement or even replace their conventional LBP care. The present study sought to assess the quality of web-based consumer health information available at the intersection of LBP and CAM.
Methods: We searched Google using six unique search terms across four English-speaking countries. Eligible websites contained consumer health information in the context of CAM for LBP. We used the DISCERN instrument, which consists of a standardized scoring system with a Likert scale from one to five across 16 questions, to conduct a quality assessment of websites.
Results: Across 480 websites identified, 32 were deemed eligible and assessed using the DISCERN instrument. The mean overall rating across all websites 3.47 (SD = 0.70); Summed DISCERN scores across all websites ranged from 25.5-68.0, with a mean of 53.25 (SD = 10.41); the mean overall rating across all websites 3.47 (SD = 0.70). Most websites reported the benefits of numerous CAM treatment options and provided relevant information for the target audience clearly, but did not adequately report the risks or adverse side-effects adequately.
Conclusion: Despite some high-quality resources identified, our findings highlight the varying quality of consumer health information available online at the intersection of LBP and CAM. Healthcare providers should be involved in the guidance of patients’ online information-seeking.
Or this one:
Background: Some chiropractors and their associations claim that chiropractic is effective for conditions that lack sound supporting evidence or scientific rationale. This study therefore sought to determine the frequency of World Wide Web claims of chiropractors and their associations to treat, asthma, headache/migraine, infant colic, colic, ear infection/earache/otitis media, neck pain, whiplash (not supported by sound evidence), and lower back pain (supported by some evidence).
Methods: A review of 200 chiropractor websites and 9 chiropractic associations’ World Wide Web claims in Australia, Canada, New Zealand, the United Kingdom, and the United States was conducted between 1 October 2008 and 26 November 2008. The outcome measure was claims (either direct or indirect) regarding the eight reviewed conditions, made in the context of chiropractic treatment.
Results: We found evidence that 190 (95%) chiropractor websites made unsubstantiated claims regarding at least one of the conditions. When colic and infant colic data were collapsed into one heading, there was evidence that 76 (38%) chiropractor websites made unsubstantiated claims about all the conditions not supported by sound evidence. Fifty-six (28%) websites and 4 of the 9 (44%) associations made claims about lower back pain, whereas 179 (90%) websites and all 9 associations made unsubstantiated claims about headache/migraine. Unsubstantiated claims were made about asthma, ear infection/earache/otitis media, neck pain,
Conclusions: The majority of chiropractors and their associations in the English-speaking world seem to make therapeutic claims that are not supported by sound evidence, whilst only 28% of chiropractor websites promote lower back pain, which is supported by some evidence. We suggest the ubiquity of the unsubstantiated claims constitutes an ethical and public health issue.
The findings were invariably disappointing and confirmed those of the above paper. As it is nearly impossible to do much about this lamentable situation, I can only think of two strategies for creating progress:
- Advise patients not to rely on Internet information about SCAM.
- Provide reliable information for the public.
Both describe the raison d’etre of my blog pretty well.
Recently, I came across a newspaper asking: “Which vaccine do you trust most?” It turned out that there was a clear favourite according to public opinion. In the present climate of heated debates about COVID vaccines, this seems to make sense.
Or doesn’t it?
What determines public opinion?
There are probably many determinants, but most are dominated by what the public is being told about a subject. If, for instance, the press incessantly reports bad things about a certain vaccine and mostly good news about another, public opinion will reflect exactly that.
What I am trying to point out is this: the man and woman in the street have no expertise in vaccines. They mostly think what they are being told about them. So, public opinion is largely determined by journalists who write about the subject. If then a newspaper presents the public opinion about a vaccine, it is all but a foregone conclusion. The paper might as well just repeat what they have been telling their readers. By presenting a ‘public opinion’ about vaccines they actually go one step further: they amplify their own opinion by pretending it is not of their making but that of the public.
All this seems fairly obvious, once you start thinking about it.
So, why do I go on about it?
If this phenomenon occurs with vaccines, it also occurs with other issues, for instance, so-called alternative medicine (SCAM). We often hear that the public is in favour of this or that type of SCAM. It is supposed to convince us and politicians that SCAM is good. If thousands or even millions are in favour of it, it must be good! Who am I to disagree with the public?
But, as we have just seen with the example of the vaccines, public opinion is merely a reflection of what the press tells people. The man and the woman in the street are not competent to reliably estimate the risk-benefit ratios of St John’s wort, Arnica, glucosamine, acupuncture, etc. etc. They can judge such issues as little as they can judge the risk-benefit balance of a vaccine. They rely on information from the outside, and that information usually reaches them by the press.
What am I aiming at?
Public opinion sounds impressive, and in the realm of SCAM, it often determines much. If the public opinion is in favour of homoeopathy, for instance, politicians are likely to lend their support to it. Yet, public opinion is just OPINION! It cannot be used as an indicator for the efficacy or safety of medical interventions, and it cannot be the reason for using or rejecting them.
It follows, I think, that journalists have a huge responsibility to inform the public correctly on SCAM (and any other matter). On this blog, we have seen numerous instances of journalists who could have done better, e.g.:
- “Scientists have shown how homeopathy works” – journalists’ obsession with ‘balance’
- ACUPUNCTURE: journalists, be aware of your responsibility not to mislead the public
- “Chiropractic treatments are too dangerous…” A TALE OF POOR JOURNALISM (by the Daily Mail)
- SUCCESS: my first official complaint about a newspaper article
- Recklessly stupid TCM-promotion by the ‘Daily Mail’
- Beware of the alkaline diet and the claims made for it! A plea for journalistic accuracy
- Ear-candles, a TV-doctor, THE DAILY MAIL, and journalistic ‘balance’
- Irresponsible promotion of quackery even by the ‘respectable’ press
Public opinion, it seems to me, can only be meaningful, if the information fed to the public is sound. And when it comes to SCAM, this condition is often not met.
Previous studies have shown inconclusive results of homeopathy in the treatment of warts. A team of Indian homeopaths aimed to assess the feasibility of a future definitive trial, with a preliminary assessment of differences between effects of individualized homeopathic (IH) medicines and placebos in the treatment of cutaneous warts.
A double-blind, randomized, placebo-controlled trial (n = 60) was conducted at the dermatology outpatient department of D.N. De Homoeopathic Medical College and Hospital, West Bengal. Patients were randomized to receive either IH (n = 30) or identical-looking placebo (n = 30). Primary outcome measures were numbers and sizes of warts; the secondary outcome was the Dermatology Life Quality Index (DLQI) questionnaire measured at baseline, and every month up to 3 months. Group differences and effect sizes were calculated on the intention-to-treat sample.
Attrition rate was 11.6% (IH, 3; placebo, 4). Intra-group changes were significantly greater (all p < 0.05, Friedman tests) in IH than placebo. Inter-group differences were statistically non-significant (all p > 0.05, Mann-Whitney U tests) with small effect sizes-both in the primary outcomes (number of warts after 3 months: IH median [inter-quartile range; IQR] 1 [1, 3] vs. placebo 1 [1, 2]; p = 0.741; size of warts after 3 months: IH 5.6 mm [2.6, 40.2] vs. placebo 6.3 [0.8, 16.7]; p = 0.515) and in the secondary outcomes (DLQI total after 3 months: IH 4.5 [2, 6.2] vs. placebo 4.5 [2.5, 8]; p = 0.935). Thuja occidentalis (28.3%), Natrum muriaticum (10%) and Sulphur (8.3%) were the most frequently prescribed medicines. No harms, homeopathic aggravations, or serious adverse events were reported.
The Indian homeopaths draw the following conclusion: As regards efficacy, the preliminary study was inconclusive, with a statistically non-significant direction of effect favoring homeopathy. The trial succeeded in showing that an adequately powered definitive trial is both feasible and warranted.
INCONCLUSIVE?
No, the findings are not inconclusive at all! Read the results again: they confirm that homeopathy is a placebo therapy.
So, why is this trial worth writing about?
Surely, we did not expect anything else than a negative outcome from such a study?!
No, we didn’t.
But there is still something quite remarkable about this study: I have previously noted that virtually all studies of homeopathy by Indian researchers report positive results. AND THIS ONE DOESN’T!!!
Alright, it tries to hide the fact that the findings were negative, but this already seems to be a step in the right direction. So, well done, my Indian friends!!!
Perhaps one day, you will be able to admit that homeopathy is a placebo therapy?