symptom-relief
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
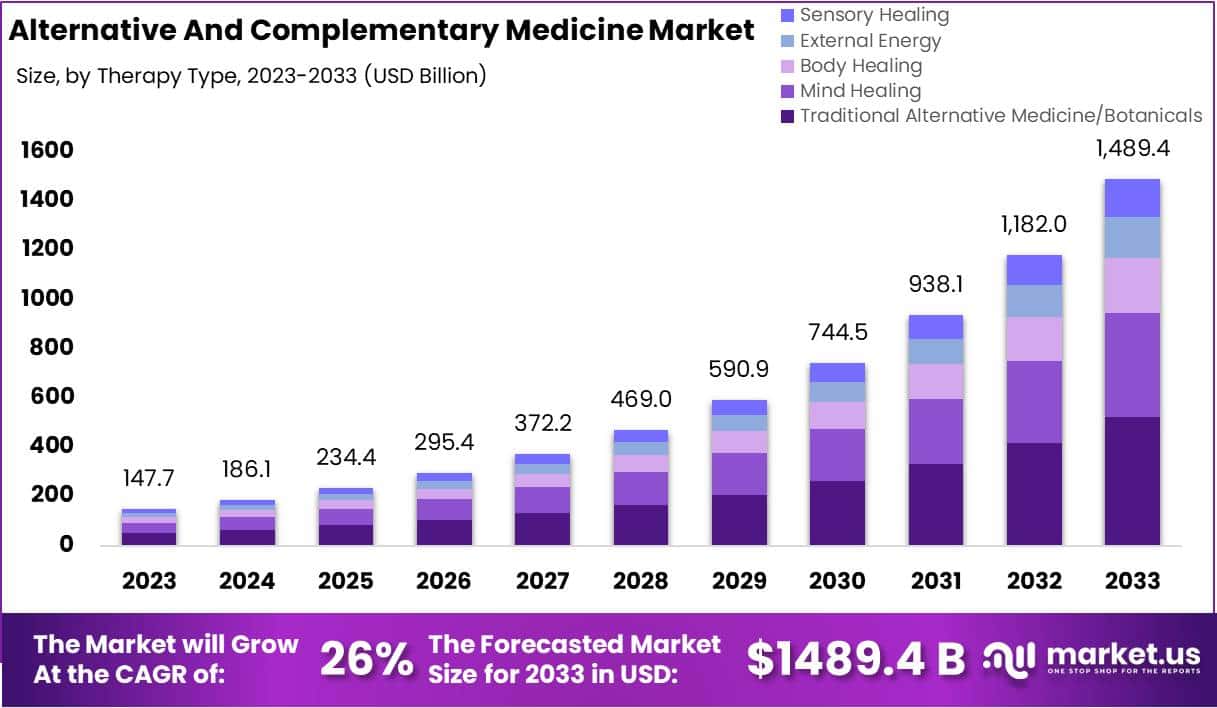
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.
Acute Otitis Media (AOM) is one of the most common acute infections in children and often injudiciously treated by antibiotics. Homeopathy has been claimed to work but is it really effective?
This open label, randomized, controlled, parallel arm trial was conducted on children (aged 0–12 years), suffering from AOM. The primary outcome was changes in Tympanic Membrane Examination scale (TMES) and Acute Otitis Media-Severity of Symptoms (AOM-SOS) scale, time to improvement in pain through Facial Pain Scale-Revised (FPS-R) over 10 days. The need for antibiotics in both groups and the recurrence of subsequent episodes of AOM over 12 months were also compared.
Intention-to-treat analysis was performed on 222 children; Homeopathy (n = 117) (H-group), Allopathy (A-group) (n = 105). There was a statistically significant reduction of scores in H-group compared with A-group at each time point: at day 3 (mean diff. ± sd: 1.71 ± 0.19; 95% CI: 1.34 to 2.07; p = 0.0001), at day 7 (mean diff. ± sd: 1.29 ± 0.24; 95% CI: 0.82 to 1.76; p = 0.0001) and at day 10 (mean diff. ± sd: 1.23 ± 0.25; 95% CI = 0.74 to 1.71; p = 0.0001) favoring homeopathy. Clinical failure by the third day of treatment was observed in 11% and 24% of children in H-group vs A-group (OR: 0.03; 95% CI: 0.001 to 0.52; p = 0.03). None of the children in the H-group required antibiotics, whereas 14 children in the A-group did.
The authors concluded that both therapies seemed to produce comparable effects and appeared safe. The study consolidated the findings observed during a pilot study, i.e., homeopathy is non-inferior to allopathy in managing AOM in children and antibiotics in children can be avoided.
This study was published in the journal ‘Homeopathy’ and originates from the Central Council for Research in Homeopathy, New Delhi, India. Sadly, I do not have the full text of the paper and cannot therefore scrutinize it adequately.
Let me just mention these three facts:
- The journal ‘Homeopathy’ never publishes negative results.
- Indian researchers of homeopathy publish as good as no negative results.
- As far as I can see, the Central Council for Research in Homeopathy, New Delhi, has never published a negative result.
These points do, of course, not necessarily mean that the study is false-positive, but they do not inspire me with confidence. In any case, it seems wise to insist on better evidence. To render it credible, we would need:
- Several rigorous RCTs that test homeopathy for AOM against placebo.
- If (and only then) they show that homeopathy is better than placebo, at least one independent replication of the present study.
As the biological plausibility of all this is close to zero, the chances that this will happen are also zero.
Of all the forms of so-called alternative medicine (SCAM), Reiki is amongst the least plausible. It is a form of paranormal or ‘energy healing’ popularised by Japanese Mikao Usui (1865–1926). Reiki is based on the assumptions of Traditional Chinese Medicine and the existence of ‘chi’, the life-force that is assumed to determine our health.
Reiki practitioners believe that, with their hands-on healing method, they can transfer ‘healing energy’ to a patient which, in turn, stimulates the self-healing properties of the body. They assume that the therapeutic effects of this technique are obtained from a ‘universal life energy’ that provides strength, harmony, and balance to the body and mind.
Despite its implausibility, Reiki is used for a very wide range of conditions. Some people are even convinced that it has positive effects on sexuality. But is that really so?
This randomised clinical trial was aimed at finding out. Specifically, its authors wanted to determine the effect of Reiki on sexual function and sexual self-confidence in women with sexual distress*. It was was conducted with women between the ages of 15–49 years who were registered at a family health center in the eastern region of Turkey and had sexual distress.
The sample of the study consisted of 106 women, 53 in the experimental group and 53 in the control group. Women in the experimental group received Reiki once a week for four weeks, while no intervention was applied to those in the control group. Data were collected using the Female Sexual Distress Scale-Revised (FSDS-R), the Arizona Sexual Experiences Scale (ASEX), and the Sexual Self-confidence Scale (SSS).
The levels of sexual distress, sexual function, and sexual self-confidence of women in both groups were similar before the intervention, and the difference between the groups was not statistically significant (p > 0.05). After the Reiki application, the FSDS-R and ASEX mean scores of women in the experimental group significantly decreased, while their SSS mean score significantly increased, and the difference between the groups was statistically significant (p < 0.05).
The authors concluded that Reiki was associated with reduced sexual distress, positive outcomes in sexual functions, and increase sexual self-confidence in women with sexual distress. Healthcare professionals may find Reiki to positively enhance women’s sexuality.
Convinced?
I hope not!
The study has the most obvious of all design flaws: it does not control for a placebo effect, nor the effect of empaty/sympathy received from the therapist, nor the negative impact of learning that you are in the control group and will thus not receive any treatment or attention.
To me, it is obvious that these three factors combined must be able to bring about the observed outcomes. Therefore, I suggest to re-write the conclusions as follows:
The intervention was associated with reduced sexual distress, positive outcomes in sexual functions, and increase sexual self-confidence in women with sexual distress. Considering the biological plausibility of a specific effect of Reiki, the most likely cause for the outcome are non-specific effects of the ritual.
*[Sexual distress refers to persistent, recurrent problems with sexual response, desire, orgasm or pain that distress you or strain your relationship with your partner. Yes, I had to look up the definition of that diagnosis.]
Current interventions for posttraumatic stress disorder (PTSD) are efficacious, yet effectiveness may be limited by adverse effects and high withdrawal rates. Acupuncture is an intervention with some positive preliminary but methodologically flawed data for PTSD. Therefore a new study compared verum acupuncture with sham acupuncture (minimal needling) on clinical and physiological outcomes.
This was a 2-arm, parallel-group, prospective blinded randomized clinical trial hypothesizing superiority of verum to sham acupuncture. The study was conducted at a single outpatient-based site, the Tibor Rubin VA Medical Center in Long Beach, California, with recruitment from April 2018 to May 2022, followed by a 15-week treatment period. Following exclusion for characteristics that are known PTSD treatment confounds, might affect biological assessment, indicate past nonadherence or treatment resistance, or indicate risk of harm, 93 treatment-seeking combat veterans with PTSD aged 18 to 55 years were allocated to group by adaptive randomization and 71 participants completed the intervention protocols.
Verum and sham were provided as 1-hour sessions, twice weekly, and participants were given 15 weeks to complete up to 24 sessions. The primary outcome was pretreatment to posttreatment change in PTSD symptom severity on the Clinician-Administered PTSD Scale-5 (CAPS-5). The secondary outcome was pretreatment to posttreatment change in fear-conditioned extinction, assessed by fear-potentiated startle response. Outcomes were assessed at pretreatment, midtreatment, and posttreatment. General linear models comparing within- and between-group were analyzed in both intention-to-treat (ITT) and treatment-completed models.
A total of 85 male and 8 female veterans (mean [SD] age, 39.2 [8.5] years) were randomized. There was a large treatment effect of verum (Cohen d, 1.17), a moderate effect of sham (d, 0.67), and a moderate between-group effect favoring verum (mean [SD] Δ, 7.1 [11.8]; t90 = 2.87, d, 0.63; P = .005) in the intention-to-treat analysis. The effect pattern was similar in the treatment-completed analysis: verum d, 1.53; sham d, 0.86; between-group mean (SD) Δ, 7.4 (11.7); t69 = 2.64; d, 0.63; P = .01). There was a significant pretreatment to posttreatment reduction of fear-potentiated startle during extinction (ie, better fear extinction) in the verum but not the sham group and a significant correlation (r = 0.31) between symptom reduction and fear extinction. Withdrawal rates were low.
The authors concluded that the acupuncture intervention used in this study was clinically efficacious and favorably affected the psychobiology of PTSD in combat veterans. These data build on extant literature and suggest that clinical implementation of acupuncture for PTSD, along with further research about comparative efficacy, durability, and mechanisms of effects, is warranted.
I am not sure that the authors’ enthusiastic verdict is correct. Its lead author was even quoted stating that his study, which used improved controls, was needed to “definitively” support acupuncture for PTSD. He noted that “acupuncture ought to be considered a potential first-line treatment for PTSD.”
While the study is an improvement on the previous research in this area, it is by no means compelling. My main point of criticism is the nature of the sham acupuncture. Such controls are used to account for placebo effects which, of course, can be considerable in the case of acupuncture.
For this concept to work adequately, the patient and the therapist need to be blinded. In the case of acupuncture, therapist blinding is difficult (but not impossible). In this study, therepists were not blinded. Thus they could have influenced the outcome by verbal and non-verbal clues given to the patient. As acupuncturists inevitably have an interest in the positive result of their study, this effect seems inevitable to me.
More important, however, is the adequate blinding of the patient. In this study, it was attempted by using shallow needling as a sham intervention. Yet, shallow needling can easily distinguished from real acupuncture by the patient. At the very least, patients should be asked what treatment – sham or real – they thought they had received. This did not happen, and we therefore might assume that the effect of patient de-blinding – combined with the confounder described above – was sufficient to bring about the relatively small effect sizes observed by the authors.
One might argue that this does not really matter; all that counts is to alleviate the suffering of the patients, never mind by what mechanism. I think, this would be erroneous. It matters because, if acupuncture itself is ineffective (which I suggest), settling for acupuncture as a first line therapy for PTSD is in nobody’s interest and a disservice to severely suffering patients. It would inhibit meaningful research aimed at finding an optimal therapy (one that works beyond placebo) and be a waste of resources.
The aim of this systematic review and network meta-analysis was to identify the optimal dose and modality of exercise for treating major depressive disorder, compared with psychotherapy, antidepressants, and control conditions.
The screening, data extraction, coding, and risk of bias assessment were performed independently and in duplicate. Bayesian arm based, multilevel network meta-analyses were performed for the primary analyses. Quality of the evidence for each arm was graded using the confidence in network meta-analysis (CINeMA) online tool. All randomised trials with exercise arms for participants meeting clinical cut-offs for major depression were included.
A total of 218 unique studies with a total of 495 arms and 14 170 participants were included. Compared with active controls (eg, usual care, placebo tablet), moderate reductions in depression were found for
- walking or jogging,
- strength training,
- mixed aerobic exercises,
- and tai chi or qigong.
The effects of exercise were proportional to the intensity prescribed. Strength training and yoga appeared to be the most acceptable modalities. Results appeared robust to publication bias, but only one study met the Cochrane criteria for low risk of bias. As a result, confidence in accordance with CINeMA was low for walking or jogging and very low for other treatments.
The authors concluded that exercise is an effective treatment for depression, with walking or jogging, yoga, and strength training more effective than other exercises, particularly when intense. Yoga and strength training were well tolerated compared with other treatments. Exercise appeared equally effective for people with and without comorbidities and with different baseline levels of depression. To mitigate expectancy effects, future studies could aim to blind participants and staff. These forms of exercise could be considered alongside psychotherapy and antidepressants as core treatments for depression.
As far as I can see, there are two main problems with these findings:
- Because too many of the studies are less than rigorous, the results are not quite as certain as the conclusions would seem to imply.
- Patients suffering from a major depressive disorder are often unable (too fatigued, demotivated, etc.) to do and/or keep up vigorous excerise over any length of time.
What I find furthermore puzzling is that, on the one hand, the results show that – as one might expect – the effects are proportional to the intensity of the excercise but, on the other hand tai chi and qugong which are both distinctly low-intensity turn out to be effective.
Nonetheless, this excellent paper is undoubtedly good news and offers hope for patients who are in desperate need of effective, safe and economical treatments.
This pilot study is “delving into the potential benefits of Reiki therapy as a complementary intervention for the treatment and management of stress and anxiety”.
A total of 31 volunteers self-reporting stress, anxiety, or psychological disorders were enrolled. Health-related quality of life (HRQoL) was assessed using the 36-Item Short Form Health Survey (SF-36) Questionnaire for anxiety and depression. Pre- and post-treatment HRQoL scores were meticulously compared, and the significance of the disparities in these scores was meticulously computed.
Analysis was restricted to volunteers who completed the 3-day Reiki sessions. Statistically significant enhancements were discerned across all outcome measures, encompassing positive affect, negative affect, pain, drowsiness, tiredness, nausea, appetite, shortness of breath, anxiety, depression, and overall well-being (P<0.0001).
The authors concluded that the constancy and extensive scope of these improvements suggest that Reiki therapy may not only address specific symptoms but also contribute significantly to a predominant escalation of mental and physical health.
This study is almost comical.
Amongst all the many forms of so-called alternative medicine (SCAM), Reiki is perhaps the most ridiculous scam. It is a form of paranormal or ‘energy healing’ popularised by Japanese Mikao Usui (1865–1926). Rei means universal spirit (sometimes thought of as a supreme being) and ki is the assumed universal life energy. It is based on the assumptions of Traditional Chinese Medicine and the existence of ‘chi’, the life-force that is assumed to determine our health.
Reiki practitioners believe that, with their hands-on healing method, they can transfer ‘healing energy’ to a patient which, in turn, stimulates the self-healing properties of the body. They assume that the therapeutic effects of this technique are obtained from a ‘universal life energy’ that provides strength, harmony, and balance to the body and mind. There is no scientific basis for such notions, and reiki is therefore not plausible.
Reiki is used for a number of conditions, including the relief of stress, tension and pain. There have been several clinical trials testing its effectiveness. Those that are rigorous fail to show that the treatment is effective – and those that are dripping with bias, like the one discussed here, tend to produce false-positive results.
The present study has many flaws that are too obvious to even mention. While reading it, I asked myself the following questions:
- How could a respectable university ever allow this pseudo-research to go ahead?
- How could a respectable ethics committee ever permit it?
- How could a respectable journal ever publish it?
The answers must be that, quite evidently, they are not respectable.
Mercury is a highly toxic chemical that threatens the health of humans and the environment. When it is released into the environment, it enters the food chain where it accumulates, particularly in fish. Exposure to high levels of mercury can cause harm to the brain, lungs, kidneys and the immune system. For these reasons, dental amalgam fillings which contain mercury have long been criticized. This is particularly true in the realm of so-called alternative medicine (SCAM) where, as discussed repeatedly, amalgam has long been a subject of both concern and misinformation, e.g.:
- Is removal of dental amalgam a good idea?
- Dental Amalgam
- Three Trends In “Alternative Dentistry” Part 3: Amalgam Removal and Avoidance
- Three Trends In “Alternative Dentistry” Part 1: The Concept of Projections—Of Meridians and Temporo-Mandibular Joint Dysfunction (TMJD)
- Holistic dentistry?
In the EU, dental amalgam might soon be merely of historical interest.
It has been announced that the EU Parliament and Council reached a provisional political agreement on the Commission’s proposal to address the remaining uses of mercury in products in the EU in line with commitments set out in the EU’s Zero Pollution Ambition.
In spite of viable mercury-free alternatives, around 40 tonnes of mercury are still used in the EU annually for dental amalgam as current rules only forbid the use of dental amalgam for treating teeth in children under 15 years old as well as pregnant and breastfeeding women.
Negotiators agreed to phase out the use of dental amalgam in the EU by 1 January 2025 except if deemed strictly necessary by the dental practitioner based on the duly justified specific medical needs of the patient.
EU countries that have not yet adjusted their reimbursement system to cover alternatives, may postpone the phase-out up until 30 June 2026, to avoid negative repercussions for low-income individuals that would otherwise be socio-economically disproportionally affected by the phase-out.
The export of dental amalgam will also be prohibited from 1 January 2025, whereas the manufacturing and import into the EU will be banned from 1 July 2026.
After the agreement, rapporteur Marlene Mortler (EPP, Germany) said: “After an intensive week of negotiations, we were able to reach an agreement today to ban dental amalgam containing mercury. This is an important step towards a mercury-free future. I am very pleased with the result – because we have ensured that such dental amalgam may only be used in medically necessary cases. Some Member States have been granted an exemption in order to mitigate the socio-economic consequences of the amalgam phase-out. After all, the ban on dental amalgam must not mean that low-income EU citizens can no longer afford adequate dental treatment in these countries. Another key point of this agreement is the decision that lamps containing mercury may only be exported to countries outside the EU until 30 June 2026. This will ensure that products that are already banned in the EU are not sold to third countries and have environmentally harmful consequences there.”
The deal still has to be adopted by the EU Parliament and Council, after which the new law will be published in the EU Official Journal and enter into force 20 days later.
This study tested whether trigger point acupuncture (TrPA) is beneficial for office workers who have reduced job performance (presenteeism) due to chronic neck and shoulder pain (katakori).
A 4-week single-center randomized clinical trial was conducted on 20 eligible female office workers with chronic neck and shoulder pain of at least 3-month duration. The control group implemented only workplace-recommended presenteeism measures, whereas the intervention group received TrPA up to 4 times per month in addition to the presenteeism measures recommended by each workplace. The major outcome measure was the relative presenteeism score on the World Health Organization Health and Work Performance (WHO-HPQ). The secondary outcome measures were pain intensity (numerical rating scale), absolute presenteeism (WHO-HPQ), anxiety and depression (Hospital Anxiety and Depression Scale; HADS), catastrophic thoughts related to pain (Pain Catastrophizing Scale; PCS), and sleep (Athens Insomnia Scale; AIS).
All 9 cases in the intervention group and 11 cases in the control group were analyzed. TrPA up to 4 times per month reduced the intensity of neck and shoulder pain by 20% (P < .01, d = 1.65) and improved labor productivity (relative presenteeism value) by 0.25 (P < .01, d = 1.33) compared with the control group over 1 month. No significant differences were observed between the 2 groups in terms of absolute presenteeism score, HADS, PCS, or AIS.
The authors concluded that these results suggest that regular intervention with TrPA may be effective in the relative presenteeism score before and after the intervention and the degree of neck and shoulder pain over 28 days compared with the control group.
Sure, TrPA may be effective.
But is it?
I thought the trial was aimed at answering that question!
But it didn’t!
Why not?
Because, as we have discussed ad nauseam on this blog, the A+B versus B study design cannot answer it. On the contrary, it will always generate a positive result without determining whether the treatment or a nonspecific (placebo) effect caused the outcome (which, of course, is the reason why this study design is so popular in SCAM research).
In view of this, I suggest to re-formulate the conclusions as follows:
The study suggests that the researchers were ill-informed when designing it. Therefore, the findings show nothing of value.
Yestderday, it was announced that King Charles has cancer. He had been in hospital for surgery for his enlarged prostate. Initially, the news was positive, as it was confirmed not to be prostate cancer. However, during the investigations, a cancer was discovered that apparently is unrelated to the prostate. Since the announcement, many journalists and other people have written to me asking what I think about it and what treatment Charles is likely to receive. I therefore decided to write a short post about the matter.
As a physician and human being I am very sorry whenever I hear that anyone has fallen ill, particularly if the condition is serious and potentially life-threatening. That this includes Charles goes without saying. Equally it is self-evident that I wish that all goes well for him, that the treatment he reportedly has already started is not too arduous, that he keeps in good spirit, that he has empathetic support from all his family and recovers quickly and fully.
Charles will, I am sure, have the best treatment anyone could wish for. Will he use so-called alternative medicine (SCAM), for example, the Gerson therapy, one of the SCAMs he once promoted as a cure of cancer? Of course not! He will receive the most effective, evidence-based care that is currently available. Will he thus not try any SCAM at all? I am confident that he will use SCAM wisely, namely not as a cure but as a supportive measure. In my book on this very subject, I go through all the relevant evidence and conclude that, while SCAM is most certainly not a cancer cure, it can have a place in supportive cancer care. Depending on the symptoms that develop during and after the conventional treatments, certain SCAMs can, according to fairly sound evidence, be helpful in improving wellness and quality of life.
Going through a battle against cancer is often a most humbling experience. Therefore, I am hopeful that, as he recovers from his ordeal, Charles will see that modern medicine – he once described it as being out of balance like the leaning tower of Pisa – is not just effective, empathetic and caring but also not nearly as unbalanced and unholistic as he often proclaimed it to be. In that sense, the experience might reform our king, and – who knows? – he might, after all, turn out to be not the self-proclaimed enemy but a true friend of the Enlightenment.
The Buteyko techniques (known in Russia as ‘Voluntary Elimination of Deep Breathing’) are treatments to control respiration developed by the Russian Konstantin Buteyko (1923–2003). Inspired by the methods of respiratory control in yoga, the original Buteyko technique was specifically aimed at easing the symptoms of respiratory conditions, particularly asthma. Konstantin Buteyko postulated that there is a connection between hyperventilation and asthma and that it should be possible to reduce asthma symptoms by deliberate breath control.
The Eucapnic Buteyko method is an adaptation of Buteyko’s original technique which was first introduced in Australia and is now used worldwide. It includes the same focus on ventilation control, but the approach has been re-designed with the aim of achieving better patient-compliance. Both treatments and further variations depend crucially on the cooperation of the patient who has to attend long sessions of learning the technique and must follow the somewhat tedious programme rigorously.
A Cochrane review of Buteyko and similar breathing techniques concluded that “there is no credible evidence regarding the effectiveness of breathing exercises for the clinical symptoms of dysfunctional breathing/hyperventilation syndrome. It is currently unknown whether these interventions offer any added value in this patient group or whether specific types of breathing exercise demonstrate superiority over others.”
Now, a new study adds to this knowledge. This randomized clinical trial included two groups (n = 30 each) of patients with asthma. They received either:
- Buteyko breathing technique (BBT) together with usual therapy (UT)
- or UT alone over a period of 3 months.
The primary outcome comprised the voluntary control pause (CP) after 3 months, secondary outcomes an additional breathhold parameter, forced expiratory volume in 1 s (FEV1), capnovolumetry, exhaled nitric oxide (FeNO), Asthma Control Questionnaire (ACQ) and Nijmegen Questionnaire (NQ), and the use of medication (β2-agonists; inhaled corticosteroids, ICS).
CP showed significant time-by-group interaction [F(1,58.09) = 28.70, p < 0.001] as well as main effects for study group [F(1,58.27) = 5.91, p = 0.018] and time [F(1,58.36) = 17.67, p < 0.001]. ACQ and NQ scores were significantly (p < 0.05 each) improved with BBT. This was associated with reductions in the use of β2-agonists and ICS (p < 0.05 each) by about 20% each. None of these effects occurred in the UT group. While FEV1 and the slopes of the capnovolumetric expiratory phases 2 and 3 did not significantly change, the capnovolumetric threshold volume at tidal breathing increased (p < 0.05) with BBT by about 10 mL or 10%, compared to baseline, suggesting a larger volume of the central airways. No significant changes were seen for FeNO.
The authors concluded that BBT was clinically effective, as indicated by the fact that the improvement in symptom scores and the small increase in bronchial volume occurred despite the significant reduction of respiratory pharmacotherapy. As the self-controlled Buteyko breathing therapy was well-accepted by the participants, it could be considered as supporting tool in asthma therapy being worth of wider attention in clinical practice.
I disagree with this conclusion and think it ought to be changed to:
BBT or a placebo effect was clinically effective.
The reason is that, as many readers have heard me say before, the infamous A+B versus B design does not control for placebo effects and thus is guaranteed to produce a positive result.
The research was conducted by an international team evidently led by the relatively new ARCIM Institute which claims on its website:
The acronym ARCIM stands for Academic Research in Complementary and Integrative Medicine.
The bridging between different treatment and research approaches, disciplines and ways of thinking achieved by the research work of the ARCIM Institute can be symbolized by our logo’s bridge arch. ARCIM integrates this bridge-building metaphor within its name since the Latin term “arcus” means “arch” or “bridge.”
