rheumatoid arthritis
The aim of this article was to review the use of homeopathy in rheumatic diseases (RDs). PubMed and Embase databases were examined for literature on homeopathy and RDs between 1966 and April 2023. 15 articles were included.
The diseases treated were
- osteoarthritis (n=3),
- rheumatoid arthritis (n=3),
- ankylosing spondylitis (n=1),
- hyperuricemia (n=1),
- tendinopathy (n=1).
The age of the patients varied from 31 to 87 years, and male gender ranged from 56.7% to 100%. The homeopathic treatments varied from a fixed medicine to an individualized homeopathy.
Most studies (9/15) demonstrated improvements after homeopathy. Side effects were not seen or minimal and were comparable to those of the placebo groups.
The authors concluded that this review shows homeopathy is a promising and safe therapy for RD treatment. However, the data needs to be reproduced in future more extensive studies, including other rheumatic conditions.
This paper amounts to an insult of its readership!
Not only is it badly written but also [and more importantly] it is missing almost everything that makes a systematic review. Despite this the authors claim that it “adhered to PRISMA standards”. This is certainly not true.
Amongst the missing items, the most important ones are probably the evaluation of the methodological quality of the inclued primary studies as well as a critical assessment of the evidence. The authors concede that their paper has limitations: “the number of participants was low. Second, a few RDs were evaluated: osteoarthritis, rheumatoid arthritis, fibromyalgia, hyperuricemia, ankylosing spondylitis, and
tendinopathy.”
When reading this, I asked myself: are they clueless or dishonest?
In my view, the authors (from Brasil and Israel) and peer-reviewers of this paper should be ashamed of such shoddy work and the editors of the journal publishing this nonsense should withdraw the paper asap.
Previous randomized controlled trials (RCTs) suggested that gut microbiota-based therapies may be effective in treating autoimmune diseases, but a systematic summary is lacking. This systematic review was aimed at filling the gap.
The literature searches identified total of 80 RCTs. They related to 14 types of autoimmune disease:
- celiac sprue,
- SLE,
- lupus nephritis (LN),
- RA,
- juvenile idiopathic arthritis (JIA),
- spondyloarthritis,
- psoriasis,
- fibromyalgia syndrome,
- MS,
- systemic sclerosis,
- type 1 diabetes mellitus (T1DM),
- oral lichen planus (OLP),
- Crohn’s disease,
- ulcerative colitis.
The results showed that gut microbiota-based therapies may improve the symptoms and/or inflammatory factor of:
- celiac sprue,
- SLE,
- LN,
- JIA,
- psoriasis,
- PSS,
- MS,
- systemic sclerosis,
- Crohn’s disease,
- ulcerative colitis.
However, gut microbiota-based therapies may not improve the symptoms and/or inflammatory factor of spondyloarthritis and RA. Gut microbiota-based therapies may relieve the pain of fibromyalgia syndrome, but the effect on fibromyalgia impact questionnaire score is not significant. Gut microbiota-based therapies may improve HbA1c in T1DM, but its effect on total insulin requirement does not seem to be significant. Probiotics did not seem to increase the incidence of adverse events.
The authors concluded that gut microbiota-based therapies may improve several autoimmune diseases (celiac sprue, SLE and LN, JIA, psoriasis, fibromyalgia syndrome, PSS, MS, T1DM, Crohn’s disease, and ulcerative colitis).
This sounds promissing, perhaps even a bit too good to be true?
To answer this question, It seems important to look at the quality of the primary studies:
- Twenty-nine RCTs failed to describe the random sequence generation methods.
- Seventeen RCTs were not blinded and their results contained subjective indicators.
- Seven RCTs were rated as high risk of bias.
And what about other caveats?
- The effect sizes vary but are often small.
- There is much heterogeneity.
- For some of the conditions there are only very few trials
- There is no uniform, plausible mode of action.
In summary, while these findings are no doubt interesting, I recommend taking them with a pinch of salt.
According to its authors, this study‘s objective was to demonstrate that acupuncture is beneficial for decreasing the risk of ischaemic stroke in patients with rheumatoid arthritis (RA).
The investigation was designed as a propensity score-matched cohort nationwide population-based study. Patients with RA diagnosed between 1 January 1997 and 31 December 2010, through the National Health Insurance Research Database in Taiwan. Patients who were administered acupuncture therapy from the initial date of RA diagnosis to 31 December 2010 were included in the acupuncture cohort. Patients who did not receive acupuncture treatment during the same time interval constituted the no-acupuncture cohort. A Cox regression model was used to adjust for age, sex, comorbidities, and types of drugs used. The researchers compared the subhazard ratios (SHRs) of ischaemic stroke between these two cohorts through competing-risks regression models.
After 1:1 propensity score matching, a total of 23 226 patients with newly diagnosed RA were equally subgrouped into acupuncture cohort or no-acupuncture cohort according to their use of acupuncture. The basic characteristics of these patients were similar. A lower cumulative incidence of ischaemic stroke was found in the acupuncture cohort (log-rank test, p<0.001; immortal time (period from initial diagnosis of RA to index date) 1065 days; mean number of acupuncture visits 9.83. In the end, 341 patients in the acupuncture cohort (5.95 per 1000 person-years) and 605 patients in the no-acupuncture cohort (12.4 per 1000 person-years) experienced ischaemic stroke (adjusted SHR 0.57, 95% CI 0.50 to 0.65). The advantage of lowering ischaemic stroke incidence through acupuncture therapy in RA patients was independent of sex, age, types of drugs used, and comorbidities.
The authors concluded that this study showed the beneficial effect of acupuncture in reducing the incidence of ischaemic stroke in patients with RA.
It seems obvious that the editors of ‘BMJ Open’, the peer reviewers of the study and the authors are unaware of the fact that the objective of such an investigeation is not to to demonstrate that acupuncture is beneficial but to test whether acupuncture is beneficial. Starting a study with the intention to to show that my pet therapy works is akin to saying: “I am intending to mislead you about the value of my intervention”.
One needs therefore not be surprised that the authors of the present study draw very definitive conclusions, such as “acupuncture therapy is beneficial for ischaemic stroke prevention”. But every 1st year medical or science student should know that correlation is not the same as causation. What the study does, in fact, show is an association between acupuncture and stroke. This association might be due to dozens of factors that the ‘propensity score matching’ could not control. To conclude that the results prove a cause effect relationship is naive bordering on scientific misconduct. I find it most disappointing that such a paper can pass all the hurdles to get published in what pretends to be a respectable journal.
Personally, I intend to use this study as a good example for drawing the wrong conclusions on seemingly rigorous research.
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. The characteristics of older adults with debilitating musculoskeletal pain who report SCAM use is also examined. For this purpose, the cross-sectional European Social Survey Round 7 from 21 countries was employed. It examined participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12 months.
Of the 4950 older adult participants, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year.
The most commonly used SCAMs were:
- manual body-based therapies (MBBTs) including massage therapy (17.9%),
- osteopathy (7.0%),
- homeopathy (6.5%)
- herbal treatments (5.3%).
SCAM use was positively associated with:
- younger age,
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe,
- multiple health problems.
(Many years ago, I have summarized the most consistent determinants of SCAM use with the acronym ‘FAME‘ [female, affluent, middle-aged, educated])
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous 12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
I often mutter about the plethora of SCAM surveys that report nothing meaningful. This one is better than most. Yet, much of what it shows has been demonstrated before.
I think what this survey confirms foremost is the fact that the popularity of a particular SCAM and the evidence that it is effective are two factors that are largely unrelated. In my view, this means that more, much more, needs to be done to inform the public responsibly. This would entail making it much clearer:
- which forms of SCAM are effective for which condition or symptom,
- which are not effective,
- which are dangerous,
- and which treatment (SCAM or conventional) has the best risk/benefit balance.
Such information could help prevent unnecessary suffering (the use of ineffective SCAMs must inevitably lead to fewer symptoms being optimally treated) as well as reduce the evidently huge waste of money spent on useless SCAMs.
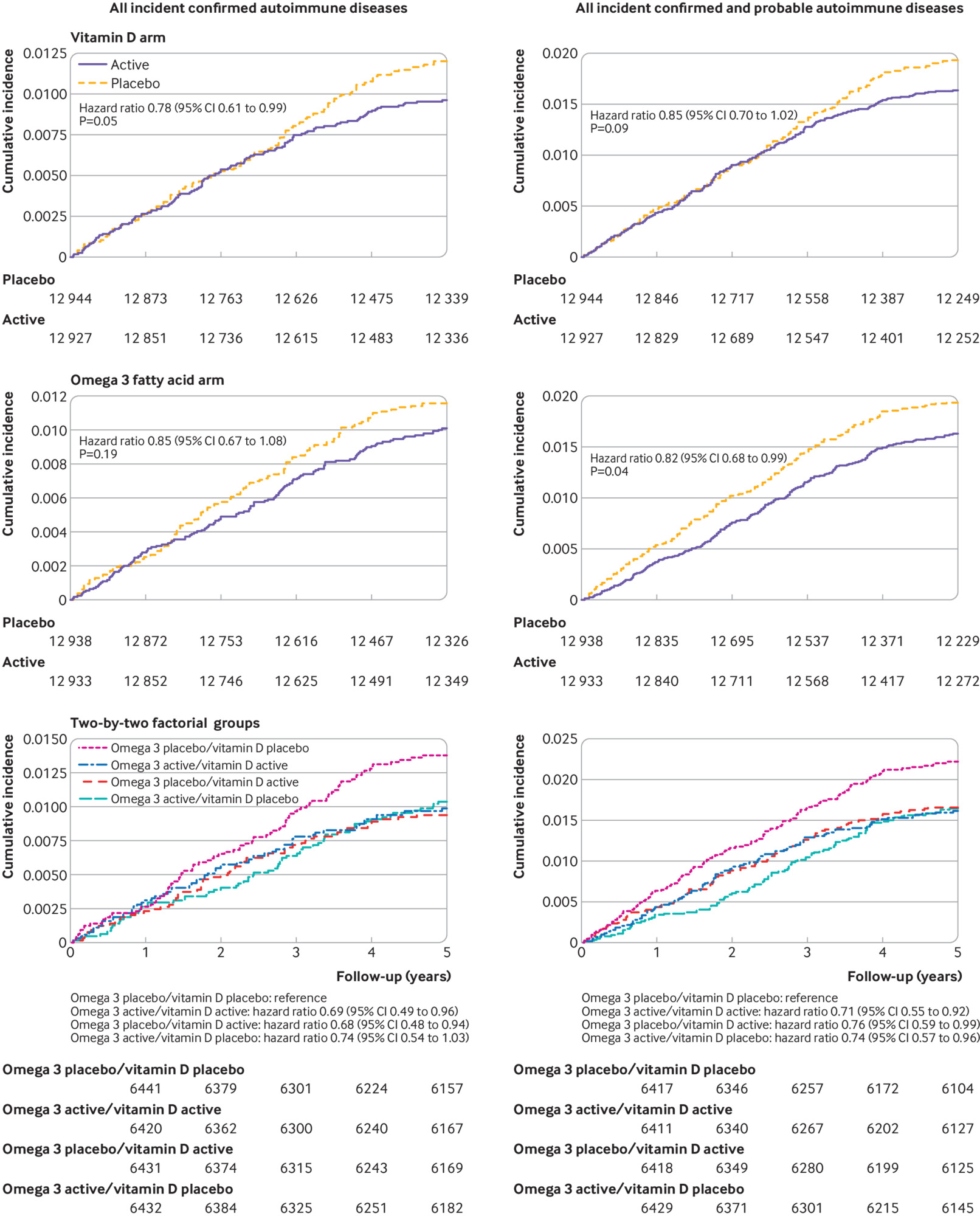
This study investigated whether vitamin D and marine-derived long-chain omega 3 fatty acids reduce autoimmune disease risk. A nationwide, randomized, double-blind, placebo-controlled trial with a two-by-two factorial design was conducted in the US. In total, 25 871 participants (12 786 men ≥50 years and 13 085 women ≥55 years at enrollment) took part.
Participants were given
- vitamin D (2000 IU/day),
- matched placebo,
- omega 3 fatty acids (1000 mg/day),
- matched placebo.
Participants self-reported all incident autoimmune diseases from baseline to a median of 5.3 years of follow-up; these diseases were confirmed by extensive medical record review. Cox proportional hazard models were used to test the effects of vitamin D and omega 3 fatty acids on autoimmune disease incidence. The primary endpoint was all incident autoimmune diseases confirmed by medical record review: rheumatoid arthritis, polymyalgia rheumatica, autoimmune thyroid disease, psoriasis, and all others.
Participants were followed for a median of 5.3 years. 18 046 self-identified as non-Hispanic white, 5106 as black, and 2152 as other racial and ethnic groups. The mean age was 67.1 years. For the vitamin D arm, 123 participants in the treatment group and 155 in the placebo group had a confirmed autoimmune disease (hazard ratio 0.78, 95% confidence interval 0.61 to 0.99, P=0.05). In the omega 3 fatty acids arm, 130 participants in the treatment group and 148 in the placebo group had a confirmed autoimmune disease (0.85, 0.67 to 1.08, P=0.19). Compared with the reference arm (vitamin D placebo and omega 3 fatty acid placebo; 88 with confirmed autoimmune disease), 63 participants who received vitamin D and omega 3 fatty acids (0.69, 0.49 to 0.96), 60 who received only vitamin D (0.68, 0.48 to 0.94), and 67 who received only omega 3 fatty acids (0.74, 0.54 to 1.03) had confirmed autoimmune disease.
The authors concluded that vitamin D supplementation for five years, with or without omega 3 fatty acids, reduced autoimmune disease by 22%, while omega 3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant). Both treatment arms showed larger effects than the reference arm (vitamin D placebo and omega 3 fatty acid placebo).
This is the best trial of dietary supplements that I have seen for a very long time. Yet, the authors caution: Because participants were older adults, the results might not generalize to autoimmune diseases that primarily have their onset in younger people. However, the pathogenesis of many of the specific autoimmune diseases observed (eg, rheumatoid arthritis and psoriasis) is similar in younger adults. The trial tested only one dose and formulation of each supplement. The relatively low number of participants with a confirmed diagnosis of most individual diseases, and the challenge of confirming diagnosis of autoimmune thyroid disease based on medical records, limited statistical power to detect an effect on individual disease outcomes and subgroups of a priori interest. Given the latency of autoimmune disease onset, longer follow-up could be informative, and participants are being followed in an open label extension study.
As regular readers know, I am not easily impressed – but today I am.
Bee venom acupuncture is a form of acupuncture in which bee venom is applied to the tips of acupuncture needles, stingers are extracted from bees, or bees are held with an instrument exposing the stinger, and applied to acupoints on the skin.
Bee venom consisting of multiple anti-inflammatory compounds such as melittin, adolapin, apamin. Other substances such as phospholipase A2 can be anti-inflammatory in low concentrations and pro-inflammatory in others. However, bee venom also contains proinflammatory substances, melittin, mast cell degranulation peptide 401, and histamine.
Bee venom acupuncture has been used to treat a number of conditions such as lumbar disc disease, osteoarthritis of the knee, rheumatoid arthritis, adhesive capsulitis, lateral epicondylitis, peripheral neuropathies, stroke and Parkinson’s Disease. The quality of these studies tends to be so poor that any verdict on the effectiveness of bee venom acupuncture would be premature.
A new clinical trial of bee-venom acupuncture for rheumatoid arthritis (RA) might change this situation. A total of 120 cases of RA patients were randomized into bee-sting acupuncture group (treatment) and western medicine group (control). The patients of the control group were treated by oral administration of Methotrexate (10 mg, once a week) and Celecoxlb (0.2 g, once a day). Those of the treatment group received 5 to 15 bee stings of Ashi-points or acupoints according to different conditions and corporeity, and with the bee-sting retained for about 5 min every time, once every other day. The treatment lasted for 8 weeks. The therapeutic effect was assessed by examining:
- symptoms and signs of the affected joints as morning stiffness duration,
- swollen/tender joint counts (indexes),
- handgrip strength,
- 15 m-walking time,
- visual analogue scale (VAS),
- Disease Activity Score including a 28-joint count (DAS 28),
- rheumatoid factor (RF),
- erythrocyte sedimentation rate (ESR),
- C-reactive protein (CRP),
- anti-cyclic citrullinated peptide antibody (ACCPA).
For assessing the safety of bee-venom acupuncture, the patients’ responses of fever, enlargement of lymph nodes, regional red and swollen, itching, blood and urine tests for routine were examined.
Findings of DAS 28 responses displayed that of the two 60 cases in the control and bee-venom acupuncture groups, 15 and 18 experienced marked improvement, 33 and 32 were effective, 12 and 10 ineffective, with the effective rates being 80% and 83. 33%, respectively. No significant difference was found between the two groups in the effective rate (P>0.05). After the treatment, both groups have witnessed a marked decrease in the levels of morning stiffness duration, arthralgia index, swollen joint count index, joint tenderness index, 15 m walking time, VAS, RF, ESR, CRP and ACCPA, and an obvious increase of handgrip strength relevant to their own levels of pre-treatment in each group (P<0.05). There were no significant differences between the two groups in the abovementioned indexes (P>0.05). The routine blood test, routine urine test, routine stool test, electrocardiogram result, the function of liver and kidney and other security index were within the normal range, without any significant adverse effects found after bee-stinging treatment.
The authors (from the Department of Acupuncture and Moxibustion, Bao’an Hospital of Traditional Chinese Medicine, Shenzhen, China) concluded that bee-venom acupuncture therapy for RA patients is safe and effective, worthy of popularization and application in clinical practice.
Where to start? There is so much – perhaps I just comment on the conclusion:
- Safety cannot be assessed on the basis of such a small sample. Bee venom can cause anaphylaxis, and several deaths have been reported in patients who successfully received the therapy prior to the adverse event. Because there is no adverse-effect monitoring system, the incidence of adverse events is unknown. Stating that it is safe, is therefore a big mistake.
- The trial was a non-superiority study. As such, it needs a much larger sample to be able to make claims about effectiveness.
- From the above two points, it follows that popularization and application in clinical practice would be a stupid exercise.
So, what is left over from this seemingly rigorous RCT?
NOTHING!
(except perhaps a re-affirmation of my often-voiced fear that we must take TCM-studies from China with more than just one pinch of salt)
We have repeatedly discussed the fact that alternative medicine (AM) is by no means free of risks. I find it helpful to divide them into two broad categories:
- direct risks of the intervention (such as stroke due to neck manipulation, or cardiac tamponade caused by acupuncture, or liver damage due to a herbal remedy) and
- indirect risks usually due to the advice given by AM practitioners.
The latter category is often more important than the former. It includes delay of effective treatment due to treatment with an ineffective or less effective form of AM. It is clear that this will cause patients to suffer unnecessarily.
Several investigations have recently highlighted this important problem, including this study from Singapore which assessed the predictors of AM-use in patients with early inflammatory arthritis (EIA), and its impact on delay to initiation of disease-modifying anti-rheumatic drugs (DMARD). Data were collected prospectively from EIA patients aged ≥ 21 years. Current or prior AM-use was ascertained by face-to-face interviews. Predictors of AM-use and its effect on time to DMARD initiation were determined by multivariate logistic regression and Cox proportional hazards, respectively.
One hundred and eighty patients were included: 83.9% had rheumatoid arthritis, 57% were seropositive. Median (IQR). Chinese race, being non-English speaking, smoking and high DAS28 were independent predictors of AM-use. AM-users initiated DMARD later (median [IQR] 21.5 [13.1-30.4] vs. 15.6 [9.4-22.7] weeks in non-users, P = 0.005). AM-use and higher DAS28 were associated with a longer delay to DMARD initiation. Race, education level, being non-English speaking, smoking and sero-positivity were not associated.
The authors concluded that healthcare professionals should be aware of the unique challenges in treating patients with EIA in Asia. Healthcare beliefs regarding AM may need to be addressed to reduce treatment delay.
These findings are not dissimilar to results previously discussed, for instance:
- AM-use delays cancer diagnosis.
- The advice of non-medically qualified practitioners may delay cancer therapy.
- Chiropractic care may delay referral to effective treatment.
- Consultations with homeopaths can delay effective therapy.
The only solution to the problem I can think of would be to educate AM practitioners and the public such that they are aware of the issue and do everything possible to prevent such problems. But this is, of course, easier said than done, and it seems more than just optimistic to hope that such endeavours might be successful. The public is currently bombarded with misleading information and outright lies about AM (many of my previous post have addressed this problem). And practitioners would have to operate against their own financial interest to prevent these problems from occurring.
This means that treatment delays caused by AM-use and advice from AM practitioners are inevitable…
unless you have a better idea.
If so, please let me know.
As I have said on several occasions before: I am constantly on the lookout for new rigorous science that supports the claims of alternative medicine. Thus I was delighted to find a recent and potentially important article with some positive evidence.
Fish oil has been studied extensively in terms of its effects on health. We know that it has powerful anti-inflammatory properties and might thus benefit a wide range of conditions. However, the effects of FO in rheumatoid arthritis (RA) have not been examined in the context of contemporary treatment of early RA.
A new study has tried to fill this gap by examining the effects of high versus low dose FO in early RA employing a ‘treat-to-target’ protocol of combination disease-modifying anti-rheumatic drugs (DMARDs).
Patients with RA <12 months’ duration and who were DMARD-naïve were enrolled and randomised 2:1 to FO at a high dose or low dose (for masking). These groups, designated FO and control, were given 5.5 or 0.4 g/day, respectively, of the omega-3 fats, eicosapentaenoic acid + docosahexaenoic acid. All patients received methotrexate (MTX), sulphasalazine and hydroxychloroquine, and DMARD doses were adjusted according to an algorithm taking disease activity and toxicity into account. DAS28-erythrocyte sedimentation rate, modified Health Assessment Questionnaire (mHAQ) and remission were assessed three monthly. The primary outcome measure was failure of triple DMARD therapy.
In the FO group, failure of triple DMARD therapy was lower (HR=0.28 (95% CI 0.12 to 0.63; p=0.002) unadjusted and 0.24 (95% CI 0.10 to 0.54; p=0.0006) following adjustment for smoking history, shared epitope and baseline anti–cyclic citrullinated peptide. The rate of first American College of Rheumatology (ACR) remission was significantly greater in the FO compared with the control group (HRs=2.17 (95% CI 1.07 to 4.42; p=0.03) unadjusted and 2.09 (95% CI 1.02 to 4.30; p=0.04) adjusted). There were no differences between groups in MTX dose, DAS28 or mHAQ scores, or adverse events.
The authors concluded that FO was associated with benefits additional to those achieved by combination ‘treat-to-target’ DMARDs with similar MTX use. These included reduced triple DMARD failure and a higher rate of ACR remission.
So here we have a dietary supplement that actually might generate more good than harm! There is a mountain of data of good research on the subject. We understand the mechanism of action and we have encouraging clinical evidence. Some people might still say that we do not need to take supplements in order to benefit from the health effects of FO, consuming fatty fish regularly might have the same effects. This is true, of course, but the amount of fish that one would need to eat every day would probably be too large for most people’s taste.
The drawback (from the perspective of alternative medicine) in all this is, of course, that some experts might deny that FO has much to do with alternative medicine. Again: what do we call alternative medicine that works? We call it MEDICINE! And perhaps FO is an excellent example of exactly that.
For this blog, I am constantly on the lookout for ‘positive news’ about alternative medicine. Admittedly, I rarely find any.
All the more delighted I was when I found this new study aimed to analyse the association between dietary long-chain n-3 polyunsaturated fatty acids (PUFAs) and incidence of rheumatoid arthritis (RA) in middle-aged and older women.
Data on diet were collected in 1987 and 1997 via a self-administered food-frequency questionnaire (FFQ). The risk of RA associated with dietary long-chain n-3 PUFAs and fish intake was estimated using Cox proportional hazard regression models, adjusted for age, cigarette smoking, alcohol intake, use of aspirin and energy intake.
The results show that, among 32 232 women born 1914–1948, 205 RA cases were identified during a mean follow-up of 7.5 years. An intake of dietary long-chain n-3 PUFAs (FFQ1997) of more than 0.21 g/day (lowest quintile) was associated with a 35% decreased risk of developing RA compared with a lower intake. Long-term intake consistently higher than 0.21 g/day (according to both FFQ1987 and FFQ1997) was associated with a 52% decreased risk. Consistent long-term consumption (FFQ1987 and FFQ1997) of fish ≥1 serving per week compared with<1 was associated with a 29% decrease in risk.
The authors concluded that this prospective study of women supports the hypothesis that dietary intake of long-chain n-3 PUFAs may play a role in aetiology of RA.
These are interesting findings which originate from a good investigation and which are interpreted with the necessary caution. As all epidemiological data, this study is open to a number of confounding factors, and it is therefore impossible to make firm causal inferences. The results thus do not led themselves to clinical recommendation, but they are an indication that more definitive research is warranted, all the more so since we have plausible mechanisms to explain the observed findings.
A most encouraging development for alternative medicine, one could conclude. But is this really true? Most experts would be surprised, I think, to find that PUFA-consumption should fall under the umbrella of alternative medicine. Remember: What do we call alternative medicine that works? It is called MEDICINE!
One alternative therapy that I have so far almost entirely neglected is Ayurveda. It is said to be one of the fastest growing system within this sector. Ayurvedic healing includes herbs, nutrition, panchakarma cleansing, acupressure massage, Yoga, Sanskrit, and Jyotish (Vedic astrology). The website of the ‘Choppra Center’ explains: Recognizing that human beings are part of nature, Ayurveda describes three fundamental energies that govern our inner and outer environments: movement, transformation, and structure. Known in Sanskrit as Vata (Wind), Pitta (Fire), and Kapha (Earth), these primary forces are responsible for the characteristics of our mind and body. Each of us has a unique proportion of these three forces that shapes our nature. If Vata is dominant in our system, we tend to be thin, light, enthusiastic, energetic, and changeable. If Pitta predominates in our nature, we tend to be intense, intelligent, and goal-oriented and we have a strong appetite for life. When Kapha prevails, we tend to be easy-going, methodical, and nurturing. Although each of us has all three forces, most people have one or two elements that predominate.
However, the evidence for its effectiveness is not overwhelming. In 2007, we published a systematic review of Ayurvedic treatments for rheumatoid arthritis (RA). Seven studies met our inclusion criteria. Trials tested either Ayurvedic medicine against placebo or other Ayurvedic medicines. Of 3 placebo-controlled RCTs, one high-quality trial did not show benefit of the active treatment against placebo, while another incompletely reported study indicated beneficial effects of an Ayurvedic medicine. A further incompletely reported study showed no significant difference. The remaining 4 trials were difficult to interpret because they tested an Ayurvedic medicine against other Ayurvedic medicines whose effects were not proven. We concluded that there is a paucity of RCTs of Ayurvedic medicines for RA. The existing RCTs fail to show convincingly that such treatments are effective therapeutic options for RA.
Because of this paucity of reliable evidence, any new assessments are welcome.
The aim of this article was to review and meta-analyze the effectiveness and safety of different Ayurvedic interventions in patients with osteoarthritis (OA). 138 electronic databases were searched through August 2013. Randomized controlled trials, randomized crossover studies, cluster-randomized trials, and non-randomized controlled clinical trials were eligible. Adults with pre-diagnosed OA were included as participants.
Interventions were included as Ayurvedic, if they were explicitly labeled as such. The main outcome measures were pain, physical function, and global improvement. Risk of bias was assessed using the Cochrane risk of bias tool.
19 randomized and 14 non-randomized controlled trials on 12 different drugs and 3 non-pharmaceutical interventions with a total of 2,952 patients were included. For the compound preparation, Rumalaya, large and apparently unbiased effects beyond placebo were found for pain (standardized mean difference [SMD] -3.73; 95 % confidence interval [CI] -4.97, -2.50; P < 0.01) and global improvement (risk ratio 12.20; 95 % CI 5.83, 25.54; P < 0.01).
There was also some evidence that effects of the herbal compound preparation Shunti-Guduchi are comparable to those of glucosamine for pain (SMD 0.08; 95 % CI -0.20, 0.36; P = 0.56) and function (SMD 0.15; 95 % CI -0.12, 0.36; P = 0.41).
Based on single trials, positive effects were found for the compound preparations RA-11, Reosto, and Siriraj Wattana. For Boswellia serrata, Lepidium Sativum, a Boswellia serrata containing multicomponent formulation and the compounds Nirgundi Taila, Panchatikta Ghrita Guggulu, and Rhumayog, and for non-pharmacological interventions like Ayurvedic massage, steam therapy, and enema, no evidence for significant effects against potential methodological bias was found.
No severe adverse events were observed in any of the trials.
The authors concluded that the drugs Rumalaya and Shunti-Guduchi seem to be safe and effective drugs for treatment of OA-patients, based on these data. However, several limitations relate to clinical research on Ayurveda. Well-planned, well-conducted and well-published trials are warranted to improve the evidence for Ayurvedic interventions.
I am, of course, pleased that other too have noticed the paucity of good evidence and recommend more and better research into this area. There are, however, several things that worry me about this systematic review:
- How can there be a total absence of adverse effects? Even placebos would generate some.
- The conclusion that Rumalaya and Shunti-Guduchi are safe does not seem justified on the basis of just a few trials.
- My own review found quite encouraging effects for Boswellia serrate.
- 138 electronic databases? I did not even know that so many existed!
- I am also concerned by the way the treatments found to be ‘safe and effective’ are being promoted on the internet:
Rumalaya is a phytopharmaceutical formulation that relieves joint and bone ache associated with various orthopedic ailments. Its natural ingredients possess potent anti-inflammatory properties that alleviate pain. As an immunomodulator, Rumalaya modulates both the humoral and cell-mediated immune response to aches and pain. The medicine has strong anti-arthritic properties that work to combat arthritis.
Indications:
- Rheumatic arthritis
- Rheumatoid arthritis
- Cervical and lumbar spondylosis
- Osteoarthritis
- Arthralgia
- Gout
- Frozen shoulder
- Traumatic inflammatory conditions like fibrositis, bursitis, synovitis, capsulitis, tenosynovitis, myositis and sciatica.
I fail to see good evidence to support most of these claims.
Lastly, I find that the authors fail to warn the public in sufficiently strong terms of some of the drawbacks of Ayurvedic medicines. Many of them seem not to be safe. One of several problems is that they have been shown to be often contaminated/adulterated with toxic substances such as heavy metals.
My conclusion about the value of Ayurvedic medicines is therefore not so optimistic: EFFICACY IS USUALLY MORE THAN DOUBTFUL, WHILE RISKS ARE WELL-DOCUMENTED.