psoriasis
Previous randomized controlled trials (RCTs) suggested that gut microbiota-based therapies may be effective in treating autoimmune diseases, but a systematic summary is lacking. This systematic review was aimed at filling the gap.
The literature searches identified total of 80 RCTs. They related to 14 types of autoimmune disease:
- celiac sprue,
- SLE,
- lupus nephritis (LN),
- RA,
- juvenile idiopathic arthritis (JIA),
- spondyloarthritis,
- psoriasis,
- fibromyalgia syndrome,
- MS,
- systemic sclerosis,
- type 1 diabetes mellitus (T1DM),
- oral lichen planus (OLP),
- Crohn’s disease,
- ulcerative colitis.
The results showed that gut microbiota-based therapies may improve the symptoms and/or inflammatory factor of:
- celiac sprue,
- SLE,
- LN,
- JIA,
- psoriasis,
- PSS,
- MS,
- systemic sclerosis,
- Crohn’s disease,
- ulcerative colitis.
However, gut microbiota-based therapies may not improve the symptoms and/or inflammatory factor of spondyloarthritis and RA. Gut microbiota-based therapies may relieve the pain of fibromyalgia syndrome, but the effect on fibromyalgia impact questionnaire score is not significant. Gut microbiota-based therapies may improve HbA1c in T1DM, but its effect on total insulin requirement does not seem to be significant. Probiotics did not seem to increase the incidence of adverse events.
The authors concluded that gut microbiota-based therapies may improve several autoimmune diseases (celiac sprue, SLE and LN, JIA, psoriasis, fibromyalgia syndrome, PSS, MS, T1DM, Crohn’s disease, and ulcerative colitis).
This sounds promissing, perhaps even a bit too good to be true?
To answer this question, It seems important to look at the quality of the primary studies:
- Twenty-nine RCTs failed to describe the random sequence generation methods.
- Seventeen RCTs were not blinded and their results contained subjective indicators.
- Seven RCTs were rated as high risk of bias.
And what about other caveats?
- The effect sizes vary but are often small.
- There is much heterogeneity.
- For some of the conditions there are only very few trials
- There is no uniform, plausible mode of action.
In summary, while these findings are no doubt interesting, I recommend taking them with a pinch of salt.
This study investigated whether vitamin D and marine-derived long-chain omega 3 fatty acids reduce autoimmune disease risk. A nationwide, randomized, double-blind, placebo-controlled trial with a two-by-two factorial design was conducted in the US. In total, 25 871 participants (12 786 men ≥50 years and 13 085 women ≥55 years at enrollment) took part.
Participants were given
- vitamin D (2000 IU/day),
- matched placebo,
- omega 3 fatty acids (1000 mg/day),
- matched placebo.
Participants self-reported all incident autoimmune diseases from baseline to a median of 5.3 years of follow-up; these diseases were confirmed by extensive medical record review. Cox proportional hazard models were used to test the effects of vitamin D and omega 3 fatty acids on autoimmune disease incidence. The primary endpoint was all incident autoimmune diseases confirmed by medical record review: rheumatoid arthritis, polymyalgia rheumatica, autoimmune thyroid disease, psoriasis, and all others.
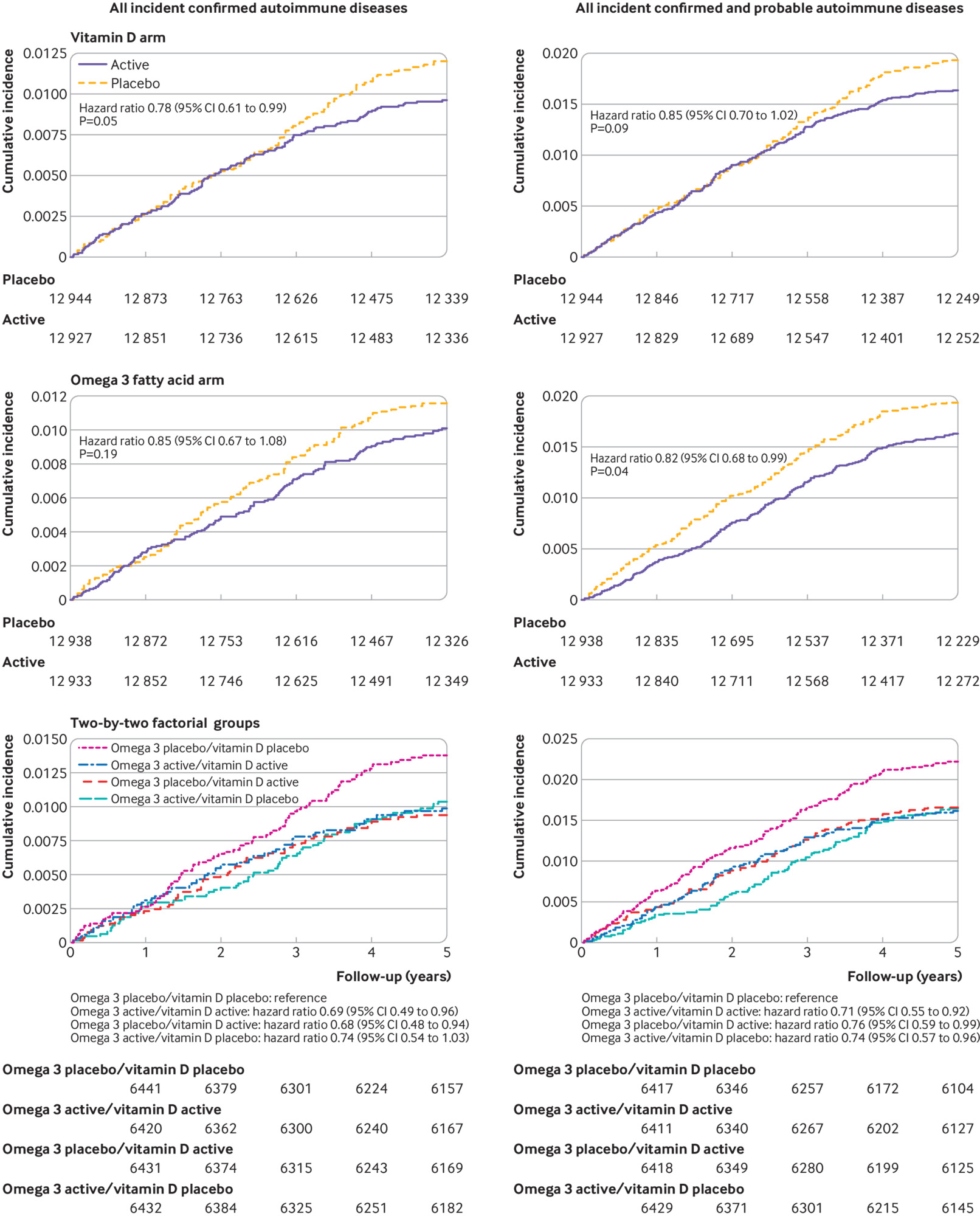
Participants were followed for a median of 5.3 years. 18 046 self-identified as non-Hispanic white, 5106 as black, and 2152 as other racial and ethnic groups. The mean age was 67.1 years. For the vitamin D arm, 123 participants in the treatment group and 155 in the placebo group had a confirmed autoimmune disease (hazard ratio 0.78, 95% confidence interval 0.61 to 0.99, P=0.05). In the omega 3 fatty acids arm, 130 participants in the treatment group and 148 in the placebo group had a confirmed autoimmune disease (0.85, 0.67 to 1.08, P=0.19). Compared with the reference arm (vitamin D placebo and omega 3 fatty acid placebo; 88 with confirmed autoimmune disease), 63 participants who received vitamin D and omega 3 fatty acids (0.69, 0.49 to 0.96), 60 who received only vitamin D (0.68, 0.48 to 0.94), and 67 who received only omega 3 fatty acids (0.74, 0.54 to 1.03) had confirmed autoimmune disease.
The authors concluded that vitamin D supplementation for five years, with or without omega 3 fatty acids, reduced autoimmune disease by 22%, while omega 3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant). Both treatment arms showed larger effects than the reference arm (vitamin D placebo and omega 3 fatty acid placebo).
This is the best trial of dietary supplements that I have seen for a very long time. Yet, the authors caution: Because participants were older adults, the results might not generalize to autoimmune diseases that primarily have their onset in younger people. However, the pathogenesis of many of the specific autoimmune diseases observed (eg, rheumatoid arthritis and psoriasis) is similar in younger adults. The trial tested only one dose and formulation of each supplement. The relatively low number of participants with a confirmed diagnosis of most individual diseases, and the challenge of confirming diagnosis of autoimmune thyroid disease based on medical records, limited statistical power to detect an effect on individual disease outcomes and subgroups of a priori interest. Given the latency of autoimmune disease onset, longer follow-up could be informative, and participants are being followed in an open label extension study.
As regular readers know, I am not easily impressed – but today I am.
Realgar, α-As4S4, is an arsenic sulfide mineral, also known as “ruby sulphur” or “ruby of arsenic”. It is a soft, sectile mineral occurring in monoclinic crystals, or in granular, compact, or powdery form, often in association with the related mineral, orpiment (As2S3).

In Traditional Chinese Medicine (TCM), realgar is often used in combination with herbs. An investigation found a total of 191 different, realgar-containing traditional Chinese patent medicines, and about 87% of them were for oral application. Realgar is said to:
counteract toxic pathogen both externally and internally. For abscess swelling and sores, it can be used singly or in compound prescription for external application mostly. When taken internally, it is combined with blood-activating and abscess-curing herbs to obtain the action of activating blood to relieve swelling, removing toxicity to cure sores. For example, it is combined with Ru Xiang, Mo Yao and She Xiang in Xing Xiao Wan from Wai Ke Quan Sheng Ji. For itching of skin due to scabies and ringworm, it is often combined with dampness-astringing and itching-relieving herbs to obtain actions of killing parasites and curing ringworm, astringing dampness and relieving itching. For instance, it is combined with the same dose of Bai Fan in powder mixed with clear tea for external application in Er Wei Ba Du San from Yi Zong Jin Jian. For poisonous insect bite, it is mixed with sesame oil and then applied on the afflicted sites.
This herb can kill parasites so it is indicated for intestine track parasites. For roundworm induced abdominal pain, it is often combined with other roundworm-killing herbs to reinforce action. For instance, it is combined with Qian Niu Zi and Bing Lang, etc. in Qian Niu Wan from Shen Shi Zun Sheng Shu. For anus pruritus caused by pinworm, it can be made into gauze strip by mixing with vaseline, and then inserted into the anus.
In addition, according to some ancient formulas, this herb can dispel phlegm and check malaria for internal application, so it can also be indicated for epilepsy, asthma and malaria.
Longtime topical over-dose or oral intake of realgar can cause chronic arsenic poisoning and even death. Chinese authors recently published the case of a 35-year-old Chinese man, who was diagnosed with severe psoriasis and died of fatal acute arsenic poisoning after he applied a local folk prescription ointment containing mainly realgar to the affected skin for about 4 days. The autopsy showed multiple punctate haemorrhages over the limbs, pleural effusion, oedematous lungs with consolidation, mild myocardial hypertrophy and normal-looking kidneys. The histopathological examination of renal tissue showed severe degeneration, necrosis and desquamation of renal tubular epithelial cells, presence of protein cast and a widened oedematous interstitium with interstitial fibrosis. The presence of arsenic in large amount in the ointment (about 6%), in blood (1.76 μg/mL), and in skin (4.71 μg/g), were confirmed analytically. The authors also review 7 similar cases in literature.
My advice is that, when you see recommendations by TCM practitioners like this one
you think again and consider that TCM really is not a form of healthcare that can be trusted to be safe.
I have repeatedly cautioned about the often poor quality of research into alternative medicine. This seems particularly necessary with studies of acupuncture, and especially true for such research carried out in China. I have also frequently noted that certain ‘CAM journals’ are notoriously prone to publishing rubbish. So, what can we expect from a paper that:
- is on alternative medicine,
- focusses on acupuncture,
- is authored by Chinese researchers,
- was published in the Journal of Alternative and Complementary Medicine (JACM)?
The answer is PROBABLY NOT A LOT!
As if for confirming my prediction, The JACM just published this systematic review. It reports pairwise and network meta-analyses to determine the effectiveness of acupuncture and acupuncture-related techniques for the treatment of psoriasis. A total of 13 RCTs were included. The methodological quality of these studies was ‘not rigorous’ according to the authors – in fact, it was lousy. Acupoint stimulation seemed to be more effective than non-acupoint stimulation. The short-term treatment effect was superior to the long-term effect (as one would expect with placebo). Network meta-analysis suggested that acupressure or acupoint catgut embedding generate superior effects compared to medications. It was noted that acupressure was the most effective treatment of all the acupuncture-like therapies.
The authors concluded that acupuncture-related techniques could be considered as an alternative or adjuvant therapy for psoriasis in short term, especially of acupressure and acupoint catgut embedding. This study recommends further well-designed, methodologically rigorous, and more head-to-head randomized trials to explore the effects of acupuncture-related techniques for treating psoriasis.
And what is wrong with that?
EVERYTHING!
- The review is of very poor quality.
- The primary studies are even worse.
- The English language is defective to the point of being not understandable.
- The conclusions are misleading.
Correct conclusions should read something like this: Due to the paucity and the poor quality of the clinical trials, this review could not determine whether acupuncture and similar therapies are effective for psoriasis.
And then there is, of course, the question about plausibility. How plausible is the assumption that acupuncture might affect a genetic autoimmune disease like psoriasis. The answer, I think, is that the assumption is highly unlikely.
In the above review, most of the 13 primary RCTs were from China. One of the few studies not conducted in China is this one:
56 patients suffering from long-standing plaque psoriasis were randomized to receive either active treatment (electrostimulation by needles placed intramuscularly, plus ear-acupuncture) or placebo (sham, ‘minimal acupuncture‘) twice weekly for 10 weeks. The severity of the skin lesions was scored (PASI) before, during, and 3 months after therapy. After 10 weeks of treatment the PASI mean value had decreased from 9.6 to 8.3 in the ‘active’ group and from 9.2 to 6.9 in the placebo group (p < 0.05 for both groups). These effects are less than the usual placebo effect of about 30%. There were no statistically significant differences between the outcomes in the two groups during or 3 months after therapy. The patient’s own opinion about the results showed no preference for ‘active’ therapy. It was also clear from the answers that the blinded nature of the study had not been discovered by the patients. In conclusion, classical acupuncture is not superior to sham (placebo) ‘minimal acupuncture‘ in the treatment of psoriasis.
Somehow, I trust these conclusions more than the ones from the review!
And somehow, I get very tired of journal editors failing to do their job of rejecting papers that evidently are embarrassing, unethical rubbish.
For many years, I have been impressed with the high quality and originality of chiropractic research. Here is the abstract of a particularly remarkable, new investigation.
The purpose of this study was to compare characteristics, likelihood to use, and actual use of chiropractic care for US survey respondents with positive and negative perceptions of doctors of chiropractic (DCs) and chiropractic care.
From a 2015 nationally representative survey of 5422 adults (response rate, 29%), we used respondents’ answers to identify those with positive and negative perceptions of DCs or chiropractic care. We used the χ2 test to compare other survey responses for these groups.
Positive perceptions of DCs were more common than those for chiropractic care, whereas negative perceptions of chiropractic care were more common than those for DCs. Respondents with negative perceptions of DCs or chiropractic care were less likely to know whether chiropractic care was covered by their insurance, more likely to want to see a medical doctor first if they were experiencing neck or back pain, less likely to indicate that they would see a DC for neck or back pain, and less likely to have ever seen a DC as a patient, particularly in the recent past. Positive perceptions of chiropractic care and negative perceptions of DCs appear to have greater influence on DC utilization rates than their converses.
CONCLUSION:
We found that US adults generally perceive DCs in a positive manner but that a relatively high proportion has negative perceptions of chiropractic care, particularly the costs and number of visits required by such care. Characteristics of respondents with positive and negative perceptions were similar, but those with positive perceptions were more likely to plan to use-and to have already received-chiropractic care.
END OF ABSTRACT
I bet you are dying to learn who the authors of this impressive article are. Here is the full list and their affiliations:
Weeks WB1, Goertz CM2, Meeker WC3, Marchiori DM4.
- 1Chair, Clinical and Health Services Research Program, Palmer Center for Chiropractic Research, Davenport, IA; Professor, The Geisel School of Medicine at Dartmouth, The Dartmouth Institute for Health Policy and Clinical Practice, Hanover, NH. Electronic address: [email protected].
- 2Vice Chancellor, Research and Health Policy, Palmer College of Chiropractic, Palmer Center for Chiropractic Research, Davenport, IA.
- 3President, Palmer College of Chiropractic West Campus, San Jose, CA.
- 4Chancellor, Palmer College of Chiropractic, Davenport, Iowa.
Not just inexperienced novices then! The authors belong to the crème de la crème of the chiropractic establishment and research!!!
In comparison, I feel like a mere beginner. But let me nevertheless try to design my own study along similar lines. It is so brilliant that I might even get the Nobel Prize for it. Here we go:
The purpose of my study would be to compare characteristics, likelihood to use, and actual use of spectacles for survey respondents with positive and negative perceptions of spectacles and opticians***. From a nationally representative survey of about 5000 adults, I would use the respondents’ answers to identify those with positive and negative perceptions of spectacles and opticians. My results would show that positive perceptions of opticians are more common than those for spectacles, whereas negative perceptions of spectacles are more common than those for opticians. Respondents with negative perceptions of opticians or spectacles were less likely to know whether spectacles were covered by their insurance, more likely to want to see a medical doctor first, if they were experiencing poor eye-sight, less likely to indicate that they would see an optician for poor eye-sight, and less likely to have ever seen an optician as a patient, particularly in the recent past. Positive perceptions of spectacles and negative perceptions of opticians appear to have greater influence on optician utilization rates than their converses. From these data, I would conclude that my sample generally perceive opticians in a positive manner but that a relatively high proportion has negative perceptions of spectacles, particularly the costs and number of visits required for getting them. Characteristics of respondents with positive and negative perceptions were similar, but those with positive perceptions were more likely to plan to use – and to have already received – care from opticians.
*** instead of opticians and spectacles, I might also opt for other things like
- acupuncturists and needles,
- aroma-therapists and essential oils,
- herbalists and herbs,
- fast food restaurants and hamburgers,
- politicians and politics,
- priests and religion,
- etc., etc.
YOU MUST AGREE, THIS DESERVES A NOBEL PRIZE!
I thank the authors of the above paper for having inspired me with their ground-breaking science. In case they receive a Nobel Prize before I do, I congratulate them on their extraordinary achievement in designing, conducting and publishing this truly cutting-edge investigation.
An Indian chain of homeopathic clinics, Dr Batra’s, has just opened its first branch in London. The new website is impressive. It claims homeopathy is effective for the following conditions:
Hair loss? Are they serious? Have they not seen pictures of Samuel Hahnemann?
I decided to look into the psoriasis claim a little closer. This is what they state regarding the homeopathic treatment of psoriasis:
Research-based evidences speak clear and loud of the success of homeopathy in treating psoriasis.
A study published in the Journal of the European Academy of Dermatology and Venereology, a conventional medical Journal, showed that psoriasis patients experienced significant improvement in their quality of life and reduction in their psoriasis symptoms with homeopathy. And this was without any kind of side-effects whatsoever. Of the 82 patients involved in the study that went on for 2 years, many had suffered psoriasis for as long as 15 years and had previously unsuccessfully tried conventional treatments.
At Dr. Batra’s we have successfully treated more than 25,000 cases of psoriasis with homeopathy over the last 35 years. Our safe and scientific solutions have brought smiles to many suffering patients of psoriasis. In fact, a study conducted by A.C. Nielson showed that as compared to general practitioners, specialists and local homeopaths, a higher than average improvement is seen at Dr. Batra’s in treatment of skin ailments.
To the reader who does not look deeper, this may sound fairly convincing. Sadly, it is not. The first study cited above was an uncontrolled trial. Here is its abstract:
Design Prospective multicentre observational study. Objective To evaluate details and effects of homeopathic treatment in patients with psoriasis in usual medical care. Methods Primary care patients were evaluated over 2 years using standardized questionnaires, recording diagnoses and complaints severity, health-related quality of life (QoL), medical history, consultations, all treatments, and use of other health services. Results Forty-five physicians treated 82 adults, 51.2% women, aged 41.6 +/- 12.2 (mean +/- SD) years. Patients had psoriasis for 14.7 +/- 11.9 years; 96.3% had been treated before. Initial case taking took 127 +/- 47 min. The 7.4 +/- 7.4 subsequent consultations (duration: 19.4 +/- 10.5 min) cumulated to 169.0 +/- 138.8 min. Patients received 6.0 +/- 4.9 homeopathic prescriptions. Diagnoses and complaints severity improved markedly with large effect sizes (Cohen’s d= 1.02-2.09). In addition, QoL improved (SF-36 physical component score d = 0.26, mental component score d = 0.49), while conventional treatment and health service use were considerably reduced. Conclusions Under classical homeopathic treatment, patients with psoriasis improved in symptoms and QoL.
It is clear that, due to the lack of a control group, no causal inference can be made between the treatment and the outcome. To claim that otherwise is in my view bogus.
I should mention that there is not a single controlled clinical trial of homeopathy for psoriasis that would support the claim that it is effective.
The second study is not listed in Medline. In fact, the only publication of an author by the name of ‘A C Nielson’ is entitled ‘Are men more intuitive when it comes to eating and physical activity?’. Until I see the evidence, I very much doubt that the study cited above produced strong evidence that homeopathy is an effective cure for psoriasis.
Dr Batra’s chain of clinics boasts to provide the best quality and the highest standards of services that percolate down to all levels in an organisation. Everyone in the institute and those associated with it strive for excellence in whatever they do. Measuring the degree of customer satisfaction was the fundamental concept on which this homeopathic institute’s commitment to become a patient-driven institution was built.
Nice words! SHAME THAT THEY HAVE DECIDED TO DILUTE THEIR TRUTH HOMEOPATHICALLY!