anxiety
In my never-ending search for novel so-called alternative medicines (SCAMs) I came across WATSU. If you had never heard of WATSU, you are in good company (for instance mine). WATSU (water and shiatsu) is a form of passive hydrotherapy in chest-deep thermoneutral water. It was created in the early 1980s by the California-based Shiatsu teacher Harold Dull and combines elements of myofascial stretching, joint mobilization, massage, and shiatsu and is used to address physical and mental issues.
To me, this sounds as though an old physiotherapeutic approach has been re-vamped in order to seem more attractive to the affluent sections of the SCAM brigade. My suspicion seems to be confirmed by SCAM ueber-guru Dr Andrew Weil’s comments:
Dr. Weil has received the therapy many times and often recommends it.
While other bodywork modalities are based on touch in a stationary, two-dimensional world, Watsu offers a different experience. A three-dimensional environment, nearly free from gravity, within a warm and comforting fluid-space and the opportunity to connect with another person all have obvious therapeutic potential.
Achieving states of deep relaxation combined with the therapeutic benefits of good massage therapy can be of great benefit in controlling pain, relieving stress, and recovering from emotional and physical trauma.

But never mind the one-dimensional Dr Weil. The question is: does WATSU work? According to a recent paper, it is effective for a wide range of conditions.
The objective of this systematic review and meta-analyses was to assess the applications, indications, and the effects of WATSU to form a basis for further studies.
Literature searches for “WATSU OR watershiatsu OR (water AND shiatsu)” were conducted without any restrictions in 32 databases. Peer reviewed original articles addressing WATSU as a stand-alone hydrotherapy were assessed for risk of bias. Quantitative data of effects on pain, physical function, and mental issues were processed in random model meta-analyses with subgroup analyses by study design.
Of 1,906 unique citations, 27 articles regardless of study design were assessed for risk of bias. WATSU has been applied to individuals of all ages. Indications covered acute (e.g. pregnancy related low back pain) and chronic conditions (e.g. cerebral palsy) with beneficial effects of WATSU regarding e.g. relaxation or sleep quality. Meta-analyses suggest beneficial effect sizes of WATSU on pain, physical function, and mental issues.
The authors concluded that various applications, indications and beneficial effects of WATSU were identified. The grade of this evidence is estimated to be low to moderate at the best. To strengthen the findings of this study, high-quality RCTs are needed.
Of the 27 studies included in this review, most were case-reports or case series, and only 5 were RCTs. Of these RCTs, none was robust. Some, for instance compared WATSU against no treatment at all, thus not controlling for placebo effects. All of these RCTs had small sample sizes, and all had been published in odd journals of dubious repute.
So, is it justified to categorically conclude that beneficial effects of WATSU were identified?
No, I don’t think so.
That physiotherapy in water can have positive effects on some symptoms would hardly be surprising. But, to convince people who think more critically than Dr Weil, better evidence would be needed.
Aromatherapy is currently one of the most popular of all alternative therapies. It consists of the use of essential oils for medicinal purposes. Aromatherapy usually involves the application of diluted essential oils via a gentle massage of the body surface. Less frequently, the essential oils are applied via inhalation. The chemist Rene-Maurice Gattefosse (1881-1950) coined the term ‘aromatherapy’ after experiencing that lavender oil helped to cure a serious burn. In 1937, he published a book on the subject: Aromathérapie: Les Huiles Essentielles, Hormones Végétales. Later, the French surgeon Jean Valnet used essential oils to help heal soldiers’ wounds in World War II.
This Iranian study aimed to investigate the effect of inhalation aromatherapy with damask rose essence on pain and anxiety in burn patients. This three group clinical trial was conducted on 120 patients with burns less than 30% of total body surface area (TBSA). The patients were randomly allocated into three groups, aromatherapy damask rose essence, placebo, and control. The pain intensity was assessed using visual analogue scale prior to intervention, immediately before, and 15 min after dressing. Anxiety was measured using Spielberger Inventory at before intervention and 15 min after dressing, also the prolonged effect of intervention on pain was assessed by number of the analgesics drugs received for four hours after dressing change. The intervention included inhalation of 6 drops of 40% damask rose essential oil in the damask group, and six drops of distilled water in placebo group one hour before dressing change. The control group received no additional intervention. All groups also received standard care.
Baseline state-trait anxiety and pain intensity were similar in these three groups. A significant reduction was found in pain intensity immediately before and after dressing and state anxiety after dressing in the damask group compared to the placebo and control groups. The researchers found no significant difference between the placebo and control groups in terms of these variables at these times. No significant difference was noted among the three groups in frequency of analgesics drugs and trait anxiety after intervention.
The authors concluded that inhaled aromatherapy with Damask rose essence reduces subjective pain intensity and state anxiety in burned patients. Therefore, it is recommended considering use of damask rose essence, as an easy and affordable method along with other treatments.
These are interesting findings for sure. Aromatherapy is far less implausible than many other so-called alternative medicines (SCAMs). It furthermore has the advantages of being safe and inexpensive.
I have no reason to doubt the validity of the study. Yet, I nevertheless think it is prudent to insist on an independent replication before issuing a general recommendation.
The aim of this systematic review was to assess the efficacy of homeopathic remedies (HRs) in the treatment of mental disorders.
Italian psychiatrists performed a Medline/Embase search for studies written in English and published from any date to October 23, 2018. All randomized controlled trials enrolling patients with any psychiatric disorder and comparing HR with placebo, no treatment, or other psychotropic drugs were included.
A total of 212 studies were screened, 9 met all selection criteria and reported data on major depressive disorder (MDD) (n = 4), generalized anxiety disorder (n = 1), attention-deficit/hyperactivity disorder (n = 2), and premenstrual syndrome/dysphoric disorder (n = 2). Eight of 9 randomized controlled trials showed high risk of bias. Homeopathy showed greater efficacy in MDD compared with fluoxetine, and in premenstrual syndrome/dysphoric disorder compared with placebo, whereas no difference emerged between homeopathy and placebo in MDD and attention deficit/hyperactivity disorder.
The authors concluded that the available data on homeopathy in psychiatric disorders are insufficient to support their use in clinical practice.
In their discussion section, they also add an interesting note of caution: Ethical considerations should therefore prevent clinicians from recommending HRs, which have a cost either for patients or for health care systems, until when a sufficient amount of solid evidence becomes available. In addition, systematic reviews of randomized trials, if unavailable, are advisable for all medical conditions for which homeopathy is currently prescribed.
This is a rigorous, transparent and clear review which generates no surprises. Few critical thinkers would have expected a positive result. It also teaches us, I think, a valuable lesson about the difference between a rigorous and a flimsy review, between independent and biased research. In 2011, evidently pro-homeopathy authors published a paper of the latter kind. Here is its abstract:
Objective: To systematically review placebo-controlled randomized trials of homeopathy for psychiatric conditions.
Data sources: Eligible studies were identified using the following databases from database inception to April 2010: PubMed, CINAHL, PsycINFO, Hom-Inform, Cochrane CENTRAL, National Center for Complementary and Alternative Medicine grantee publications database, and ClinicalTrials.gov. Gray literature was also searched using Google, Google Scholar, the European Committee for Homeopathy, inquiries with homeopathic experts and manufacturers, and the bibliographic lists of included published studies and reviews. Search terms were as follows: (homeopath* or homoeopath*) and (placebo or sham) and (anxiety or panic or phobia or post-traumatic stress or PTSD or obsessive-compulsive disorder or fear or depress* or dysthym* or attention deficit hyperactivity or premenstrual syndrome or premenstrual disorder or premenstrual dysphoric disorder or traumatic brain injury or fibromyalgia or chronic fatigue syndrome or myalgic encephalitis or insomnia or sleep disturbance). Searches included only English-language literature that reported randomized controlled trials in humans.
Study selection: Trials were included if they met 7 criteria and were assessed for possible bias using the Scottish Intercollegiate Guidelines Network (SIGN) 50 guidelines. Overall assessments were made using the Grading of Recommendations Assessment, Development and Evaluation procedure. Identified studies were grouped into anxiety or stress, sleep or circadian rhythm complaints, premenstrual problems, attention-deficit/hyperactivity disorder, mild traumatic brain injury, and functional somatic syndromes.
Results: Twenty-five eligible studies were identified from an initial pool of 1,431. Study quality according to SIGN 50 criteria varied, with 6 assessed as good, 9 as fair, and 10 as poor. Outcome was unrelated to SIGN quality. Effect size could be calculated in 16 studies, and number needed to treat, in 10 studies. Efficacy was found for the functional somatic syndromes group (fibromyalgia and chronic fatigue syndrome), but not for anxiety or stress. For other disorders, homeopathy produced mixed effects. No placebo-controlled studies of depression were identified. Meaningful safety data were lacking in the reports, but the superficial findings suggested good tolerability of homeopathy. A funnel plot in 13 studies did not support publication bias (χ(2)(1) = 1.923, P = .166).
Conclusions: The database on studies of homeopathy and placebo in psychiatry is very limited, but results do not preclude the possibility of some benefit.
The two conclusions speak for themselves, I think. They should remind us that, although systematic reviews are in principle the most reliable source of evidence, it is still necessary to check the quality of the work and the independence of the worker.
Bach-Flower Remedies (BFRs) are often confused with homeopathics. Like them, they contain no active molecule; unlike them, they are not potentised nor used according to the ‘like cures like’ assumption. Both have in common that they are as popular as implausible.
Few studies have tested BFRs; my own systematic review of controlled clinical trials was published in 2010:
Bach flower remedies continue to be popular and its proponents make a range of medicinal claims for them. The aim of this systematic review was to critically evaluate the evidence for these claims. Five electronic databases were searched without restrictions on time or language. All randomised clinical trials of flower remedies were included. Seven such studies were located. All but one were placebo-controlled. All placebo-controlled trials failed to demonstrate efficacy. It is concluded that the most reliable clinical trials do not show any differences between flower remedies and placebos.
Now a new study has emerged. This trial from the Department of Pedodontics and Preventive Dentistry, DY Patil University – School of Dentistry, Navi Mumbai, Maharashtra, India, compared the effects of Bach Flower Therapy (BFT) and music therapy (MT) on the dental anxiety in paediatric patients. A total of 120 children (aged 4-6 years) were selected and randomly allocated to one of three groups:
- BFT group: Children from this group were administered orally four drops of “rescue remedy” diluted in 40 mL of water 15 min before the treatment. Children were asked to wear headphones without playing any music during the dental treatment
- MT group: Children from this group were provided with a headphone, and Indian classical instrumental music (Raag Sohni played by Pandit Shiv Kumar Sharma on santoor) was played during the scheduled dental treatment. Children were also given 40 mL plain water to drink 15 min before the treatment
- Control group: Children from this group were given 40 mL plain water 15 min before the treatment. During the treatment, children were asked to wear the headphone without playing any music.
All children received oral prophylaxis and fluoride treatment (no further details provided). Dental anxiety was evaluated using
- North Carolina Behavior Rating Scale (NCBRS), the primary outcome measure,
- Facial Image Scale (FIS),
- and physiological parameters.
Significantly better behaviour was seen in children from the BFT group as compared to the control group (P = 0.014). FIS scores measured postoperatively did not show significant differences among the groups.


Children from the BFT and MT groups showed a significant decrease in the pulse rates intraoperatively from the preoperative period. Intraoperative systolic blood pressure in children from the MT group was significantly lower than both the BFT and the control groups. Diastolic blood pressure significantly increased in the control group intra-operatively, whereas other groups showed a decrease.
The authors concluded that the results of this study demonstrate significant effects of both single dose of BFT and exposure to MT, on reduction of dental anxiety in children aged between 4 and 6 years.
I find these findings most puzzling (like all BFRs, Rescue Remedies do not contain a single active molecule that could explain them) and strongly recommend that we wait until we have an independent replication before accepting these results as trustworthy.
The University College London Hospitals (UCLH) include the ‘Royal London Hospital for Integrated Medicine’ (RLHIM). The RLHIM offers a range of so-called alternative medicines (SCAMs), including acupuncture.

This is how they advertise traditional acupuncture to the unsuspecting public:
Acupuncture is a part of Traditional Chinese Medicine (TCM). This is a system of healing which has been practised in China and other Eastern countries for thousands of years.
Although often used as a means of pain relief, it can treat people with other illnesses. The focus is on improving the overall well-being of the patient, rather than the isolated treatment of specific symptoms.
You will be seen individually and assessed by an acupuncturist trained in TCM. They will use traditional Chinese techniques including pulse, tongue and abdominal diagnosis. They will also ask you about your medical history and lifestyle.
The TCM trained acupuncturist can stimulate the body’s own healing response and help to restore its natural balance.
The principal aim of acupuncture in treating the whole person is to create balance between your physical, emotional and spiritual needs. It can help to relax, improve mood and sleep, relieve tension and improve your sense of well-being, as well as improving symptoms.
We will assess your individual needs and discuss a treatment plan with you during your initial consultation.
The treatment may include the use of the following:
- The use of fine acupuncture needles
- Moxibustion (burning of the herb mugwort close to the surface of the skin)
- Cupping therapy (to create local suction on the skin)
- Acupressure (pressure applied to acu-points to stimulate energy flow)
- Electro-acupuncture (a low voltage current is passed between 2 needles)
________________________________________________________________
How reliable is this information? I will try to answer this question by discussing the 6 statements that, in my view, are most questionable.
Although often used as a means of pain relief, it can treat people with other illnesses
Whether acupuncture is effective for pain relief is debatable. A recent analysis cast considerable doubt on the assumption. The notion that acupuncture ‘can treat people with other illnesses’ seems like a ‘carte blanche’ for treating virtually any condition regardless of evidence.
Improving the overall well-being of the patient
I am not aware of sound evidence that acupuncture is an effective treatment for improving overall well-being.
Traditional Chinese techniques including pulse, tongue and abdominal diagnosis
These diagnostic techniques have not been adequately validated and have no place in evidence-based healthcare.
The TCM trained acupuncturist can stimulate the body’s own healing response and help to restore its natural balance
I am not aware of sound evidence to show that acupuncture stimulates healing. The statement seems like another ‘carte blanche’ for treating anything the therapist feels like, regardless of evidence.
The principal aim of acupuncture in treating the whole person is to create balance between your physical, emotional and spiritual needs
The claim that acupuncture is a holistic treatment is based on little more than wishful thinking by acupuncturists.
It can help to relax, improve mood and sleep, relieve tension and improve your sense of well-being, as well as improving symptoms
I am not aware of sound evidence that acupuncture is effective in treating any of the named conditions. The end of the sentence (‘as well as improving symptoms’) is another ‘carte blanche’ for doing anything the acupuncturists feels like.
______________________________________________________________________
The UCLH are firmly committed to EBM. The RLHIM claims to be ‘a centre for evidence-based practice’. This claim is not supported by the above advertisement of acupuncture which is clearly not based on good evidence. Moreover, it has the potential to mislead vulnerable patients and thus cause considerable harm. In my view, it is high time that the UCLH address this problem.
Neurolinguistic programming (NLP) was developed in the mid-seventies. It is a so-called alternative therapy (SCAM) that is not easy to define. Those who started it and those involved in it use such vague language that NLP means different things to different people. One metaphor keeps recurring: NLP claims to help people change by teaching them to program their brains. We were given brains, we are told, without an instruction manual, and NLP offers a user-manual for the brain. Consciously or unconsciously, NLP is based on the assumptions that:
- the unconscious mind constantly influences our conscious thoughts and actions;
- Freud’s theories are correct;
- hypnotherapy is effective.

Wikipedia is more outspoken about it: Neuro-linguistic programming (NLP) is a pseudoscientific approach to communication, personal development, and psychotherapy…
Despite the fact that NLP is unproven (to say the least), the COLLEGE OF MEDICINE AND INTEGRATED HEALTH (COMAIH) is sufficiently impressed by NLP to offer a course for GPs and SCAM practitioners. Here is their announcement:
Neurolinguistic Healthcare in association with the College of Medicine brings you a 2-day Introduction to Hypnosis, Neurolinguistic Programming (NLP) and Neurolinguistic Healthcare (NLH). Dr Wong and Dr Akhtar who lead the course are Trainers in NLP and Hypnosis and GPs who apply their skills in daily practice within the 10-minute consultation. The course is suitable for both medical professionals and complementary therapists. This is a limited training event offered by them to share their years of knowledge and skills with you.
You will learn:
-
- A basic overview of NLP and the most useful aspects to use it to begin making effective changes in how you and the people you treat think and behave
- An understanding of the NLH model of the mind so that you understand the concepts of therapy using this mixed hypnosis/ NLP approach in relation to health.
- The ability to Hypnotise effectively in a very short period of time with practical experience – the ability to go through all the stages of hypnosis – the induction, deepening, therapy, and emergence, including rapid hypnosis techniques. (Hypnosis courses which are less practical often charge in excess of £2000 for this)
- Learn at least 3 therapeutic techniques, including the NLP therapeutic techniques which work much better in trance, so using and applying the skills you will learn in hypnosis
- Access to an online mentorship programme with Dr Akhtar or Dr Wong for 6 months and who will provide 3x30mins group webinar meetings after the course to ensure any remaining questions get answered and that you are actually going forth to apply these skills. (worth another £600 in value)
- Access to an online learning membership site with educational videos and other content like pain relief techniques, papers with therapeutic scripts, etc
This is an opportunity to learn a different way of helping people from doctors who target the 10-minute consultation with fast, effective formal hypnosis techniques and sleight-of-mouth. It is possible to make change happen in 10-minutes.
Note that attending this course will not make you a certified hypnotherapist, but confer you the skills you will learn to use personally and in the context of guided meditations and relaxations that are commonplace now.
And what evidence do I have for stating that NLP is unproven?
Is there an up-to-date and sound systematic review of NLP?
The answer is yes.
This systematic review of NLP included 10 experimental studies. Five studies were RCTs and five were uncontrolled pre-post studies. Targeted health conditions were anxiety disorders, weight maintenance, morning sickness, substance misuse, and claustrophobia during MRI scanning. NLP interventions were mainly delivered across 4-20 sessions although three were single session. Eighteen outcomes were reported and the RCT sample sizes ranged from 22 to 106. Four RCTs reported no significant between group differences with the fifth finding in favour of NLP. Three RCTs and five pre-post studies reported within group improvements. Risk of bias across all studies was high or uncertain.
The authors concluded that there is little evidence that NLP interventions improve health-related outcomes. This conclusion reflects the limited quantity and quality of NLP research, rather than robust evidence of no effect. There is currently insufficient evidence to support the allocation of NHS resources to NLP activities outside of research purposes.
Surprised?
I am not!
I did not expect the COMAIH to allow critical thinking to get in the way of quackery-promotion.
This post is dedicated to all who claim that I never discuss anything positive about so-called alternative medicine (SCAM).
Autogenic training is a therapy developed in the 1920s by the German psychiatrist Johannes Heinrich Schultz (1884 – 1970). It is an auto-hypnotic relaxation technique popular in Germany but less so other countries. (The lack of international appreciation of autogenic training might be related to Schultz’ well-documented Nazi past. In 1935, he published an essay which supported compulsory sterilization of men to eliminate hereditary illnesses. Later he was appointed deputy director of the Göring Institute in Berlin. Through this institute, he had an active role in the extermination of mentally handicapped individuals in the framework of the ‘Aktion T4’, the Nazi’s infamous euthanasia programme.)
Autogenic training consists of mental exercises using instructions directed at different parts of the body to control bodily perceptions, such as ‘my right foot feels warm’ or ‘my left arm feels heavy’. Patients tend to report an intense sense of relaxation during and after autogenic training. Autogenic training is taught in a series of lessons by a qualified instructor.
Autogenic training should be practised regularly and does not require further supervision. It is thus an inexpensive therapy. The technique is claimed to help for a range of (mostly stress-related) conditions. However, the evidence from clinical trials is scarce and, not least due to methodological problems, less than convincing.
This systematic review was conducted to evaluate the effectiveness of autogenic training on stress responses. A total 11 studies were included in a meta-analysis. They showed that autogenic training decreased anxiety and depression, and increased the high frequency of heart rate variability as well as a reduction of anxiety score by 1.37 points (n=85, SMD=-1.37: 95% CI -2.07 to -0.67), in the studies on short-term intervention targeting healthy adults.For depression, a reduction was noted of the symptom score by 0.29 point (n=327, SMD=-0.29: 95% CI -0.50 to -0.07) in the studies on long term intervention targeting the patient group.
The authors concluded that autogenic training is effective for adults’ stress management, and nurses will be able to effectively perform autogenic training programs for workers’ stress relief at the workplace.
I cannot access the full article because it was published in Korean. Nevertheless, I feel that the conclusions are probably correct.
Why?
Because I know (most of) the primary studies and three of the RCTs are my own.
(Yet, some of my critics continue to claim that I never conducted any positive studies of SCAM)
After a previous post about aromatherapy, someone recently commented:
I love essential oils and use them daily. Essential oils became a part of my life! I do feel better with it! Why I need clinical trials so?
The answer is probably: you don’t need clinical trials for a little pampering that makes you feel good.
But, if someone claims that aromatherapy (or indeed any other treatment) is effective for this or that medical condition, we need proof in the form of a clinical trial. By proof, we usually mean a clinical trial.
One like this new study, perhaps?
The aim of this study was to evaluate the use of a lavender aromatherapy skin patch on anxiety and vital sign variability during the preoperative period in female patients scheduled for breast surgery. Participants received an aromatherapy patch in addition to standard preoperative care. Anxiety levels were assessed with a 10-cm visual analogue scale (VAS) at baseline and then every 15 minutes after patch placement. Vital sign measurements were recorded at the same interval. There was a statistically significant decrease (P = .03) in the anxiety VAS measurements from baseline to final scores.
The authors concluded that the findings from this study suggest the use of aromatherapy is beneficial in reducing anxiety experienced by females undergoing breast surgery. Further research is needed to address the experience of preoperative anxiety, aromatherapy use, and the challenges of managing preoperative anxiety.
No, not one like this study!
This study – its called it a ‘pilot study’ – tells us nothing of value.
Why?
- It was not a pilot study because it did not pilot anything; its aim was to evaluate aromatherapy.
- But it could not evaluate aromatherapy because it had no control group. This means the reduction in anxiety was almost certainly not a specific effect of the therapy, but a non-specific effect due to the extra attention, expectation, etc.
- This means that the conclusion (the use of aromatherapy is beneficial) is not justified.
- In turn, this means that the paper is not helpful in any way. All it can possibly do is to mislead the public.
In summary: another fine example of pseudo-research that, I believe, is worse than no research at all.
Aromatherapy usually involves the application of diluted essential (volatile) oils via a gentle massage of the body surface. The chemist Rene-Maurice Gattefosse (1881-1950) coined the term ‘aromatherapy’ after experiencing that lavender oil helped to cure a severe burn of his hand. In 1937, he published a book on the subject: Aromathérapie: Les Huiles Essentielles, Hormones Végétales. Later, the French surgeon Jean Valnet used essential oils to help heal soldiers’ wounds in World War II.
Aromatherapy is currently one of the most popular of all alternative therapies. The reason for its popularity seems simple: it is an agreeable, luxurious form of pampering. Whether it truly merits to be called a therapy is debatable.
The authors of this systematic review stated that they wanted to critically assess the effect of aromatherapy on the psychological symptoms as noted in the postmenopausal and elderly women. They conducted electronic literature searches and fount 4 trials that met their inclusion criteria. The findings demonstrated that aromatherapy massage significantly improves psychological symptoms in menopausal, elderly women as compared to controls. In one trial, aromatherapy massage was no more effective than the untreated group regarding their experience of symptoms such as nervousness.
The authors concluded that aromatherapy may be beneficial in attenuating the psychological symptoms that these women may experience, such as anxiety and depression, but it is not considered as an effective treatment to manage nervousness symptom among menopausal women. This finding should be observed in light of study limitations.
In the discussion section, the authors state that to the best of our knowledge, this is the first meta-analysis evaluating the effect of aromatherapy on the psychological symptoms. I believe that they might be mistaken. Here are two of my own papers (other researchers have published further reviews) on the subject:
- Aromatherapy is the therapeutic use of essential oil from herbs, flowers, and other plants. The aim of this overview was to provide an overview of systematic reviews evaluating the effectiveness of aromatherapy. We searched 12 electronic databases and our departmental files without restrictions of time or language. The methodological quality of all systematic reviews was evaluated independently by two authors. Of 201 potentially relevant publications, 10 met our inclusion criteria. Most of the systematic reviews were of poor methodological quality. The clinical subject areas were hypertension, depression, anxiety, pain relief, and dementia. For none of the conditions was the evidence convincing. Several SRs of aromatherapy have recently been published. Due to a number of caveats, the evidence is not sufficiently convincing that aromatherapy is an effective therapy for any condition.
- Aromatherapy is becoming increasingly popular; however there are few clear indications for its use. To systematically review the literature on aromatherapy in order to discover whether any clinical indication may be recommended for its use, computerised literature searches were performed to retrieve all randomised controlled trials of aromatherapy from the following databases: MEDLINE, EMBASE, British Nursing Index, CISCOM, and AMED. The methodological quality of the trials was assessed using the Jadad score. All trials were evaluated independently by both authors and data were extracted in a pre-defined, standardised fashion. Twelve trials were located: six of them had no independent replication; six related to the relaxing effects of aromatherapy combined with massage. These studies suggest that aromatherapy massage has a mild, transient anxiolytic effect. Based on a critical assessment of the six studies relating to relaxation, the effects of aromatherapy are probably not strong enough for it to be considered for the treatment of anxiety. The hypothesis that it is effective for any other indication is not supported by the findings of rigorous clinical trials.
Omitting previous research may be odd, but it is not a fatal flaw. What makes this review truly dismal is the fact that the authors fail to discuss the poor quality of the primary studies. They are of such deplorable rigor that one can really not draw any conclusion at all from them. I therefore find the conclusions of this new paper unacceptable and think that our statement (even though a few years old) is much more accurate: the evidence is not sufficiently convincing that aromatherapy is an effective therapy for any condition.
Fish oil (omega-3 PUFA) preparations are today extremely popular and amongst the best-researched dietary supplement. During the 1970s, two Danish scientists, Bang and Dyerberg, remarked that Greenland Eskimos had a baffling lower prevalence of coronary artery disease than mainland Danes. They also noted that their diet contained large amounts of seal and whale blubber and suggested that this ‘Eskimo-diet’ was a key factor in the lower prevalence. Subsequently, a flurry of research stared to investigate the phenomenon, and it was shown that the ‘Eskimo-diet’ contained unusually high concentrations of omega-3 polyunsaturated fatty acids from fish oils (seals and whales feed predominantly on fish).
Initial research also demonstrated that the regular consumption of fish oil has a multitude of cardiovascular and anti-inflammatory effects. This led to the promotion of fish oil supplements for a wide range of conditions. Meanwhile, many of these encouraging findings have been overturned by more rigorous studies, and the enthusiasm for fish oil supplements has somewhat waned. But now, a new paper has come out with surprising findings.
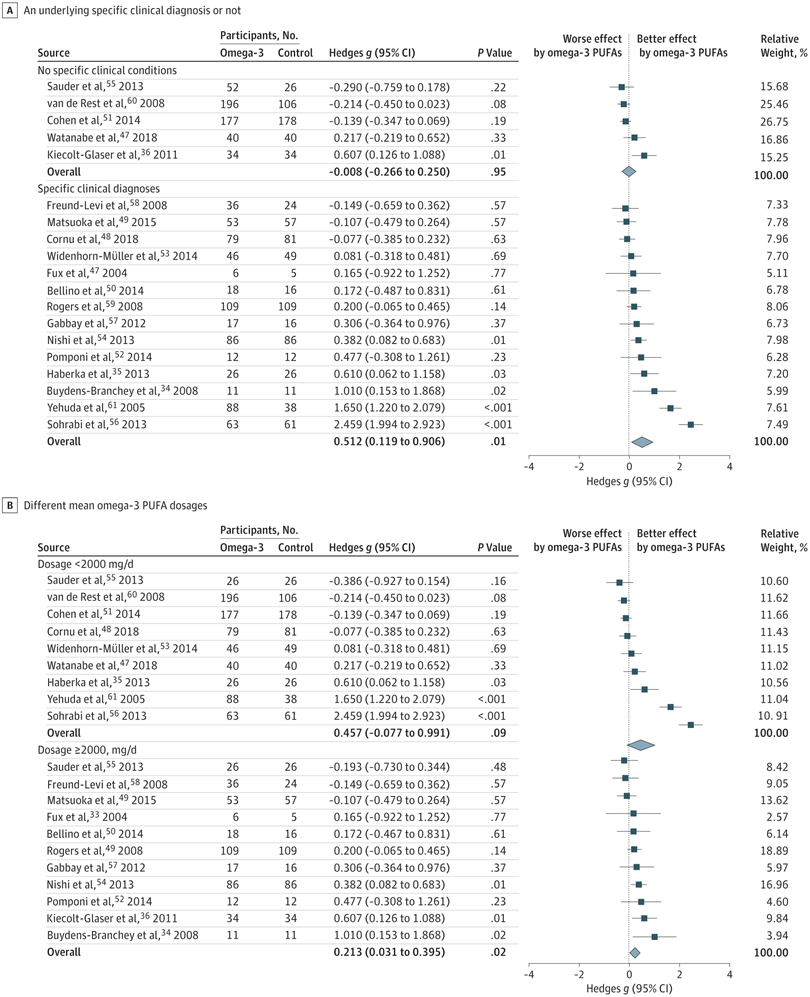
The objective of this meta-analysis was to evaluate the association of anxiety symptoms with omega-3 PUFA treatment compared with controls in varied populations.
A search was performed of clinical trials assessing the anxiolytic effect of omega-3 PUFAs in humans, in either placebo-controlled or non–placebo-controlled designs. Of 104 selected articles, 19 entered the final data extraction stage. Two authors independently extracted the data according to a predetermined list of interests. A random-effects model meta-analysis was performed. Changes in the severity of anxiety symptoms after omega-3 PUFA treatment served as the main endpoint.
In total, 1203 participants with omega-3 PUFA treatment and 1037 participants without omega-3 PUFA treatment showed an association between clinical anxiety symptoms among participants with omega-3 PUFA treatment compared with control arms. Subgroup analysis showed that the association of treatment with reduced anxiety symptoms was significantly greater in subgroups with specific clinical diagnoses than in subgroups without clinical conditions. The anxiolytic effect of omega-3 PUFAs was significantly better than that of controls only in subgroups with a higher dosage (at least 2000 mg/d) and not in subgroups with a lower dosage (<2000 mg/d).
The authors concluded that this review indicates that omega-3 PUFAs might help to reduce the symptoms of clinical anxiety. Further well-designed studies are needed in populations in whom anxiety is the main symptom.
I think this is a fine meta-analysis reporting clear results. I doubt that this paper truly falls under the umbrella of alternative medicine, but fish oil is a popular food supplement and should be mentioned on this blog. Of course, the average effect size is modest, but the findings are nevertheless intriguing.