alternative therapist
I hear this argument so regularly that it might be worth analysing it (yet again) a bit closer.
It is used with the deepest of convictions by proponents of all sorts of quackery who point out that science does not know or explain everything – and certainly not their (very special) therapy. Science is just not sophisticated enough, they say; in fact, a few years ago, it could not even explain how Aspirin works. And just like Aspirin, their very special therapy – let’s call it energy healing (EH) for the sake of this post – does definitely and evidently work. There even is ample proof:
- Patients get better after using EH, and surely patients don’t lie.
- Patients pay for EH, and who would pay for something that does not work?
- EH has survived hundreds of years, and ineffective therapies don’t.
- EH practitioners have tons of experience and therefore know best.
- They are respected by very important people and organisations.
- EH is even reimbursed by some insurance companies.
You have all heard the argument, I’m sure.
How to respond?
The ‘proofs’ listed above are simply fallacies; as such they do not need more detailed discussions, I hope.
But how can we refute the notion that science is not yet sufficiently advanced to explain EH?
The simplest approach might be to explain that science has already tested EH and found it to be ineffective. There really is nothing more to say. And the often-quoted example of Aspirin does clearly not wash. True, a few decades ago, we did not know how it worked. But we always knew that it worked because we conducted clinical trials, and they generated positive results. These findings we the main reasons why scientists wanted to find out how it works, and eventually they did (and even got a Nobel Prize for it). Had the clinical trials not shown effectiveness, nobody would have been interested in alleged mechanisms of action.
With EH, things are different. Rigorous clinical trials of EH have been conducted, and the totality of this evidence fails to show that EH works. Therefore, chasing after a mechanism of action would be silly and wasteful. It’s true, science cannot explain EH, but this is not because it is not yet sophisticated enough; it is because there is nothing to explain. EH has been disproven, and waffling about ‘science is not yet able to explain it’ is either a deliberate lie or a serious delusion.
So far so good. But what if EH had not been submitted to clinical trials?
In such cases, the above line of argument would not work very well.
For instance, as far as I know, there is not a single rigorous clinical trial of crystal healing (CH). Does that mean that perhaps CH-proponents are correct when claiming that it does evidently work and science simply cannot yet understand how?
No, I don’t think so.
Like most of the untested alternative therapies, CH is not based on plausible assumptions. In fact, the implausibility of the underlying assumptions is the reason why such treatments have not and probably never will be submitted to rigorous clinical trials. Why should anyone waste his time and our money running expensive tests on something that is so extremely unlikely? Arguably doing so would even be unethical.
With highly implausible therapies we need no trials, and we do not need to fear that science is not yet sufficiently advance to explain them. In fact, science is sufficiently advanced to be certain that there can be no explanation that is in line with the known laws of nature.
Sadly, some truly deluded fans of CH might still not be satisfied and respond to our reasoning that we need a ‘paradigm shift’. They might say that science cannot explain CH because it is stuck in the straightjacket of an obsolete paradigm which does not cater for phenomena like CH.
Yet this last and desperate attempt of the fanatics is not a logical refuge. Paradigm shifts are not required because some quack thinks so, they are needed only if data have been emerging that cannot possibly be explained within the current paradigm. But this is never the case in alternative medicine. We can explain all the experience of advocates, positive results of researchers and ‘miracle’ cures of patients that are being reported. We know that the experiences are real, but are sure that their explanations of the experience are false. They are not due to the treatment per se but to other phenomena such as placebo effects, natural history, regression towards the mean, spontaneous recovery, etc.
So, whichever way we turn things, and whichever way enthusiasts of alternative therapies twist them, their argument that ‘SCIENCE IS NOT YET ABLE TO EXPLAIN’ is simply wrong.
Samuel Hahnemann published a lot, but his main ideas about homeopathy are summarised in his ‘Organon‘ which has thus become ‘the bible’ for all homeopaths. They regularly refer to this book, yet I sometimes get the impression that many of them have even read it.
I did! Most recently, I re-studied it when writing my own book ‘HOMEOPATHY, THE UNDILUTED FACTS‘. And I have to say, it is rather boring, full of contradictions and obsolete nonsense.
To mark Samuel’s birthday – he was born on 10 April 1755 in Meissen – I take the liberty of quoting directly from Dudgeon’s translation of the 1st edition of the Organon:
- In no way whatever can [a] disease itself be recognized.
- This eternal, universal law of nature [the like cures like assumption]…
- …only one disease can exist in the body at any one time…
- …if an acute infection attacks an organism already suffering from a similar acute disease, then the stronger infection uproots the weaker entirely and removes it homoeopathically.
- …diseases are only destroyed by similar diseases.
- …it is certain that a suitably selected homoeopathic remedy gently destroys and removes disease…
- …aggravation during the first hours… is, in fact, a very good prognostic sign…
- …even the smallest dose of a homoeopathic remedy always causes a small homoeopathic aggravation…
- …we should always choose the very smallest doses…
- …hardly any dose of the homoeopathically selected remedy can be so small as not to be stronger than the natural disease…
- If dilution is also employed… an excessive effect is easily produced.
- …a single drop of a tincture to a pound of water and shaking vigorously… will produce more effect than a single dose of eight drops of the tincture.
- …this action must be called spirit-like.
For homeopaths, these quotes (should) depict some of the central assumptions of homeopathy. For non-homeopaths, they are just gibberish that makes no sense whatsoever. Time has moved on, and most of us have moved with it. Yet homeopaths still live by (and from) the errors of 200 years ago.
Hahnemann died on 2 July 1843 in Paris. I don’t want to be disrespectful, but perhaps we should, in future, rather celebrate this date? It could be a celebration of the progress we made since (and because) we have recognised Hahnemann’s errors.
In the current issue of the Faculty of Homeopathy‘s Simile publication, Dr Peter Fisher, the Queen’s homeopath, re-visits the old story of the ‘Smallwood Report’. To my big surprise, I found the following two paragraphs in his editorial:
A prepublication draft [of the Smallwood report] was circulated for comment with prominent warnings that it was confidential and not to be shared more widely (I can personally vouch for this, since I was one of those asked to comment). Regrettably, Prof Ernst did precisely this, leaking it to The Times who used it as the basis of their lead story. The editor of The Lancet, Richard Horton, certainly no friend of homeopathy, promptly denounced Ernst for having “broken every professional code of scientific behaviour”.
Sir Michael Peat, the Prince of Wales’ Principal Private Secretary, wrote to the vice chancellor of Exeter University protesting at the leak, and the university conducted an investigation. Ernst’s position became untenable, funding for his department dried up and he took early retirement. Thirteen years later he remains sore; in his latest book More Harm than Good? he attacks the Prince of Wales as “foolish and immoral”.
END OF QUOTE
Sadly it is true that Horton wrote these defaming words. Subsequently, I asked him to justify them explaining that they were being used by my university against me. He ignored several of my emails, but eventually he sent a reply. In it, he said that, since the university was investigating the issue, the truth would doubtlessly be disclosed. I remember that I was livid at the arrogance and ignorance of this reply. However, being in the middle of my university’s investigation against me, never did anything about it. Looking back at this part of the episode, I feel that Horton behaved abominably.
But back to Dr Fisher.
Why did his defamatory and false accusation in his new editorial come as a ‘big surprise’ to me?
Should I not have gotten used to the often odd way in which some homeopaths handle the truth?
Yes, I did get used to this phenomenon; but I am nevertheless surprised because I have tried to correct Fisher’s ‘error’ before.
This is from a post about Fisher which I published in 2015:
In this article [available here in archive,org – Admin] which he published as Dr. Peter Fisher, Homeopath to Her Majesty, the Queen, he wrote: There is a serious threat to the future of the Royal London Homoeopathic Hospital (RLHH), and we need your help…Lurking behind all this is an orchestrated campaign, including the ’13 doctors letter’, the front page lead in The Times of 23 May 2006, Ernst’s leak of the Smallwood report (also front page lead in The Times, August 2005), and the deeply flawed, but much publicised Lancet meta-analysis of Shang et al…
If you have read my memoir, you will know that even the hostile 13-months investigation my own university did not find me guilty of the ‘leak’. The Times journalist who interviewed me about the Smallwood report already had the document on his desk when we spoke, and I did not disclose any contents of the report to him…
END OF QUOTE
So, assuming that Dr Peter Fisher has seen my 2015 post, he is knowingly perpetuating a slanderous untruth. However, giving him the benefit of the doubt, he might not have read the post nor my memoir and could be unaware of the truth. Error or lie? I am determined to find out and will send him today’s post with an offer to clarify the situation.
I will keep you posted.
In recent days, journalists across the world had a field day (mis)reporting that doctors practising integrative medicine were doing something positive after all. I think that the paper shows nothing of the kind – but please judge for yourself.
The authors of this article wanted to determine differences in antibiotic prescription rates between conventional General Practice (GP) surgeries and GP surgeries employing general practitioners (GPs) additionally trained in integrative medicine (IM) or complementary and alternative medicine (CAM) (referred to as IM GPs) working within National Health Service (NHS) England.
They conducted a retrospective study on antibiotic prescription rates per STAR-PU (Specific Therapeutic group Age–sex weighting Related Prescribing Unit) using NHS Digital data over 2016. Publicly available data were used on prevalence of relevant comorbidities, demographics of patient populations and deprivation scores. setting Primary Care. Participants were 7283 NHS GP surgeries in England. The association between IM GPs and antibiotic prescribing rates per STAR-PU with the number of antibiotic prescriptions (total, and for respiratory tract infection (RTI) and urinary tract infection (UTI) separately) as outcome. results IM GP surgeries (n=9) were comparable to conventional GP surgeries in terms of list sizes, demographics, deprivation scores and comorbidity prevalence.
Statistically significant fewer total antibiotics were prescribed at NHS IM GP surgeries compared with conventional NHS GP surgeries. In contrast, the number of antibiotics prescribed for UTI were similar between both practices.
The authors concluded that NHS England GP surgeries employing GPs additionally trained in IM/CAM have lower antibiotic prescribing rates. Accessibility of IM/CAM within NHS England primary care is limited. Main study limitation is the lack of consultation data. Future research should include the differences in consultation behaviour of patients self-selecting to consult an IM GP or conventional surgery, and its effect on antibiotic prescription. Additional treatment strategies for common primary care infections used by IM GPs should be explored to see if they could be used to assist in the fight against antimicrobial resistance.
The study was flimsy to say the least:
- It was retrospective and is therefore open to no end of confounders.
- There were only 9 surgeries in the IM group.
Moreover, the results were far from impressive. The differences in antibiotic prescribing between the two groups of GP surgeries were minimal or non-existent. Finally, the study was financed via an unrestricted grant of WALA Heilmittel GmbH, Germany (“approx. 900 different remedies conforming to the anthroposophic understanding of man and nature”) and its senior author has a long track record of publishing papers promotional for anthroposophic medicine.
Such pseudo-research seems to be popular in the realm of CAM, and I have commented before on similarly futile projects. The comparison, I sometimes use is that of a Hamburger restaurant:
Employees by a large Hamburger chain set out to study the association between utilization of Hamburger restaurant services and vegetarianism. The authors used a retrospective cohort design. The study population comprised New Hampshire residents aged 18-99 years, who had entered the premises of a Hamburger restaurant within 90 days for a primary purpose of eating. The authors excluded subjects with a diagnosis of cancer. They measured the likelihood of vegetarianism among recipients of services delivered by Hamburger restaurants compared with a control group of individuals not using meat-dispensing facilities. They also compared the cohorts with regard to the money spent in Hamburger restaurants. The adjusted likelihood of being a vegetarian was 55% lower among the experimental group compared to controls. The average money spent per person in Hamburger restaurants were also significantly lower among the Hamburger group.
To me, it is obvious that such analyses must produce a seemingly favourable result for CAM. In the present case, there are several reasons for this:
- GPs who volunteer to be trained in CAM tend to be in favour of ‘natural’ treatments and oppose synthetic drugs such as antibiotics.
- Education in CAM would only re-inforce this notion.
- Similarly, patients electing to consult IM GPs tend to be in favour of ‘natural’ treatments and oppose synthetic drugs such as antibiotics.
- Such patients might be less severely ill that the rest of the patient population (the data from the present study do in fact imply this to be true).
- These phenomena work in concert to generate less antibiotic prescribing in the IM group.
In the final analysis, all this finding amounts to is a self-fulfilling prophecy: grocery shops sell less meat than butchers! You don’t believe me? Perhaps you need to read a previous post then; it concluded that physicians practicing integrative medicine (the 80% who did not respond to the survey were most likely even worse) not only use and promote much quackery, they also tend to endanger public health by their bizarre, irrational and irresponsible attitudes towards vaccination.
What is upsetting with the present paper, in my view, are the facts that:
- a reputable journal published this junk,
- the international press has a field-day reporting this study implying that CAM is a good thing.
The fact is that it shows nothing of the kind. Imagine we send GPs on a course where they are taught to treat all their patients with blood-letting. This too would result in less prescription of antibiotics, wouldn’t it? But would it be a good thing? Of course not!
True, we prescribe too much antibiotics. Nobody doubts that. And nobody doubts that it is a big problem. The solution to this problem is not more CAM, but less antibiotics. To realise the solution we do not need to teach GPs CAM but we need to remind them of the principles of evidence-based practice. And the two are clearly not the same; in fact, they are opposites.
Did you know that chiropractic is a religion?
Well, not quite but almost.
DD Palmer seriously toyed with the idea of turning chiropractic into a religion.
And rightly so!
In the absence of evidence, belief is everything.
And this is why, to this day, so many chiropractors bank (a most appropriate term in this context!) on belief rather than evidence.
Look, for instance at this lovely advertisement I found on Twitter (there are many more, but this one has to stand for the many).
Seven common benefits of chiropractic care!?!
Beneath the picture of a pathologically straight spine – if that is what chiro does to you, avoid it at all cost! – we see the name of the ‘doctor’ who seems to have designed this impressive picture. ‘Dr’ Schluter is even more versatile than his pretty advertisement implies; he also seems to treat newborn babies! And on his website he also tells us that he is able to treat allergies:
You may be surprised to find that chiropractic can do a great deal to alleviate some allergies. Allergies are very common and we become so used to their effect on us that we tend to ignore their symptoms. And many people are unaware of the gradual decline in health that results. Chiropractic treatment didn’t necessarily set out specifically to provide care for allergies, but due to the nature of the chiropractic care and its effect on the nervous system, it has been shown to help.
If we look at some of the common signs of allergies we find that they include some unexpected examples. Not only do we find the usual ones – asthma, sinus congestion, sneezing, itchy eyes, skin rashes and running nose – but also weight gain, Acne and even fluid retention and heartburn.
Many people approach the problem of allergies as though all allergens affect everyone in the same way; this is not the case. Because we are individuals, different allergens affect each of us in differing ways. Some allergens affect some and not others. Consequently treating the condition must be approached on this basis of individuality.
It may not be the pet fur or dried saliva that is kicked up as your pooch washes and scratches; it may also not be the pollen, grass dust or other one of the many irritants in the air at any one time. It could be that due to a misalignment of the spine (or subluxation), mild though it may be, the nervous system is finding it difficult to help the body adapt to its surroundings and is therefore unable to deal with the necessary adjustments.
As an individual you need to treat your body’s physical and nervous system as such. You could be, without even being aware of it, in a generally stressed condition – this may be through lack of sleep, poor nutrition or any one of a combination of the many other stressors affecting us daily. Suddenly you find that with the first spring pollen dust that comes along you begin to wheeze and sneeze!
You may not have previously connected chiropractors and allergies but, for you or someone you know, the connection could help.
Schluter Chiropractic works on the principle of reducing interference so the nervous system and body can work better. Providing that any symptom or condition (including pain) is occurring as a result of nerve interference from vertebral subluxation, there is a very good chance that it will improve with chiropractic care.
END OF QUOTE
Wise words indeed.
Like most chiros, ‘Dr’ Schulter seems to be a true miracle-worker; and because he can do miracles, he does not need to be rational or concerned about evidence or worried about telling the truth.
For Christ sake, it’s Easter!
We ought to show a bit of belief!!!
Why?
Because without it, the benefits of chiropractic would be just an illusion.
Chiropractors are fast giving up the vitalistic and obsolete concepts of their founding fathers, we are told over and over again. But are these affirmations true? There are good reasons to be sceptical. Take this recent paper, for instance.
The objective of this survey was to investigate the proportion of Australian chiropractic students who hold non-evidence-based beliefs in the first year of study and to determine the extent to which they may be involved in non-musculoskeletal health conditions.
Students from two Australian chiropractic programs were invited to answer a questionnaire on how often they would give advice on 5 common health conditions in their future practices, as well as to provide their opinion on whether chiropractic spinal adjustments could prevent or help seven health-related conditions.
The response rate of this survey was 53%. Students were highly likely to offer advice on a range of non-musculoskeletal conditions. The proportions were lowest in first year and highest the final year. For instance, 64% of students in year 4/5 believed that spinal adjustments improve the health of infants. Also, high numbers of students held non-evidence-based beliefs about ‘chiropractic spinal adjustments’ which tended to occur in gradually decreasing in numbers in sequential years, except for 5th and final year, when a reversal of the pattern occurred.
The authors concluded that new strategies are required for chiropractic educators if they are to produce graduates who understand and deliver evidence-based health care and able to be part of the mainstream health care system.
This is an interesting survey, but I think its conclusion is wrong!
- Educators do not require ‘new strategies’, I would argue; they simply need to take their duty of educating students seriously – educating in this context does not mean brain-washing, it means teaching facts and evidence-based practice. And this is were any concept of true education would run into problems: it would teach students that chiropractic is built on sand.
- Conclusions need to be based on the data presented. Therefore, the most fitting conclusion, in my view, is that chiropractic students are currently being educated such that, once let loose on the unsuspecting and often all too gullible public, they will be a menace and a serious danger to public health.
You might say that this survey is from Australia and that the findings therefore do not necessarily apply to other countries. Correct! However, I very much fear that elsewhere the situation is similar or perhaps even worse. And my fear does not come out of thin air, it is based on things we have discussed before; see for instance these three posts:
Chiropractic education seems to be a form of religious indoctrination
What are the competencies of a ‘certified paediatric doctor of chiropractic’?
But I would be more than willing to change my mind – provided someone can show me good evidence to the contrary.
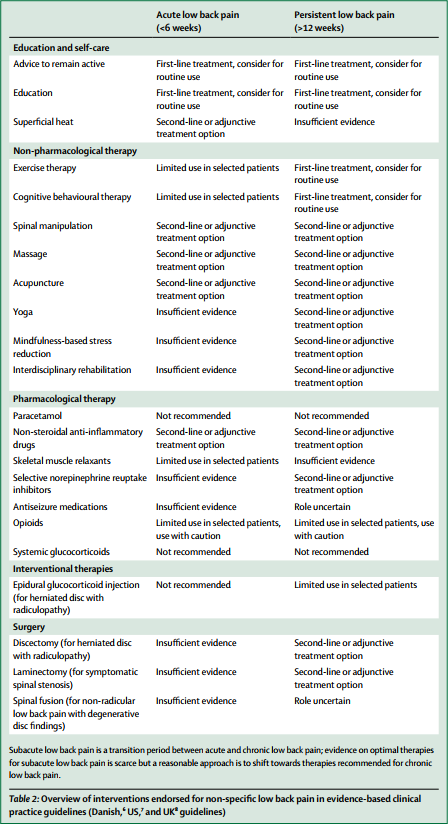
The media have (rightly) paid much attention to the three Lancet-articles on low back pain (LBP) which were published this week. LBP is such a common condition that its prevalence alone renders it an important subject for us all. One of the three papers covers the treatment and prevention of LBP. Specifically, it lists various therapies according to their effectiveness for both acute and persistent LBP. The authors of the article base their judgements mainly on published guidelines from Denmark, UK and the US; as these guidelines differ, they attempt a synthesis of the three.
Several alternative therapist organisations and individuals have consequently jumped on the LBP bandwagon and seem to feel encouraged by the attention given to the Lancet-papers to promote their treatments. Others have claimed that my often critical verdicts of alternative therapies for LBP are out of line with this evidence and asked ‘who should we believe the international team of experts writing in one of the best medical journals, or Edzard Ernst writing on his blog?’ They are trying to create a division where none exists,
The thing is that I am broadly in agreement with the evidence presented in Lancet-paper! But I also know that things are a bit more complex.
Below, I have copied the non-pharmacological, non-operative treatments listed in the Lancet-paper together with the authors’ verdicts regarding their effectiveness for both acute and persistent LBP. I find no glaring contradictions with what I regard as the best current evidence and with my posts on the subject. But I feel compelled to point out that the Lancet-paper merely lists the effectiveness of several therapeutic options, and that the value of a treatment is not only determined by its effectiveness. Crucial further elements are a therapy’s cost and its risks, the latter of which also determines the most important criterion: the risk/benefit balance. In my version of the Lancet table, I have therefore added these three variables for non-pharmacological and non-surgical options:
| EFFECTIVENESS ACUTE LBP | EFFECTIVENESS PERSISTENT LBP | RISKS | COSTS | RISK/BENEFIT BALANCE | |
| Advice to stay active | +, routine | +, routine | None | Low | Positive |
| Education | +, routine | +, routine | None | Low | Positive |
| Superficial heat | +/- | Ie | Very minor | Low to medium | Positive (aLBP) |
| Exercise | Limited | +/-, routine | Very minor | Low | Positive (pLBP) |
| CBT | Limited | +/-, routine | None | Low to medium | Positive (pLBP) |
| Spinal manipulation | +/- | +/- | vfbmae sae |
High | Negative |
| Massage | +/- | +/- | Very minor | High | Positive |
| Acupuncture | +/- | +/- | sae | High | Questionable |
| Yoga | Ie | +/- | Minor | Medium | Questionable |
| Mindfulness | Ie | +/- | Minor | Medium | Questionable |
| Rehab | Ie | +/- | Minor | Medium to high | Questionable |
Routine = consider for routine use
+/- = second line or adjunctive treatment
Ie = insufficient evidence
Limited = limited use in selected patients
vfbmae = very frequent, minor adverse effects
sae = serious adverse effects, including deaths, are on record
aLBP = acute low back pain
The reason why my stance, as expressed on this blog and elsewhere, is often critical about certain alternative therapies is thus obvious and transparent. For none of them (except for massage) is the risk/benefit balance positive. And for spinal manipulation, it even turns out to be negative. It goes almost without saying that responsible advice must be to avoid treatments for which the benefits do not demonstrably outweigh the risks.
I imagine that chiropractors, osteopaths and acupuncturists will strongly disagree with my interpretation of the evidence (they might even feel that their cash-flow is endangered) – and I am looking forward to the discussions around their objections.
We all know that there is a plethora of interventions for and specialists in low back pain (chiropractors, osteopaths, massage therapists, physiotherapists etc., etc.); and, depending whether you are an optimist or a pessimist, each of these therapies is as good or as useless as the next. Today, a widely-publicised series of articles in the Lancet confirms that none of the current options is optimal:
Almost everyone will have low back pain at some point in their lives. It can affect anyone at any age, and it is increasing—disability due to back pain has risen by more than 50% since 1990. Low back pain is becoming more prevalent in low-income and middle-income countries (LMICs) much more rapidly than in high-income countries. The cause is not always clear, apart from in people with, for example, malignant disease, spinal malformations, or spinal injury. Treatment varies widely around the world, from bed rest, mainly in LMICs, to surgery and the use of dangerous drugs such as opioids, usually in high-income countries.
The Lancet publishes three papers on low back pain, by an international group of authors led by Prof Rachelle Buchbinder, Monash University, Melbourne, Australia, which address the issues around the disorder and call for worldwide recognition of the disability associated with the disorder and the removal of harmful practices. In the first paper, Jan Hartvigsen, Mark Hancock, and colleagues draw our attention to the complexity of the condition and the contributors to it, such as psychological, social, and biophysical factors, and especially to the problems faced by LMICs. In the second paper, Nadine Foster, Christopher Maher, and their colleagues outline recommendations for treatment and the scarcity of research into prevention of low back pain. The last paper is a call for action by Rachelle Buchbinder and her colleagues. They say that persistence of disability associated with low back pain needs to be recognised and that it cannot be separated from social and economic factors and personal and cultural beliefs about back pain.
Overview of interventions endorsed for non-specific low back pain in evidence-based clinical practice guidelines (Danish, US, and UK guidelines)
In this situation, it makes sense, I think, to opt for a treatment (amongst similarly effective/ineffective therapies) that is at least safe, cheap and readily available. This automatically rules out chiropractic, osteopathy and many others. Exercise, however, does come to mind – but what type of exercise?
The aim of this meta-analysis of randomized controlled trials was to gain insight into the effectiveness of walking intervention on pain, disability, and quality of life in patients with chronic low back pain (LBP) at post intervention and follow ups.
Six electronic databases (PubMed, Science Direct, Web of Science, Scopus, PEDro and The Cochrane library) were searched from 1980 to October 2017. Randomized controlled trials (RCTs) in patients with chronic LBP were included, if they compared the effects of walking intervention to non-pharmacological interventions. Pain, disability, and quality of life were the primary health outcomes.
Nine RCTs were suitable for meta-analysis. Data was analysed according to the duration of follow-up (short-term, < 3 months; intermediate-term, between 3 and 12 months; long-term, > 12 months). Low- to moderate-quality evidence suggests that walking intervention in patients with chronic LBP was as effective as other non-pharmacological interventions on pain and disability reduction in both short- and intermediate-term follow ups.
The authors concluded that, unless supplementary high-quality studies provide different evidence, walking, which is easy to perform and highly accessible, can be recommended in the management of chronic LBP to reduce pain and disability.
I know – this will hardly please the legions of therapists who earn their daily bread with pretending their therapy is the best for LBP. But healthcare is clearly not about the welfare of the therapists, it is/should be about patients. And patients should surely welcome this evidence. I know, walking is not always easy for people with severe LBP, but it seems effective and it is safe, free and available to everyone.
My advice to patients is therefore to walk (slowly and cautiously) to the office of their preferred therapist, have a little rest there (say hello to the staff perhaps) and then walk straight back home.
On this blog, we had many chiropractors commenting that their profession is changing fast and the old ‘philosophy’ is a thing of the past. But are these assertions really true? This survey might provide an answer. A questionnaire was sent to chiropractic students in all chiropractic programs in Australia and New Zealand. It explored student viewpoints about the identity, role/scope, setting, and future of chiropractic practice as it relates to chiropractic education and health promotion. Associations between the number of years in the program, highest degree preceding chiropractic education, institution, and opinion summary scores were evaluated by multivariate analysis of variance tests.
A total of 347 chiropractic students participated. For identity, most students (51.3%) hold strongly to the traditional chiropractic theory but also agree (94.5%) it is important that chiropractors are educated in evidence-based practice. The main predictor of student viewpoints was a student’s chiropractic institution. Chiropractic institution explained over 50% of the variance around student opinions about role/scope of practice and approximately 25% for identity and future practice.
The authors concluded that chiropractic students in Australia and New Zealand seem to hold both traditional and mainstream viewpoints toward chiropractic practice. However, students from different chiropractic institutions have divergent opinions about the identity, role, setting, and future of chiropractic practice, which is most strongly predicted by the institution. Chiropractic education may be a potential determinant of chiropractic professional identity, raising concerns about heterogeneity between chiropractic schools.
Traditional chiropractic theory is, of course, all the palmereque nonsense about ‘95% of all diseases are caused by subluxations of the spine’ etc. And evidence-based practice means knowing that subluxations are a figment of the chiropractic imagination.
Imagine a physician who believes in evidence and, at the same time, in the theory of the 4 humours determining our health.
Imagine a geologist thinking that the earth is flat and also spherical.
Imagine a biologist subscribing to both creationism and evolution.
Imagine a surgeon earning his livelihood with blood-letting and key-hole surgery.
Imagine a doctor believing in vital energy after having been taught physiology.
Imagine an airline pilot considering the use of flying carpets.
Imagine a chemist engaging in alchemy.
Imagine a Brexiteer who is convinced of doing the best for the UK.
Imagine a homeopath who thinks he practices evidence-based medicine.
Imagine a plumber with a divining rod.
Imagine an expert in infectious diseases believing is the miasma theory.
Imagine a psychic hoping to use her skills for winning a fortune on the stock market.
————————————————————————————————————————————-
Once you have imagined all of these situations, I fear, you might know (almost) all worth knowing about chiropractic.
Dr. Dietmar Payrhuber is not famous – no, by no means. I had never heard of him until a watched this TV discussion about homeopathy (it’s in German, and well-worth watching, if you understand the language). I found the discussion totally mesmerising: Payrhuber is allowed to come out with case after case alleging he cured cancer of various types with homeopathy. Prof Frass is also there to defend the indefensible, but hardly intervenes, other than repeatedly and pompously stating that he is a professor with 200 publications who runs a homeopathy clinic at the university hospital of Vienna and therefore he is a cut above.
There are also three very bright and eloquent sceptical disputants who do their best to oppose Payrhuber’s moronic monstrosities. One of them even alerts us (and the broadcaster!) to the fact that some cancer patients might watch this and conclude that homeopathy cues cancer. Yes, TV can be dangerous!
After watching Payrhuber, I felt the urge to learn more about this man. On TV, he mentioned repeatedly his publications, so I first of all conducted a Medline search; it turns out that Medline lists not a single article in his name. However, I did find his (self-published) book: ‘HOMOEOPATHIE UND KREBS’ (HOMEOPATHY AND CANCER). It greatly impressed me – but not in a positive sense.
The preface (in English) is by Jan Scholten (who IS quite famous in the realm of homeopathy); here is a short quote from it:
[Payrhuber’s book] … is an important book for several reasons. The first reason is that it shows that homeopathy is a real healing art. Often homeopathy is seen as good for superficial, light and self-healing diseases such as colds, eczema’s, bronchitis and the like. Together with this view goes the opinion that it is not a real medicine, because it cannot treat „real diseases“. But this shows the opposite: cancer can be healed, cured with homeopathy. It shows that homeopathy can have very profound effect and can really cure deeply. Of course cancer was cured already in the past with homeopathy by famous homeopaths such as Grimmer and Resch. But Dietmar shows that it can be done in a consistent way. Homeopathy cannot be set aside as superficial anymore…But it gets worse! Payrhuber himself is equally clear that homeopathy can cure cancer; here is a quote that I translated from his German text into English:
The book shows options to treat cancer; this is not an exclusive option of homeopathy. However, it offers an alternative for therapy-resistant and slow-responding cases treated conventionally… The question whether homeopathy is an alternative or a complementary therapy is superfluous. As the cases presented here demonstrate, homeopathy is part of medicine, a method which is more scientific than conventional medicine, because it has clear principles and laws. In certain cases or in certain phases of cancer, homeopathy is quite simply indicated! Homeopathy is holistic and puts the whole patient rather than a local symptom in the centre.
We must not keep homeopathy from cancer patients, because it offers in many cases a cure which cannot be achieved by other means.
(For those who can read German, here is the original: Das Buch zeigt Möglichkeiten auf, Krebs zu behandeln, es stellt keinen Alleinanspruch der Homöopathie dar. Es bietet allerdings alternative Möglichkeiten für therapieresistente und therapieträge Behandlungsverläufe bei konventioneller Therapie an….
Es erübrigt sich die Frage, ob Homöopathie eine alternative oder komplementäre Medizin ist. Wie die vorliegenden Fälle zeigen, ist sie ein Teil der Medizin, eine Methode, die „eher wissenschaftlicher ist als die Schulmedizin, weil die Homöopathie deutliche Prinzipien und Gesetze hat“. Die Homöopathie ist in bestimmten Fällen oder in bestimmten Phasen der Behandlung schlicht und einfach indiziert! Sie ist ganzheitlich, setzt den Menschen ins Zentrum und nicht das Lokalsymptom…
Die Homöopathie darf dem Patienten nicht vorenthalten werden, da sie in vielen Fällen Heilungsmöglichkeiten bietet, die auf andere Weise nicht erreicht werden können…)
END OF QUOTE
As I said, Payrhuber is not famous – he is infamous!
This sad story left me with three questions:
- Can someone please stop Payrhuber before he does more damage to cancer patients?
- And can someone please tell the medical faculty of the university of Vienna (my former employer) that running a homeopathy clinic for cancer patients is not ethical?
- Can someone please teach journalists that, in healthcare, giving a voice to dangerous nonsense can do serious harm?