Monthly Archives: November 2019
I have reported previously about the tragic death of John Lawler. Now after the inquest into the events leading to it has concluded, I have the permission to publish the statement of Mr Lawler’s family:
We were devastated to lose John in such tragic and unforeseen circumstances two years ago. A much-loved husband, father and grandfather, he continues to be greatly missed by all of us. Having to re-live the circumstances of his death has been particularly difficult for us but we are grateful to have a clearer picture of the events that led to John’s death. We would like to take this opportunity to thank the coroner’s team, our legal representatives and our wider family and friends for their guidance, empathy and sensitivity throughout this process.
There were several events that went very wrong with John’s chiropractic treatment, before, during, and after the actual manipulation that broke his neck.
Firstly, John thought he was being treated by a medically qualified doctor, when he was not. Furthermore, he had not given informed consent to this treatment.
The chiropractor diagnosed so-called ‘vertebral subluxation complex’ which she aimed to treat by manipulating his neck. We heard this week from medical experts that John had ossified ligaments in his spine, where previously flexible ligaments had turned to bone and become rigid. This condition is not uncommon, and is present in about 10% of those over 50. It would have showed on an X-ray or other imaging technique. The chiropractor did not ask for any images before commencing treatment and was seemingly unaware of the risks of doing a manual manipulation on an elderly patient.
It has become clear that the chiropractor did the manipulation incorrectly, and broke these rigid ligaments during a so-called ‘drop table’ manipulation, causing discs in the cervical spine to rupture and the spinal cord to become crushed. Although these manipulations are done frequently by chiropractors, we have heard that the force applied to his neck by the chiropractor would have had to have been “significant”.
Immediately John reported loss of sensation and paralysis in his arms. At this stage the only safe and appropriate response was to leave him on the treatment bed and await the arrival of the paramedics, and provide an accurate history to the ambulance controller and paramedics. The chiropractor, in fact, manhandled John from the treatment bed into a chair; then tipped his head backwards and gave “mouth to mouth” breaths. She provided an inaccurate and misleading history to the paramedic and ambulance controller, causing the paramedic to treat the incident as “medical” not “traumatic” and to transport John downstairs to the ambulance without stabilising his neck. If the paramedics had been given the full and accurate story, they would have stabilised his neck in situ and transported him on a scoop stretcher – and he would have subsequently survived.
The General Chiropractic Council decided not to suspend the chiropractor from practicing in September 2017. They heard evidence from the chiropractor that she had “not touched the neck during the appointment” and from an expert chiropractor that it would be “physically impossible” for the treatment provided to cause the injury which followed. We have heard this week that this is incorrect. The family was not allowed to attend or give evidence at that hearing, and we are waiting – now 2 years further on – for the GCC to complete their investigations.
We hope that the publicity surrounding this event will highlight the dangers of chiropractic, especially in the elderly and those with already compromised spines. We would again urge the regulator to take immediate measures to ensure that the profession is properly controlled: that chiropractors are prevented from styling themselves as medical professionals; that patients are fully informed and consent to the risks involved; that imaging is done before certain procedures and on high risk clients; and that the limits of the benefits chiropractic can provide are fully explored.
___________________________________________________________________
Before someone comments pointing out that this is merely a single case which does not amount to evidence, let me remind you of the review of cervical manipulation prepared for the Manitoba Health Professions Advisory Council. Here is the abstract:
Neck manipulation or adjustment is a manual treatment where a vertebral joint in the cervical spine—comprised of the 7 vertebrae C1 to C7—is moved by using high-velocity, low-amplitude (HVLA) thrusts that cannot be resisted by the patient. These HVLA thrusts are applied over an individual, restricted joint beyond its physiological limit of motion but within its anatomical limit. The goal of neck manipulation, referred to throughout this report as cervical spine manipulation (CSM), is to restore optimal motion, function, and/or reduce pain. CSM is occasionally utilized by physiotherapists, massage therapists, naturopaths, osteopaths, and physicians, and is the hallmark treatment of chiropractors; however the use of CSM is controversial. This paper aims to thoroughly synthesize evidence from the academic literature regarding the potential risks and benefits of cervical spine manipulation utilizing a rapid literature review method.
METHODS Individual peer-reviewed articles published between January 1990 and November 2016 concerning the safety and efficacy of cervical spine manipulation were identified through MEDLINE (PubMed), EMBASE, and the Cochrane Library.
KEY FINDINGS
- A total of 159 references were identified and cited in this review: 86 case reports/ case series, 37 reviews of the literature, 9 randomized controlled trials, 6 surveys/qualitative studies, 5 case-control studies, 2 retrospective studies, 2 prospective studies and 12 others.
- Serious adverse events following CSM seem to be rare, whereas minor adverse events occur frequently.
- Minor adverse events can include transient neurological symptoms, increased neck pain or stiffness, headache, tiredness and fatigue, dizziness or imbalance, extremity weakness, ringing in the ears, depression or anxiety, nausea or vomiting, blurred or impaired vision, and confusion or disorientation.
- Serious adverse events following CSM can include the following: cerebrovascular injury such as cervical artery dissection, ischemic stroke, or transient ischemic attacks; neurological injury such as damage to nerves or spinal cord (including the dura mater); and musculoskeletal injury including injury to cervical vertebral discs (including herniation, protrusion, or prolapse), vertebrae fracture or subluxation (dislocation), spinal edema, or issues with the paravertebral muscles.
- Rates of incidence of all serious adverse events following CSM range from 1 in 10,000 to 1 in several million cervical spine manipulations, however the literature generally agrees that serious adverse events are likely underreported.
- The best available estimate of incidence of vertebral artery dissection of occlusion attributable to CSM is approximately 1.3 cases for every 100,000 persons <45 years of age receiving CSM within 1 week of manipulative therapy. The current best incidence estimate for vertebral dissection-caused stroke associated with CSM is 0.97 residents per 100,000.
- While CSM is used by manual therapists for a large variety of indications including neck, upper back, and shoulder/arm pain, as well as headaches, the evidence seems to support CSM as a treatment of headache and neck pain only. However, whether CSM provides more benefit than spinal mobilization is still contentious.
- A number of factors may make certain types of patients at higher risk for experiencing an adverse cerebrovascular event after CSM, including vertebral artery abnormalities or insufficiency, atherosclerotic or other vascular disease, hypertension, connective tissue disorders, receiving multiple manipulations in the last 4 weeks, receiving a first CSM treatment, visiting a primary care physician, and younger age. Patients whom have experience prior cervical trauma or neck pain may be at particularly higher risk of experiencing an adverse cerebrovascular event after CSM.
CONCLUSION The current debate around CSM is notably polarized. Many authors stated that the risk of CSM does not outweigh the benefit, while others maintained that CSM is safe—especially in comparison to conventional treatments—and effective for treating certain conditions, particularly neck pain and headache. Because the current state of the literature may not yet be robust enough to inform definitive prohibitory or permissive policies around the application of CSM, an interim approach that balances both perspectives may involve the implementation of a harm-reduction strategy to mitigate potential harms of CSM until the evidence is more concrete. As noted by authors in the literature, approaches might include ensuring manual therapists are providing informed consent before treatment; that patients are provided with resources to aid in early recognition of a serious adverse event; and that regulatory bodies ensure the establishment of consistent definitions of adverse events for effective reporting and surveillance, institute rigorous protocol for identifying high-risk patients, and create detailed guidelines for appropriate application and contraindications of CSM. Most authors indicated that manipulation of the upper cervical spine should be reserved for carefully selected musculoskeletal conditions and that CSM should not be utilized in circumstances where there has not yet been sufficient evidence to establish benefit.
___________________________________________________________________
Just three points which, in my view, sand out most in relation to Mr Lawler’s death:
- Mr Lawler had no proven indication (and at least one very important contra-indication) for neck manipulation.
- He did not give infromed consent.
- The neck manipulation was not within the limits of the physiological range of motion.
An intercessory prayer (IP) is an intervention characterized by one or more individuals praying for the well-being or a positive outcome of another person. There have been several trials of IP, but the evidence is far from clear-cut. Perhaps this new study will bring clarity?
The goal of this double-blind RCT was to assess the effects of intercessory prayer on psychological, spiritual and biological scores of breast 31 cancer patients who were undergoing radiotherapy (RT). The experimental group was prayed for, while the controla group received no such treatment. The intercessory prayer was performed by a group of six Christians, who prayed daily during 1 h while participant where under RT. The prayers asked for calm, peace, harmony and recovery of health and spiritual well-being of all participants. Data collection was performed in three time points (T0, T1 and T2).
Significant changes were noted in the intra-group analysis, concerning the decrease in spiritual distress score; negative religious/spiritual coping prevailed, while the total religious/spiritual coping increased between the posttest T2 to T0.
The authors concluded that begging a higher being for health recovery is a common practice among people, regardless of their spirituality and religiosity. In this study, this practice was performed through intercessory prayer, which promoted positive health effects, since spiritual distress and negative spiritual coping have reduced. Also, spiritual coping has increased, which means that participants facing difficult situations developed strategies to better cope and solve the problems. Given the results related to the use of intercession prayer, as a complementary therapeutic intervention, holistic nursing care should integrate this intervention, which is included in the Nursing Interventions Classification. Additionally, further evidence and research is needed about the effect of this nursing spiritual intervention in other cultures, in different clinical settings and with larger samples.
The write-up of this study is very poor and most confusing – so much so that I find it hard to make sense of the data provided. If I understand it correctly, the positive findings relate to changes within the experimental group. As RCTs are about compating one group to another, these changes are irrelevant. Therefore (and for several other methodological flaws as well), the conclusion that IP generates positive effects is not warranted by these new findings.
Like all other forms of paranormal healing, IP is implausible and lacks support of clinical effectiveness.
The tragic case of John Lawler who died after being treated by a chiropractor has been discussed on this blog before. Naturally, it generated much discussion which, however, left many questions unanswered. Today, I am able to answer some of them.
- Mr Lawler died because of a tear and dislocation of the C4/C5 intervertebral disc caused by considerable external force.
- The pathologist’s report also shows that the deceased’s ligaments holding the vertebrae of the upper spine in place were ossified.
- This is a common abnormality in elderly patients and limits the range of movement of the neck.
- There was no adequately informed consent by Mr Lawler.
- Mr Lawler seemed to have been under the impression that the chiropractor, who used the ‘Dr’ title, was a medical doctor.
- There is no reason to assume that the treatment of Mr Lawler’s neck would be effective for his pain located in his leg.
- The chiropractor used an ‘activator’ which applies only little and well-controlled force. However, she also employed a ‘drop table’ which applies a larger and not well-controlled force.
I have the permission to publish the submissions made to the coroner by the barrister representing the family of Mr Lawler. The barrister’s evidence shows that:
- Chiropractors are not medical doctors and should make this perfectly clear to all of their patients.
- Elderly patients can have several contra-indications to spinal manipulations. They should therefore think twice before consulting a chiropractor.
- A limited range of spinal movement usually is the sign for a chiropractor to intervene. However, this may lead to dramatically bad consequences, if the patient’s para-vertebral ligaments are ossified which happens in about 10% of all elderly individuals.
- Chiropractors are by no means exempt from obtaining informed consent. (In the case of Mr Lawler, this would have had to include the information that the neck manipulation carries serious risks and has not shown to work for any type of pain in the leg and might have saved his life, as he then might have refused to accept the treatment.)
- Chiropractors are not trained to deal with medical emergencies and must leave that to those healthcare professionals who are fully trained.
It has been reported that pharmacies in New Zealand continue to ignore a code of ethics that requires them to inform customers, if a product has no evidence of efficacy. The code of ethics states: “Pharmacists must advise patients when scientific support for treatment is lacking.”
Eight Auckland pharmacies were visited to enquire about a homeopathic product for sale. Pharmacy staff were asked what they knew about a homeopathic product on their shelves and if it worked. All failed to share information about the lack of scientific evidence showing the product works. Instead, they claimed that homeopathic solution of arnica sold as a treatment for injuries, bruising and post-surgery trauma “works really, really well”, was “awesome” and could also cure headaches. One salesperson checked with the pharmacist whether the product was suitable for swelling post-surgery and was told it was fine as long as no other medication was being taken at the same time.
There is no credible evidence the highly diluted homeopathic remedies sold by pharmacists work better than a placebo. Homeopathy’s effectiveness has been rejected by many scientists and by large government reviews conducted in the UK, Australia and Europe.
Even if a staff member personally believes a homeopathic product works, guidelines referenced by the code of ethics say this should not sway the information given to the customer: “Patients must be made aware of the likely effectiveness of a given therapy according to recognised peer-reviewed medical publications, in spite of your personal beliefs.”
Shortly after the code was changed in March 2018, Newsroom performed the same secret shopper experiment at four pharmacies and found the new rule was not followed. Eighteen months on, nothing has improved.
The chair of the consumer advocate group the ‘Society for Science Based Healthcare’, Mark Hanna, said there was no excuse for pharmacies to sell this kind of thing without warning. “Pharmacists should know better. Full stop. They should not be misleading their patients, they should not be letting their staff mislead their patients. If they don’t know, that’s incompetence. I would expect to be given reasonable, evidence-based advice, possibly some different options with the reason why I might choose one over the other. I wouldn’t expect to be misled and sold something that wouldn’t work.
Asked why the code was not being followed a spokesperson of the NZ pharmacists said a reminder of the code of ethics had been sent to pharmacies in June. It was recommended all staff be made aware of the code: “We encourage you to share this protocol with your entire team – even though it is a protocol for pharmacists, the reasoning also extends to other staff members in the pharmacy and it is important that all staff ensure that the patient has been provided with sufficient information to make an informed choice.”
By Jove, we have discussed this issue often enough. If you are interested, here are a few of my more recent posts on this subject:
- “Pharmacists should not sell or dispense homeopathic products”
- German pharmacists fail their customers when advising them on homeopathy
- Pharmacists put themselves at risk by selling homeopathic remedies
- Pro and Contra: should UK community pharmacists sell homeopathic remedies?
- Pharmacists’ responsibilities vis a vis alternative medicine: the violation of healthcare ethics continues.
- It is “disappointing that some pharmacists are still stocking homeopathy products”
- Pharmacists: to sell quackery means you are quacks – or have I got that wrong?
- Pharmacists must use their professional judgement to prevent the supply of homeopathic remedies
But pharmacists seem utterly reluctant to change – in NZ or elsewhere. Why? Could it have something to do with money?
If doctors violate their code of ethics, they face being reprimanded by their professional body. It is high time that the same happens with pharmacists, I feel.
I almost forgot!
This would have been no good, after all, Charles has for decades been the most influential supporter of so-called alternative medicine (SCAM) in the UK. He is one of SCAM’s greatest proponent.
So, here is my up-dated, extended and illustrated summary of his achievements in this area.
HAPPY BIRTHDAY CHARLES!
Charles went on a journey of ‘spiritual discovery’ into the wilderness of northern Kenya. His guru and guide at the time was Laurens van der Post (later discovered to be a fraud and compulsive fantasist and to have fathered a child with a 14-year old girl entrusted to him during a sea voyage).
 Van der Post wanted to awake Charles’ mind and attune it to the vitalistic ideas of Carl Jung’s ‘collective unconscious’, and it is this belief in vitalism that provides the crucial link to alternative medicine: virtually every form of alternative therapies is based on the assumption that some sort of vital force exists. Charles was so taken by van der Post that he made him the godfather of Prince William. After Post’s death, he established an annual lecture in his honour (the lecture series was discontinued after Van der Post was discovered to be a fraud).
Van der Post wanted to awake Charles’ mind and attune it to the vitalistic ideas of Carl Jung’s ‘collective unconscious’, and it is this belief in vitalism that provides the crucial link to alternative medicine: virtually every form of alternative therapies is based on the assumption that some sort of vital force exists. Charles was so taken by van der Post that he made him the godfather of Prince William. After Post’s death, he established an annual lecture in his honour (the lecture series was discontinued after Van der Post was discovered to be a fraud).

Some time in the 1970s, Charles met Jimmy Saville and befriended him. Apparently, Saville later advised Charles on several occasions in various health-related matters.

Throughout the 1980s, Charles lobbied for the statutory regulation of chiropractors and osteopaths in the UK. In 1993, this finally became reality. These two SCAM professions are to this day the only ones regulated by statute in the UK.
Osteopathy has strong Royal links: Prince Charles is the President of the GOsC; Princess Diana was the President of the GCRO; and Princess Anne is the patron of the British School of Osteopathy (statement dated 2011).
In 1982, Prince Charles was elected as President of the British Medical Association (BMA) and promptly challenged the medical orthodoxy by advocating alternative medicine. In a speech at his inaugural dinner as President, the Prince lectured the medics: ‘Through the centuries healing has been practised by folk healers who are guided by traditional wisdom which sees illness as a disorder of the whole person, involving not only the patient’s body, but his mind, his self-image, his dependence on the physical and social environment, as well as his relation to the cosmos.’ The BMA-officials ordered a full report on alternative medicine which promptly condemned this area as implausible nonsense.
Six years later, a second report, entitled Complementary Medicine – New Approaches to Good Practice, heralded an astonishing about-turn stating that: “the demand for non-conventional therapies had become so pressing that organised medicine in Britain could no longer ignore its contribution”. At the same time, however, the BMA set in motion a further chapter in the history of SCAM by insisting that it was “unacceptable” to allow the unrestricted practice of non-conventional therapies, irrespective of training or experience.
In 1993, Charles founded his lobby group which, after being re-named several times, ended up being called the ‘Foundation for Integrated Health’ (FIH). It was closed down in 2010 amidst allegations of money laundering and fraud. Its chief executive, George Gray, was later convicted and went to jail. The FIH had repeatedly been a little economical with the truth.
In 2000, Charles wrote an open letter to The Times stating that…It makes good sense to evaluate complementary and alternative therapies. For one thing, since an estimated £1.6 billion is spent each year on them, then we want value for our money. The very popularity of the non-conventional approaches suggests that people are either dissatisfied with their orthodox treatment, or they find genuine relief in such therapies. Whatever the case, if they are proved to work, they should be made more widely available on the NHS…But there remains the cry from the medical establishment of “where’s the proof?” — and clinical trials of the calibre that science demands cost money…The truth is that funding in the UK for research into complementary medicine is pitiful…So where can funding come from?…Figures from the department of complementary medicine at the University of Exeter show that less than 8p out of every £100 of NHS funds for medical research was spent on complementary medicine. In 1998-99 the Medical Research Council spent no money on it at all, and in 1999 only 0.05 per cent of the total research budget of UK medical charities went to this area…
In 2001, Charles worked on plans to help build a model hospital of integrated medicine. It was to train doctors to combine conventional medicine and alternative treatments, such as homeopathy, Ayurvedic medicine and acupuncture, and was to have up to 100 beds. The prince’s intervention marked the culmination of years of campaigning by him for the NHS to assign a greater role to alternative medicine. Teresa Hale, founder of the Hale Clinic in London, said: “Twenty-five years ago people said we were quacks. Now several branches, including homeopathy, acupuncture and osteopathy, have gained official recognition.” The proposed hospital, which was due to open in London in 2003/4, was to be overseen by Mosaraf Ali, who runs the Integrated Medical Centre (IMC) in London. But the hospital never materialised.
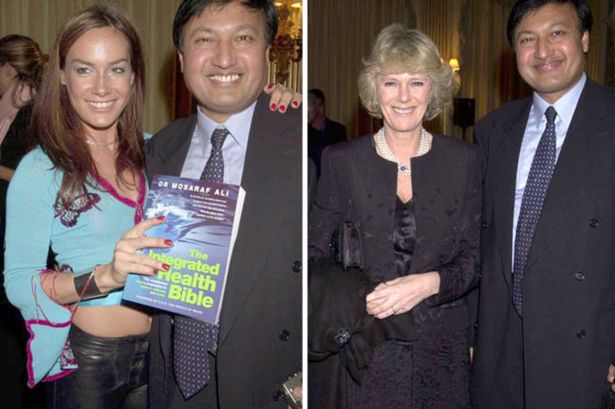
This might be due to Mosaraf Ali falling in disrepute: Raj Bathija, 69 and from India, went for a massage at the clinic of Dr Mosaraf Ali and his brother Imran in 2005 after suffering from two strokes. However, he claims that shortly after the treatment, his legs became pale and discoloured. Four days afterwards, Mr Bathija was admitted to hospital, where he had to have both legs amputated below the knee due to a shortage of blood. According to Mr Bathija, Dr Ali and his brother were negligent in that they failed to diagnose his condition and neglected to advise him to go to hospital. His daughter Shibani said: “My father was in a wheelchair but was making progress with his walking. He hoped he might become a bit more independent. With the amputations, that’s all gone.” Dr Ali was sued (if anyone knows the outcome of this case, please let me know).
At the age of 53, Mrs Parker Bowles went on a trek to the Himalayas to ‘re-energise’ her spirits and encourage her to give up smoking. She was in a party of 12 accompanied by the Prince of Wales’s favourite health guru, Dr Mosaraf Ali. Mrs Parker Bowles subsequently became a regular visitor to Dr Ali’s London practice where she has been encouraged to take up yoga both to combat her back pain and to help her give up smoking.
In the same year, Charles published an editorial in the BMJ promoting his ideas around integrative medicine. Its title: THE BEST OF BOTH WORLDS.
In 2003, Prince Charles’ FIH launched a five-year plan which outlined how to improve access to alternative therapies.
In 2004, Charles publicly supported the Gerson diet as a treatment for cancer and Prof Baum, an eminent oncologist, was invited to respond in an open letter to the British Medical Journal: …Over the past 20 years I have treated thousands of patients with cancer and lost some dear friends and relatives to this dreaded disease…The power of my authority comes with knowledge built on 40 years of study and 25 years of active involvement in cancer research. Your power and authority rest on an accident of birth. I don’t begrudge you that authority but I do beg you to exercise your power with extreme caution when advising patients with life-threatening diseases to embrace unproven therapies.
In 2005, the ‘Smallwood-Report’ was published; it had been commissioned by Charles and paid for by Dame Shirley Porter to inform health ministers. It stated that up to 480 million pounds could be saved, if one in 10 family doctors offered homeopathy as an “alternative” to standard drugs for asthma. Savings of up to 3.5 billion pounds could be achieved by offering spinal manipulation rather than drugs to people with back pain. Because I had commented on this report, Prince Charles’ first private secretary asked my vice chancellor to investigate my alleged indiscretion; even though I was found to be not guilty of any wrong-doing, all local support at Exeter stopped which eventually led to my early retirement. ITV later used this incident in a film entitled THE MEDDLING PRINCE, I later published a full account of this sad story in my memoir.
In a 2006 speech, Prince Charles told the World Health Organisation in Geneva that alternative medicine should have a more prominent place in health care and urged every country to come up with a plan to integrate conventional and alternative medicine into the mainstream. But British science struck back. Anticipating Prince Charles’s sermon in Geneva, 13 of Britain’s most eminent physicians and scientists wrote an “Open Letter” which expressed concern over “ways in which unproven or disproved treatments are being encouraged for general use in Britain’s National Health Service.” The signatories argued that “it would be highly irresponsible to embrace any medicine as though it were a matter of principle.”
In 2008, The Times published my letter asking the FIH to withdraw two guides promoting alternative medicine, stating: “the majority of alternative therapies appear to be clinically ineffective, and many are downright dangerous.” A speaker for the FIH countered the criticism by stating: “We entirely reject the accusation that our online publication Complementary Healthcare: A Guide contains any misleading or inaccurate claims about the benefits of complementary therapies. On the contrary, it treats people as adults and takes a responsible approach by encouraging people to look at reliable sources of information… so that they can make informed decisions. The foundation does not promote complementary therapies.”
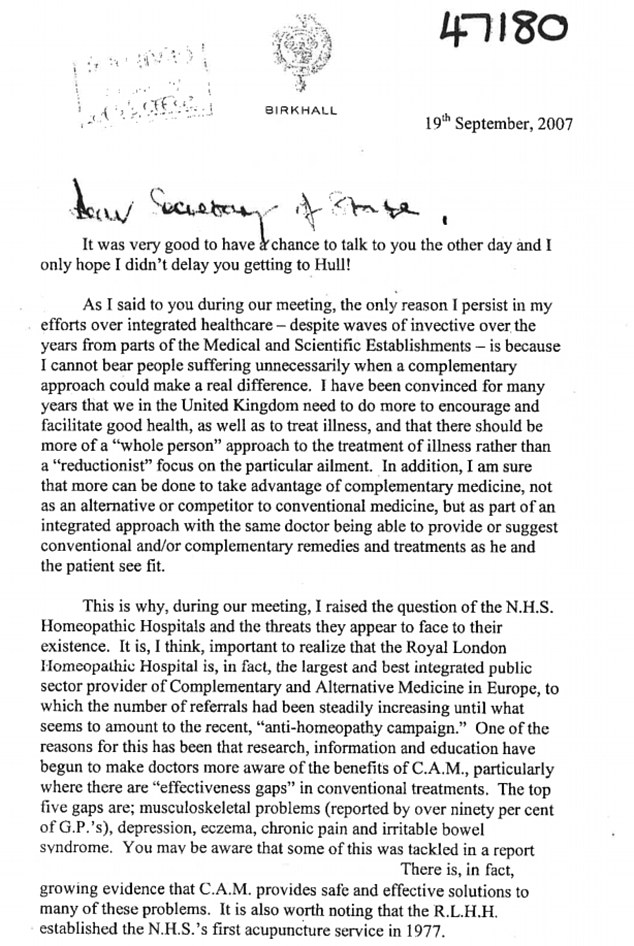
In 2009, the Prince held talks with the health Secretary to persuade him to introduce safeguards amid a crackdown by the EU that could prevent anyone who is not a registered health practitioner from selling remedies. This, it seems, was yet another example of Charles’ disregard of his constitutional role.
In the same year, Charles urged the government to protect alternative medicine because “we fear that we will see a black market in herbal products”, as Dr Michael Dixon (LVO,2015; OBE 2001), then medical director of Charles’ FIH, put it.
In 2009, the health secretary wrote to the prince suggesting a meeting on the possibility of a study on integrating complementary and conventional healthcare approaches in England. The prince had written to Burnham’s predecessor, Alan Johnson, to demand greater access to complementary therapies in the NHS alongside conventional medicine. The prince told him that “despite waves of invective over the years from parts of the medical and scientific establishment” he continued to lobby “because I cannot bear people suffering unnecessarily when a complementary approach could make a real difference”. He opposed “large and threatened cuts” in the funding of homeopathic hospitals and their possible closure. He complained that referrals to the Royal London homeopathic hospital were increasing “until what seems to amount to a recent ‘anti-homeopathic campaign’”. He warned against cuts despite “the fact that these homeopathic hospitals deal with many patients with real health problems who otherwise would require treatment elsewhere, often at greater expense”.
In 2009, it was announced that the ‘College of Integrated Medicine’ (the name was only later changed to ‘College of Medicine’, see below) was to have a second base in India. An Indian spokesman commented: “The second campus of the Royal College will be in Bangalore. We have already proposed the setting up of an All India Institute of Integrated Medicine to the Union health ministry. At a meeting in London last week with Prince Charles, we finalized the project which will kick off in July 2010”.
In 2010, Charles publicly stated that he was proud to be perceived as ‘an enemy of the enlightenment’.
In 2010, ‘Republic’ filed an official complaint about FIH alleging that its trustees allowed the foundation’s staff to pursue a public “vendetta” against a prominent critic of the prince’s support for complementary medicines. It also suggested that the imminent closure of Ernst’s department may be partly down to the charity’s official complaint about him after he publicly attacked its draft guide to complementary medicines as “outrageous and deeply flawed”.
In 2010, former fellows of Charles’ disgraced FIH launched a new organisation, The College of Medicine’ supporting the use of integrated treatments in the NHS. One director of the college is Michael Dixon, a GP in Cullompton, formerly medical director of the Foundation for Integrated Health. My own analysis of the activities of the new college leaves little doubt that it is promoting quackery.
In 2010, Charles published his book HARMONY which is full of praise for even the most absurd forms of alternative therapies and even bogus diagnostic tests used by alternative practitioners.

In 2011, after the launch of Charles’ range of herbal tinctures, I had the audacity to publicly criticise Charles for selling the Duchy Herbals detox tincture which I named ‘Dodgy Originals Detox Tincture’.

In 2011, Charles forged a link between ‘The College of Medicine’ and an Indian holistic health centre (see also above). The collaboration was reported to include clinical training to European and Western doctors in ayurveda and homoeopathy and traditional forms of medicine to integrate them in their practice. The foundation stone for the extended campus of the Royal College known as the International Institution for Holistic and Integrated Medicine was laid by Dr Michael Dixon in collaboration with the Royal College of Medicine.
In 2012, Charles was nominated for ‘THE GOLDEN DUCK AWARD’ for his achievements in promoting quackery. However, Andrew Wakefield beat him to it; Charles certainly was a deserving runner-up.
In 2013, Charles called for society to embrace a broader and more complex concept of health. In his article he described a vision of health that includes the physical and social environment, education, agriculture and architecture.
In 2013, Charles’ Highgrove enterprise offered ‘baby-hampers’ for sale at £195 a piece and made a range of medicinal claims for the products it contained. As these claims were not supported by evidence, there is no way to classify them other than quackery.
By 2013, the ‘Association of Osteomyologists’ were seeking to become regulated by statute, with the help of Prince Charles as their patron. The chairman and founder of this organisation was knighted for services to alternative medicine. Osteomyologists encourage the use of techniques including cranio-sacral therapy and claim that “we all know that Colleges, Institutions, and Medical Practitioners, are brain washed from the very outset into believing that their discipline is the only way to go.”
In November 2013, Charles invited alternative medicine proponents from across the world, including Dean Ornish, Michael Dixon, chair of College of Medicine, UK and Issac Mathai of Soukya Foundation, Bangalore, to India for a ‘brain storm’ and a subsequent conference on alternative medicine. The prince wanted the experts to collaborate and explore the possibilities of integrating different systems of medicines and to better the healthcare delivery globally, one of the organisers said.

In June 2014, BBC NEWS published the following text about a BBC4 broadcast entitled ‘THE ROYAL ACTIVIST’ aired on the same day: Prince Charles has been a well-known supporter of complementary medicine. According to a… former Labour cabinet minister, Peter Hain, it was a topic they shared an interest in. He had been constantly frustrated at his inability to persuade any health ministers anywhere that that was a good idea, and so he, as he once described it to me, found me unique from this point of view, in being somebody that actually agreed with him on this, and might want to deliver it. Mr Hain added: “When I was Secretary of State for Northern Ireland in 2005-7, he was delighted when I told him that since I was running the place I could more or less do what I wanted to do.*** I was able to introduce a trial for complementary medicine on the NHS, and it had spectacularly good results, that people’s well-being and health was vastly improved. And when he learnt about this he was really enthusiastic and tried to persuade the Welsh government to do the same thing and the government in Whitehall to do the same thing for England, but not successfully,” added Mr Hain. On this blog, I have pointed out that the research in question was fatally flawed and that Charles, once again, overstepped the boundaries of his constitutional role.
In 2015, two books were published which are relevant in this context. My memoir A SCIENTIST IN WONDERLAND recounts most of my dealings with Charles and his sycophants, including how an intervention from his first private secretary eventually led to the closure of my department. The book by Catherine Meyer CHARLES, THE HEART OF A KING is far less critical about our heir to the throne; it nevertheless severely criticises his stance on alternative medicine.
In October 2015, the Guardian obtained the infamous “black spider memos” which revealed that Charles had repeatedly lobbied politicians in favour of alternative medicine (see also above).
 In 2016, speaking at a global leaders summit on antimicrobial resistance, Prince Charles warned that Britain faced a “potentially disastrous scenario” because of the “overuse and abuse” of antibiotics. The Prince explained that he had switched to organic farming on his estates because of the growing threat from antibiotic resistance and now treats his cattle with homeopathic remedies rather than conventional medication. “As some of you may be aware, this issue has been a long-standing and acute concern to me,” he told delegates from 20 countries “I have enormous sympathy for those engaged in the vital task of ensuring that, as the world population continues to increase unsustainably and travel becomes easier, antibiotics retain their availability to overcome disease… It must be incredibly frustrating to witness the fact that antibiotics have too often simply acted as a substitute for basic hygiene, or as it would seem, a way of placating a patient who has a viral infection or who actually needs little more than patience to allow a minor bacterial infection to resolve itself.”
In 2016, speaking at a global leaders summit on antimicrobial resistance, Prince Charles warned that Britain faced a “potentially disastrous scenario” because of the “overuse and abuse” of antibiotics. The Prince explained that he had switched to organic farming on his estates because of the growing threat from antibiotic resistance and now treats his cattle with homeopathic remedies rather than conventional medication. “As some of you may be aware, this issue has been a long-standing and acute concern to me,” he told delegates from 20 countries “I have enormous sympathy for those engaged in the vital task of ensuring that, as the world population continues to increase unsustainably and travel becomes easier, antibiotics retain their availability to overcome disease… It must be incredibly frustrating to witness the fact that antibiotics have too often simply acted as a substitute for basic hygiene, or as it would seem, a way of placating a patient who has a viral infection or who actually needs little more than patience to allow a minor bacterial infection to resolve itself.”
In 2017, the ‘College of Medicine’ mentioned above was discretely re-named ‘College of Medicine and Integrated Health’
In the same year, Charles declared that he will open a centre for alternative medicine in the recently purchased Dumfries House in Scotland. Currently, the College of Medicine and Integrated Health is offering two-day Foundation Courses at this iconic location. Gabriel Chiu, a US celebrity cosmetic and reconstructive surgeon, and his wife Christine, joined the Prince of Wales as he opened the integrated health and wellbeing centre on the Dumfries House Estate in East Ayrshire in 2019. As he unveiled a plaque at the event, Prince Charles said: “I’m so glad that all of you have been able to get here today, particularly because I could not be more proud to see the opening of this new integrated health centre at Dumfries House. It’s something I’ve been wanting to do for the last 35 years. I’m also so proud of all the team at Dumfries House who built it, an all in-house team.
“To reach this point where we can now offer a range of social prescribing opportunities is enormously encouraging and I hope it will be able to make some difference to a lot of the health issues that exist in this area.”
Also in 2017, ‘Country News’ published an article about our heir to the throne stating that Prince of Wales has revealed he uses homeopathic treatments for animals on his organic farm at Highgrove to help reduce reliance on antibiotics, the article stated. He said his methods of farming tried wherever possible to ‘‘go with the grain of nature’’ to avoid dependency on antibiotics, pesticides and other forms of chemical intervention.
In 2018, The Prince of Wales accompanied the Prime Minister of India, Narendra Modi, to the Science Museum in London, and praised Asian medicine practices. The heir to the throne and the Indian Prime Minister then jointly unveiled a plaque for the UK’s first centre of excellence for Indian traditional medicine.
In the same year, it was revealed that UK farmers are being taught how to treat their livestock with homeopathy “by kind permission of His Royal Highness, The Prince Of Wales”
In 2019, the Faculty of Homeopathy announced that His Royal Highness The Prince of Wales had accepted to become Patron of the Faculty of Homeopathy. Dr Gary Smyth, President of the Faculty of Homeopathy comments, “As the Faculty celebrates its 175th anniversary this year, it is an enormous honour for us to receive the Patronage of His Royal Highness The Prince of Wales and I am delighted to announce this news today.” Charles’ move amazed observers who saw it as a deliberate protest against the discontinuation of reimbursement of homeopathy by the NHS.
In 2019, Prince Charles said that yoga had “proven beneficial effects on both body and mind,” and has “tremendous social benefits” that help build “discipline, self-reliance and self-care.”
___________________________________________________________________
So again, Happy Birthday Your Royal Highness – and please don’t forget: it’s not too late to start doing good in the realm of healthcare by supporting good science, critical thinking and evidence-based medicine.
Sincerely yours
Edzard Ernst
The Telegraph published an article entitled ‘Crack or quack: what is the truth about chiropractic treatment?’ and is motivated by the story of Mr Lawler, the 80-year-old former bank manager who died after a chiropractic therapy. Here are 10 short quotes from this article which, in the context of this blog and the previous discussions on the Lawler case, are worthy further comment:
1. … [chiropractic] was established in the late 19th century by D.D. Palmer, an American magnetic healer.
“A lot of people don’t realise it’s a form of alternative medicine with some pretty strange beliefs at heart,” says Michael Marshall, project director at the ‘anti-quack’ charity the Good Thinking Society. “Palmer came to believe he was able to cure deafness through the spine, by adjusting it. The theory behind chiropractic is that all disease and ill health is caused by blockages in the flow of energy through the spine, and by adjusting the spine with these grotesque popping sounds, you can remove blockages, allowing the innate energy to flow freely.” Marshall says this doesn’t really chime with much of what we know about human biology…“There is no reason to believe there’s any possible benefit from twisting vertebra. There is no connection between the spine and conditions such as deafness and measles.”…
Michael Marshall is right, chiropractic was built on sand by Palmer who was little more than a charlatan. The problem with this fact is that today’s chiros have utterly failed to leave Palmer’s heritage behind.
2. According to the British Chiropractic Association (BCA), the industry body, “chiropractors are well placed to deliver high quality evidence-based care for back and neck pain.” …
They would say so, wouldn’t they? The BCA has a long history of problems with knowing what high quality evidence-based care is.
3. But it [chiropractic] isn’t always harmless – as with almost any medical treatment, there are possible side effects. The NHS lists these as aches and pains, stiffness, and tiredness; and then mentions the “risk of more serious problems, such as stroke”….
Considering that 50% of patients suffer adverse effects after chiropractic spinal manipulations, this seems somewhat of an understatement.
4. According to one systematic review, spinal manipulation, “particularly when performed on the upper body, is frequently associated with mild to moderate adverse effects. It can also result in serious complications such as vertebral artery dissection followed by stroke.” …
Arterial dissection followed by a stroke probably is the most frequent serious complication. But there are many other risks, as the tragic case of Mr Lawler demonstrates. He had his neck broken by the chiropractor which resulted in paraplegia and death.
5. “There have been virtually hundreds of published cases where neck manipulations have led to vascular accidents, stroke and sometimes death,” says Prof Ernst. “As there is no monitoring system, this is merely the tip of a much bigger iceberg. According to our own UK survey, under-reporting is close to 100 per cent.” …
The call for an effective monitoring system has been loud and clear since many years. It is nothing short of a scandal that chiros have managed to resist it against the best interest of their patients and society at large.
6. Chiropractors are regulated by the General Chiropractic Council (GCC). Marshall says the Good Thinking Society has looked into claims made on chiropractors’ websites, and found that 82 per cent are not compliant with advertising law, for example by saying they can treat colic or by using the misleading term ‘doctor’…
Yes, and that is yet another scandal. It shows how serious chiropractors are about the ‘evidence-based care’ mentioned above.
7. According to GCC guidelines, “if you use the courtesy title ‘doctor’ you must make it clear within the text of any information you put into the public domain that you are not a registered medical practitioner but that you are a ‘Doctor of Chiropractic’.”…
True, and the fact that many chiropractors continue to ignore this demand presenting themselves as doctors and thus misleading the public is the third scandal, in my view.
8. A spokesperson for the BCA said “Chiropractic is a registered primary healthcare profession and a safe form of treatment. In the UK, chiropractors are regulated by law and required to adhere to strict codes of practice, in exactly the same ways as dentists and doctors. Chiropractors are trained to diagnose, treat, manage and prevent disorders of the musculoskeletal system, specialising in neck and back pain.”…
Chiropractors also like to confuse the public by claiming they are primary care physicians. If we understand this term as describing a clinician who is a ‘specialist in Family Medicine, Internal Medicine or Paediatrics who provides definitive care to the undifferentiated patient at the point of first contact, and takes continuing responsibility for providing the patient’s comprehensive care’, we realise that chiropractors fail to fulfil these criteria. The fact that they nevertheless try to mislead the public by calling themselves ‘primary healthcare professionals’ and ‘doctors’ is yet another scandal, in my opinion.
9. The spokesperson said, “medication, routine imaging and invasive surgeries are all commonly used to manage low back pain, despite limited evidence that these methods are effective treatments. Therefore, ensuring there are other options available for patients is paramount.”…
Here the spokesperson misrepresents mainstream medicine to make chiropractic look good. He should know that imaging is used also by chiros for diagnosing back problems (but not for managing them). And he must know that surgery is never used for the type of non-specific back pain that chiros tend to treat. Finally, he should know that exercise is a cheap, safe and effective therapy which is the main conventional option to treat and prevent back pain.
10. According to the European Chiropractors’ Union, “serious harm from chiropractic treatment is extremely rare.”
How do they know, if there is no system to capture cases of adverse effects?
_________________________________________________________
So, what needs to be done? How can we make progress? I think the following five steps would be a good start in the interest of public health:
- Establish an effective monitoring system for adverse effects that is accessible to the public.
- Make sure all chiros are sufficiently well trained to know about the contra-indications of spinal manipulation, including those that apply to elderly patients and infants.
- Change the GCC from a body defending chiros and their interests to one regulating, controlling and, if necessary, reprimanding chiros.
- Make written informed consent compulsory for neck manipulations, and make sure it contains the information that neck manipulations can result in serious harm and are of doubtful efficacy.
- Prevent chiros from making therapeutic claims that are not based on sound evidence.
If these measures had been in place, Mr Lawler might still be alive today.
On 11/11/2019, the York Press reported from coroner’s inquest regarding a chiropractor who allegedly killed a patient. John Lawler suffered a broken neck while being treated by a chiropractor for an aching leg, an inquest has been told. His widow told how her husband was on the treatment table when things started to go wrong. She said he started shouting at chiropractor Dr Arleen Scholten: “You are hurting me. You are hurting me.” Then he began moaning and then said: “I can’t feel my arms.”
Mrs Lawler said Scholten tried to turn him over and then manoeuvred him into a chair next to the treatment table but he had become unresponsive. “He was like a rag doll,” she said. “His lips looked a little bit blue but I knew he was breathing. “I said ‘Has he had a stroke?’ She put his head back and said ‘no, his features are symmetrical’.
When the paramedics arrived, they treated Mr Lawler and to hospital. He had an MRI scan and a doctor told Mrs Lawler that he had suffered a broken neck. She was then informed that her husband was a paraplegic and he could undergo a 14 hour operation which would be traumatic but even before that could happen he “faded away” and died.
__________________________________________
There are, as far as I can see, four issues of interest here:
- It could be that Mr Lawler had osteoporosis; we will no doubt hear about this in the course of the inquest. If so, normal force could have led to the fracture, and the chiropractor would claim that she is not to blame for the fracture and the subsequent death of her patient. The question then would be whether she was under an obligation to check whether, in a man of Mr Lawler’s age, his bone density was normal or whether she could just assume that it was. In my view, any clinician applying a potentially harmful therapy has the obligation to make sure there are no contra-indications to it. If that all is so, the chiropractor might have been both negligent and reckless.
- Has neck manipulation been shown to be effective for any type of pain in the leg? That’s an easy one: No!
- Has the chiropractor obtained informed consent from her patient before commencing the treatment? The inquest will no doubt verify this. As many chiropractors fail to do it, I would not be too surprised if, in the present case, this was also not done. Should that be so, the chiropractor would have been negligent.
- One might be surprised to hear that the chiropractor manipulated the neck of a patient who consulted her not because of neck pain but because of a condition seemingly unrelated to the neck. This is an issue that comes up regularly and which is therefore importan; some people might be aware that it is dangerous to see a chiropractor when suffering from neck pain because he/she is bound to manipulate the neck. By contrast, most people would probably think it is ok to consult a chiropractor when suffering from lower back pain, because manipulations in that region is far less risky. The truth, however, is that chiropractors have been taught that the spine is one organ and one entity. Thus they tend to check for subluxations (or whatever name they give to the non-existing condition they all aim to treat) in every region of the spine. If they find one in the neck – and they usually do – they would ‘adjust’ it, meaning they would apply one or more high-velocity, low-amplitude thrusts and manipulate the neck. This could well be, I think, how the chiropractor in the case that is before the court at present came to manipulate the neck of her patient. And this might be how poor Mr Lawler lost his life.
Is there a lesson to be learnt from this tragic case?
Yes, I think there is: if you want to make sure that a chiropractor does not break your neck, don’t go and consult one – whatever your health problem happens to be.
“Maybe it is as simple as: I enjoyed that treatment, it was worth the amount I spent on it and I feel better.”
This argument between the fans and the critics of so-called alternative medicine (SCAM) might be the key to understanding the two opposing positions. It applies across the board to all the SCAMs that lack solid evidence (which, of course, is most).
- The sceptic asks for evidence of effectiveness and finds none that is convincing. He concludes that the SCAM is not evidence-based.
- The SCAM enthusiast cannot argue with the evident lack of evidence, but says (as Angela did in a recent comment): “Maybe it is as simple as: I enjoyed that treatment, it was worth the amount I spent on it and I feel better.”
Both positions may well be correct. And both are held with total conviction. Thus, many consumers who are not deeply into SCAM are confused or even bewildered.
So, how can we make sense of this situation?
Let me start with the argument of the SCAM enthusiast. She is, of course, right to sate that she enjoyed reflexology, or aromatherapy, or crystal therapy. She might also enjoy having her hair done, or soaking in a bath, or drinking a glass of champagne. There is nothing wrong with that, and we should all be happy for her.
Enjoying something is often good for you – often but not always. Enjoying a fag isn’t. Enjoying a bottle of whiskey per evening isn’t. Enjoying a drive at neck-breaking speed on a public motorway isn’t. Enjoying sending out hate-mail isn’t. But innocent treats like a foot massage by an aromatherapist probably is!
But none of these things can be considered to be a THERAPY. Feeling better is not necessarily a therapeutic aim.
So, the situation might not be so confusing after all: enjoyments are enjoyments. They are usually fine, and they are often very personal. Some people enjoy being massaged, others don’t. But enjoyments are not therapies. This means that all would be fine, if we stopped calling aromatherapy, reflexology, crystal therapy THERAPIES, and if we stopped calling aromatherapists, etc. THERAPISTS.
Therapies are medical interventions, and as such they need evidence to back them up, evidence that they do something positive to our health. Therapists are healthcare professionals who make therapeutic claims that need evidence to back them up. If that is missing, sceptics are entirely correct to criticise them. In fact, they fulfil a public service when criticising bogus therapies or claims.
So, the confusion mentioned above mainly arises from mislabelling enjoyments as therapies. Lets call aromatherapists, etc. by different names, and the confusion disappears. Let’s stop aromatherapists, etc. making therapeutic claims, and there is no more reason for sceptics to criticise.
When I worked as a junior doctor in a homeopathic hospital, this is what I was told in no uncertain terms: children are ideal patients of homeopathy, because they respond particularly well to it. Most books on the subject confirm this message. The reason for the assumption is as simple as it is simplistic: children are relatively unspoilt by conventional drugs that can hinder the effects of homeopathy.
Many years later, when we conducted one of our clinical trials of homeopathy, we opted for a study with children, because all homeopaths believe in this dogma. For the same reason, it made (homeopathic) sense for the paediatricians of my former medical school (LMU Munich) to run a homeopathic clinic for decades. Not just that, they also taught homeopathy to medical students.

In the course of doing this for such a long time, they did their research and, of course, gathered tons of experience. And what does this wisdom and insight collected over decades reveal? Does it confirm the dogma that kids are excellent homeopathy-responders? Or perhaps does it reject the notion?
The question has just been definitively answered by a (well-hidden) remark in an announcement from the university paediatrics department entitled Integrative Pädiatrie. The original text is below; for those who don’t read German, I will translate:
Our healthcare for children is devoted to a holistic approach which considers biological and psychosocial dimensions of health and disease.
We see positive potential in the use of music, art and humour. Methods from integrative medicine such as mind/body therapies or integrative movement therapy can have curative effects. These and other methods are also being tested in scientific studies.
Homeopathic remedies, however, are not being used in Hanauer’s Paediatric Hospital because, after 200 years of research, it has become clear that the basis of homeopathy is not in accordance with the modern concepts of the natural sciences.
________________________________________________________________
Unsere Medizin für kranke Kinder ist einer ganzheitlichen Sicht verpflichtet, die neben den biologischen auch psychosoziale Dimensionen von Gesundheit und Krankheit berücksichtigt.
Wir sehen das positive Potential durch den Einsatz von Musik, Kunst oder Humor. Auch Methoden der “Integrativen Medizin”, wie zum Beispiel die “mind-body-Medizin” oder die Technik der integrativen Bewegungstherapie können eine heilende Wirkung haben. Diese und andere Methoden werden zum Teil auch in wissenschaftlichen Studien geprüft.
Homöopathische Arzneimittel kommen im Dr. von Haunerschen Kinderspital hingegen nicht zum Einsatz, da sich nach über 200 Jahren wissenschaftlicher Forschung klar herausgestellt hat, dass ihre Grundlagen nicht mit dem modernen Verständnis der Naturwissenschaft in Einklang zu bringen sind.
__________________________________________________________________
Let’s be clear what exactly the last paragraph means:
- This institution has bee open to homeopathy for a very long time.
- They treated children homeopathically.
- They conducted research in homeopathy.
- They taught homeopathy to medical students.
- Eventually, they could no longer ignore what was before their eyes.
- They stopped using homeopathy.
- And they discontinued their course of homeopathy.
Why?
Because highly diluted homeopathic remedies are pure placebos – and that is true for children, adults and even animals.
The Sueddeutsche Zeitung reported yesterday that the Bavarian government has given the go-ahead to a major study of homeopathy, and Die Zeit published a similar article. For those who read German, I append the text from the SZ below. For those who don’t, let me give a short summary.
The study is aimed at clarifying whether the use of homeopathic remedies can reduce the use of antibiotics in humans and animals. The vote was carried because of the CDU delegates being in favour. The debate of the project was, however, controversial. Critics stressed that, at best, the study is superfluous and pointed out that the project is negligent because it implies that homeopathics might be effective, whereas the evidence shows the opposite. A SPD delegate stated that he is ‘open moth’, homeopathy works because of the doctor-patient contact and not because of its remedies which are pure placebos.
The project was tabled because some people had worried about antibiotic resistance and felt that homeopathy might be an answer. Some CSU delegates stated that in ENT medicine, there is evidence that homeopathics can reduce the use of antibiotics. Even in cases of severe sepsis, there was good evidence, they claimed.
___________________________________________________________________
Mit einer medizinischen Studie soll die Staatsregierung klären, ob durch homöopathische Mittel der Einsatz von Antibiotika reduziert werden kann. Dies hat der Landtag am Donnerstag mit den Stimmen der Regierungsfraktionen von CSU und Freien Wählern beschlossen. Bei der namentlichen Abstimmung votierten 120 Abgeordnete für den Antrag und damit acht mehr, als die Koalition selbst stellt. Im Plenum löste der Antrag, der im Zusammenhang mit weiteren Maßnahmen gegen sogenannte multiresistente Keime besprochen wurde, teils kontroverse Debatten aus. Kritiker der Homöopathie betonten, dass die Studie bestenfalls überflüssig sei.
“Das Vorhaben der bayerischen Staatsregierung ist fahrlässig, weil es bereits mit der Fragestellung suggeriert, dass homöopathische Mittel wie Globuli multiresistente Keime bekämpfen könnten”, sagte Dominik Spitzer (FDP). Bisher habe keine wissenschaftliche Studie beweisen können, dass homöopathische Mittel allein gegen Beschwerden wirkten.
Auch die SPD-Abgeordnete Ruth Waldmann hatte bereits vor der Debatte zum Ansinnen der CSU gesagt: “Da bleibt einem der Mund offen stehen.” Wenn an Homöopathie “wirklich nachweislich etwas wirkt, dann ist es der Anteil der sprechenden Medizin, der ganzheitliche Blick auf die Patienten”. Das tue vielen Menschen gut. “Und da bin ich auch dafür, das den Leuten zu lassen”, betonte Waldmann. “Aber bei schwerer Sepsis auch nur daran zu denken, diese Kügelchen womöglich anstelle von Antibiotika zu verabreichen”, das könne sie nicht mehr nachvollziehen.
Die CSU-Landtagsfraktion hatte ein Paket von insgesamt fünf Anträgen eingereicht, mit denen sie erreichen will, dass es weniger Todesfälle durch multiresistente Keime gibt. Dazu gehöre es, im Alltag den Antibiotika-Einsatz zu reduzieren, auch in der Landwirtschaft. Fahrlässig eingesetzte Antibiotika werden von Forschern mit als Grund dafür genannt, dass Krankheitserreger resistent werden. In einem dieser Anträge wird die Staatsregierung aufgefordert, per Studie untersuchen zu lassen, wie der Antibiotika-Einsatz reduziert werden kann – und ob dabei womöglich auch homöopathische Präparate eine “positive Rolle” spielen.
Im Bereich der Hals-Nasen-Ohren-Erkrankungen, so die CSU-Abgeordneten, hätten Studien aufzeigen können, “dass durch den Einsatz klassischer Homöopathie sowohl ein Einsatz von Antibiotika vermieden als auch eine Verbesserung der individuellen Infektabwehr erreicht werden konnte”. Auch an schwer septischen Patienten – also Patienten, bei denen das körpereigene Abwehrsystem bereits die Organe und das Gewebe schädigte – habe eine Studie Hinweise darauf gebracht, dass eine homöopathische Behandlung “eine nützliche Behandlungsmethode” darstellen könne.
________________________________________________________________________
The notion that there might be good evidence for the efficacy of homeopathy in ENT and sepsis is clearly mistaken. On this blog, we have even discussed a tragic case of a child dying because of this erroneous belief. Homeopathy does not work in humans nor in animals as an alternative to antibiotics. And, of course, the notion that there is good, reproducible evidence to show that homeopathy effectively cures sepsis is a most dangerous fallacy. (There have been some experiments along these lines in the Dachau concentration camp, but they cannot seriously mean that!)
As far as I know it is as yet unclear what the precise research questions of the Bavarian project are, how much money will be spent on it (I saw a mention of 400 000 Euros), who is going to conduct the research, etc. No doubt, we will learn all this in due course. Meanwhile, if I may be so bold as to recommend someone for designing the research, I can think of nobody better suited than the only person who truly believes that it can produce a positive result: PRINCE CHARLES.
