The claim that homeopathy has a role in oncology does not seem to go away. Some enthusiasts say it can be used as a causal therapy, while others insist it might be a helpful symptomatic adjuvant. Almost all oncologists agree that homeopathy has no place at all in cancer care.
Who is right?
This systematic review included clinical studies from 1800 until 2020 to evaluate evidence of the effectiveness of homeopathy on physical and mental conditions in patients during oncological treatment.
In February 2021 a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning use, effectiveness, and potential harm of homeopathy in cancer patients.
From all 1352 search results, 18 studies with 2016 patients were included in this SR. The patients treated with homeopathy were mainly diagnosed with breast cancer. The therapy concepts included single and combination homeopathic remedies (used systemically or as mouth rinses) of various dilutions. The outcomes assessed were:
- the influence on toxicity of cancer treatment (mostly hot flashes and menopausal symptoms),
- the time to drain removal in breast cancer patients after mastectomy,
- survival,
- quality of life,
- global health,
- subjective well-being,
- anxiety and depression,
- safety and tolerance.
The included studies reported heterogeneous results: some studies described significant differences in quality of life or toxicity of cancer treatment favoring homeopathy, whereas others did not find an effect or reported significant differences to the disadvantage of homeopathy or side effects caused by homeopathy. The majority of the studies had low methodological quality.
The authors concluded that, the results for the effectiveness of homeopathy in cancer patients are heterogeneous, mostly not significant and fail to show an advantage of homeopathy over other active or passive comparison groups. No evidence can be provided that homeopathy exceeds the placebo effect. Furthermore, the majority of the included studies shows numerous and severe methodological weaknesses leading to a high level of bias and are consequently hardly reliable. Therefore, based on the findings of this SR, no evidence for positive effectiveness of homeopathy can be verified.
This could not be clearer. Some might argue that, of course, homeopathy cannot change the natural history of cancer, but it might improve the quality of life of those patients who believe in it via a placebo response. I would still oppose this notion: there are many effective treatments in the supportive treatment of cancer, and it seems much better to use those options and tell patients the truth about homeopathy.
In Germany, so-called alternative medicine (SCAM) is used by about 6o% of the population. The type and extent of in-patient complementary care are, however, largely unknown.
The objective of this study was, therefore, to conduct a survey on SCAM procedures in Bavarian acute care hospitals by screening the websites of all respective facilities in order to cover a broad range of SCAMs.
In 2020, an independent and comprehensive website screening of all 389 Bavarian acute hospitals, including all departments, was conducted by two independent raters. SCAMs offered were analyzed in total as well as separately by specialty.
Among all 389 Bavarian acute care hospitals, 82% offered at least one and 66% at least three different SCAMs on their website. Relaxation techniques (52%), acupuncture (44%), massage (41%), movement-, art-, and music therapy (33%, 30%, and 28%), meditative movement therapies like yoga (30%), and aromatherapy (29%) were offered most frequently. Separated by specialty, SCAMs were most common in psychiatry/psychosomatics (relaxation techniques 69%, movement and art therapy 60% each) at 87%, and in gynecology/obstetrics (most common acupuncture 64%, homeopathy 60%, and aromatherapy 41%) at 72%.
The stated areas of application of SCAM included:
- use as a stand-alone therapy (65%; n=254),
- for prevention (7%; n=27),
- as support for conventional therapy (7%; n=27)
- as preparation before drug therapy or surgery (5%; n=18).
The authors concluded that the vast majority of Bavarian acute care hospitals also seem to conduct complementary medicine procedures in therapy, especially for psychological indications and in obstetrics and gynaecology, according to the hospital websites. How often these procedures are used in inpatient or outpatient settings as well as evidence on effectiveness of the applied procedures should be investigated in further studies.
In my view, this article invites several points of criticism.
Something that irritates me regularly is the fact that much of SCAM research takes years to be published. If a given research project is important, it would seem unethical to sit on it for so long. If it is not important, it is unethical to conduct it in the first place. In the above case, we are dealing with a survey of SCAM use, and we know that SCAM use is strongly influenced by fashion which means it changes fast and frequently. I would therefore argue that data that are now three years old are of limited interest.
Another point is the lack of a definition or range of treatments included. The authors state they looked for whatever form of SCAM the websites mentioned (herbal medicine is popular in Germany, yet absent in this survey; this suggests that the survey method has created a blind spot). Yet, they include as SCAM things like massage (which in Germany is entirely mainstream), physiotherapeutic exercise (Bewegungstherapie), and biofeedback all of which are arguably conventional treatments. This means that the true prevalence figures of SCAM use are not nearly as high as they pretend.
My main criticism would be that the authors abstain from any comments about the evidence for the SCAMs they monitored. They stated that this was beyond the scope of the project. As the research was supported by the Bavarian government, it would nevertheless have been essential, in my view, to dedicate a few words about the fact that many of the SCAMs and their uses are not evidence-based.
Essentially, this survey is in the tradition of hundreds of previous SCAM prevalence surveys that show a high degree of popularity of SCAM and thus imply that
IF SCAM IS SO VERY POPULAR, IT MUST BE GOOD;
AND IF IT’S GOOD, WE MUST HAVE MORE OF IT.
PS
It is often said that SCAM researchers are relatively free of financial conflicts of interest. Let me show you the complete list of conflicts declared by the authors of this survey.
- JL: received funding for this project from the Bavarian State Ministry of Health and Care; Further research support: Steigerwald Arzneimittelwerke GmbH, Falk Foundation; TechLab, Dr. Willmar Schwabe; Repha GmbH biologic drugs; Lecture fees: Falk Foundation, Repha GmbH biologic drugs; Celgene GmbH; Dr. Willmar Schwabe; Medice Arzneimittel, Galapagos Biopharma; consultant/expert: Medizinverlage Stuttgart; Steigerwald Arzneimittelwerke GmbH; Repha GmbH; Ferring Arzneimittel GmbH; Dr. Willmar Schwabe
- TK: received funding for this project from the Bavarian State Ministry of Health and Care, beyond that there are no other conflicts of interest
- CL: Lecture fees: Celgene GmbH, Roche GmbH, Novartis Pharma GmbH, BMS GmbH & Co. KGaA, Mundipharma GmbH Co. KG, Merck KGaA.
A “null field” is a scientific field where there is nothing to discover and where observed associations are thus expected to simply reflect the magnitude of bias.
This analysis aimed to characterize a null field using a known example, homeopathy (a pseudoscientific medical approach based on using highly diluted substances), as a prototype. The researchers identified 50 randomized placebo-controlled trials of homeopathy interventions from highly cited meta-analyses. The primary outcome variable was the observed effect size in the studies. Variables related to study quality or impact were also extracted.
The mean effect size for homeopathy was 0.36 standard deviations (Hedges’ g; 95% confidence interval: 0.21, 0.51) better than placebo, which corresponds to an odds ratio of 1.94 (95% CI: 1.69, 2.23) in favor of homeopathy. 80% of studies had positive effect sizes (favoring homeopathy). The effect size was significantly correlated with citation counts from journals in the directory of open-access journals and CiteWatch. We identified common statistical errors in 25 studies.
The authors concluded that a null field like homeopathy can exhibit large effect sizes, high rates of favorable results, and high citation impact in the published scientific literature. Null fields may represent a useful negative control for the scientific process.
The paper is perhaps not the easiest to comprehend but once you got the idea, you will agree with me that it is BRILLIANT. I warmly recommend it to all fans of homeopathy – in fact, if I could I’d offer it to King Charles as a present for the coronation.
Its authors are among the most prominent medical epidemiologist of our time with affiliations that speak for themselves:
- Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA; Meta-Research Innovation Center at Stanford (METRICS), Stanford University, Stanford, CA, USA.
- 2Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA.
- 3Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA; Meta-Research Innovation Center at Stanford (METRICS), Stanford University, Stanford, CA, USA; Department of Medicine, Stanford University, Stanford, CA, USA; Department of Biomedical Data Science, Stanford University, Stanford, CA, USA; Department of Statistics, Stanford University, Stanford, CA, USA.
It is, of course, a pity that the article is behind a paywall – but fortunately, the senior author, John Ioannidis, published his email address together with the abstract: [email protected]. So, if you have trouble understanding the point of the analysis, I suggest you ask for a reprint to get your head around it. I promise it’s worth it.
Irritable bowel syndrome (IBS) is a common chronic disorder associated with psychological distress and reduced health-related quality of life (HRQoL). Therefore, stress management is often employed in the hope of alleviating IBS symptoms. But does it work?
This systematic review investigated the effects of stress management for adults with IBS on typical symptoms, HRQoL, and mental health. The predefined criteria included:
- patients: adults with IBS;
- intervention: stress management;
- control: care as usual or waitlist;
- outcome: patient-relevant;
- study-type: controlled trials.
Two researchers independently reviewed the publications retrieved through electronic searches and assessed the risk of bias using the Scottish Intercollegiate Guidelines Network checklist. The researchers performed a meta-analysis with homogeneous trials of acceptable quality.
After screening 6656 publications, 10 suitable randomized trials of acceptable (n = 5) or low methodological quality (n = 5) involving 587 patients were identified. The meta-analysis showed no effect of stress management on IBS severity 1-2 months after the intervention (Hedges’ g = -0.23, 95%-CI = -0.84 to -0.38, I2 = 86.1%), and after 3-12 months (Hedges’ g = -0.77, 95%-CI = -1.77 to -0.23, I2 = 93.3%). One trial found a short-term reduction of symptoms, and one trial found symptom relief in the long term (at 6 months). One of two studies that examined HRQoL found an improvement (after 2 months). One of two studies that examined depression and anxiety found a reduction of these symptoms (after 3 weeks).
The authors concluded that stress management may be beneficial for patients with IBS regarding the short-term reduction of bowel and mental health symptoms, whereas long-term benefits are unclear. Good quality RCTs with more than 6 months follow-up are needed.
Considering the actual evidence, I find the conclusions rather odd. Would it not have been more honest to state something along the following lines?:
There is currently no convincing evidence to suggest that stress management benefits IBS patients.
So why, be not more open and less misleading?
Could some of the authors’ affiliations provide a clue?
- Department for Internal and Integrative Medicine, Sozialstiftung Bamberg Hospital, Bamberg, Germany.
- Department for Integrative Medicine, University of Duisburg-Essen, Medical Faculty, Bamberg, Germany.
Quite possibly, yes!
Massages are experienced as agreeable by most patients. But that does not necessarily mean that it improves our quality of life. This study tests whether it does.
This study compared three massage dosing strategies among inpatients receiving palliative care consultation. It was designed as a three-armed randomized trial examining three different doses of therapist-applied massage to test change in overall quality of life (QoL) and symptoms among hospitalized adult patients receiving palliative care consultation for any indication:
- Arm I: 10-min massage daily × 3 days;
- Arm II: 20-min massage daily × 3 days;
- Arm III: single 20-min massage.
The primary outcome measure was the single-item McGill QoL question. Secondary outcomes measured pain/symptoms, rating of peacefulness, and satisfaction with the intervention. Data were collected at baseline, pre-and post-treatment, and one-day post-last treatment (follow-up). Repeated measure analysis of variance and paired t-test were used to determine significant differences.
A total of 387 patients participated (55.7 (±15.49) years old, mostly women (61.2%) and African-American (65.6%)). All three arms demonstrated within-group improvement at follow-up for McGill QoL (all P < 0.05). No significant between-group differences were found. Finally, repeated measure analyses demonstrated time to predict immediate improvement in distress (P ≤ 0.003) and pain (P ≤ 0.02) for all study arms; however, only improvement in distress was sustained at follow-up measurement in arms with three consecutive daily massages of 10 or 20 minutes.
The authors concluded that massage therapy in complex patients with advanced illness was beneficial beyond dosage. Findings support session length (10 or 20 minutes) was predictive of short-term improvements while treatment frequency (once or three consecutive days) predicted sustained improvement at follow-up.
I like this study because it teaches us an important lesson:
IF ONE DESIGNS A SILLY STUDY, ONE IS LIKELY TO ARRIVE AT A SILLY CONCLUSION.
This study does not have a proper control group. Therefore, we cannot know whether the observed outcomes were due to the different interventions or to non-specific effects such as expectation, the passing of time, etc.
The devil’s advocate conclusion of the findings is thus dramatically different from that of the authors: the results of this trial are consistent with the notion that massage has no effect on QoL, no matter how it is dosed.
Reiki is a Japanese form of energy healing used predominantly for stress reduction and relaxation. It is based on the notion that a mystical “life force energy” flows through us and is what causes us to be alive.
This study was conducted by researchers from the Department of Elderly Care, Vocational School of Health Services, Mardin Artuklu University, Mardin, Turkey, and the Internal Medicine Nursing Department, Mersin University Faculty of Nursing, Mersin, Turkey. Its aim was to determine the effect of Reiki when applied before upper gastrointestinal endoscopy on levels of anxiety, stress, and comfort. It was designed as a single-blind, randomized, sham-controlled study and conducted between February and July 2021.
Patients who were scheduled for gastrointestinal endoscopy and who met the inclusion criteria were randomized into three groups: 
- Reiki,
- sham Reiki,
- control (no intervention).
A total of 159 patients participated in the study. In groups 1 and 2, Reiki and sham Reiki was applied once for approximately 20 to 25 minutes before gastrointestinal endoscopy.
When the Reiki group was compared to the sham Reiki and control groups following the intervention, the decrease in the levels of patient stress (P < .001) and anxiety (P < .001) and the increase in patient comfort (P < .001) were found to be statistically significant.
The authors concluded that Reiki applied to patients before upper gastrointestinal endoscopy was effective in reducing stress and anxiety and in increasing comfort.
As this paper is behind a paywall, I wrote to the authors and asked for a reprint. Unfortunately, I received no reply at all. Thus, I find it difficult to comment. Yet, the study might be important, particularly because there are not many sham-controlled trials of Reiki.
The abstract merely informs us that Reiki was better than sham Reiki. It does not tell us what constituted the sham intervention. Crucially, we also cannot know whether the patients were adequately blinded or whether they were able to tell the sham from the verum.
In the absence of this information, I am merely able to state that Reiki lacks plausibility and is most unlikely, in my view, to have any specific therapeutic effects. This means that the most likely explanation for the extraordinary results of this study is the de-blinding of some of the patients in group 2 or some other source of bias that cannot be identified from just studying the abstract.
PS
If someone can send me the full paper, I’d be more than happy to clarify the apparent mystery.
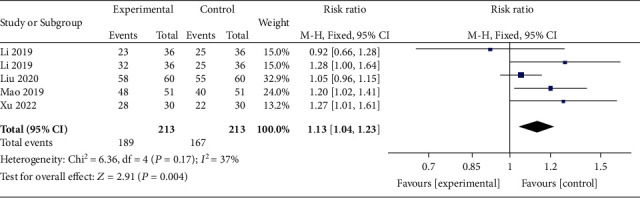
This meta-analysis aimed “to provide better evidence of the efficacy of manual therapy (MT) on adolescent idiopathic scoliosis (AIS)”. 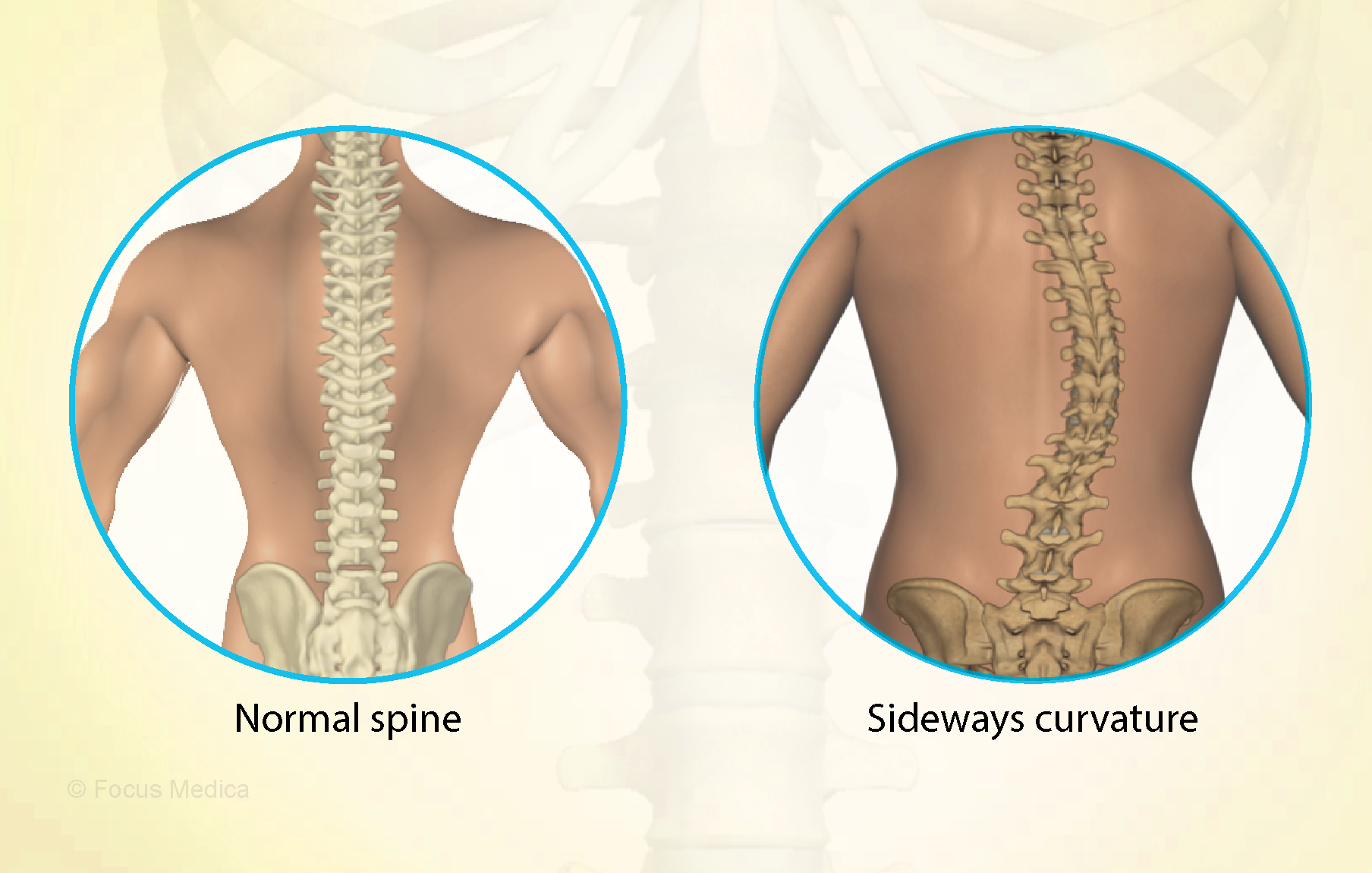
All RCTs of MT for the management of patients with AIS were included in the present study. The treatment difference between the experimental and control group was mainly MT. The outcomes consisted of the total effective rate, the Cobb angle, and Scoliosis Research Society-22 (SRS-22) questionnaire score. Electronic database searches were conducted from database inception to July 2022, including the Cochrane Library, PubMed, Web of Science, Embase, Wanfang Data, CNKI, and VIP. The pooled data were analyzed using RevMan 5.4 software.
Four RCTs with 213 patients in the experimental groups were finally included. There are 2 studies of standalone MT in the experimental group and 3 studies of MT with identical conservative treatments in the control group. Three trials reported the total effective rate and a statistically significant difference was found (P = 0.004). Three trials reported Cobb angle; a statistical difference was found (P = 0.01). Then, sensitivity analysis showed that there was a significant difference in the additional MT subgroup (P < 0.00001) while not in the standalone MT subgroup (P = 0.41). Three trials reported SRS-22 scores (P = 0.55) without significant differences.
The authors concluded that there is insufficient data to determine the effectiveness of spinal manipulation limited by the very low quality of included studies. High-quality studies with appropriate design and follow-up periods are warranted to determine if MT may be beneficial as an adjunct therapy for AIS. Currently, there is no evidence to support spinal manipulation. 
The treatment of idiopathic scoliosis depends on the age, curve size, and progression of the condition. Therapeutic options include observation, bracing, physiotherapy, and surgery. They do NOT include MT because it is neither a plausible nor effective solution to this problem. It follows that further studies are not warranted and should be discouraged.
And, even if you disagree with me here and feel that further studies might be justified, let me remind you that proper research is never aimed at providing better evidence that a therapy works (as the authors of this odd paper seem to think); it must be aimed at testing whether it is effective!
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 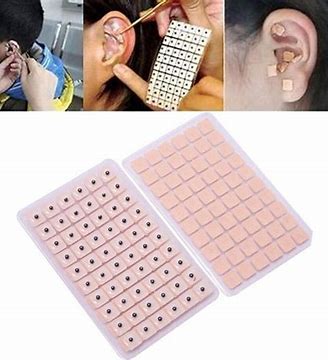
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.
Austrian doctors recently received a notice in their mailbox about a postgraduate training event that is remarkable, to say the least.
The Vienna Medical Association is organizing a postgraduate training course on “Complementary Medical Homeopathy for Post- and Long Covid“. The date for the event is 20.4.2023. Registration for it is via the Association’s “Department of Complementary and Integrative Medicine”.
In case you ask, what is wrong with such a course? There is no scientific evidence that homeopathy has a specific, positive effect in long/post covid. Therefore the announced event has about the same validity as a lecture series for:
- BUNGEE JUMPING FOR DIABETES
or
- DOUGHNUT EATING FOR CORONARY HEART DISEASE
or
- CIGARETTE SMOKING IN CANCER PREVENTION
While relevant pseudomedicine training courses have in the past been organized by the relevant Austrian SCAM-organizations, the Vienna Medical Association itself is now joining the ranks of the organizers of pseudomedicine training courses. Whereas pseudomedicine has so far been the domain of physicians in private practice in Austria, it now appears to be promoted by the Vienna Medical Association in hospitals as well.
The Vienna Medical Association boldly claims that MEDICAL ETHICS IS THE BASIS OF OUR WORK. Well guess what, guys: teaching nonsense is not very ethical!
The ‘tasks and goals’ of the Association’s ‘Department for Complementary and Integrative Medicine’ of the Vienna Medical Association are explained on their website:
The aim of our department is to represent doctors with additional diplomas in the medical association and to inform about the value of their special therapeutic approaches better than previously – particularly in cases of serious side effects of conventional therapies.
In the sense of conveying up-to-date, high-quality, medical, and complementary education and training in complementary medicine, our department aims to publish relevant articles and announcements of dates of the respective professional societies in the chamber’s own media.
Practice-oriented introductory lectures or study groups on the following topics are also planned topics:
- medical homeopathy,
- psychosomatic relaxation therapy (bipolar harmonising abdominal breathing, autogenic training),
- acupuncture,
- regulation therapy based on skin resistance measurements at acupuncture points,
- TCM,
- herbal therapy, etc.
“Up-to-date, high-quality, medical, and complementary education and training in complementary medicine” – oh really? If the Association’s “Department of Complementary and Integrative Medicine” is truly interested in this, I herewith offer to give a free lecture series for them that would teach them the high-quality evidence truly shows.
Meanwhile, as there is no good evidence that homeopathy is an effective therapy for post/long Covid, the question of whether the ‘Vienna Medical Association’ has taken leave of its senses, must be answered in the affirmative.
I am pleased to announce that our regular contributors ‘DC‘ as well as ‘mimi‘ both correctly guessed the person responsible for the quote about informed consent that was the subject of yesterday’s post. Congratulations to both; that certainly wasn’t easy!
The quote is by Karl Brandt.
Who was Karl Brandt?
Brandt was a young and evidently gifted doctor when, during a series of coincidences, he became a member of Hitler’s ‘inner circle’ and acted as one of Hitler’s personal physicians (originally, he had wanted to join the team of Albert Schweitzer!). Hitler liked the good-looking, ambitious Brandt and thus gave him greater and greater responsibilities and power. Amongst other things, Brandt managed to become in charge of the German euthanasia program which killed about 70 000 patients who the Nazis considered to be ‘useless eaters’ and unworthy of their support. It had the cynical purpose of freeing up hospital beds for the war and cleansing the German gene pool. Brandt also was responsible for many of the unspeakably cruel and immoral medical experiments in the concentration camps.
After the war, Brandt was put on trial in Nuremberg. The trial became known as the ‘Doctors’ Trail‘. Twenty of the 23 defendants were medical doctors (Viktor Brack, Rudolf Brandt, and Wolfram Sievers were Nazi officials). They were accused of having been involved in Nazi human experimentation and mass murder under the guise of euthanasia. Brandt insisted that he had never done anything wrong, had followed orders, and had been guided by the highest morals, solid medical ethics, and his determination to do the very best for the German people.
During his interrogations, he stated the sentences that fascinated me when I first read it: ” On the one hand, there are experiments that are carried out for or with someone on a voluntary basis; on the other hand, there are those that take place against the will of the person concerned. A further subdivision indicates whether they are particularly dangerous or comparatively harmless and without any potential for danger. A further distinction must be made as to whether the result of the experiment is important or whether it is merely a ridiculous game played by a scientifically educated person. These six criteria form a kind of guideline that enables one to say YES or NO from a medical point of view.”
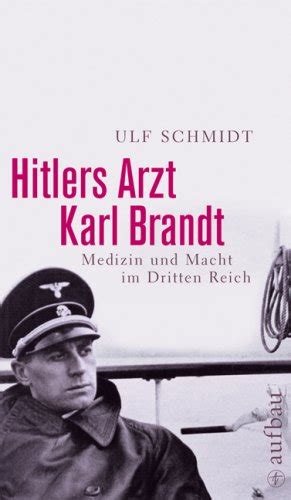 The quote is cited in the book by Ulf Schmidt which is extremely well-researched and worth reading for anyone with an interest in the subject. In my view, it gives a unique insight into the thinking of someone who clearly was bright yet power-hungry, scrupulous and deeply immoral:
The quote is cited in the book by Ulf Schmidt which is extremely well-researched and worth reading for anyone with an interest in the subject. In my view, it gives a unique insight into the thinking of someone who clearly was bright yet power-hungry, scrupulous and deeply immoral:
- experiments “against the will of the person concerned” always were unlawful, immoral, and unethical according to the guidelines that existed at the time;
- “particularly dangerous” experiments should have never been considered;
- research that is merely a “ridiculous game played by a scientifically educated person” is pseudoscience and not ethical.
Brandt tried to present himself as the ‘honest’, upright Nazi who did what he did because of a deep conviction and because he wanted the best. He seemed to have fooled others and possibly even himself. Several influential personalities rallied to his support. Yet, the judges at Nuremberg did neither believe his version of events nor were they inclined to pardon his behavior. Brandt was found guilty of:
- War crimes: performing medical experiments, without the subjects’ consent, on prisoners of war and civilians of occupied countries, in the course of which experiments the defendants committed murders, brutalities, cruelties, tortures, atrocities, and other inhuman acts. Also planning and performing the mass murder of prisoners of war and civilians of occupied countries, stigmatized as aged, insane, incurably ill, deformed, and so on, by gas, lethal injections, and diverse other means in nursing homes, hospitals, and asylums during the Euthanasia Program and participating in the mass murder of concentration camp inmates;
- Crimes against humanity: committing crimes also on German nationals;
- Membership in a criminal organization, the SS. The charges against him included special responsibility for, and participation in, Freezing, Malaria, LOST Gas, Sulfanilamide, Bone, Muscle and Nerve Regeneration and Bone Transplantation, Sea-Water, Epidemic Jaundice, Sterilization, and Typhus Experiments.
Brandt was executed on 2 June 1948.
The discussions around informed consent at the Nuremberg ‘doctors trial’ brought this subject into a renewed focus and eventually led to the formulation of the now famous ‘Nuremberg Code‘.