clinical trial
Konjac glucomannan (KGM), also just called ‘glucomannan’, is a dietary fiber hydro colloidal polysaccharide isolated from the tubers of Amorphophallus konjac. It is used as a food, a food additive, as well as a dietary supplement in many countries. KGM is claimed to reduce the levels of glucose, cholesterol, triglycerides, and blood pressure.
The objective of this study was to evaluate the effect of the consumption of gummy candy enriched with KGM on appetite and to evaluate anthropometric data, biochemical, and oxidative stress markers in overweight individuals. Forty-two participants aged 18 to 45 years completed this randomized, double-blind, placebo-controlled clinical trial. Participants were randomly assigned to consume for 14 days, 2 candies per day, containing 250 mg of KGM or identical-looking placebo candy with 250 mg of flaxseed meal, shortly after breakfast and dinner. As a result, we observed that there was a reduction in waist circumference and in the intensity of hunger of the participants who consumed KGM. The authors believe that a longer consumption time as well as an increased dose of KGM would contribute to even more satisfactory body results.
These findings seem promising, yet somehow I am not convinced. The study was small and short-term; moreover, the authors seem uncritical and, instead of a conclusion, they offer speculations.
Our own review of 2014 included 9 clinical studies. There was a variation in the reporting quality of the included RCTs. A meta-analysis (random effect model) of 8 RCTs revealed no significant difference in weight loss between glucomannan and placebo (mean difference [MD]: -0.22 kg; 95% confidence interval [CI], -0.62, 0.19; I(2) = 65%). Adverse events included abdominal discomfort, diarrhea, and constipation. We concluded that the evidence from available RCTs does not show that glucomannan intake generates statistically significant weight loss. Future trials should be more rigorous and better reported.
Rigorous trials are required to change my mind, and I am not sure that the new study falls into this category.
If you think that scanning through dozens of new scientific articles every week is a dry and often somewhat tedious exercise, you are probably correct. But every now and then, this task is turned into prime entertainment by some pseudoscientists trying to pretend to be scientists. Take, for instance, the latest homeopathy study by Indian researchers with no less than 9 seemingly impressive affiliations:
- 1Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector III, Salt Lake, Kolkata, West Bengal, India.
- 3Department of Homoeopathy, State Homoeopathic Dispensary, Karaila, Pratapgarh, Uttar Pradesh, India.
- 4Department of Homoeopathy, State Homoeopathic Dispensary, Tulsipur, Shrawasti, Uttar Pradesh, India.
- 5Department of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 6State Homoeopathic Dispensary, Mangalbari Rural Hospital, Matiali Block, Jalpaiguri, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 7Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 8Department of Homoeopathy, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Village and Post Office: Gouripur (South), Police Station Bishnupur, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 9Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
Now that I have whetted your appetite, here is their study:
Lumbar spondylosis (LS) is a degenerative disorder of the lumbar spine. Despite substantial research efforts, no gold-standard treatment for LS has been identified. The efficacy of individualized homeopathic medicines (IHMs) in lumbar spondylosis (LS) is unknown. In this double-blind, randomized, placebo-controlled trial, the efficacy of IHMs was compared with identical-looking placebos in the treatment of low back pain associated with LS. It was conducted at the National Institute of Homoeopathy, West Bengal, India.
Patients were randomized to receive IHMs or placebos; standardized concomitant care was administered in both groups. The Oswestry low back pain and disability questionnaire (ODQ) was used as the primary outcome measure; the Roland-Morris questionnaire (RMQ) and the short form of the McGill pain questionnaire (SF-MPQ) served as secondary outcome measures. They were measured at baseline and every month for 3 months. Intention-to-treat analyses (ITT) were used to detect any inter-group differences using two-way repeated measures analysis of variance models overall and by unpaired t-tests at different time points.
Enrolment was stopped prematurely because of time restrictions; 55 patients had been randomized (verum: 28; control: 27); 49 could be analyzed by ITT (verum: 26; control: 23).
The results are as follows:
- Inter-group differences in ODQ (F 1, 47 = 0.001, p = 0.977), RMQ (F 1, 47 = 0.190, p = 0.665) and SF-MPQ total score (F 1, 47 = 3.183, p = 0.081) at 3 months were not statistically significant.
- SF-MPQ total score after 2 months (p = 0.030) revealed an inter-group statistical significance, favoring IHMs against placebos.
- Some of the SF-MPQ sub-scales at different time points were also statistically significant: e.g., the SF-MPQ average pain score after 2 months (p = 0.002) and 3 months (p = 0.007).
- Rhus Toxicodendron, Sulphur, and Pulsatilla nigricans were the most frequently indicated medicines.
The authors concluded that owing to failure in detecting a statistically significant effect for the primary outcome and in recruiting a sufficient number of participants, our trial remained inconclusive.
Now that I (and hopefully you too) have recovered from laughing out loud, let me point out why this paper had me in stitches:
- The trial was aborted not because of a “time limit” but because of slow recruitment, I presume. The question is why were not more patients volunteering? Low back pain with LS is extremely common. Could it be that patients know only too well that homeopathy does not help with low back pain?
- If a trial gets aborted because of very low patient numbers, it is probably best not to publish it or at least not to evaluate its results at all.
- If the researchers insist on publishing it, their paper should focus on the reason why it did not succeed so that others can learn from their experience by avoiding their mistakes.
- However, once the researchers do run statistical tests, they should be honest and conclude clearly that, because the primary outcome measure showed no inter-group difference, the study failed to demonstrate that the treatment is effective.
- The trial did not “remain inconclusive”; it was squarely negative.
- The editor of the journal HOMEOPATHY should know better than to publish such nonsense.
A final thought: is it perhaps the ultimate proof of homeopathy’s ‘like cures like’ assumption to use sound science (i.e. an RCT), submit it to the homeopathic process of endless dilutions and succussions, and – BINGO – generate utter nonsense?
About 3 years ago, I reported that the Bavarian government had decided to fund research into the question of whether the use of homeopathy would reduce the use of antibiotics (an idea that also King Charles fancies). With the help of some friends, I found further details of the project. Here are some of them:
The study on individualized homeopathic treatment to reduce the need for antibiotics in patients with recurrent urinary tract infections is a randomized, placebo-controlled, multicenter, double-blind trial. Frequent urinary tract infections (more than two infections within six months or more than three infections within twelve months) occur in up to three percent of all women during their lifetime and represent a high risk for increased antibiotic use in this population.
The current guidelines therefore also provide for therapeutic approaches without antibiotic administration under close monitoring. The approach to be investigated in the study is the administration of a homeopathic medicine individually selected for the patient for prophylaxis. The number of urinary tract infections and the need for antibiotics will be recorded and evaluated at the end of the trial period, around mid to late 2023.
The aim of the study is to find out whether patients taking homeopathics need antibiotics for the treatment of urinary tract infections less often compared to the placebo group. This could lead to a reduction in the use of antibiotics for recurrent urinary tract infections.
Project participants: Technical University of Munich, Klinikum Rechts der Isar
Project funding: 709,480.75 Euros
Project duration: January 1, 2021 to December 31, 2023
____________________
This sketch is of course not enough for providing a full evaluation of the study concept (if someone has more details, I’d be interested to learn more). From the little information given above, I feel that:
- the design of the trial might be quite rigorous,
- a fairly large sample will be required to have enough power,
- the closing date of 31/12/2023 seems optimistic (but this obviously depends on the number of centers cooperating),
- I, therefore, predict that we will have to wait a long time for the results (the pandemic and other obstacles will have delayed recruitment),
- the costs of the trial are already substantial and might increase due to delays etc.
My main criticism of the study is that:
- I see no rationale for doing such a trial,
- there is no evidence to suggest that homeopathy might prevent recurrent urinary tract infections,
- there is compelling evidence that homeopathic remedies are placebos,
- the study thus compares one placebo with another placebo (in fact, it is a classic example of what my late friend Harriet Hall would have called TOOTH FAIRY SCIENCE),
- therefore, its results will show no difference between the 2 groups (provided the trial was conducted without bias),
- if that is true, enthusiastic homeopaths will claim that the homeopathic verum was inadequate (e.g. because the homeopaths prescribing the verum did not or could not do their job properly),
- when that happens, they will therefore not stop claiming that homeopathy can reduce the over-prescribing of antibiotics;
- that means we will be exactly where we were before the trial.
In other words, the study will turn out to be a waste of 709,480.75 Euros. To express it as I did in my previous post: the Bavarian government has gone barmy!
On 20/1/2023, I conducted multiple Medline searches aimed at generating a rough idea about which areas of so-called alternative medicine (SCAM) are currently more research active than others. I searched for:
- the topic in question
- clinical trial
- publication in 2023
Here are my findings (subject area and the number of hits):
- TCM 56
- dietary supplements 47
- acupuncture 34
- integrative medicine 27
- mindfulness 26
- herbal medicine 23
- massage 10
- aromatherapy 2
- hypnotherapy 2
- osteopathy 2
- tai chi 2
- chiropractic 1
- homeopathy 0
- iridology 0
- naturopathy 0
- Reiki 0
Several caveats must be considered, of course: The searches do not include all SCAMs. The results are not precise and most of the retrieved articles are not really clinical trials (in fact, only a minority are). The numbers are low because I deliberately did this exercise early in the year.
Yet, the findings do, I think, give an indication as to the current state of SCAM research and indicate which areas are more research active than others. To put the numbers in perspective, here are a few conventional therapies for which I searched on the same day and in the same manner:
- pharmacology 539
- physiotherapy 162
- psychiatry 239
- surgery 879
I think this makes one point fairly clear: SCAM is not an impressively research-active area. Another point stems from looking at the individual articles. TCM and acupuncture articles are almost exclusively authored by Chinese researchers. While this might not be surprising, the fact that herbal medicine is similar did amaze me; about half of the papers in this category are by Chinese authors. Essentially, this suggests that more than half of the SCAM articles currently originate from China. Considering the concerns one must have about Chinese SCAM research (see for instance here and here), do you think this finding might be worrying?
The far greater worry, I feel, is the attitude of the SCAM researchers publishing their work. Glancing at these papers I did not get the impression that many approached their subject critically, In fact, most of the papers looked to me overtly promotional and of poor quality. For instance, I did not see a single paper assessing the risks of SCAM which arguably is the most important issue in SCAM research. I admit that these concerns cannot be addressed by the above simple head count; they are best dealt with by critically analyzing individual studies – a task I regularly try to tackle on this blog
In this study, the impact of a multimodal integrative oncology pre- and intraoperative intervention on pain and anxiety among patients undergoing gynecological oncology surgery was explored.
Study participants were randomized into three groups:
- Group A received preoperative touch/relaxation techniques, followed by intraoperative acupuncture, plus standard care;
- Group B received preoperative touch/relaxation only, plus standard care;
- Group C (the control group) received standard care.
Pain and anxiety were scored before and after surgery using the Measure Yourself Concerns and Wellbeing (MYCAW) and Quality of Recovery (QOR-15) questionnaires, using Part B of the QOR to assess pain, anxiety, and other quality-of-life parameters.
A total of 99 patients participated in the study: 45 in Group A, 25 in Group B, and 29 in Group C. The three groups had similar baseline demographic and surgery-related characteristics. Postoperative QOR-Part B scores were significantly higher in the treatment groups (A and B) when compared with controls (p = .005), including for severe pain (p = .011) and anxiety (p = .007). Between-group improvement for severe pain was observed in Group A compared with controls (p = .011). Within-group improvement for QOR depression subscales was observed in only the intervention groups (p <0.0001). Compared with Group B, Group A had better improvement of MYCAW-reported concerns (p = .025).
The authors concluded that a preoperative touch/relaxation intervention may significantly reduce postoperative anxiety, possibly depression, in patients undergoing gynecological oncology surgery. The addition of intraoperative acupuncture significantly reduced severe pain when compared with controls. Further research is needed to confirm these findings and better understand the impact of intraoperative acupuncture on postoperative pain.
Regular readers of my blog know only too well what I am going to say about this study.
Imagine you have a basket full of apples and your friend has the same plus a basket full of pears. Who do you think has more fruit?
Dumb question, you say?
Correct!
Just as dumb, it seems, as this study: therapy A and therapy B will always generate better outcomes than therapy B alone. But that does not mean that therapy A per se is effective. Because therapy A generates a placebo effect, it might just be that it has no effect beyond placebo. And that acupuncture can generate placebo effects has been known for a very long time; to verify this we need no RCT.
As I have so often pointed out, the A+B versus B study design never generates a negative finding.
This is, I fear, precisely the reason why this design is so popular in so-called alternative medicine (SCAM)! It enables promoters of SCAM (who are not as dumb as the studies they conduct) to pretend they are scientists testing their therapies in rigorous RCTs.
The most disappointing thing about all this is perhaps that more and more top journals play along with this scheme to mislead the public!
Brillia for Children is probably the most amazing homeopathic quackery I have ever encountered:
Uses: Enhance clarity, improve concentration of attention, reduce feelings of anxiety & stress, excitability, irritability and hyperactivity to improve attention, focus and mood regulation.
Active Ingredient: Lapine S-100 immune globulin mixture of homeopathic dilutions 12C, 30C and 50C.
Brillia is a unique combination of antibody science and homeopathic formulation. The active ingredient of Brillia is antibodies to the brain-specific S100 protein (S100B). This protein is an important regulator of many different intracellular and extracellular brain processes, e.g. various enzymes activities, calcium homeostasis, communication between neurons, etc. Since almost all mental and neurological diseases as well as temporal stress-induced conditions are accompanied by disturbance of the above-mentioned processes, especially communication between neurons, the normalization of these processes is considered to be a prospective way to treat people with such undesirable conditions. Brillia is an antibody conjugated to the S100B protein and does not alter the concentration of the S100B protein in the bloodstream. Brillia’s efficacy stems from its ability to regulate the activity of the S100B protein and does not alter its concentration. In order for a protein to have an effect in the body, it needs to bind to its target, such as an enzyme. Proteins have very specific conformations that ensure that only the correct protein binds to the correct target molecule. Once the protein correctly orients itself into the active site of the target molecule, this is when the protein causes an effect in the body. When Brillia binds to the S100B protein, the overall shape of the protein is altered, hindering its ability to bind to its target molecule and thereby controlling its activity in the body. In short, Brillia stops the S100B protein from acting in the body by changing its shape, consequently regulating levels of anxiety and hyperactivity.
PARENT TOOL | WATCH: DISCOVER BRILLIA
WATCH: WHY & HOW BRILLIA WORKS
Inactive Ingredients: Lactose monohydrate, magnesium stearate, microcrystalline cellulose. Does not contain artificial colors or artificial flavors.
Food Allergy Warning: This product contains lactose. Brillia is gluten free and nut free.
About active ingredients, the website tells us this:
Let’s start off with the active ingredient, registered with the FDA as Lapine S-100B immune globulin. Now we know this name can be intimidating, so we are going to break it down for you. Working backwards, “immune globulin” is just the “sciency” way of saying “antibody”, and don’t worry, we will get into what an antibody actually is in just a second. Next, “S-100B” is the name of the protein the antibody is designed to recognize in the body. Lastly, “Lapine” is just a descriptor of the origin of the antibody, just like the millions of other antibodies used each and every day in laboratories all across the world.
So, what exactly is an antibody? Antibodies are a naturally occurring protein and component of our immune system that are individually programmed to target a very specific protein, in the case of Brillia, the S-100B protein. It is important to understand that antibodies are one of the most specific and targeted molecules in our bodies, resulting in zero off-target effects — meaning that antibodies specifically look for and attach to their target only. This is why Brillia has no harmful side effects, because it only interacts with the S-100B protein. Not only does Brillia have absolutely zero side effects, it also has no contraindications with any other medications or supplements your child may be taking. This is due to Brillia’s extremely high level of target specificity, meaning that Brillia is so well targeted to the S-100B protein, it won’t even think about touching anything else in the body, including any other drugs or supplements.
Now that we know more about the active ingredient, let’s talk about its target, the S-100B protein.
The S-100B protein is a naturally occurring protein and is most prevalent in the brain. It is an important regulator of many processes such as regulating calcium levels and helping neurons communicate, but in our case, we care about how it influences the symptoms we mentioned earlier, such as anxiety and hyperactivity.
Given that S-100B protein influences these symptoms, it is quite intuitive that when the S-100B protein doesn’t do its job properly, these symptoms become more prevalent, and this is exactly what happens in those who suffer from anxiety, hyperactivity, stress and lack of focus.
So, what makes the S-100B protein, for a lack of a better term, mess up? The answer is quite simple, when the S-100B protein is overproduced or overactive, its activity becomes unnecessarily high, making it capable of causing these symptoms.
The firm even has something vaguely resembling evidence: a study that “shows that over the course of 12 weeks, Brillia had a significantly better effect on the severity of anxiety over those that did not take Brillia, therefore proving Brillia’s efficacy.” They show some actual results but the methods or source of the study are not disclosed. On Medline, I could not find it either. Therefore, I asked the firm to send it to me. This is the answer I got:
“Our studies were conducted in Europe and then published on our website. Please click here to view the full details found on our site.”
So, they have a study that they commissioned in Europe; it was done by researchers unnamed. The firm then put some data of it on their website. In other words:
- we don’t know who was responsible for the study;
- we cannot evaluate how rigorous it was;
- it has never been peer-reviewed;
- it is now being used for promotional purposes.
Personally, I don’t find this acceptable. In my view, this does not provide a legitimation to make far-reaching claims about the remedy. Until I have evidence to the contrary, I thus deem it safe to conclude that Brillia has no effect other than enriching the manufacturer.
It has been reported that a German consumer association, the ‘Verbraucherzentrale NRW’, has first cautioned the manufacturer MEDICE Arzneimittel Pütter GmbH & Co. and then sued them for misleading advertising statements. The advertisement in question gave the wrong impression that their homeopathic remedy MEDITONSIN would:
- for certain generate a health improvement,
- have no side effects,
- be superior to “chemical-synthetic drugs”.
The study used by the manufacturer in support of such claims was not convincing according to the Regional Court of Dortmund. The results of a “large-scale study with more than 1,000 patients” presented a pie chart indicating that 90% of the patients were satisfied or very satisfied with the effect of Meditonsin. However, this was only based on a “pharmacy-based observational study” with little scientific validity, as pointed out by the consumer association. Despite the lack of evidence, the manufacturer claimed that their study “once again impressively confirms the good efficacy and tolerability of Meditonsin® Drops”. The Regional Court of Dortmund disagreed with the manufacturer and agreed with the reasoning of the consumer association.
“It is not permitted to advertise with statements that give the false impression that a successful treatment can be expected with certainty, as suggested by the advertising for Meditonsin Drops,” emphasizes Gesa Schölgens, head of “Faktencheck Gesundheitswerbung,” a joint project of the consumer centers of North Rhine-Westphalia and Rhineland-Palatinate. According to German law, this is prohibited. In addition, the Regional Court of Dortmund considered consumers to be misled by the advertising because the false impression was created that no harmful side effects are to be expected when Meditonsin Drops are taken. The package insert of the drug lists several side effects, according to which there could even be an initial worsening of symptoms after taking the drug.
The claim of advantages of the “natural remedy” represented by the manufacturer in comparison with “chemical-synthetic medicaments, which merely suppress the symptoms”, was also deemed to be inadmissible. Such comparative advertising is inadmissible.
__________________________________
This ruling is, I think, interesting in several ways. The marketing claims of so-called alternative medicine (SCAM) products seem all too often not within the limits of the laws. One can therefore hope that this case might inspire many more legal cases against the inadmissible advertising of SCAMs.
You, the readers of this blog, have spoken!
The WORST PAPER OF 2022 competition has concluded with a fairly clear winner.
To fill in those new to all this: over the last year, I selected articles that struck me as being of particularly poor quality. I then published them with my comments on this blog. In this way, we ended up with 10 papers, and you had the chance to nominate the one that, in your view, stood out as the worst. Votes came in via comments to my last post about the competition and via emails directly to me. A simple count identified the winner.
It is PAUL VARNAS, DC, a graduate of the National College of Chiropractic, US. He is the author of several books and has taught nutrition at the National University of Health Sciences. His award-winning paper is entitled “What is the goal of science? ‘Scientific’ has been co-opted, but science is on the side of chiropractic“. In my view, it is a worthy winner of the award (the runner-up was entry No 10). Here are a few memorable quotes directly from Paul’s article:
- Most of what chiropractors do in natural health care is scientific; it just has not been proven in a laboratory at the level we would like.
- In many ways we are more scientific than traditional medicine because we keep an open mind and study our observations.
- Traditional medicine fails to be scientific because it ignores clinical observations out of hand.
- When you think about it, in natural health care we are much better at utilizing the scientific process than traditional medicine.
But I am surely doing Paul an injustice. To appreciate his article, please read his article in full.
I am especially pleased that this award goes to a chiropractor who informs us about the value of science and research. The two research questions that undoubtedly need answering more urgently than any other in the realm of chiropractic relate to the therapeutic effectiveness and risks of chiropractic. I just had a quick look in Medline and found an almost complete absence of research from 2022 into these two issues. This, I believe, makes the award for the WORST PAPER OF 2022 all the more meaningful.
PS
Yesterday, I wrote to Paul informing him about the good news (as yet, no reply). Once he provides me with a postal address, I will send him a copy of my recent book on chiropractic as his well-earned prize. I have also invited him to contribute a guest post to this blog. Watch this space!
This meta-analysis of randomized clinical trials (RCTs) was aimed at evaluating the effects of massage therapy in the treatment of postoperative pain.
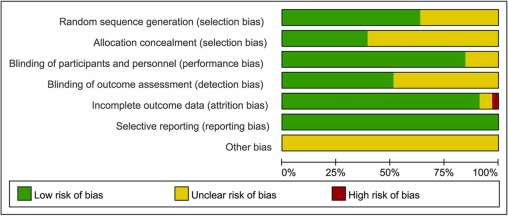
Three databases (PubMed, Embase, and Cochrane Central Register of Controlled Trials) were searched for RCTs published from database inception through January 26, 2021. The primary outcome was pain relief. The quality of RCTs was appraised with the Cochrane Collaboration risk of bias tool. The random-effect model was used to calculate the effect sizes and standardized mean difference (SMD) with 95% confidential intervals (CIs) as a summary effect. The heterogeneity test was conducted through I2. Subgroup and sensitivity analyses were used to explore the source of heterogeneity. Possible publication bias was assessed using visual inspection of funnel plot asymmetry.
The analysis included 33 RCTs and showed that MT is effective in reducing postoperative pain (SMD, -1.32; 95% CI, −2.01 to −0.63; p = 0.0002; I2 = 98.67%). A similarly positive effect was found for both short (immediate assessment) and long terms (assessment performed 4 to 6 weeks after the MT). Neither the duration per session nor the dose had a significant impact on the effect of MT, and there was no difference in the effects of different MT types. In addition, MT seemed to be more effective for adults. Furthermore, MT had better analgesic effects on cesarean section and heart surgery than orthopedic surgery.
The authors concluded that MT may be effective for postoperative pain relief. We also found a high level of heterogeneity among existing studies, most of which were compromised in the methodological quality. Thus, more high-quality RCTs with a low risk of bias, longer follow-up, and a sufficient sample size are needed to demonstrate the true usefulness of MT.
The authors discuss that publication bias might be possible due to the exclusion of all studies not published in English. Additionally, the included RCTs were extremely heterogeneous. None of the included studies was double-blind (which is, of course, not easy to do for MT). There was evidence of publication bias in the included data. In addition, there is no uniform evaluation standard for the operation level of massage practitioners, which may lead to research implementation bias.
Patients who have just had an operation and are in pain are usually thankful for the attention provided by carers. It might thus not matter whether it is provided by a massage or other therapist. The question is: does it matter? For the patient, it probably doesn’t; However, for making progress, it does, in my view.
In the end, we have to realize that, with clinical trials of certain treatments, scientific rigor can reach its limits. It is not possible to conduct double-blind, placebo-controlled studies of MT. Thus we can only conclude that, for some indications, massage seems to be helpful (and almost free of adverse effects).
This is also the conclusion that has been drawn long ago in some countries. In Germany, for instance, where I trained and practiced in my younger years, Swedish massage therapy has always been an accepted, conventional form of treatment (while exotic or alternative versions of massage therapy had no place in routine care). And in Vienna where I was chair of rehab medicine I employed about 8 massage therapists in my department.
Animals cannot consent to the treatments they are given when ill. This renders the promotion and use of SCAM in animals a tricky issue. This systematic review assessed the evidence for the clinical efficacy of 24 so-called alternative medicines (SCAMs) used in cats, dogs, and horses.
A bibliographic search, restricted to studies in cats, dogs, and horses, was performed on Web of Science Core Collection, CABI, and PubMed. Relevant articles were assessed for scientific quality, and information was extracted on study characteristics, species, type of treatment, indication, and treatment effects.
Of 982 unique publications screened, 42 were eligible for inclusion, representing 9 different SCAM therapies, which were
- aromatherapy,
- gold therapy,
- homeopathy,
- leeches (hirudotherapy),
- mesotherapy,
- mud,
- neural therapy,
- sound (music) therapy,
- vibration therapy.
For 15 predefined therapies, no study was identified. The risk of bias was assessed as high in 17 studies, moderate to high in 10, moderate in 10, low to moderate in four, and low in one study. In those studies where the risk of bias was low to moderate, there was considerable heterogeneity in reported treatment effects.
The authors concluded that the present systematic review has revealed significant gaps in scientific knowledge regarding the effects of a number of “miscellaneous” SCAM methods used in cats, dogs, and horses. For the majority of the therapies, no relevant scientific articles were retrieved. For nine therapies, some research documentation was available. However, due to small sample sizes, a lack of control groups, and other methodological limitations, few articles with a low risk of bias were identified. Where beneficial results were reported, they were not replicated in other independent studies. Many of the articles were in the lower levels of the evidence pyramid, emphasising the need for more high-quality research using precise methodologies to evaluate the potential therapeutic effects of these therapies. Of the publications that met the inclusion criteria, the majority did not have any scientific documentation of sufficient quality to draw any conclusion regarding their effect. Several of our observations may be translated into lessons on how to improve the scientific support for SCAM therapies. Crucial efforts include (a) a focus on the evaluation of therapies with an explanatory model for a mechanism of action accepted by the scientific community at large, (b) the use of appropriate control animals and treatments, preferably in randomized controlled trials, (c) high-quality observational studies with emphasis on control for confounding factors, (d) sufficient statistical power; to achieve this, large-scale multicenter trials may be needed, (e) blinded evaluations, and (f) replication studies of therapies that have shown promising results in single studies.
What the authors revealed in relation to homeopathy was particularly interesting, in my view. The included studies, with moderate risk of bias, such as homeopathic hypotensive treatment in dogs with early, stage two heart failure and the study on cats with hyperthyroidism, showed no differences between treated and non-treated animals. An RCT with osteoarthritic dogs showed a difference in three of the six variables (veterinary-assessed mobility, two force plate variables, an owner-assessed chronic pain index, and pain and movement visually analogous scales).
The results on homeopathy are supported by another systematic review of 18 RCTs, representing four species (including two dog studies) and 11 indications. The authors excluded generalized conclusions about the effect of certain homeopathic remedies or the effect of individualized homeopathy on a given medical condition in animals. In addition, a meta-analysis of nine homeopathy trials with a high risk of bias, and two studies with a lower risk of bias, concluded that there is very limited evidence that clinical intervention in animals using homeopathic remedies can be distinguished from similar placebo interventions.
In essence, this review confirms what I have been pointing out numerous times: SCAM for animals is not evidence-based, and this includes in particular homeopathy. It follows that its use in animals as an alternative to treatments with proven effectiveness borders on animal abuse.