Gosh, we in the UK needed that boost of jingoism (at least, if you are white, non-Jewish and equipped with a British passport)! But it’s all very well to rejoice at the news that we have a new little Windsor. With all the joy and celebration, we must not forget that the blue-blooded infant might be in considerable danger!
I am sure that chiropractors know what I am talking about.
KISS (Kinematic Imbalance due to Suboccipital Strain) is a term being used to describe a possible causal relation between imbalance in the upper neck joints in infants and symptoms like postural asymmetry, development of asymmetric motion patterns, hip problems, sleeping and eating disorders. Chiropractors are particularly fond of KISS. It is a problem that chiropractors tend to diagnose in new-borns.
This website explains further:
The kinematic imbalances brought on by the suboccipital strain at birth give rise to a concept in which symptoms and signs associated with the cervical spine manifest themselves into two easily recognizable clinical presentations. The leading characteristic is a fixed lateroflexion [called KISS I] or fixed retroflexion [KISS II]. KISS I may be associated with torticollis, asymmetry of the skull, C–scoliosis of the neck and trunk, asymmetry of the gluteal area and of the limbs, and retardation of the motor development of one side. KISS II, on the other hand, displays hyperextension during sleep, occipital flattening that may be asymmetrical, hunching of the shoulders, fixed supination of the arms, orofacial muscular hypotonia, failure to lift the trunk from a ventral position, and difficulty in breast feeding on one side. [34] The leading trademarks of both KISS I and KISS II are illustrated in Figure 1. [31]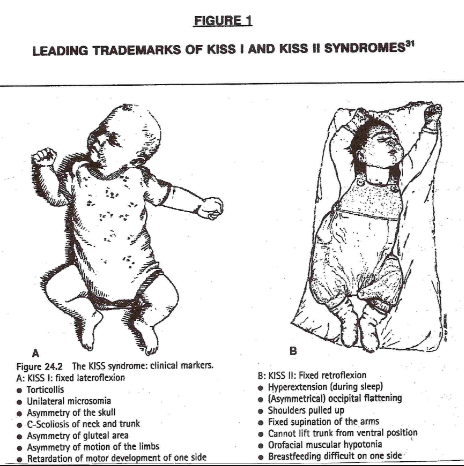
In essence, these birth experiences lay the groundwork for rationalizing the wisdom of providing chiropractic healthcare to the pediatric population…
END OF QUOTE
KISS must, of course, be treated with chiropractic spinal manipulation: the manual adjustment is the most common, followed by an instrument adjustment. This removes the neurological stress, re-balances the muscles and normal head position. Usually a dramatic change can be seen directly after the appropriate adjustment has been given…
Don’t frown! We all know that we can trust our chiropractors.
Evidence?
Do you have to insist on being a spoil-sport?
Alright, alright, the evidence tells a different story. A systematic review concluded that, given the absence of evidence of beneficial effects of spinal manipulation in infants and in view of its potential risks, manual therapy, chiropractic and osteopathy should not be used in infants with the KISS-syndrome, except within the context of randomised double-blind controlled trials.
And this means I now must worry for a slightly different reason: we all know that the new baby was born into a very special family – a family that seems to embrace every quackery available! I can just see the baby’s grandfather recruiting a whole range of anti-vaccinationists, tree-huggers, spoon-benders, homeopaths, faith healers and chiropractors to look after the new-born.
By Jove, one does worry about one’s Royals!
Have you ever wondered whether doctors who practice homeopathy are different from those who don’t.
Silly question, of course they are! But how do they differ?
Having practised homeopathy myself during my very early days as a physician, I have often thought about this issue. My personal (and not very flattering) impressions were noted in my memoir where I describe my experience working in a German homeopathic hospital:
… some of my colleagues used homeopathy and other alternative approaches because they could not quite cope with the often exceedingly high demands of conventional medicine. It is almost understandable that, if a physician was having trouble comprehending the multifactorial causes and mechanisms of disease and illness, or for one reason or another could not master the equally complex process of reaching a diagnosis or finding an effective therapy, it might be tempting instead to employ notions such as dowsing, homeopathy or acupuncture, whose theoretical basis, unsullied by the inconvenient absolutes of science, was immeasurably more easy to grasp.
Some of my colleagues in the homeopathic hospital were clearly not cut out to be “real” doctors. Even a very junior doctor like me could not help noticing this somewhat embarrassing fact…
But this is anecdote and not evidence!
So, where is the evidence?
It was published last week and made headlines in many UK daily papers.
Our study was aimed at finding out whether English GP practices that prescribe any homeopathic preparations might differ in their prescribing of other drugs. We identified practices that made any homeopathy prescriptions over six months of data. We measured associations with four prescribing and two practice quality indicators using multivariable logistic regression.
Only 8.5% of practices (644) prescribed homeopathy between December 2016 and May 2017. Practices in the worst-scoring quartile for a composite measure of prescribing quality were 2.1 times more likely to prescribe homeopathy than those in the best category. Aggregate savings from the subset of these measures where a cost saving could be calculated were also strongly associated. Of practices spending the most on medicines identified as ‘low value’ by NHS England, 12.8% prescribed homeopathy, compared to 3.9% for lowest spenders. Of practices in the worst category for aggregated price-per-unit cost savings, 12.7% prescribed homeopathy, compared to 3.5% in the best category. Practice quality outcomes framework scores and patient recommendation rates were not associated with prescribing homeopathy.
We concluded that even infrequent homeopathy prescribing is strongly associated with poor performance on a range of prescribing quality measures, but not with overall patient recommendation or quality outcomes framework score. The association is unlikely to be a direct causal relationship, but may reflect underlying practice features, such as the extent of respect for evidence-based practice, or poorer stewardship of the prescribing budget.
Since our study was reported in almost all of the UK newspapers, it comes as no surprise that, in the interest of ‘journalistic balance’, homeopaths were invited to give their ‘expert’ opinions on our work.
Margaret Wyllie, head of the British Homeopathic Association, was quoted commenting: “This is another example of how real patient experience and health outcomes are so often discounted, when in actuality they should be the primary driver for research to improve our NHS services. This study provides no useful evidence about homeopathy, or about prescribing, and gives absolutely no data that can improve the health of people in the UK.”
The Faculty of Homeopathy was equally unhappy about our study and stated: “The study did not include any measures of patient outcomes, so it doesn’t tell us how the use of homeopathy in English general practice correlates with patients doing well or badly, nor with how many drugs they use.”
Cristal Summer from the Society of Homeopathy said that our research was just a rubbish bit of a study.
Peter Fisher, the Queen’s homeopath and the president of the Faculty of Homeopathy, stated: “We don’t know if these measures correlate with what matters to patients – whether they get better and have side-effects.”
A study aimed at determining whether GP practices that prescribe homeopathic preparations differ in their prescribing habits from those that do not prescribe homeopathics can hardly address these questions, Peter. A test of washing machines can hardly tell us much about the punctuality of trains. And an investigation into the risks of bungee jumping will not inform us about the benefits of regular exercise. Call me biased, but to me these comments indicate mainly one thing: HOMEOPATHS SEEM TO HAVE GREAT DIFFICULTIES UNDERSTANDING SCIENTIFIC PAPERS.
I much prefer the witty remarks of Catherine Bennett in yesterday’s Observer: Homeopath-GPs, naturally, have mustered in response and challenge Goldacre’s findings, with a concern for methodology that could easily give the impression that there is some evidential basis for their parallel system, beyond the fact that the Prince of Wales likes it. In fairness to Charles, his upbringing is to blame. But what is the doctors’ excuse?
Amongst all the implausible treatments to be found under the umbrella of ‘alternative medicine’, Reiki might be one of the worst, i. e. least plausible and outright bizarre (see for instance here, here and here). But this has never stopped enthusiasts from playing scientists and conducting some more pseudo-science.
This new study examined the immediate symptom relief from a single reiki or massage session in a hospitalized population at a rural academic medical centre. It was designed as a retrospective analysis of prospectively collected data on demographic, clinical, process, and quality of life for hospitalized patients receiving massage therapy or reiki. Hospitalized patients requesting or referred to the healing arts team received either a massage or reiki session and completed pre- and post-therapy symptom questionnaires. Differences between pre- and post-sessions in pain, nausea, fatigue, anxiety, depression, and overall well-being were recorded using an 11-point Likert scale.
Patients reported symptom relief with both reiki and massage therapy. Reiki improved fatigue and anxiety more than massage. Pain, nausea, depression, and well being changes were not different between reiki and massage encounters. Immediate symptom relief was similar for cancer and non-cancer patients for both reiki and massage therapy and did not vary based on age, gender, length of session, and baseline symptoms.
The authors concluded that reiki and massage clinically provide similar improvements in pain, nausea, fatigue, anxiety, depression, and overall well-being while reiki improved fatigue and anxiety more than massage therapy in a heterogeneous hospitalized patient population. Controlled trials should be considered to validate the data.
Don’t I just adore this little addendum to the conclusions, “controlled trials should be considered to validate the data” ?
The thing is, there is nothing to validate here!
The outcomes are not due to the specific effects of Reiki or massage; they are almost certainly caused by:
- the extra attention,
- the expectation of patients,
- the verbal or non-verbal suggestions of the therapists,
- the regression towards the mean,
- the natural history of the condition,
- the concomitant therapies administered in parallel,
- the placebo effect,
- social desirability.
Such pseudo-research only can only serve one purpose: to mislead (some of) us into thinking that treatments such as Reiki might work.
What journal would be so utterly devoid of critical analysis to publish such unethical nonsense?
Ahh … it’s our old friend the Journal of Alternative and Complementary Medicine
Say no more!
Osteopathy is an odd alternative therapy. In many parts of the world it is popular; the profession differs dramatically from country to country; and there is not a single condition for which we could say that osteopathy out-performs other options. No wonder then that osteopaths would be more than happy to find a new area where they could practice their skills.
Perhaps surgical care is such an area?
The aim of this systematic review was to present an overview of published research articles within the subject field of osteopathic manipulative treatment (OMT) in surgical care. The authors evaluated peer-reviewed research articles published in osteopathic journals during the period 1990 to 2017. In total, 10 articles were identified.
Previous research has been conducted within the areas of abdominal, thoracic, gynecological, and/or orthopedic surgery. The studies included outcomes such as pain, analgesia consumption, length of hospital stay, and range of motion. Heterogeneity was identified in usage of osteopathic techniques, treatment duration, and occurrence, as well as in the osteopath’s experience.
The authors concluded that despite the small number of research articles within this field, both positive effects as well as the absence of such effects were identified. Overall, there was a heterogeneity concerning surgical contexts, diagnoses, signs and symptoms, as well as surgical phases in current interprofessional osteopathic publications. In this era of multimodal surgical care, the authors concluded, there is an urgent need to evaluate OMT in this context of care and with a proper research approach.
This is an odd conclusion, if there ever was one!
The facts are fairly straight forward:
- Osteopaths would like to expand into the area of surgical care [mainly, I suspect, because it would be good for business]
- There is no plausible reason why OMT should be beneficial in this setting.
- Osteopaths are not well-trained for looking after surgical patients.
- Physiotherapists, however, are and therefore there is no need for osteopaths on surgical wards.
- The evidence is extremely scarce.
- The available trials are of poor quality.
- Their results are contradictory.
- Therefore there is no reliable evidence to show that OMT is effective.
The correct conclusion of this review should thus be as follows:
THE AVAILABLE EVIDENCE FAILS TO SHOW EFFECTIVENESS OF OMT. THEREFORE THIS APPROACH CANNOT BE RECOMMENDED.
End of story.
I have often criticised papers published by chiropractors.
Not today!
This article is excellent and I therefore quote extensively from it.
The objective of this systematic review was to investigate, if there is any evidence that spinal manipulations/chiropractic care can be used in primary prevention (PP) and/or early secondary prevention in diseases other than musculoskeletal conditions. The authors conducted extensive literature searches to locate all studies in this area. Of the 13.099 titles scrutinized, 13 articles were included (8 clinical studies and 5 population studies). They dealt with various disorders of public health importance such as diastolic blood pressure, blood test immunological markers, and mortality. Only two clinical studies could be used for data synthesis. None showed any effect of spinal manipulation/chiropractic treatment.
The authors concluded that they found no evidence in the literature of an effect of chiropractic treatment in the scope of PP or early secondary prevention for disease in general. Chiropractors have to assume their role as evidence-based clinicians and the leaders of the profession must accept that it is harmful to the profession to imply a public health importance in relation to the prevention of such diseases through manipulative therapy/chiropractic treatment.
In addition to this courageous conclusion (the paper is authored by a chiropractor and published in a chiro journal), the authors make the following comments:
Beliefs that a spinal subluxation can cause a multitude of diseases and that its removal can prevent them is clearly at odds with present-day concepts, as the aetiology of most diseases today is considered to be multi-causal, rarely mono-causal. It therefore seems naïve when chiropractors attempt to control the combined effects of environmental, social, biological including genetic as well as noxious lifestyle factors through the simple treatment of the spine. In addition, there is presently no obvious emphasis on the spine and the peripheral nervous system as the governing organ in relation to most pathologies of the human body.
The ‘subluxation model’ can be summarized through several concepts, each with its obvious weakness. According to the first three, (i) disturbances in the spine (frequently called ‘subluxations’) exist and (ii) these can cause a multitude of diseases. (iii) These subluxations can be detected in a chiropractic examination, even before symptoms arise. However, to date, the subluxation has been elusive, as there is no proof for its existence. Statements that there is a causal link between subluxations and various diseases should therefore not be made. The fourth and fifth concepts deal with the treatment, namely (iv) that chiropractic adjustments can remove subluxations, (v) resulting in improved health status. However, even if there were an improvement of a condition following treatment, this does not mean that the underlying theory is correct. In other words, any improvement may or may not be caused by the treatment, and even if so, it does not automatically validate the underlying theory that subluxations cause disease…
Although at first look there appears to be a literature on this subject, it is apparent that most authors lack knowledge in research methodology. The two methodologically acceptable studies in our review were found in PubMed, whereas most of the others were identified in the non-indexed literature. We therefore conclude that it may not be worthwhile in the future to search extensively the non-indexed chiropractic literature for high quality research articles.
One misunderstanding requires some explanations; case reports are usually not considered suitable evidence for effect of treatment, even if the cases relate to patients who ‘recovered’ with treatment. The reasons for this are multiple, such as:
- Individual cases, usually picked out on the basis of their uniqueness, do not reflect general patterns.
- Individual successful cases, even if correctly interpreted must be validated in a ‘proper’ research design, which usually means that presumed effect must be tested in a properly powered and designed randomized controlled trial.
- One or two successful cases may reflect a true but very unusual recovery, and such cases are more likely to be written up and published as clinicians do not take the time to marvel over and spend time on writing and publishing all the other unsuccessful treatment attempts.
- Recovery may be co-incidental, caused by some other aspect in the patient’s life or it may simply reflect the natural course of the disease, such as natural remission or the regression towards the mean, which in human physiology means that low values tend to increase and high values decrease over time.
- Cases are usually captured at the end because the results indicate success, meaning that the clinical file has to be reconstructed, because tests were used for clinical reasons and not for research reasons (i.e. recorded by the treating clinician during an ordinary clinical session) and therefore usually not objective and reproducible.
- The presumed results of the treatment of the disease is communicated from the patient to the treating clinician and not to a third, neutral person and obviously this link is not blinded, so the clinician is both biased in favour of his own treatment and aware of which treatment was given, and so is the patient, which may result in overly positive reporting. The patient wants to please the sympathetic clinician and the clinician is proud of his own work and overestimates the results.
- The long-term effects are usually not known.
- Further, and most importantly, there is no control group, so it is impossible to compare the results to an untreated or otherwise treated person or group of persons.
Nevertheless, it is common to see case reports in some research journals and in communities with readers/practitioners without a firmly established research culture it is often considered a good thing to ‘start’ by publishing case reports.
Case reports are useful for other reasons, such as indicating the need for further clinical studies in a specific patient population, describing a clinical presentation or treatment approach, explaining particular procedures, discussing cases, and referring to the evidence behind a clinical process, but they should not be used to make people believe that there is an effect of treatment…
For groups of chiropractors, prevention of disease through chiropractic treatment makes perfect sense, yet the credible literature is void of evidence thereof. Still, the majority of chiropractors practising this way probably believe that there is plenty of evidence in the literature. Clearly, if the chiropractic profession wishes to maintain credibility, it is time seriously to face this issue. Presently, there seems to be no reason why political associations and educational institutions should recommend spinal care to prevent disease in general, unless relevant and acceptable research evidence can be produced to support such activities. In order to be allowed to continue this practice, proper and relevant research is therefore needed…
All chiropractors who want to update their knowledge or to have an evidence-based practice will search new information on the internet. If they are not trained to read the scientific literature, they might trust any article. In this situation, it is logical that the ‘believers’ will choose ‘attractive’ articles and trust the results, without checking the quality of the studies. It is therefore important to educate chiropractors to become relatively competent consumers of research, so they will not assume that every published article is a verity in itself…
END OF QUOTES
YES, YES YES!!!
I am so glad that some experts within the chiropractic community are now publishing statements like these.
This was long overdue.
How was it possible that so many chiropractors so far failed to become competent consumers of research?
Do they and their professional organisations not know that this is deeply unethical?
Actually, I fear they do and did so for a long time.
Why then did they not do anything about it ages ago?
I fear, the answer is as easy as it is disappointing:
If chiropractors systematically trained to become research-competent, the chiropractic profession would cease to exist; they would become a limited version of physiotherapists. There is simply not enough positive evidence to justify chiropractic. In other words, as chiropractic wants to survive, it has little choice other than remaining ignorant of the current best evidence.
Most diabetics need life-long medication. Understandably, this makes many fed-up, and some think that perhaps natural remedies might be a less harmful, less intrusive way to control their condition. They don’t have to look far to find an impressively large choice.
This article in the Canadian Journal of Diabetes was aimed at reviewing CAM, including natural health products (NHP) and others, such as yoga, acupuncture, tai chi and reflexology, that have been studied for the prevention and treatment of diabetes and its complications. It claims that, in adults with type 2 diabetes, the following NHP have been shown to lower glycated hemoglobin (A1C) by at least 0.5% in randomized controlled trials lasting at least 3 months:
Ayurveda polyherbal formulation
Citrullus colocynthis
Coccinia cordifolia
Eicosapentaenoic acid
Ganoderma lucidum
Ginger (Zingiber officinale)
Gynostemma pentaphyllum
Hintonia latiflora
Lichen genus Cladonia BAFS “Yagel-Detox”
Marine collagen peptides
Nettle (Urtica dioica)
Oral aloe vera
Pterocarpus marsupium (vijayasar)
Salacia reticulate
Scoparia dulcis porridge
Silymarin
Soybean-derived pinitol extract
Touchi soybean extract
Traditional Chinese medicine herbs:
Berberine
Fructus Mume
Gegen Qinlian Decoction (GQD)
Jianyutangkang (JYTK) with metformin
Jinlida with metformin
Sancaijiangtang
Shen-Qi-Formula (SQF) with insulin
Tang-Min-Ling-Wan (TM81)
Xiaoke (contains glyburide)
Zishentongluo (ZSTL)
Trigonella foenum-graecum (fenugreek)
Even though the authors caution that these remedies should not be recommended for routine use, I fear that such lists do motivate diabetics to give them a try. If they do, the outcome could be that:
- Nothing at all happens other than the patient wasting some money on useless remedies. The clinical trials on which the above list is based are usually so flimsy that their findings are next to meaningless and quite possibly false-positive.
- The patient might, if the remedy does affect blood sugar levels, develop hypoglycaemia. If severe, this could be life-threatening.
- The patient might trust in a natural remedy and thus discontinue the prescribed anti-diabetic medication. In this case, she could develop hyperglycaemia. If severe, this could be life-threatening.
It seems obvious that none of the possible outcomes are in the patients’ interest. I fear that it is dangerous to tempt diabetics with the possibility that a natural remedy. Even if such treatments did work, they are not well-researched, unreliable and do not have sufficiently large effects (a 0.5% decrease of glycated haemoglobin is hardly impressive) to represent realistic options.
I hear this argument so regularly that it might be worth analysing it (yet again) a bit closer.
It is used with the deepest of convictions by proponents of all sorts of quackery who point out that science does not know or explain everything – and certainly not their (very special) therapy. Science is just not sophisticated enough, they say; in fact, a few years ago, it could not even explain how Aspirin works. And just like Aspirin, their very special therapy – let’s call it energy healing (EH) for the sake of this post – does definitely and evidently work. There even is ample proof:
- Patients get better after using EH, and surely patients don’t lie.
- Patients pay for EH, and who would pay for something that does not work?
- EH has survived hundreds of years, and ineffective therapies don’t.
- EH practitioners have tons of experience and therefore know best.
- They are respected by very important people and organisations.
- EH is even reimbursed by some insurance companies.
You have all heard the argument, I’m sure.
How to respond?
The ‘proofs’ listed above are simply fallacies; as such they do not need more detailed discussions, I hope.
But how can we refute the notion that science is not yet sufficiently advanced to explain EH?
The simplest approach might be to explain that science has already tested EH and found it to be ineffective. There really is nothing more to say. And the often-quoted example of Aspirin does clearly not wash. True, a few decades ago, we did not know how it worked. But we always knew that it worked because we conducted clinical trials, and they generated positive results. These findings we the main reasons why scientists wanted to find out how it works, and eventually they did (and even got a Nobel Prize for it). Had the clinical trials not shown effectiveness, nobody would have been interested in alleged mechanisms of action.
With EH, things are different. Rigorous clinical trials of EH have been conducted, and the totality of this evidence fails to show that EH works. Therefore, chasing after a mechanism of action would be silly and wasteful. It’s true, science cannot explain EH, but this is not because it is not yet sophisticated enough; it is because there is nothing to explain. EH has been disproven, and waffling about ‘science is not yet able to explain it’ is either a deliberate lie or a serious delusion.
So far so good. But what if EH had not been submitted to clinical trials?
In such cases, the above line of argument would not work very well.
For instance, as far as I know, there is not a single rigorous clinical trial of crystal healing (CH). Does that mean that perhaps CH-proponents are correct when claiming that it does evidently work and science simply cannot yet understand how?
No, I don’t think so.
Like most of the untested alternative therapies, CH is not based on plausible assumptions. In fact, the implausibility of the underlying assumptions is the reason why such treatments have not and probably never will be submitted to rigorous clinical trials. Why should anyone waste his time and our money running expensive tests on something that is so extremely unlikely? Arguably doing so would even be unethical.
With highly implausible therapies we need no trials, and we do not need to fear that science is not yet sufficiently advance to explain them. In fact, science is sufficiently advanced to be certain that there can be no explanation that is in line with the known laws of nature.
Sadly, some truly deluded fans of CH might still not be satisfied and respond to our reasoning that we need a ‘paradigm shift’. They might say that science cannot explain CH because it is stuck in the straightjacket of an obsolete paradigm which does not cater for phenomena like CH.
Yet this last and desperate attempt of the fanatics is not a logical refuge. Paradigm shifts are not required because some quack thinks so, they are needed only if data have been emerging that cannot possibly be explained within the current paradigm. But this is never the case in alternative medicine. We can explain all the experience of advocates, positive results of researchers and ‘miracle’ cures of patients that are being reported. We know that the experiences are real, but are sure that their explanations of the experience are false. They are not due to the treatment per se but to other phenomena such as placebo effects, natural history, regression towards the mean, spontaneous recovery, etc.
So, whichever way we turn things, and whichever way enthusiasts of alternative therapies twist them, their argument that ‘SCIENCE IS NOT YET ABLE TO EXPLAIN’ is simply wrong.
Generally speaking, Cochrane reviews provide the best (most rigorous, transparent and independent) evidence on the effectiveness of medical or surgical interventions. It is therefore important to ask what they tell us about homeopathy. In 2010, I did exactly that and published it as an overview of the current best evidence. At the time, there were 6 relevant Cochrane reviews. They covered the following conditions: cancer, attention-deficit hyperactivity disorder, asthma, dementia, influenza and induction of labour. And their results were clear: they did not show that homeopathic medicines have effects beyond placebo.
Now a further Cochrane review has been published.
Does it change this situation?
This systematic review assessed the effectiveness and safety of oral homeopathic medicinal products compared with placebo or conventional therapy to prevent and treat acute respiratory tract infections (ARTIs) in children. The researchers conducted extensive literature searches, checked references, and contacted study authors to identify additional studies. They included all double-blind, randomised controlled trials (RCTs) or double-blind cluster-RCTs comparing oral homeopathy medicinal products with identical placebo or self selected conventional treatments to prevent or treat ARTIs in children aged 0 to 16 years.
Eight RCTs of 1562 children receiving oral homeopathic medicinal products or a control treatment (placebo or conventional treatment) for upper respiratory tract infections (URTIs). Four treatment studies examined the effect on recovery from URTIs, and four studies investigated the effect on preventing URTIs after one to three months of treatment and followed up for the remainder of the year. Two treatment and two prevention studies involved homeopaths individualising treatment for children. The other studies used predetermined, non-individualised treatments. All studies involved highly diluted homeopathic medicinal products.
Several key limitations to the included studies were identified, in particular methodological inconsistencies and high attrition rates, failure to conduct intention-to-treat analysis, selective reporting, and apparent protocol deviations. The authors deemed three studies to be at high risk of bias in at least one domain, and many had additional domains with unclear risk of bias. Three studies received funding from homeopathy manufacturers; one reported support from a non-government organisation; two received government support; one was co-sponsored by a university; and one did not report funding support.
Methodological inconsistencies and significant clinical and statistical heterogeneity precluded robust quantitative meta-analysis. Only four outcomes were common to more than one study and could be combined for analysis. Odds ratios (OR) were generally small with wide confidence intervals (CI), and the contributing studies found conflicting effects, so there was little certainty that the efficacy of the intervention could be ascertained.
All studies assessed as at low risk of bias showed no benefit from oral homeopathic medicinal products; trials at uncertain and high risk of bias reported beneficial effects. The authors found low-quality evidence that non-individualised homeopathic medicinal products confer little preventive effect on ARTIs (OR 1.14, 95% CI 0.83 to 1.57). They also found low-quality evidence from two individualised prevention studies that homeopathy has little impact on the need for antibiotic usage (N = 369) (OR 0.79, 95% CI 0.35 to 1.76).
The authors also assessed adverse events, hospitalisation rates and length of stay, days off school (or work for parents), and quality of life, but were not able to pool data from any of these secondary outcomes. There is insufficient evidence from two pooled individualised treatment studies (N = 155) to determine the effect of homeopathy on short-term cure (OR 1.31, 95% CI 0.09 to 19.54; very low-quality evidence) and long-term cure rates (OR 1.01, 95% CI 0.10 to 9.96; very low-quality evidence). Adverse events were reported inconsistently; however, serious events were not reported. One study found an increase in the occurrence of non-severe adverse events in the treatment group.
The authors concluded that pooling of two prevention and two treatment studies did not show any benefit of homeopathic medicinal products compared to placebo on recurrence of ARTI or cure rates in children. We found no evidence to support the efficacy of homeopathic medicinal products for ARTIs in children. Adverse events were poorly reported, so conclusions about safety could not be drawn.
In their paper, the authors state that “there are no established explanatory models for how highly diluted homeopathic medicinal products might work. For this reason, homeopathy remains highly controversial because the key concepts governing this form of medicine are not consistent with the established laws of conventional therapeutics.” In other words, there is no reason why highly diluted homeopathic remedies should work. Yet, remarkably, when asked what conditions responds best to homeopathy, most homeopaths would probably include ARTI of children.
The authors also point out that “The results of this review are consistent with all previous systematic reviews on homeopathy. Funders and study investigators contemplating any further research in this area need to consider whether further research will advance our knowledge, given the uncertain mechanism of action and debate about how the lack of a measurable dose can make them effective. The studies we identified did not use a uniform approach to choosing and measuring outcomes or assigning appropriate time points for outcome measurement. The use of validated symptom scales would facilitate future meta-analyses. It is unclear if there is any benefit from individualised (classical) homeopathy over the use of commercially available products.”
Even though I agree with the authors on most of their views and comment their excellent work, I would be more outspoken regarding the need of further research. In my view, it would be a foolish, wasteful and therefore unethical activity to fund, plan or conduct further research in this area.
The UK ‘COLLEGE OF MEDICINE’ has recently (and very quietly) renamed itself; it now is THE COLLEGE OF MEDICINE AND INTEGRATED HEALTH (COMIH). This takes it closer to its original intentions of being the successor of the PRINCE OF WALES FOUNDATION FOR INTEGRATED MEDICINE (PWFIM), the organisation that had to be shut down amidst charges of fraud and money-laundering. Originally, the name of COMIH was to be COLLEGE OF INTEGRATED HEALTH (as opposed to disintegrated health?, I asked myself at the time).
Under the leadership of Dr Michael Dixon, OBE (who also led the PWFIM into its demise), the COMIH pursues all sots of activities. One of them seems to be publishing ‘cutting-edge’ articles.
A recent and superb example is on the fascinating subject of ‘holistic dentistry‘:
START OF QUOTE
Professor Sonia Williams … explores how integrated oral health needs to consider the whole body, not just the dentition…
Complementary and alternative approaches can also be considered as complementary to ‘mainstream’ care, with varying levels of evidence cited for their benefit.
Dental hypnosis (British Society of Medical and Dental Hypnosis) can help support patients including those with dental phobia or help to reduce pain experience during treatment.
Acupuncture in dentistry (British Society of Dental Acupuncture) can, for instance, assist with pain relief and allay the tendency to vomit during dental care. There is also a British Homeopathic Dental Association.
For the UK Faculty of General Dental Practitioners, holistic dentistry refers to strengthening the link between general and oral health.
For some others, the term also represents an ‘alternative’ form of dentistry, which may concern itself with the avoidance and elimination of ‘toxic’ filling materials, perceived potential harm from fluoride and root canal treatments and with treating dental malocclusion to put patients back in ‘balance’.
In the USA, there is a Holistic Dental Association, while in the UK, there is the British Society for Mercury-free Dentistry. Unfortunately the evidence base for many of these procedures is weak.
Nevertheless, pressure to avoid mercury in dental restorative materials is becoming mainstream.
In summary, integrated health and care in dentistry can mean different things to different people. The weight of evidence supports the contention that the mouth is an integral part of the body and that attention to the one without taking account of the other can have adverse consequences.
END OF QUOTE
Do I get this right? ‘Holistic dentistry’ in the UK means the recognition that my mouth belongs to my body, and the adoption of a few dubious treatments with w ‘weak’ evidence base?
Well, isn’t this just great? I had no idea that my mouth belongs to my body. And clearly the non-holistic dentists in the UK are oblivious to this fact as well. I am sooooooo glad we got this cleared up.
Thanks COMIH!!!
And what about the alternative treatments used by holistic dentists?
The British Society of Medical and Dental Hypnosis (Scotland) inform us on their website that a trained medical and dental hypnotherapists can help you to deal with a large variety of challenges that you face in your everyday life e.g.
| Asthma | Migraines |
| Anxiety & Stress | Smoking Cessation |
| Dental Problems | Insomnia |
| Weight Problems | Psychosexual Disorders |
| Depression | Pain Management |
| Irritable Bowel | And many other conditions |
I hasten to add that, for most of these conditions, the evidence fails to support the claims.
The British Society of Dental Acupuncture claim on their website that the typical conditions that may be helped by acupuncture are:
- TMJ (jaw joint) problems
- Facial pain
- Muscle spasm in the head and neck
- Stress headaches & Migraine
- Rhinitis & sinusitis
- Gagging
- Dry mouth problems
- Post-operative pain
- Dental anxiety
I hasten to add that, for most of these conditions, the evidence fails to support the claims.
The British Homeopathic Dental Association claim on their website that studies have shown improved bone healing around implants with Symphytum and reduced discomfort and improved healing time with ulcers and beneficial in oral lichen planus.
I hasten to add that none of these claims are not supported by sound evidence.
The COMIH article is entitled “The mouth reflects whole body health – but what does integrated care mean for dentists?’ So, what does it mean? Judging from this article, it means an amalgam (pun intended) of platitudes, bogus claims and outright nonsense.
Pity that they did not change their name to College of Medicine and Integrated Care – I could have abbreviated it as COMIC!
Daniel P Wirth used to be THE star amongst researchers and proponents of paranormal healing. About 15 years ago, there was nobody who had published more studies of it than Wirth. The extraordinary phenomenon was not just the number of studies, but also the fact that these trials all reported positive findings.
At the time, this puzzled me a lot. I had conducted two trials of paranormal healing myself; and, in both, cases the results had turned out to be negative (see here and here). Thus I made several attempts to contact Wirth or his co-authors hoping to better understand the phenomenon. Yet I never received a reply and became increasingly suspicious of their research.
In 2004, it was announced that Wirth together with one of his co-workers had been arrested and later imprisoned for fraud. Several of his 20 papers published in various journals were subsequently withdrawn. I remember writing to several journal editors myself urging them to follow suit so that, in future, the literature would not be polluted with dubious studies. Eventually, we all forgot about the whole story.
Recently, I took a renewed interest in paranormal healing. To my surprise, I found that several of Wirth’s papers are still listed on Medline:
Cha KY, Wirth DP.
J Reprod Med. 2001 Sep;46(9):781-7. Erratum in: J Reprod Med. 2004 Oct;49(10):100A. Lobo, RA [removed].
PMID: 11584476
2 Multisite electromyographic analysis of therapeutic touch and qigong therapy.
Wirth DP, Cram JR, Chang RJ.
J Altern Complement Med. 1997 Summer;3(2):109-18.
PMID: 9395700
3 Multisite surface electromyography and complementary healing intervention: a comparative analysis.
Wirth DP, Cram JR.
J Altern Complement Med. 1997 Winter;3(4):355-64.
PMID: 9449057
4 Wound healing and complementary therapies: a review.
Wirth DP, Richardson JT, Eidelman WS.
J Altern Complement Med. 1996 Winter;2(4):493-502. Review.
PMID: 9395679
5 The significance of belief and expectancy within the spiritual healing encounter.
Wirth DP.
Soc Sci Med. 1995 Jul;41(2):249-60.
PMID: 7667686
6 Complementary healing intervention and dermal wound reepithelialization: an overview.
Wirth DP.
Int J Psychosom. 1995;42(1-4):48-53.
PMID: 8582812
7 The psychophysiology of nontraditional prayer.
Wirth DP, Cram JR.
Int J Psychosom. 1994;41(1-4):68-75.
PMID: 7843870
8 Complementary healing therapies.
Wirth DP, Barrett MJ.
Int J Psychosom. 1994;41(1-4):61-7.
PMID: 7843869
9 Multi-site electromyographic analysis of non-contact therapeutic touch.
Wirth DP, Cram JR.
Int J Psychosom. 1993;40(1-4):47-55.
PMID: 8070986
____________________________________________________________________________
Of these 9 papers, only the first one in the list carries a note indicating that the paper has been removed. In other words, 8 of Wirth’s articles are still available as though they are fine and proper.
The situation is even worse on ‘Research Gate’. Here we find all of the following articles with no indication of any suspicion of fraud:
———-
KY Cha · · RA Lobo
Abstract: To assess the potential effect of intercessory prayer (IP) on pregnancy rates in women being treated with in vitro fertilization-embryo transfer (IVF-ET). Prospective, double-blind, randomized clinical trial in which patients and providers were not informed about the intervention. Statisticians and investigators were masked until all the data had been collected and clinical outcomes were known. The setting was an IVF-ET program at Cha Hospital, Seoul, Korea. IP was carried out by prayer…
Article · Oct 2001 · The Journal of reproductive medicine
———-
Article: Exploring Further Menstruation and Spiritual Healing
Daniel P. Wirth
Article · Apr 1997 · Alternative and Complementary Therapies
———-
Article: Multisite Surface Electromyography and Complementary Healing Intervention: A Comparative Analysis
Daniel P. Wirth · Jeffrey R. Cram
Abstract: A comparative analysis was conducted on a series of three experimental studies that examined the effect of various local and nonlocal (distant) complementary healing methods on multisite surface electromyographic (sEMG) and autonomic measures. The series concentrated sEMG electrode placement on specific neuromuscular paraspinal centers (cervical [C4], thoracic [T6], and lumbar [L3]), along with the frontalis region, due to the fact that these sites corresponded to the location of individual…
Article · Feb 1997 · The Journal of Alternative and Complementary Medicine
———-
Article: Multisite Electromyographic Analysis of Therapeutic Touch and Qigong Therapy
Daniel P. Wirth · Jeffrey R. Cram · Richard J. Chang
Abstract: The influence of complementary healing treatment on paraspinal electromagnetic activity at specific neuromuscular sites was examined in an exploratory pilot study that used a multisite surface electromyographic (sEMG) assessment procedure. The study was a replication and extension of previous research that indicated that complementary healing had a significant effect in normalizing the activity of the “end organ” for the central nervous system (CNS). Multisite sEMG electrodes were placed on…
Article · Feb 1997 · The Journal of Alternative and Complementary Medicine
———-
Article: Non-contact Therapeutic Touch intervention and full thickness cutaneous wounds: A replication
Daniel P Wirth · Joseph T. Richardson · Robert D. Martinez · William S. Eidelman · Maria E.L. Lopez
Abstract: The study described here utilized a randomized double-blind methodological protocol in order to examine the effect of non-contact therapeutic touch (NCTT) on the healing rate of full-thickness human dermal wounds. This study is the fifth experiment in a series of extensions based on the original research design, and is an exact methodological replication of the second study in the series. Thirty-two healthy subjects were randomly divided into treatment and control groups and biopsies were…
Article · Oct 1996 · Complementary Therapies in Medicine
———-
Article: Wound Healing and Complementary Therapies: A Review
Daniel P. Wirth · Joseph T. Richardson · William S. Eidelman
Abstract: A series of five innovative experiments conducted by Wirth et al. which examined the effect of various complementary healing interventions on the reepithelialization rate of full thickness human dermal wounds was assessed as to specific methodological and related factors. The treatment interventions utilized in the series included experimental derivatives of the Therapeutic Touch (TT), Reiki, LeShan, and Intercessory Prayer techniques. The results of the series indicated statistical…
Article · Feb 1996 · The Journal of Alternative and Complementary Medicine
———-
Article: Haematological indicators of complementary healing intervention
Daniel P. Wirth · Richard J. Chang · William S. Eidelman · Joanne B. Paxton
Abstract: The effect of Therapeutic Touch, Reiki, LeShan, and Qigong Therapy in combination on haematological measures was examined in an exploratory pilot study utilizing a randomized, double-blind, within-subject, crossover design. Fourteen subjects were randomly assigned to treatment and control conditions for two one-hour evaluation sessions separated by a 24-hour period. Six blood samples were taken from each subject — three during the treatment condition and three during the control condition —…
Article · Jan 1996 · Complementary Therapies in Medicine
———-
Article: The significance of belief and expectancy within the spiritual healing encounter
Daniel P. Wirth
Abstract: Historically, traditional cultures recognized the importance of belief and expectancy within the healing encounter and created complex rituals and ceremonies designed to elicit or foster the expectancy and participation of both the healer and patient, as well as the community as a whole. This holistic approach to health care was a fundamental component in the spiritual healing rituals of virtually all traditional native cultures. The focus of the current study was to assess the impact of…
Article · Aug 1995 · Social Science & Medicine
———-
Article: Non-contact Therapeutic Touch and wound re-epithelialization: An extension of previous research
Daniel P. Wirth · Margaret J Barrett · William S. Eidelman
Abstract: The results demonstrated a non-significant effect for the treatment versus control groups. Several factors may have contributed to the non-significance, including: the ineffectiveness of the healers, the inhibitive or dampening effect of plastic, the use of self-regulatory techniques, the dependent variable examined, the type of dressing utilized, the influence of distance, and the healers’ belief as to the effect of distance. Future studies would benefit by examining the methodological…
Article · Oct 1994 · Complementary Therapies in Medicine
———-
Daniel P. Wirth · David R. Brenlan · Richard J. Levine · Christine M. Rodriguez
Abstract: This study utilized a randomized, double-blind, within subject, crossover design to examine the effect of Reiki and LeShan healing in combination on iatrogenic pain experienced after unilateral operative extraction of the lower third molar. Two separate operations were performed on 21 patients with bilateral, asymptomatic, impacted lower third molar teeth. The patients were randomly assigned to the treatment or control condition prior to the first operation. For the second operation,…
Article · Jul 1993 · Complementary Therapies in Medicine
———-
Article: Full thickness dermal wounds treated with non-contact Therapeutic Touch: a replication and extension
Daniel P. Wirth · Joseph T. Richardson · William S. Eidelman · Alice C. O’Malley
Abstract: The effect of non-contact Therapeutic Touch (NCTT) therapy on the healing rate of full thickness human dermal wounds was examined in a double-blind, placebo controlled study. Punch biopsies were performed on the lateral deltoid in 24 healthy subjects who were randomly assigned to treatment and control groups. Active and control treatments were comprised of daily sessions of 5 min of exposure to a hidden NCTT practitioner or control exposure. Placebo effects and the possible influences of…
Article · Jul 1993 · Complementary Therapies in Medicine
———-
Article: The Effect of Alternative Healing Therapy on the Regeneration Rate of Salamander Forelimbs
DANIEL P. WIRTH · CATHY A. JOHNSON · JOSEPH S. HORVATH
Article · Jan 1992
———-
Article: Complementary Healing Therapy For Patients With Type I Diabetes Mellitus
DANIEL P. WIRTH · BARBARA J. MITCHELL
Abstract: The effect of Noncontact Therapeutic Touch (NCTT) therapy and Intercessory Prayer (IP) on patient determined insulin dosage was exam- ined in an exploratory pilot study which utilized a randomized, double-blind, within subject, crossover design. Sixteen type I diabetes mellitus patients were examined and treated daily by NCTT and IP healers for a duration of two weeks. Each patient underwent two separate sessions-one in the treat- ment condition and one in the control condition-with the…
____________________________________________________________________
What is even worse, Wirth’s papers continue to get cited. In other words, Wirth’s research lives on regardless of the fact that it is highly dubious.
In my view, it is long over-due for all journal-editors to fully and completely delete Wirth’s dubious papers. This is particularly true since several experts have alerted them to the problem. Furthermore, I submit that failing to take action amounts to unethical behaviour which is quite simply unacceptable.