In previous posts, I have been scathing about chiropractors (DCs) treating children; for instance here:
- Despite calling themselves ‘doctors’, they are nothing of the sort.
- DCs are not adequately educated or trained to treat children.
- They nevertheless often do so, presumably because this constitutes a significant part of their income.
- Even if they felt confident to be adequately trained, we need to remember that their therapeutic repertoire is wholly useless for treating sick children effectively and responsibly.
- Therefore, harm to children is almost inevitable.
- To this, we must add the risk of incompetent advice from DCs – just think of immunisations.
Now we have more data on this subject. This new study investigated the effectiveness of adding manipulative therapy to other conservative care for spinal pain in a school-based cohort of Danish children aged 9–15 years.
The design was a two-arm pragmatic randomised controlled trial, nested in a longitudinal open cohort study in Danish public schools. 238 children from 13 public schools were included. A text message system and clinical examinations were used for data collection. Interventions included either (1) advice, exercises and soft-tissue treatment or (2) advice, exercises and soft-tissue treatment plus manipulative therapy. The primary outcome was number of recurrences of spinal pain. Secondary outcomes were duration of spinal pain, change in pain intensity and Global Perceived Effect.
No significant difference was found between groups in the primary outcomes of the control group and intervention group. Children in the group receiving manipulative therapy reported a higher Global Perceived Effect. No adverse events were reported.
The authors – well-known proponents of chiropractic (who declared no conflicts of interest) – concluded that adding manipulative therapy to other conservative care in school children with spinal pain did not result in fewer recurrent episodes. The choice of treatment—if any—for spinal pain in children therefore relies on personal preferences, and could include conservative care with and without manipulative therapy. Participants in this trial may differ from a normal care-seeking population.
The study seems fine, but what a conclusion!!!
After demonstrating that chiropractic manipulation is useless, the authors state that the treatment of kids with back pain could include conservative care with and without manipulative therapy. This is more than a little odd, in my view, and seems to suggest that chiropractors live on a different planet from those of us who can think rationally.
The indefatigable Robert Mathie has published another systematic review/meta-analysis, and yet again he failed to come up with a convincingly positive result. This new paper reviews randomised controlled trials (RCTs) of individualised homeopathic treatment (IHT) in which the control (comparator) group was other than placebo (OTP). Its stated aim was to determine the comparative effectiveness of IHT on health-related outcomes in adults and children for any clinical condition that has been the subject of at least one OTP-controlled trial.
For each eligible trial, published in the peer-reviewed literature up to the end of 2015, the authors assessed its risk of bias (internal validity) using the Cochrane tool, and its relative pragmatic or explanatory attitude (external validity) using the 10-domain PRECIS tool. All RCTs were categorised according to whether they examined IHT as an alternative treatment (study design Ia), adjunctively with another intervention (design Ib), or compared with a no-intervention group (design II). For each RCT, the researchers identified a ‘main outcome measure’ to use in meta-analysis: ‘relative effect size’ was reported as odds ratio (OR; values >1 favouring homeopathy) or standardised mean difference (SMD; values < 0 favouring homeopathy).
Eleven RCTs, representing 11 different medical conditions, were eligible for inclusion in this systematic review. Five of the RCTs (four of which in design Ib) were judged to have pragmatic study attitude, two were explanatory, and four were equally pragmatic and explanatory. Ten trials were rated ‘high risk of bias’ overall: one of these, a pragmatic study with design Ib, had high risk of bias solely regarding participant blinding (a bias that is intrinsic to such trials); the other trial was rated ‘uncertain risk of bias’ overall. Eight trials had data that were extractable for meta-analysis: for 4 heterogeneous trials with design Ia, the pooled OR was statistically non-significant; collectively for three clinically heterogeneous trials with design Ib, there was a statistically significant SMD favouring adjunctive IHT; in the remaining trial of design 1a, IHT was non-inferior to fluoxetine in the treatment of depression.
The authors concluded that due to the low quality, the small number and the heterogeneity of studies, the current data preclude a decisive conclusion about the comparative effectiveness of IHT. Generalisability of findings is limited by the variable external validity identified overall; the most pragmatic study attitude was associated with RCTs of adjunctive IHT. Future OTP-controlled trials in homeopathy should aim, as far as possible, to promote both internal validity and external validity.
Considering that almost all of the authors are known proponents of homeopathy – Mathie himself is employed by the London-based ‘Homeopathy Research Institute’ – one has to applaud their rigour and enthusiasm in publishing negative findings about their trade. But why so complicated? I would have thought that a much simpler conclusion would have been clearer: THESE ANALYSES FAILED TO GENERATE EVIDENCE TO SUGGEST THAT HOMEOPATHY IS EFFECTIVE.
“Physiotherapy generally offers a highly science based approach to clinical practice.” This was a recent comment by someone (I presume a physiotherapist) on this blog. It got me thinking – is it true or false? I am in no position to review the entire field of physiotherapy in a blog post. What I will do instead, is list a few alternative therapies often used by physiotherapists.
- Acupuncture: many physiotherapists seem to love acupuncture. In the UK, for example, they have their own organisations. The AACP is the largest professional body for acupuncture in the UK with a membership of around 6000 chartered physiotherapists, practising medical acupuncture. They state that there is an increasing number of research publications in the UK and worldwide proving the treatment effectiveness of acupuncture when compared to (chemical) medication for example.
- Applied kinesiology: some physiotherapists offer applied kinesiology. This clinic, for instance, states that applied Kinesiology combines a system of muscle tests with acupuncture, reflex points emotion and nutrition to find any imbalances present in the whole person.
- Bowen technique: many physiotherapists use the Bowen technique. This practice advertises it as follows. If you’re looking for a way to treat tightness in your upper back, neck or shoulders or are suffering from respiratory pain or headaches, The Bowen Technique could be the answer you’re searching for. Achieving all these things as well as being a great way to treat sports injuries and enhance sporting performance, this therapy also promotes emotional wellbeing. A non-invasive therapy, it is equally suited for the treatment of acute (short-term) and chronic (long-term) conditions.
- Craniosacral therapy: some physios also employ craniosacral therapy. Here is an example. Craniosacral therapy as experienced by thousands of babies and people all around the country, has a proven track record at easing and relieving what makes babies upset. If your baby suffers from:
- Colic
- Wind
- Digestive issues
- Reflux
- Unsettledness
- Sleep problems
- Ongoing crying
- Difficulty with breast feeding/latch/suck
- Other problems
then call…
- Cupping: One physio writes this about cupping. It was good to see the public (Western cultures) exposed more to cupping therapy practice thanks to the recent Olympics in Rio 2016. Last Olympics in London 2012, the Chinese and Japanese Athletes, amongst neighbouring nations, were readily seen to use and advocate the practice, along with the approval no doubt of their large team of Medical and Physiotherapy related support staff. This time however it has bridged to divide to Western World Athletes, such as Michael Phelps (he of 23 Olympic Golds fame). This advocacy of the practice and again the presumed support from his Medical and Sports science entourage with team USA, is a good barometer of the progress and acceptance within Western Medicine, for Cupping Therapy.
- Massage therapy: in many countries, massage and related techniques therapy always have been an integral part of physiotherapy.
- Feldenkrais method: The same applies to The Feldenkrais Method® is based on principles of physics, biomechanics, neuroscience, and the study of human motor development. Feldenkrais recognized the capability of the human brain to learn and relearn at any age – neuroplasticity. The method utilizes slow, gentle movements, and awareness of subtle differences to optimize learning, improve movement, and make changes in the brain.
- Kinesiology tape: If you have suffered an injury or illness that causes a problem with your functional mobility or normal activity, you may benefit from the skilled services of a physical therapist to help you return to your previous level of mobility. Your physical therapist may use various exercises and modalities to help treat your specific problem.
- Reflexology: Here is what the UK Chartered Society of Physiotherapists writes about reflexology: Developed centuries ago in countries such as China, Egypt and India, reflexology is often referred to as a ‘gentle’ and ‘holistic’ therapy that benefits both mind and body. It centres on the feet because these are said by practitioners to be a mirror, or topographical map, for the rest of the body. Manipulation of certain pressure, or reflex, points is claimed to have an effect on corresponding zones in the body. The impact, say reflexologists, extends throughout – to bones, muscles, organs, glands, circulatory and neural pathways. The head and hands can also be massaged in some cases. The treatment is perhaps best known for use in connection with relaxation and relief from stress, anxiety, pain, sleep disorders, headaches, migraine, menstrual and digestive problems. But advocates say it can be used to great effect far more widely, often in conjunction with other treatments…
- Spinal manipulation: Physiotherapists learn spinal manipulation as part of continuing education courses in Canada. The Orthopaedic Division of the Canadian Physiotherapy Association is responsible for the standards of education and supervises exams required to meet the standards of the International Federation of Manipulative Physiotherapists (IFOMPT). In many other countries, the situation is similar.
These 10 therapies have all been discussed on this blog before. They lack
- plausibility or
- proof of efficacy or
- proof of safety or
- all of the above
In other words, they are NOT highly science-based.
QED
It has been reported that the faculty of medicine of Lille unversity in France has suspended its degree in homeopathy for the 2018-19 academic year. The university announced its decision on Twitter, and the faculty of medicine’s dean, Didier Gosset, confirmed it to the AFP news agency: “It has to be said that we teach medicine based on proof – we insist on absolute scientific rigour – and it has to be said that homeopathy has not evolved in the same direction, that it is a doctrine that has remained on the margins of the scientific movement, that studies on homeopathy are rare, that they are not very substantial,” he explained. “Continuing to teach it would be to endorse it.”
The decision is, of course, long overdue and must be welcomed. Personally, however, I wonder why defenders of reason like Prof Gosset often employ such unclear lines of argument. Would it not be clearer to make (some of) these simple points?
- The assumptions on which homeopathy is based are obsolete and implausible.
- It is not that we do not understand homeopathy’s mode of action, but we understand that there cannot be one that does not fly in the face of science.
- The clinical evidence fails to show that highly diluted homeopathic remedies are more than placebos.
- Homeopathy can cause significant harm, e. g. through neglect.
- Homeopathy costs millions which would be much better used for evidence-based treatments.
- The practice of homeopathy hinders progress and does not provide benefit for the public.
- Teaching homeopathy at university-level is unscientific, unethical and nonsensical.
The French are among the world’s largest consumers of homeopathic remedies. The French social security system does normally reimburse homeopathic therapy. A group of doctors challenged this situation in an open letter in Le Figaro newspaper in March 2018. They called practitioners of homeopathy and other alternative medicines “charlatans”, pointing to a 2017 report by the European Academies Science Advisory Council that stressed, like a plethora of previous reports, the “absence of proof of homeopathy’s efficacy”. They challenged the French medical council to stop allowing doctors to practice homeopathy and asked the social security system to stop paying for it. Subsequently, a group of French homeopaths filed a formal complaint with the medical council against the signatories of this letter.
France’s health ministry has asked France’s National Health Authority to prepare and publish a report on whether homeopathy works and should be paid for by the public purse. It is due to be delivered in February 2019.
WATCH THIS SPACE
Psoriasis is one of those conditions that is
- chronic,
- not curable,
- irritating to the point where it reduces quality of life.
In other words, it is a disease for which virtually all alternative treatments on the planet are claimed to be effective. But which therapies do demonstrably alleviate the symptoms?
This review (published in JAMA Dermatology) compiled the evidence on the efficacy of the most studied complementary and alternative medicine (CAM) modalities for treatment of patients with plaque psoriasis and discusses those therapies with the most robust available evidence.
PubMed, Embase, and ClinicalTrials.gov searches (1950-2017) were used to identify all documented CAM psoriasis interventions in the literature. The criteria were further refined to focus on those treatments identified in the first step that had the highest level of evidence for plaque psoriasis with more than one randomized clinical trial (RCT) supporting their use. This excluded therapies lacking RCT data or showing consistent inefficacy.
A total of 457 articles were found, of which 107 articles were retrieved for closer examination. Of those articles, 54 were excluded because the CAM therapy did not have more than 1 RCT on the subject or showed consistent lack of efficacy. An additional 7 articles were found using references of the included studies, resulting in a total of 44 RCTs (17 double-blind, 13 single-blind, and 14 nonblind), 10 uncontrolled trials, 2 open-label nonrandomized controlled trials, 1 prospective controlled trial, and 3 meta-analyses.
Compared with placebo, application of topical indigo naturalis, studied in 5 RCTs with 215 participants, showed significant improvements in the treatment of psoriasis. Treatment with curcumin, examined in 3 RCTs (with a total of 118 participants), 1 nonrandomized controlled study, and 1 uncontrolled study, conferred statistically and clinically significant improvements in psoriasis plaques. Fish oil treatment was evaluated in 20 studies (12 RCTs, 1 open-label nonrandomized controlled trial, and 7 uncontrolled studies); most of the RCTs showed no significant improvement in psoriasis, whereas most of the uncontrolled studies showed benefit when fish oil was used daily. Meditation and guided imagery therapies were studied in 3 single-blind RCTs (with a total of 112 patients) and showed modest efficacy in treatment of psoriasis. One meta-analysis of 13 RCTs examined the association of acupuncture with improvement in psoriasis and showed significant improvement with acupuncture compared with placebo.
The authors concluded that CAM therapies with the most robust evidence of efficacy for treatment of psoriasis are indigo naturalis, curcumin, dietary modification, fish oil, meditation, and acupuncture. This review will aid practitioners in advising patients seeking unconventional approaches for treatment of psoriasis.
I am sorry to say so, but this review smells fishy! And not just because of the fish oil. But the fish oil data are a good case in point: the authors found 12 RCTs of fish oil. These details are provided by the review authors in relation to oral fish oil trials: Two double-blind RCTs (one of which evaluated EPA, 1.8g, and DHA, 1.2g, consumed daily for 12 weeks, and the other evaluated EPA, 3.6g, and DHA, 2.4g, consumed daily for 15 weeks) found evidence supporting the use of oral fish oil. One open-label RCT and 1 open-label non-randomized controlled trial also showed statistically significant benefit. Seven other RCTs found lack of efficacy for daily EPA (216mgto5.4g)or DHA (132mgto3.6g) treatment. The remainder of the data supporting efficacy of oral fish oil treatment were based on uncontrolled trials, of which 6 of the 7 studies found significant benefit of oral fish oil. This seems to support their conclusion. However, the authors also state that fish oil was not shown to be effective at several examined doses and duration. Confused? Yes, me too!
Even more confusing is their failure to mention a single trial of Mahonia aquifolium. A 2013 meta-analysis published in the British Journal of Dermatology included 5 RCTs of Mahonia aquifolium which, according to these authors, provided ‘limited support’ for its effectiveness. How could they miss that?
More importantly, how could the reviewers miss to conduct a proper evaluation of the quality of the studies they included in their review (even in their abstract, they twice speak of ‘robust evidence’ – but how can they without assessing its robustness? [quantity is not remotely the same as quality!!!]). Without a transparent evaluation of the rigour of the primary studies, any review is nearly worthless.
Take the 12 acupuncture trials, for instance, which the review authors included based not on an assessment of the studies but on a dodgy review published in a dodgy journal. Had they critically assessed the quality of the primary studies, they could have not stated that CAM therapies with the most robust evidence of efficacy for treatment of psoriasis …[include]… acupuncture. Instead they would have had to admit that these studies are too dubious for any firm conclusion. Had they even bothered to read them, they would have found that many are in Chinese (which would have meant they had to be excluded in their review [as many pseudo-systematic reviewers, the authors only considered English papers]).
There might be a lesson in all this – well, actually I can think of at least two:
- Systematic reviews might well be the ‘Rolls Royce’ of clinical evidence. But even a Rolls Royce needs to be assembled correctly, otherwise it is just a heap of useless material.
- Even top journals do occasionally publish poor-quality and thus misleading reviews.
Medline is the biggest electronic databank for articles published in medicine and related fields. It is therefore the most important source of information in this area. I use it regularly to monitor what new papers have been published in the various fields of alternative medicine.
As the number of Medline-listed papers dated 2018 on homeopathy has just reached 100, I thought it might be the moment to run a quick analysis on this material. The first thing to note is that it took until August for 100 articles dated 2018 to emerge. To explain how embarrassing this is, we need a few comparative figures. At the same moment (6/9/18), we have, for instance:
- 126576 articles for surgery
- 5001 articles or physiotherapy
- 30215 articles for psychiatry
- 60161 articles for pharmacology
Even compared to other types of alternative medicine, homeopathy is being dwarfed. Currently the figures are, for instance:
- 2232 for herbal medicine
- 1949 for dietary supplements
- 1222 for acupuncture
This does not look as though homeopathy is a frightfully active area of research, if I may say so. Looking at the type of articles (yes, I did look at all the 100 papers and categorised them the best I could) published in homeopathy, things get even worse:
- 29 were comments, letters, editorials, etc.
- 16 were basic and pre-clinical papers,
- 12 were non-systematic reviews,
- 10 were surveys,
- 7 were case-reports,
- 5 were pilot or feasibility studies,
- 5 were systematic reviews,
- 5 were controlled clinical trials,
- 2 were case series,
- the rest of the articles was not on homeopathy at all.
I find this pretty depressing. Most of the 100 papers turn out to be no real research at all. Crucial topics are not being covered. There was, for example, not a single paper on the risks of homeopathy (no, don’t tell me it is harmless; it can and does regularly cost the lives of patients who trust the bogus claims of homeopaths). There was no article investigating the important question whether the practice of homeopathy does not violate the rules of medical ethics (think of informed consent or the imperative to do more harm than good). And a mere 5 clinical trials is just a dismal amount, in my view.
In a previous post, I have already shown that, in 2015, homeopathy research was deplorable. My new analysis suggests that the situation has become much worse. One might even go as far as asking whether 2018 might turn out to be the year when homeopathy research finally died a natural death.
PROGRESS AT LAST!!!
Yesterday, I was interviewed and filmed by a Canadian TV-journalist. Even though the subject was osteopathy (apparently, in Canada, osteopathy is strong and full of woo), we found ourselves talking about ‘oil pulling’. I knew next to nothing about this alternative therapy, but learnt that it was big in North America. When the TV-crew had left my home, I therefore read up about it. I must admit, I was more than a little sceptical about the therapy – not least because I soon found articles by fellow sceptics that were less than complimentary – but, as I studied the original research on oil pulling, my scepticism somewhat waned.
So, what is oil pulling? It is the use of oil for swishing it around your mouth for alleged health benefits. Here are several short points that might explain it more fully:
- Oil pulling is said to have roots that reach back to ancient Hindu texts. Coconut or sesame oils are usually employed for this therapy.
- The mechanism of action (if there is one at all) is poorly understood, and several theories have been put forward:
Alkali hydrolysis of fat results in saponification or “soap making” process. Since the oils used for oil pulling contain fat, the alkali hydrolysis process emulsifies the fat into bicarbonate ions, normally found in the saliva. Soaps then blend in the oil, increase the surface area of the oil, and thus cleanse the teeth and gums.
A second theory suggests that the viscous nature of the oil inhibits plaque accumulation and adhesion of bacteria.
A third theory holds that the antioxidants present in the oil prevent lipid peroxidation, resulting in an antibiotic-like effect helping in the destruction of microorganisms.
- Oil pulling is recommended to be carried out in the morning on an empty stomach. About 10 ml of oil is swished between the teeth for a duration of approximately 15-20 min and spat out. This ritual should be followed by rinsing and tooth brushing. The practice should be repeated regularly, even three times daily for acute diseases.
- To my surprise, oil pulling has been tested in clinical trials. Some of these investigations seem reasonably sound and suggest that coconut oil pulling reduces potentially harmful bacteria in the mouth.[1] This effect has been shown to lead to a reduction in dental plaque formation[2] , halitosis (bad breath) [3] and gingivitis. [4]
- The evidence for these oral effects is by no means strong, but I have not found studies that show negative results.
- Dentists – even the bizarre species of ‘holistic dentists‘ – do not seem to be balled over by oil pulling (some malicious minds might speculate that this is so because they cannot earn much money with it).
- The claimed benefits of oil pulling are, however, not limited to the oral cavity. It is advocated also for the prevention and treatment of conditions such as headaches, migraines, thrombosis, eczema, diabetes and asthma.[5] Some proponents also claim that oil pulling is a detox therapy. Unsurprisingly, none of these claims are supported by good evidence.
- As long as you don’t swallow the oil, there are no serious risks associated with oil pulling.
So, what is the conclusion? To me, the evidence looks promising as far as oral health is concerned. For all other indication, oil pulling is neither plausible nor evidence-based.
[1] https://www.ncbi.nlm.nih.gov/pubmed/27891311
[2] https://www.ncbi.nlm.nih.gov/pubmed/18408265
[3] https://www.ncbi.nlm.nih.gov/pubmed/21911944
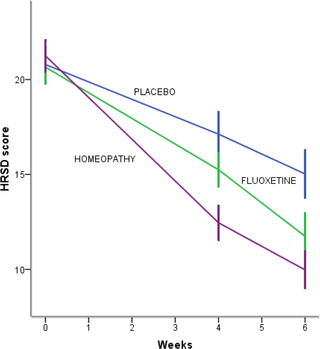
This systematic review included 18 studies assessing homeopathy in depression. Two double-blind placebo-controlled trials of homeopathic medicinal products (HMPs) for depression were assessed. The first trial (N = 91) with high risk of bias found HMPs were non-inferior to fluoxetine at 4 (p = 0.654) and 8 weeks (p = 0.965); whereas the second trial (N = 133), with low risk of bias, found HMPs was comparable to fluoxetine (p = 0.082) and superior to placebo (p < 0.005) at 6 weeks.
The remaining research had unclear/high risk of bias. A non-placebo-controlled RCT found standardised treatment by homeopaths comparable to fluvoxamine; a cohort study of patients receiving treatment provided by GPs practising homeopathy reported significantly lower consumption of psychotropic drugs and improved depression; and patient-reported outcomes showed at least moderate improvement in 10 of 12 uncontrolled studies. Fourteen trials provided safety data. All adverse events were mild or moderate, and transient. No evidence suggested treatment was unsafe.
The authors concluded that limited evidence from two placebo-controlled double-blinded trials suggests HMPs might be comparable to antidepressants and superior to placebo in depression, and patients treated by homeopaths report improvement in depression. Overall, the evidence gives a potentially promising risk benefit ratio. There is a need for additional high quality studies.
It is worth having a look at these two studies, I think.
The 1st (2011) study is from Brazil
Here is its abstract:
Homeopathy is a complementary and integrative medicine used in depression, The aim of this study is to investigate the non-inferiority and tolerability of individualized homeopathic medicines [Quinquagintamillesmial (Q-potencies)] in acute depression, using fluoxetine as active control. Ninety-one outpatients with moderate to severe depression were assigned to receive an individualized homeopathic medicine or fluoxetine 20 mg day−1 (up to 40 mg day−1) in a prospective, randomized, double-blind double-dummy 8-week, single-center trial. Primary efficacy measure was the analysis of the mean change in the Montgomery & Åsberg Depression Rating Scale (MADRS) depression scores, using a non-inferiority test with margin of 1.45. Secondary efficacy outcomes were response and remission rates. Tolerability was assessed with the side effect rating scale of the Scandinavian Society of Psychopharmacology. Mean MADRS scores differences were not significant at the 4th (P = .654) and 8th weeks (P = .965) of treatment. Non-inferiority of homeopathy was indicated because the upper limit of the confidence interval (CI) for mean difference in MADRS change was less than the non-inferiority margin: mean differences (homeopathy-fluoxetine) were −3.04 (95% CI −6.95, 0.86) and −2.4 (95% CI −6.05, 0.77) at 4th and 8th week, respectively. There were no significant differences between the percentages of response or remission rates in both groups. Tolerability: there were no significant differences between the side effects rates, although a higher percentage of patients treated with fluoxetine reported troublesome side effects and there was a trend toward greater treatment interruption for adverse effects in the fluoxetine group. This study illustrates the feasibility of randomized controlled double-blind trials of homeopathy in depression and indicates the non-inferiority of individualized homeopathic Q-potencies as compared to fluoxetine in acute treatment of outpatients with moderate to severe depression.
There are many important points to make about this trial:
- Contrary to what the reviewers claim, the trial had no placebo group.
- It was a double-dummy equivalence study comparing individualised homeopathy with the antidepressant fluoxetine.
- Fluoxetine might have been under-dosed (see below).
- Equivalence studies require large sample sizes, and with just 91 patients (only 55 of whom finished the study), this trial was underpowered which means the finding of equivalence is false positive.
- The authors noted that a higher percentage of troublesome adverse effects reported by patients receiving fluoxetine. This means that the trial was not double-blind; patients were able to tell by their side-effects which group they were in.
- The authors also state that more patients randomized to homeopathy than to fluoxetine were excluded due to worsening of their depressive symptoms. I think this confirms that homeopathy was ineffective.
The 2nd (2015) study is from Mexico
Here is its abstract:
Background: Perimenopausal period refers to the interval when women’s menstrual cycles become irregular and is characterized by an increased risk of depression. Use of homeopathy to treat depression is widespread but there is a lack of clinical trials about its efficacy in depression in peri- and postmenopausal women. The aim of this study was to assess efficacy and safety of individualized homeopathic treatment versus placebo and fluoxetine versus placebo in peri- and postmenopausal women with moderate to severe depression.
Methods/Design: A randomized, placebo-controlled, double-blind, double-dummy, superiority, three-arm trial with a 6 week follow-up study was conducted. The study was performed in a public research hospital in Mexico City in the outpatient service of homeopathy. One hundred thirty-three peri- and postmenopausal women diagnosed with major depression according to DSM-IV (moderate to severe intensity) were included. The outcomes were: change in the mean total score among groups on the 17-item Hamilton Rating Scale for Depression, Beck Depression Inventory and Greene Scale, after 6 weeks of treatment, response and remission rates, and safety. Efficacy data were analyzed in the intention-to-treat population (ANOVA with Bonferroni post-hoc test).
Results: After a 6-week treatment, homeopathic group was more effective than placebo by 5 points in Hamilton Scale. Response rate was 54.5% and remission rate, 15.9%. There was a significant difference among groups in response rate definition only, but not in remission rate. Fluoxetine-placebo difference was 3.2 points. No differences were observed among groups in the Beck Depression Inventory. Homeopathic group was superior to placebo in Greene Climacteric Scale (8.6 points). Fluoxetine was not different from placebo in Greene Climacteric Scale.
Conclusion: Homeopathy and fluoxetine are effective and safe antidepressants for climacteric women. Homeopathy and fluoxetine were significantly different from placebo in response definition only. Homeopathy, but not fluoxetine, improves menopausal symptoms scored by Greene Climacteric Scale.
And here are my critical remarks about this trial:
- The aim of a small study like this cannot be to assess or draw conclusions about the safety of the interventions used; for this purpose, we need sample sizes that are at least one dimension bigger.
- Fluoxetine might have been under-dosed (see below).
- The blinding of patients might have been jeopardized by patients experiencing the specific side-effects of fluoxetine. The authors reported adverse effects in all three groups. However, the characteristic and most common side-effects of fluoxetine (such as hives, itching, skin rash, restlessness, inability to sit still) were not included.
________________________________________________
Usual Adult Dose for Depression
Immediate-release oral formulations:
Initial dose: 20 mg orally once a day in the morning, increased after several weeks if sufficient clinical improvement is not observed
Maintenance dose: 20 to 60 mg orally per day
Maximum dose: 80 mg orally per day
Delayed release oral capsules:
Initial dose: 90 mg orally once a week, commenced 7 days after the last daily dose of immediate-release fluoxetine 20 mg formulations.
_________________________________________________
Considering all this, I feel that the conclusions of the above review are far too optimistic and not justified. In fact, I find them misleading, dangerous, unethical and depressing.
On 4 September 2018, during the FIP (78th FIP World Congress of Pharmacy and Pharmaceutical Sciences), a meeting took place intended to give an opportunity to practising pharmacists to voice their opinions on the question whether pharmacies should stop selling homeopathic products. Attendees were provided with voting materials to allow them to express their views in a spontaneous and powerful manner, and for FIP to ascertain genuine opinions about this important matter. The debate and subsequent voting is likely to influence FIP policymaking and statement formulation. Here is the outline of the meeting:
The Great Debate – The motion “Pharmacists should not sell or dispense homeopathic products”
12:30 – 12:34 Introduction by the chairs
- 12:34 – 12:57 For the motion
Geoff Tucker (University of Sheffield, UK) - 12:57 – 13:20 Against the motion
Christine Glover (Glover’s Integrated Healthcare, UK) - 13:20 – 13:25 Ethical considerations related to homeopathy
Betty Chaar (The University of Sydney, Australia) - 13:25 – 13:35 Responses and summary
Facilitator: Andy Gray (University of KwaZulu Natal, South Africa)- Against the motion
Christine Glover (Glover’s Integrated Healthcare, UK) - For the motion
Geoff Tucker (University of Sheffield, UK)
- Against the motion
- 13:35 -14:00 Open forum – Questions from the audience with speakers and chairs as panel/ Vote and concluding comments
The German ‘Pharmazeutische Zeitung‘ just published a report about the outcome of the meeting:
“Bei der Abstimmung im Anschluss sprachen sich fast zwei Drittel der im Auditorium anwesenden Pharmazeuten gegen eine Distribution von homöopathischen Produkten durch Apotheken aus. Mehr als ein Drittel stimmte für den Erhalt der Produkte in den Apotheken. Das Ergebnis habe keine bindende Wirkung für den Entscheidungsprozess des FIP, machte der Moderator der Sitzung, Andy Gray von der Universität KwaZulu Natal in Südafrika, deutlich. Es gebe aber einen Hinweis, in welche Richtung sich die Organisation orientieren sollte. (ch).”
In plain English: two thirds voted for the motion and against homeopathic products remaining on sale in pharmacies. The vote has, however, no binding effect on FIP policy. It is nevertheless likely to determine the direction in which FIP will decide.
I think this is long-overdue (I have been trying to persuade pharmacists to do something like this since ~15 years). I now applaud the FIP for raising the issue. Bravo!
What next?
The vote needs to be translated into policy.
Other healthcare professionals – not least doctors – must follow suit.
Just when I thought I had seen all homeopathy has to offer, here comes this:
THE BRISTOL STOOL CHART AND CORRESPONDING HOMEOPATHIC REMEDIES!
“With mere examination of stool appearance, Homoeopathic remedy can easily be selected….”
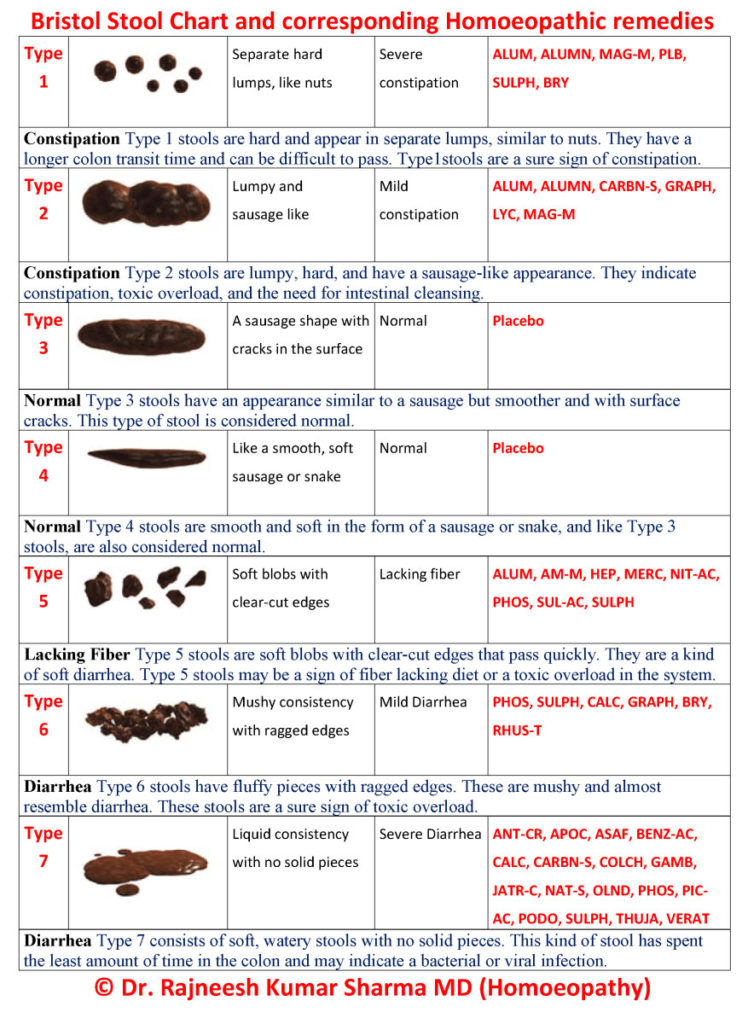 The chart was, according to Wikipedia, developed and proposed for the first time by Dr. Stephen Lewis and Dr. Ken Heaton at the University Department of Medicine, Bristol Royal Infirmary, it was suggested by the authors as a clinical assessment tool in 1997 in the journal Scandinavian Journal of Gastroenterology after a previous prospective study, conducted in 1992 on a sample of the population (838 men and 1,059 women), had shown an unexpected prevalence of defecation disorders related to the shape and type of stool. The authors of the former paper concluded that the form of the stool is a useful surrogate measure of colon transit time. That conclusion has since been challenged as having limited validity for Types 1 and 2; however, it remains in use as a research tool to evaluate the effectiveness of treatments for various diseases of the bowel, as well as a clinical communication aid.
The chart was, according to Wikipedia, developed and proposed for the first time by Dr. Stephen Lewis and Dr. Ken Heaton at the University Department of Medicine, Bristol Royal Infirmary, it was suggested by the authors as a clinical assessment tool in 1997 in the journal Scandinavian Journal of Gastroenterology after a previous prospective study, conducted in 1992 on a sample of the population (838 men and 1,059 women), had shown an unexpected prevalence of defecation disorders related to the shape and type of stool. The authors of the former paper concluded that the form of the stool is a useful surrogate measure of colon transit time. That conclusion has since been challenged as having limited validity for Types 1 and 2; however, it remains in use as a research tool to evaluate the effectiveness of treatments for various diseases of the bowel, as well as a clinical communication aid.
Nobody had meant this chart to get in any way related to homeopathy. I congratulate Dr Sharma to have spotted the connection. Thanks to him, we all can now easily find which homeopathic remedies are the ones we need. The writing is not on the wall, it is in the loo! I think someone should inform the Karolinska Institute in Stockholm – this surely is Nobel Prize material!!!