Doubtlessly, you will have noted that homeopathy missed out yet again at this year’s Nobels. Personally, I am convinced that this is all due to the evil propaganda put about by malicious sceptics (paid lavishly by BIG PHARMA, of course). But all is not lost! Down under, ‘CHOICE’ do know what is truly prize-worthy!
The Australian Consumers’ Association ‘CHOICE’ reviews everyday items like aspirin, detergents and instant coffee – but also major purchases like cars and washing machines. Each year, CHOICE awards ‘SHONKIES’ (from ‘shonky‘ = dishonest, unreliable, or illegal, especially in a devious way). CHOICE receive hundreds of nominations for Shonky products and services from CHOICE members and staff. While some Shonky nominees may not be breaking laws or breaching regulations – though sometimes they are – they believe that consumers deserve better products and services.
And how do they decide which nominations make the cut?
First and foremost, a nomination has to meet one or more of the following Shonky criteria:
- Fails a standard
- Poor performance on CHOICE tests
- Hidden charges
- Lack of transparency
- False claims or broken promises
- Consumers are worse off because of it
- Consumer confusion
- Poor value for money
- Consumer frustration, or just plain outrage
Products that meet one or more of these criteria make it to the short list. From there CHOICE look at how the issue will resonate with consumers, as well as government authorities and the media, which have the power to prod companies to pick up their act.
This year, CHOICE awarded 7 shonkies. My favourite, of course, is the award for trickery that leaves people sleepless – here is what CHOICE tell us about it:
Big pharmaceutical companies, or ‘big pharma’, are synonymous with big medical production, big money and a big impact on the type of healthcare products we can access. One thing that’s rarely expected from big pharma is homeopathic cures, which are more typically found in the domain of alternative therapies.
However, at least one big pharma company in Australia is selling homeopathic products on a very large scale. Pharmacare, which boasts on LinkedIn that it’s “the largest private, Australian-owned consumer health, fitness and consumer goods company in the country”, currently operates 23 brands, including Bioglan. According to their website, their products are available in “5200 pharmacies, 3000 supermarket outlets, department and variety stores nationwide, and hundreds of overseas outlets in Asia, America and Europe.”
In 2017, we awarded Bioglan and another Pharmacare brand, Nature’s Way, a Shonky for its outrageous claims that sticky, sugary lollies are in fact good for teeth. This year, Pharmacare and Bioglan receive another dubious honour for its over-the-counter Melatonin Homeopathic Sleep Formula. While melatonin (currently a prescription-only medicine in Australia) is known to promote sleep and is used to help people suffering jet lag or sleep disorders, there’s no reliable evidence that homeopathic melatonin (or homeopathic products in general) has any effect other than as a placebo. Despite this, the company makes the claim that Bioglan Melatonin helps “relieve mild temporary insomnia and symptoms of mild nervous tension”.
Bioglan’s Melatonin Homeopathic Sleep Formula is also available in chewable tablet form or spray and both products promise to “relieve mild temporary insomnia”.
On the product’s web page, we’re told “results depend on how often the homeopathic remedy is taken, not on the quantity used”, because in homeopathy, “the amount consumed is not relevant, children are treated in the same way as adults”.
However, directions for the tablet version state, “To aid sleep: Chew 3-5 tablets half an hour before bedtime”, while the spray is “rapidly absorbed to start working quickly”.
To be fair to Bioglan, consuming more does support the primary reason for this product’s existence – the more tablets people chew, the sooner they’ll potentially cough up another $24.50 (RRP).
Melatonin Homeopathic Sleep Formula is packaged like medication and sold in a pharmacy. But with murky claims that are not supported with evidence, wasting money is the only area where this product is proven to be effective. Not only does Bioglan Melatonin not help you sleep, it’s Shonky enough that you might lose sleep worrying about the brazen trickery this company gets away with.
END OF QUOTE
As I said, it’s not a Nobel, but it’s certainly a start.
My heart-felt congratulations to homeopaths across the world!
Evening primrose oil (EPO) is amongst the best-selling herbal remedies of all times. It is marketed in most countries as a dietary supplement. It is being promoted for eczema, rheumatoid arthritis, premenstrual syndrome, breast pain, menopause symptoms, and many other conditions. EPO seems to be a prime example for the fact that, in alternative medicine, the commercial success of a remedy is not necessarily determined by the strength of the evidence but by the intensity and cleverness of the marketing activities.
Evening primrose oil has been extensively tested in clinical trials for a wide range of conditions, including eczema (atopic dermatitis), postmenopausal symptoms, asthma, psoriasis, cellulite, hyperactivity, multiple sclerosis, schizophrenia, obesity, chronic fatigue syndrome, rheumatoid arthritis, and mastalgia. As I have reported previously, these data were burdened with mischief and scientific misconduct, and it is therefore not easy to differentiate between science, pseudoscience and fraud. The results of the more reliable investigations fail to show that it is effective for any condition. A Cochrane review of 2013, for instance, concluded that supplements of evening primrose oil lack effect on eczema; improvement was similar to respective placebos used in trials.
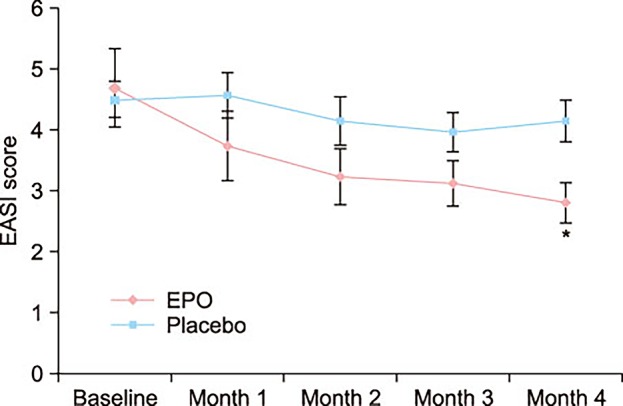
But now, a new study has emerged that casts doubt on this conclusion. The aim of this double-blinded, placebo-controlled RCT is to evaluate the efficacy and safety of EPO in Korean patients with atopic dermatitis (AD).
Fifty mild AD patients with an Eczema Area Severity Index (EASI) score of 10 or less were randomly divided into two groups. The first group received an oval unmarked capsule containing 450 mg of EPO (40 mg of GLA) per capsule, while placebo capsules identical in appearance and containing 450 mg of soybean oil were given to the other group. Treatment continued for a period of 4 months. EASI scores, transepidermal water loss (TEWL), and skin hydration were evaluated in all the AD patients at the baseline, and in months 1, 2, 3, and 4 of the study.
At the end of month 4, the patients of the EPO group showed a significant improvement in the EASI score, whereas the patients of the placebo group did not. There was a significant difference in the EASI score between the EPO and placebo groups. Although not statistically significant, the TEWL and skin hydration also slightly improved in the EPO patients group. Adverse effect were not found in neither the experimental group nor the control group during the study period.
The authors concluded by suggesting that EPO is a safe and effective medicine for Korean patients with mild AD.
I find this study odd for several reasons:
- One cannot possibly draw conclusions based on such a small sample.
- The authors state that a total of 69 mild AD patients were enrolled and randomized into either the control group (14 males and 17 females) or the EPO group (20 males and 18 females). Six patients in the control group and 13 patients in the EPO group dropped out due to follow up loss. No patient dropped out because the disease worsened. Should this not have necessitated an intention-to-treat analysis? And, if 19 patients were lost to follow-up, how do the authors know that their disease did not worsen?
- The graph shows impressively the lack of a placebo-response. I don’t understand why there was none.
- The authors state that there were no adverse effects at all. I find this implausible; we know that even taking placebos will prompt patients to report adverse effects.
So, what to make out of this?
I am not at all sure, but one thing is certain: this study does not alter my verdict on EPO; as far as I am concerned, the effectiveness of EPO for AD is unproven.
On 29 August, I published a post discussing a case report of a patient who had suffered multiple unilateral pre-retinal haemorrhages immediately following chiropractic neck manipulation suggesting that chiropractic spinal adjustments can not only affect the carotid artery, but also could lead to pre-retinal haemorrhages. Two days ago (over one month after my blog-post), the story was reported in the Daily Mail. They (originally) quoted me both in their on-line and print version as follows: “Edzard Ernst, an expert in alternative medicine, said chiropractic treatments were too dangerous and not sufficiently effective to be recommended for any condition.”
I think this is a statement that does not really relate well to the story. Crucially, it is a sentence that I do not identify with.
So, why did I say it?
The answer is simple: I didn’t!
What happened is this:
The ‘science correspondent’ of the Mail emailed me asking whether she could speak to me. I replied that I am currently in Brittany and that it would be better to send me questions which I promised to answer swiftly. She then send a press-release about the above-mentioned case report and asked for a quote. The paragraph I swiftly sent her read as follows:
“Chiropractors frequently manipulate patients’ neck in such a way that the joints are taken beyond their physiological range of motion. This can lead to all sorts of problems, sometimes even death. This new report suggests that chiropractic neck manipulations can also damage the eyes. As the ensuing problems tend to be temporary, it is likely that such eye-damage occurs often after chiropractic treatments. Chiropractic neck manipulations are not convincingly effective for any condition; as they can cause a lot of harm, their risk/benefit balance is clearly negative. In other words, we should not use or recommend them.”
The science correspondent thanked me and replied that my quote was too long and had to be shortened; would I be happy, she asked, with the following text:
“Edzard Ernst, an expert in the study of alternative medicine and former professor at the University of Exeter, said: ‘Chiropractors frequently manipulate patients’ neck in such a way that the joints are taken beyond their physiological range of motion.
‘The ensuing problems tend to be temporary but it is likely that this kind of eye damage occurs often after chiropractic treatments.
‘Chiropractic neck manipulations are not convincingly effective for any condition as they can cause a lot of harm. Therefore we should not use or recommend them.’ ”
I made a slight alteration (exchanging ‘the ensuing problems’ for ‘the ensuing eye-problems’) and replied that this was fine by me.
When I saw what was eventually published (the nonsense printed in bold above), I was baffled and irritated. Therefore I instantly complained to the science correspondent. She apologised saying that my quote had been “paraphrased from [my] full quote, probably for reasons of space during the production process”. She also changed the quote in the on-line version to what it says currently.
I replied: “of course, I accept your apology personal, as I knew it was not your doing. nevertheless, I find it totally unacceptable that someone at the DM can just go ahead and change direct quotes. you say he/she paraphrased me; I disagree! the published sentence has an entirely different meaning. this is not journalism! I want an apology from the person who is responsible.”
The science correspondent then promised to take care of it; but, so far, nothing has happened.
One could easily view this episode as trivial. However, I believe that decent journalism should stick to the rules. And one of the most fundamental one is that journalists cannot put words into people’s mouths just because it fits their story-line (Boris Johnson did this when he was a journalist, and look what a formidable mess he is now creating!). If we let journalists get away with such behaviour, we cannot have trust in journalism. And if we cannot trust journalism, it has lost its purpose.
So, should I continue insisting on an adequate apology from the person responsible or not?
What do you think?
The aim of this RCT was to investigate the effects of an osteopathic manipulative treatment (OMT) which includes a diaphragm intervention compared to the same OMT with a sham diaphragm intervention in chronic non-specific low back pain (NS-CLBP).
Participants (N=66) with a diagnosis of NS-CLBP lasting at least 3 months were randomized to receive either an OMT protocol including specific diaphragm techniques (n=33) or the same OMT protocol with a sham diaphragm intervention (n=33), conducted in 5 sessions provided during 4 weeks.
The primary outcomes were pain (evaluated with the Short-Form McGill Pain Questionnaire [SF-MPQ] and the visual analog scale [VAS]) and disability (assessed with the Roland-Morris Questionnaire [RMQ] and the Oswestry Disability Index [ODI]). Secondary outcomes were fear-avoidance beliefs, level of anxiety and depression, and pain catastrophization. All outcome measures were evaluated at baseline, at week 4, and at week 12.
A statistically significant reduction was observed in the experimental group compared to the sham group in all variables assessed at week 4 and at week 12. Moreover, improvements in pain and disability were clinically relevant.
The authors concluded that an OMT protocol that includes diaphragm techniques produces significant and clinically relevant improvements in pain and disability in patients with NS-CLBP compared to the same OMT protocol using sham diaphragm techniques.
This seems to be a rigorous study. The authors describe in detail their well-standardised interventions in the full text of their paper. This, of course, will be essential, if someone wants to repeat the trial.
I have but a few points to add:
- What I fail to understand is this: why the authors call the interventions osteopathic? The therapist was a physiotherapist and the techniques employed are, if I am not mistaken, as much physiotherapeutic as osteopathic.
- The findings of this trial are encouraging but almost seem a little too good to be true. They need, of course, to be independently replicated in a larger study.
- If that is done, I would suggest to check whether the blinding of the patient was successful. If not, there is a suspicion that the diaphragm technique works partly or mostly via a placebo effect.
- I would also try to make sure that the therapist cannot influence the results in any way, for instance, by verbal or non-verbal suggestions.
- Finally, I suggest to employ more than one therapist to increase generalisability.
Once all these hurdles are taken, we might indeed have made some significant progress in the manual therapy of NS-CLBP.
In Germany, homeopathic firms are – as I recently mentioned – starting to panic. Sales figures have, for the first time since decades, declined. This is undoubtedly the work of all those evil sceptics (including, or perhaps foremost?, my evil self!) who are well-organised and even better-funded.
At least, this is what their new PR-man seems to think.
Christian J Becker has been exceedingly active on Twitter provoking everyone who said a word against homeopathy. He is without any doubt the fiercest PR-defender of German homeopathy since Claus Fritzsche. But just like with the late Fritzsche, all those years ago, I am beginning to worry. Is Mr Becker feeling alright? I see increasingly worrying signs and parallels. Might he be drifting into some sort of a psychopathologic episode?
- Despite being a novice to this field, he seems to think that a substance which had no therapeutic effect to start with – think of Berlin wall – becomes highly active, if you dilute it at a rate of 1:1000000000000000000000000000000000000000000000000000000000000, for instance. Could this be the first sign of a deeper problem developing?
- He hints at his suspicion that poor old Fritzsche did, in fact, not commit suicide as generally believed and well-documented. No, he seems to think that he was murdered! By whom? Not the evil sceptics, surely?!
- He seems persuaded that I am some sort of master mind of the growing German opposition to homeopathy. As I obviously know better, I find his persuasion worrying.
- A further concern, in my view, is Becker‘s assumption about the huge amounts of money that are behind the criticism of homeopathy. As the big money is demonstrably on the other side, i. e. the homeopathic industry, this loss of reality might be an ominous sign.
- Similarly, Becker believes that the German government has decided to go against homeopathy. As the opposite is (and always has been) the case, one might ask: do his opinions indicate some type of a paranoid trait?
- Becker thinks, as already mentioned, that those who speak out against homeopathy are all paid by some sinister source. We all receive big cheques and live a life of Reilly because of this lavish support? This theory supposes that we all act against better knowledge and, deep down, we all know that homeopathics diluted at a rate of 1:1000000000000000000000000000000000000000000000000000000000000 are effective. More loss of reality?, I ask myself.
- Becker has a strategy that he proudly admits to: he provokes people on Twitter to a point where they lose their nerve and reply something offensive. Armed with this statement, he then recruits a lawyer* and sues them for libel. He tried his trick recently likening several homeopathy-critics to Roland Freisler, the infamous judge of the Nazi era. Such actionable behaviour could be seen as a sign of a man in serious trouble – has Becker lost so much contact with reality that he does not realise that, in court, his insults would harm him and not his opponent?
- Or perhaps he misunderstood the prime dogma of homeopathy? ‘Like cures like’ does not mean one can cure criticism with aggression. I am sure that Hahnemann, who knew a fair bit about aggression, never said so.
- One of the most concerning features of homeopathy’s new defender is that Becker thinks anyone might believe him when he implies that, as a professional PR-man, he does a time-consuming PR-job for free. Yes, he did indicate that he conducts PR for homeopathy for a hobby. Would you find such behaviour normal?
So, should we be worried about the state of mind of homeopathy’s staunch defender? It might be too early to issue a final judgement on this question. But I am the first to admit that the signs are somewhat ominous. The man might need our help! Therefore, let me emphatically and empathetically stress this:
Mr Becker, if you read this – and I suspect you will – please stay calm. I know several good physicians who might be able to help you. And I promise, they will not prescribe a single homeopathic remedy!
*if you are one, please note this article is pure satire!
Traditional Chinese Medicine (TCM) is the umbrella term for modalities historically used in ancient China. TCM includes many therapeutic and some diagnostic modalities. Even though, these modalities differ in many respects, they are claimed to have in common that they are based on assumptions most of which originate from Taoist philosophy:
- The human body is a miniature version of the universe.
- Harmony between the two opposing forces, yin and yang, means health.
- Disease is caused by an imbalance between these forces.
- Five elements—fire, earth, wood, metal, and water—symbolically represent all phenomena, including the stages of human life, and explain the functioning of the body and how it changes during disease.
- The vital energy, qi or chi, flows through the body in meridians, is essential for maintaining health.
TCM is a construct of Mao Zedong who lumped all historical Chinese treatments together under this umbrella and created the ‘barefoot doctor’ to practice TCM nationwide – not because he believed in TCM, but because China was desperately short of real doctors and needed at least a semblance of healthcare.
Over the past few years, China has been aggressively promoting TCM for expanding its global influence and for a share of the estimated US$50-billion global market (of products of dubious quality). A recent article in ‘Nature’ explains that the WHO’s governing body, the World Health Assembly, is set to adopt the 11th version of the organization’s global compendium — known as the International Statistical Classification of Diseases and Related Health Problems (ICD). For the first time, the ICD will include information about TCM. Chapter 26 of the ICD will feature a classification system on TCM, largely based not on science or facts, but on obsolete nonsense.
The WHO’s support applies to all traditional medicines, but its relationship with Chinese medicine, and with China, has grown especially close, in particular during the tenure of Margaret Chan, who ran the organization from 2006 to 2017 and made sure that several documents favourable to TCM were passed. The WHO’s declarations about traditional medicine are puzzling. Various of these WHO documents call for the integration of “traditional medicine, of proven quality, safety and efficacy”, while being silent as to which traditional medicines and diagnostics are proven. Wu Linlin, a WHO representative in the Beijing office, told Nature that the “WHO does not endorse particular traditional and complementary medicine procedures or remedies”.
But this is evidently not the case and in sharp contrast to the WHO’s actions in other areas. The agency provides, for instance, specific advice on what vaccines and drugs to use and what foods to avoid. With traditional medicines, however, such specifics are missing. The message therefore can only be that the WHO endorses TCM as safe and effective.
The evidence, however, tells us a different story. On this blog, we have repeatedly discussed that:
- the clinical trials of TCM are often of poor quality,
- there are several good reasons why one has to be very sceptical about research coming out of China,
- critics are silenced,
- in general, the evidence on TCM is neither positive nor trustworthy.
China’s drug regulator gets more than 230,000 reports of adverse effects from TCM each year, and Chinese herbal medicines carry multiple direct risks:
- one or more ingredients can be toxic,
- some have been shown to be contaminated with toxic materials such as heavy metals,
- others are adulterated with synthetic drugs such as steroids,
- others again can interact with prescription drugs taken concomitantly,
- and not to forget, the risk for endangered species.
To this, we have to add the indirect risk of employing useless treatments for otherwise treatable conditions.
In view of all this, the WHO’s endorsement of TCM and its obsolete concepts is not just not understandable, it is a dangerous step backwards and, in my view, even intolerable.
Endocrine therapy (ET) is often used to reduce the risk of recurrence in hormone receptor-expressing disease. It is associated with worsening of climacteric symptoms can therefore have a negative impact on the quality of life (QoL) of those affected. Homeopathy is sometimes recommended for management of hot flushes (HF), and a new study aimed to test whether it is effective.
In this multi-centre, double-blind, placebo-controlled RCT, women were included suffering from histologically proven non-metastatic localized breast cancer, with Eastern Cooperative Oncology Group-Performance Status (ECOG-PS) ≤ 1, treated for at least 1 month with adjuvant ET, and complaining about moderate to severe HF. Patients scheduled for chemotherapy, or radiotherapy, or those with associated pathology known to induce HF were excluded. After a 2- to 4-week placebo administration, patients were randomly assigned to receiving the homeopathic medicine complex Actheane® (arm A) or placebo (arm P). Randomization was stratified by adjuvant ET (taxoxifen/aromatase inhibitor) and recruiting site. HF scores (HFS) were calculated as the mean of HF frequencies before randomization, at 4, and at 8 weeks post-randomization (pre-, 4w,- and 8w-) weighted by a 4-level intensity scale. The primary endpoint was the variation between pre- and 4week-HFS. Secondary endpoints included HFS variation between pre- and 8week-HFS. Compliance and tolerance were assessed 8 weeks after randomization, and QoL and satisfaction were assessed at 4- and 8-week post-randomization.
In total, 138 patients were randomized (A, 65; P, 73). Median 4week-HFS absolute variation (A, - 2.9; P, - 2.5 points, p = 0.756) and relative decrease (A, - 17%; P, - 15%, p = 0.629) were not statistically different between the two arms. However, 4week-HFS decreased for 46 (75%) in A vs 48 (68%) patients in P arm. 4week-QoL was stable or improved for respectively 43 (72%) vs 51 (74%) patients (p = 0.470).
The authors concluded that the efficacy endpoint was not reached, and BRN-01 administration was not demonstrated as an efficient treatment to alleviate HF symptoms due to adjuvant ET in breast cancer patients. However, the study drug administration led to decreased HFS with a positive impact on QoL. Without any recommended treatment to treat or alleviate the HF-related disabling symptoms, Actheane® could be a promising option, providing an interesting support for better adherence to ET, thereby reducing the risk of recurrence with a good tolerance profile.
At the start of their abstract, the authors state that homeopathy might allow a better management of hot flushes (HF). Frankly, I fail to see the evidence for this statement. The only study I know of (by a known advocate of homeopathy) showed no effect of homeopathy.
Acthéane is a mixture marketed by Boiron of 5 ingredients:
– Actaea racemosa 4 CH : 0,5 mg
– Arnica montana 4 CH : 0,5 mg
– Glonoinum 4 CH : 0,5 mg
– Lachesis mutus 5 CH : 0,5 mg
– Sanguinaria canadensis 4 CH : 0,5 mg
I am not aware of evidence that this remedy might work.
If there is no plausible rationale for conducting a study, does that not mean it is ethically questionable to do it?
Apart from that, the study seems well-designed. It is not very well presented, but the paper is clear enough. Its results are as one would expect from a rigorous trial of homeopathy. The fact that the authors try to squeeze out some positive messages from this squarely negative study is, of course, pathetic. To mention in the abstract that 4week-HFS decreased for 46 (75%) in A vs 48 (68%) patients (not the primary outcome measure) in P arm is little more than an embarrassing tribute to the sponsor, in my view.
Boiron Canada state on their website that Acteane® is a homeopathic medicine used for the relief of perimenopause and menopause symptoms such as hot flashes, night sweats, sleep disorders, headache, irritability and mood swings.
 The benefits of Acteane, a new solution for women:
The benefits of Acteane, a new solution for women:
• Hormone-free
• Soy-free
• Can be associated with other treatments used during perimenopause
• Non-drowsy
• Chewable tablets
• Does not require water
WILL THEY NOW ADD ‘EFFECT-FREE’ TO THEIR LIST?
Do musculoskeletal conditions contribute to chronic non-musculoskeletal conditions? The authors of a new paper – inspired by chiropractic thinking, it seems – think so. Their meta-analysis was aimed to investigate whether the most common musculoskeletal conditions, namely neck or back pain or osteoarthritis of the knee or hip, contribute to the development of chronic disease.
The authors searched several electronic databases for cohort studies reporting adjusted estimates of the association between baseline neck or back pain or osteoarthritis of the knee or hip and subsequent diagnosis of a chronic disease (cardiovascular disease , cancer, diabetes, chronic respiratory disease or obesity).
There were 13 cohort studies following 3,086,612 people. In the primary meta-analysis of adjusted estimates, osteoarthritis (n= 8 studies) and back pain (n= 2) were the exposures and cardiovascular disease (n=8), cancer (n= 1) and diabetes (n= 1) were the outcomes. Pooled adjusted estimates from these 10 studies showed that people with a musculoskeletal condition have a 17% increase in the rate of developing a chronic disease compared to people without a musculoskeletal condition.
The authors concluded that musculoskeletal conditions may increase the risk of chronic disease. In particular, osteoarthritis appears to increase the risk of developing cardiovascular disease. Prevention and early
treatment of musculoskeletal conditions and targeting associated chronic disease risk factors in people with long
standing musculoskeletal conditions may play a role in preventing other chronic diseases. However, a greater
understanding about why musculoskeletal conditions may increase the risk of chronic disease is needed.
For the most part, this paper reads as if the authors are trying to establish a causal relationship between musculoskeletal problems and systemic diseases at all costs. Even their aim (to investigate whether the most common musculoskeletal conditions, namely neck or back pain or osteoarthritis of the knee or hip, contribute to the development of chronic disease) clearly points in that direction. And certainly, their conclusion that musculoskeletal conditions may increase the risk of chronic disease confirms this suspicion.
In their discussion, they do concede that causality is not proven: While our review question ultimately sought to assess a causal connection between common musculoskeletal conditions and chronic disease, we cannot draw strong conclusions due to poor adjustment, the analysis methods employed by the included studies, and a lack of studies investigating conditions other than OA and cardiovascular disease…We did not find studies that satisfied all of Bradford Hill’s suggested criteria for casual inference (e.g. none estimated dose–response effects) nor did we find studies that used contemporary causal inference methods for observational data (e.g. a structured identification approach for selection of confounding variables or assessment of the effects of unmeasured or residual confounders. As such, we are unable to infer a strong causal connection between musculoskeletal conditions and chronic diseases.
In all honesty, I would see this a little differently: If their review question ultimately sought to assess a causal connection between common musculoskeletal conditions and chronic disease, it was quite simply daft and unscientific. All they could ever hope is to establish associations. Whether these are causal or not is an entirely different issue which is not answerable on the basis of the data they searched for.
An example might make this clearer: people who have yellow stains on their 2nd and 3rd finger often get lung cancer. The yellow fingers are associated with cancer, yet the link is not causal. The association is due to the fact that smoking stains the fingers and causes cancer. What the authors of this new article seem to suggest is that, if we cut off the stained fingers of smokers, we might reduce the cancer risk. This is clearly silly to the extreme.
So, how might the association between musculoskeletal problems and systemic diseases come about? Of course, the authors might be correct and it might be causal. This would delight chiropractors because DD Palmer, their founding father, said that 95% of all diseases are caused by subluxation of the spine, the rest by subluxations of other joints. But there are several other and more likely explanations for this association. For instance, many people with a systemic disease might have had subclinical problems for years. These problems would prevent them from pursuing a healthy life-style which, in turn, resulted is musculoskeletal problems. If this is so, musculoskeletal conditions would not increase the risk of chronic disease, but chronic diseases would lead to musculoskeletal problems.
Don’t get me wrong, I am not claiming that this reverse causality is the truth; I am simply saying that it is one of several possibilities that need to be considered. The fact that the authors failed to do so, is remarkable and suggests that they were bent on demonstrating what they put in their conclusion. And that, to me, is an unfailing sign of poor science.
 The AMERICAN INSTITUTE OF HOMEOPATHY (AIH) is the oldest national medical association in the United States. The AIH’s mission is “to promote the science and art of homeopathic medicine, to safeguard the interests of the homeopathic medical profession, to improve the standards of homeopathic medical education, to educate the medical and scientific communities about the scientific basis for homeopathic medicine, and to increase public knowledge and acceptance of homeopathy as a medical specialty.”
The AMERICAN INSTITUTE OF HOMEOPATHY (AIH) is the oldest national medical association in the United States. The AIH’s mission is “to promote the science and art of homeopathic medicine, to safeguard the interests of the homeopathic medical profession, to improve the standards of homeopathic medical education, to educate the medical and scientific communities about the scientific basis for homeopathic medicine, and to increase public knowledge and acceptance of homeopathy as a medical specialty.”
The AIH is about to hold its annual conference. This year’s theme is “Tackling Patients with Severe Pathology”. The announcement reads as follows:
Homeopathy has been found to be effective in the great majority of patients suffering from infectious and autoimmune diseases. The limits of homeopathic treatment are encountered in the treatment of patients with Parkinson’s disease, ALS and late-stage cancers. After finding a way to treat patients with Parkinson’s disease with homeopathy, Dr. Saine began to apply this approach to cancer patients in stages III and IV. In this seminar, he will review case analysis, posology and case management for this cohort of patients.
We are fortunate to have the opportunity to learn from Dr. Saine in this seminar. He is recognized as one of the foremost homeopathic teachers and clinicians in the world, with special expertise in extremely difficult cases of severe and advanced pathology.
Who, for heaven sake, is this foremost homeopathic teachers and clinicians in the world, Dr Saine?, I asked myself after reading this (and even more so after listening to the rather spectacular video provided with the announcement). Here is what I found out about him:
Dr. Saine is a 1982 graduate of the National College of Naturopathic Medicine in Portland, Oregon. He is board-certified in homeopathy (1988) by the Homeopathic Academy of Naturopathic Physicians and has been teaching and lecturing on homeopathy since 1985. He is considered one of the world’s foremost experts on the subject of homeopathy.
And this is what non-doctor* Saine writes about medicine etc.:
The Organon of Medicine is a blueprint on how to practice medicine rationally and wisely through an integration of all the fundamental principles of medicine into a comprehensive whole. Unfortunately, to the detriment of the sick, very few homeopaths have delved, as Hahnemann did, into the practice of lifestyle medicine and the use of complementary care to homeopathy.
With rare exceptions, patients will present with a portion of their disease that ensues from an unhealthy environment or ways of living. The role of the physician is to determine in the equation of disease what is primarily due to an untuned vital force versus a causa occasionalis, as both will have to be addressed in due time.
After reading and listening to all this I am mildly shocked.
It does not seem to me that the AIH is fit for purpose. Neither am I convinced that non-doctor Saine should be let near any patient, let alone one with cancer or another severe pathology.
There should be a law protecting patients from this sort of thing!
[*in the context of healthcare, a doctor is for me someone who has studied medicine]Fish oil (omega-3 PUFA) preparations are today extremely popular and amongst the best-researched dietary supplement. During the 1970s, two Danish scientists, Bang and Dyerberg, remarked that Greenland Eskimos had a baffling lower prevalence of coronary artery disease than mainland Danes. They also noted that their diet contained large amounts of seal and whale blubber and suggested that this ‘Eskimo-diet’ was a key factor in the lower prevalence. Subsequently, a flurry of research stared to investigate the phenomenon, and it was shown that the ‘Eskimo-diet’ contained unusually high concentrations of omega-3 polyunsaturated fatty acids from fish oils (seals and whales feed predominantly on fish).
Initial research also demonstrated that the regular consumption of fish oil has a multitude of cardiovascular and anti-inflammatory effects. This led to the promotion of fish oil supplements for a wide range of conditions. Meanwhile, many of these encouraging findings have been overturned by more rigorous studies, and the enthusiasm for fish oil supplements has somewhat waned. But now, a new paper has come out with surprising findings.
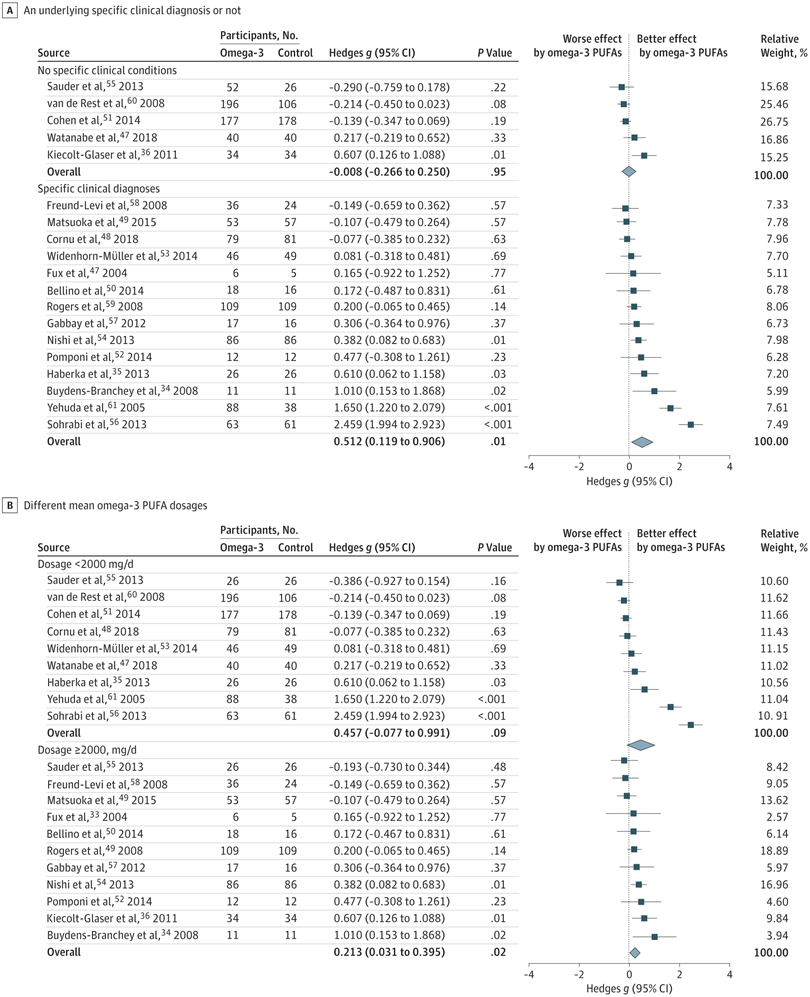
The objective of this meta-analysis was to evaluate the association of anxiety symptoms with omega-3 PUFA treatment compared with controls in varied populations.
A search was performed of clinical trials assessing the anxiolytic effect of omega-3 PUFAs in humans, in either placebo-controlled or non–placebo-controlled designs. Of 104 selected articles, 19 entered the final data extraction stage. Two authors independently extracted the data according to a predetermined list of interests. A random-effects model meta-analysis was performed. Changes in the severity of anxiety symptoms after omega-3 PUFA treatment served as the main endpoint.
In total, 1203 participants with omega-3 PUFA treatment and 1037 participants without omega-3 PUFA treatment showed an association between clinical anxiety symptoms among participants with omega-3 PUFA treatment compared with control arms. Subgroup analysis showed that the association of treatment with reduced anxiety symptoms was significantly greater in subgroups with specific clinical diagnoses than in subgroups without clinical conditions. The anxiolytic effect of omega-3 PUFAs was significantly better than that of controls only in subgroups with a higher dosage (at least 2000 mg/d) and not in subgroups with a lower dosage (<2000 mg/d).
The authors concluded that this review indicates that omega-3 PUFAs might help to reduce the symptoms of clinical anxiety. Further well-designed studies are needed in populations in whom anxiety is the main symptom.
I think this is a fine meta-analysis reporting clear results. I doubt that this paper truly falls under the umbrella of alternative medicine, but fish oil is a popular food supplement and should be mentioned on this blog. Of course, the average effect size is modest, but the findings are nevertheless intriguing.