A chiro, a arms dealer and a Brexit donor meet in a bar.
The arms dealer: my job is so secret, I cannot tell my neighbour what I do.
The Brexit donor: I have to keep things so close to my chest that not even my wife knows what I am doing.
The chiro: that’s nothing; my work is so secret that not even I know what I am doing.
CHILDISH, I KNOW!
But I am yet again intrigued by a survey aimed at finding out what chiropractors are up to. One might have thought that, after 120 years, they know what they are doing.
This survey described the profiles of chiropractors’ practice and the reasons, nature of the care provided to their patients and extent of interprofessional collaborations in Ontario, Canada. The researchers randomly recruited chiropractors from a list of registered chiropractors (n=3978) in active practice in 2015. Of the 135 randomly selected chiropractors, 120 were eligible, 43 participated and 42 completed the study.
Each chiropractor recorded information for up to 100 consecutive patient encounters, documenting patient health profiles, reasons for encounter, diagnoses and care provided. Descriptive statistics summarised chiropractor, patient and encounter characteristics, with analyses accounting for clustering and design effects. Thus data on 3523 chiropractor-patient encounters became available. More than 65% of participating chiropractors were male, mean age 44 years and had practised on average 15 years. The typical patient was female (59% of encounters), between 45 and 64 years (43%) and retired (21%) or employed in business and administration (13%). Most (39.4%) referrals were from other patients, with 6.8% from physicians. Approximately 68% of patients paid out of pocket or claimed extended health insurance for care. Most common diagnoses were back (49%, 95% CI 44 to 56) and neck (15%, 95% CI 13 to 18) problems, with few encounters related to maintenance/preventive care (0.86%, 95% CI 0.2 to 3.9) and non-musculoskeletal problems (1.3%, 95% CI 0.7 to 2.3). The most common treatments included spinal manipulation (72%), soft tissue therapy (70%) and mobilisation (35%).
The authors concluded that this is the most comprehensive profile to date of chiropractic practice in Canada. People who present to Ontario chiropractors are mostly adults with a musculoskeletal condition. Our results can be used by stakeholders to make informed decisions about workforce development, education and healthcare policy related to chiropractic care.
I am so sorry to have mocked this paper. I shouldn’t have, because it actually does reveal a few interesting snippets:
- Only 7% of referrals come from real doctors.
- The vast majority of all patients receive spinal manipulations.
- About 6% of them are under 14 years of age.
- Chiropractors seem to dislike surveys; only 35% of those asked complied.
- 23% of all consultations were for general or unspecified problems,
- 8% for neurologically related problems,
- 5% for non-musculoskeletal problems (eg, digestive, ear, eye, respiratory, skin, urology, circulatory, endocrine and metabolic, psychological).
- Chiropractors rarely refer patients to other clinicians; this only happened in less than 3% of encounters.
- Apart from manipulation, chiropractors employ all sorts of other dubious therapies (ultrasound 3%, acupuncture 3%, , traction 1%, interferential therapy 3%, soft laser therapy 3%).
- 68% of patients pay out of their own pocket…
… NO WONDER, THEY DO NOT SEEM TO BE IN NEED OF ANY TYPE OF TREATMENT: 54% of all patients reported being in “excellent/very good overall health”!
After yesterday’s low light, I am in need of cheering up.
Here we go:
John Ioannidis is a pioneer of meta-research, i.e. research on published research papers. Through this work, he has made seminal contributions to evidence-based medicine. I have met John just once; this was when we were both on the panel creating the PRISMA guidelines. Recently, he and his colleagues published a publicly available database of 100,000 top researchers of all scientific disciplines. Researchers who have published more than just a couple of articles can thus look up where exactly they are ranked amongst 100 000 other scientist.
The resource can also be used for multiple other purposes. For instance, the journal NATURE just published this comment about it: The world’s most-cited researchers, according to newly released data, are a curiously eclectic bunch. Nobel laureates and eminent polymaths rub shoulders with less familiar names, such as Sundarapandian Vaidyanathan from Chennai in India. What leaps out about Vaidyanathan and hundreds of other researchers is that many of the citations to their work come from their own papers, or from those of their co-authors…
As you might imagine, the temptation to locate myself in this list of the ‘100 000 best’ proved irresistible. To my utter surprise (and, of course, delight) I found my name on rank 97 of Ioannidis’ ‘composite score’. This means that I am amongst the 100 most cited scientists worldwide. Only 8 other scientists from the UK and globally only 4 other researchers in the category of ‘general & internal medicine’ are in this group. Nobody in Ioannidis’ list of ‘the top 100’ is a researcher of so-called alternative medicines (SCAM). (And Exeter appears again only in the low thousands.)
I find this truly exciting, especially as this is not the only indicator of the standing of our (yes, it is important to stress that much of it was team-work) SCAM research. Another 2019 paper demonstrated that mine was the ‘leading institution’ in homeopathy research. And a 2001 analysis had shown that my unit was the most productive team worldwide doing SCAM research.

School of Music: Blowing Your Own Trumpet.
But what does all this mean? Does it suggest that I am infallible and cannot be wrong? Does it mean that I am immune to cognitive biases that cloud our judgements?
No, certainly not!
Like anyone else, I am prone to getting things wrong, to making mistakes and to being fooled by my own prejudices. And yes, like everyone else, I did make mistakes in the past, plenty of them!
Evidently, I had to learn the skill of critical thinking the hard way, but it certainly was worth it. Critical thinking leads to wiser decisions and to a better, more responsible life. This is why I want more people to try it.
And this is why I spend so much time and effort publishing this blog.
The ‘OFFICIAL HOMEOPATHY RESOURCE‘ is an odd publication which, until very recently, I did not know about. They inform us about homeopathy as follows:
Homeopathy is a non-corporate 200-year-old system of medicine used successfully by tens of millions worldwide, and the second most utilized complementary health discipline in the world (according to the World Health Organization 2005). It has a laudable 200-year clinical record. There are literally hundreds of high quality basic science, pre-clinical and clinical studies showing it works.
This is the online web site for accurate information on homeopathy, homeopaths and homeopathic organizations. Its hard to get accurate information on this popular and traditional healing modality as a result of Drug Company Sponsored Blogs, Web Sites and their sponsored “Science Writers”.
Finally, there is a positive and comprehensive resource and you have found it. We hope you enjoy this site’s information and decide on or continue homeopathic treatment to experience it’s benefits.
THIS IS AN INDEPENDENT MEDIA SOURCE
About Comments on this Web Site:
We welcome POSITIVE comments about your experience with homeopathy or positive feedback about a particular topic.
Thank you for your positive support of homeopathy and getting the word out there.
The articles and posts contained herein are educational and informational and should not be considered medical advise. We recommend that you see a licensed medical practitioner.
__________________________________________________________
So far so good; well not SO good actually: this short text opens a lot of questions. But this is not what I want to address today. The ‘OFFICIAL HOMEOPATHY RESOURCE’ appeared on my screen only for one reason; they just published a whole, albeit short article about me! It is entitled ‘Pharmaceutical Company Found Guilty of Fuelling Opioid Epidemic But Sponsored Skeptics Continue Attacks on Safe Alternatives‘. Here it is in its full and unabbreviated beauty:
Even though the pharmaceutical industry has paid billions in fines over the years for failures and deceptions that have caused serious injuries and death, the pharmaceutical sponsored skeptic organizations and skeptics like Edzard Ernst spread outright lies about the false dangers of alternatives. They try to take the heat off the failures and dangers of drugs by smearing safe alternatives like homeopathy. They even go to the point of going to government organizations and falsely claiming alternatives are dangerous. They say nothing or a minimum about their sponsors.
One such skeptic Edzard Ernst attempts to present himself as an expert which most skeptics do. As a means of puffing himself up and making it seemed like he knows something about homeopathy, he claimed he was a homeopath and switched to allopathic medicine when homeopathy did not work. This has been proven to be an outright lie. He has had no training in homeopathy.
Unfortunately skeptics, like lemmings, support only pharmaceutical company generated science as if it was the holy grail.
Homeopathy has been proven to be very effective in pain relief and is non-addictive.
_____________________________________________________________________
I am afraid they must have missed what I disclosed repeatedly about my sponsors. Let me therefore repeat it especially for them (I tried to find out who exactly ‘THEY’ are, but they are not disclosing this information, as far as I can see):
- I am sponsored to the tune of zero £.
- There is not a single commercial company that backs me.
- This blog receives no funding from anywhere.
- Its running costs are paid by me.
- I live off my pension and savings and receive no other income.
I will not bother to correct the other falsehoods in the text above. I think, they are too obvious to bother. To those of my readers who find them not obvious, I recommend reading my memoir and my book entitled ‘Homeopathy, the Undiluted Facts‘ and considering ‘Ernst’s law‘.
Apparently, Hahnemann gave a lecture on the subject of veterinary homeopathy in the mid-1810s. Ever since, homeopathy has been used for treating animals. Von Boennighausen was one of the first influential proponents of veterinary homeopathy. However, veterinary medical schools tended to reject homoeopathy, and the number of veterinary homeopaths remained small. In the 1920ies, veterinary homoeopathy was revived in Germany. Members of the “Studiengemeinschaft für tierärztliche Homöopathie” (Study Group for Veterinary Homoeopathy) which was founded in 1936 started to investigate this approach systematically.
Today, veterinary homeopathy is still popular in some countries. Prince Charles has become a prominent advocate who claims to treat his own life stock with homeopathy. In many countries, veterinary homeopaths have their own professional organisations. Elsewhere, however, veterinarians are banned from practicing homeopathy. In the UK, only veterinarians are allowed to use homeopathy on animals (but anyone regardless of background can use it on human patients) and there is a British Academy of Veterinary Homeopathy. In the US, homeopathic vets are organised in the Academy of Veterinary Homeopathy.
If this sounds promising, we should not forget that, as discussed so often on this blog, homeopathy lacks plausibility the evidence for veterinary homeopathy fails to be positive (see for instance here). But, hold on, there is a new study, perhaps it will change everything?
This ‘study‘ was aimed at providing an initial insight into the existing prerequisites on dairy farms for the use of homeopathy (i.e. the consideration of homeopathic principles) and on homeopathic treatment procedures (including anamnesis, clinical examination, diagnosis, selection of a remedy, follow-up checks, and documentation) on 64 dairy farms in France, Germany and Spain.
The use of homeopathy was assessed via a standardised questionnaire during face-to-face interviews. The results revealed that homeopathic treatment procedures were applied very heterogeneously and differed considerably between farms and countries. Farmers also use human products without veterinary prescription as well as other prohibited substances.
The authors of this ‘study’ concluded that the subjective treatment approach using the farmers’ own criteria, together with their neglecting to check the outcome of the treatment and the lack of appropriate documentation is presumed to substantially reduce the potential for a successful recovery of the animals from diseases. There is, thus, a need to verify the effectiveness of homeopathic treatments in farm practices based on a lege artis treatment procedure and homeopathic principles which can be achieved by the regular monitoring of treatment outcomes and the prevailing rate of the disease at herd level. Furthermore, there is a potential risk to food safety due to the use of non-veterinary drugs without veterinary prescription and the use of other prohibited substances.
So did this ‘study’ change the evidence on veterinary homeopathy?
Sadly not!
This ‘study’ is hardly worth the paper it is printed on.
Who conceives such nonsense?
And who finances such an investigation?
The answer to the latter question is one of the few provided by the authors: This project has received funding from the European Union’s Seventh Framework Programme for research, technological development and demonstration under Grant Agreement No 311824 (IMPRO).
Time for a constructive suggestion! Could the European Union’s Seventh Framework Programme with their next research project in veterinary homeopathy please evaluate the question why farmers in the EU are allowed to use disproven therapies on defenceless animals?
Dr Tony Pinkus has been featured on this blog before. The reason for this is that he claimed – falsely, of course – I have ‘faked’ research data. Recently, he re-appeared on my radar when he (or another spokesperson of his firm) was quoted in The Telegraph accusing me of ‘ignorance’. Subsequently, Mr Ullman published this letter by Pinkus to the TIMES journalist, Rosie Taylor, in the comments section of my previous blog-post:
Dear Rosie,
Its clearly a very slow summer as this is a very old story being peddled by an arch skeptic of homoeopathy who is little more than a charlatan himself.
The well respected researcher Professor Robert Hahn recently stated, at a research conference in London, that, in order to agree with Ernst’s castigation of homoeopathy you would literally have to ignore over 90% of the high quality research material already published.
Ernst has made a name for himself by criticising homoeopathy and attacking HRH The Prince of Wales for his life long support of the therapy. Meanwhile this upstart, with an unhealthy interest in Nazi medicine, has risen to prominence by taking a position as the first professor of complementary medicine in a chair supported wholly by a British philanthropist who provided the money based on his beneficial experiences of homoeopathy.
To comment on a single remedy without context or appreciation of the wider principles of the subject would be akin to understanding how your car works by examining the tread of the near side tyre. As such I refuse to lend currency to his idiocy and your paper’s promotion of it as science. He has no understanding of the principles and continues to demonstrate his ignorance with ludicrous remarks. This is scientism not science.
Under his misguidance of a bunch of ignorant sceptics, a large number or poor and aged patients have been deprived of the benefits of homoeopathy on the NHS, hitherto available since the inception of the system in 1948. Five private hospitals dedicated to homoeopathic practice, that were built by private donations from wealthy benefactors were ceded to the NHS have been lost as a result.
In a crucial time when antibiotics are failing and we need more natural solutions people like Ernst are masquerading as heroes when in fact they are villains.
Kind regards
Tony Pinkus
Director
Ainsworths
_______________________________________________________________
 Naturally, I wanted to learn more about a man who can compose such charming letters. Who exactly is he, and what brings him to putting such liable nonsense on paper? Here is how Pinkus describes himself:
Naturally, I wanted to learn more about a man who can compose such charming letters. Who exactly is he, and what brings him to putting such liable nonsense on paper? Here is how Pinkus describes himself:
Tony Pinkus qualified as a pharmacist in 1980 and accepted the offer to take over Ainsworths Homeopathic Pharmacy when John Ainsworth retired in 1989. Having learnt from John Ainsworth, Tony went on to teach homoeopathic practitioners including doctors, vets, and dentists at both the Faculty of Homoeopathy and The College of Homoeopathic Education amongst others both in the UK and overseas. Tony has co-written five books on the homoeopathic treatment of animals with homoeopathic vet Mark Elliott and herdsman Philip Handsford. He also wrote self-help books for the kits and a self-help, interactive computer program for the OTC range. Tony is the grantee of two Royal Warrants of Appointment to HM The Queen and HRH The Prince of Wales and previously HM The Queen Mother. In this position he is consulted on matters concerning homoeopathic remedies by The Royal Family.
Interesting?
Not really!
But I did find something that fascinated me: a pilot study of homeopathy for children with autism and ASD which Pinus conducted in 1998 and published in 2015. Here are some excerpts from it:
Over 3000 children received homoeopathic secretin sufficient for the period of the pilot study and each parent received a questionnaire to complete and return. Oral reports were received from 6 weeks to 18 months during which homoeopathic secretin was in continual use. Written reports were received from a number of patients and 159 completed questionnaires were returned, forming the basis of the graph below. This number was less than expected but nonetheless representative of the responses obtained by continued contact with the patient group.
CONCLUSIONS
The results demonstrate an incremental benefit from possible to moderate change observed in 12 key symptoms of ASD over the seven weeks of recording. There is a clear variation in benefit over the symptom range and direct communication faculties improve more significantly than behavior patterns. Eye contact and vocalization being the most profound and immediate changes observed. Continued use beyond the study period maintained the upward trend demonstrated in the first seven weeks. The individual variation in response between patients was also quite large with some children fairing well above average and others below average, hence the results understate the actual picture that can occur, whilst it must be appreciated that secretin will not help all cases. The negative value for a worsening of symptoms was unwise in retrospect as this is generally indicative of a positive outcome with homoeopathic treatment and in experience undervalued the outcome of the symptom when further examined.
The modest aim of this pilot study was met insofar that a large sample size, far greater than in any trial to date, reported incremental beneficial improvement to their ASD symptoms over a seven week period with many concurrent reports of a profound change in the child as a whole person. Many children were able to reduce stringent diets or stop taking Ritalin and Risperidone as a consequence of taking secretin. At least one report has been received of a child taking homoeopathic secretin for over seven years
As to why homoeopathy has been less successful than anticipated, the results indicate a clear reason. Each meal that a child consumes acts as a maintaining cause for their symptoms and as such a block to individually chosen treatment. By taking a regular dose of homoeopathic secretin the maintaining cause is offset enabling other remedies to act more significantly. In addition it became apparent that increasing size of dose increases effect (2-6 drops) and this was necessary over longer term use of the remedy. Homoeopathic secretin was also found to potentiate the action of the injected secretin, in particular increasing its longevity from six to nine weeks.
The outcome of this study has been discussed with many homoeopathic practitioners who have as a consequence changed their management of ASD cases. It has also promoted a further clinical pilot study of the use of homoeopathic secretin in autistic adolescents.
_____________________________________________________________________
Pinkus added comments to his pilot study, evidently made at the time of its publication (2015). There I found this remarkable statement: ‘If you look at Wakefields work here it fits in nicely.’
Here I don’t want to comment on the abysmal quality of Pinkus’ study (too obvious to mention, I think). What I do want to mention, however, is the fact that, in his study, I don’t find any mention of an approval from an ethics committee to carry out this study. Could it be that I have missed it? Or might Pinus be in violation of research ethics? If the latter is the case, should the Royal Warrants (see above) not be withdrawn as a matter of urgency? After all, it is Pinkus personally who ‘is the grantee of two Royal Warrants of Appointment to HM The Queen and HRH The Prince of Wales’!
I have written about this more often than I care to remember, and today I do it again.
Why?
Because it is important!
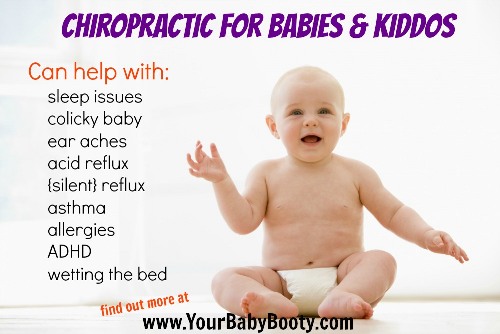
Chiropractic is not effective for kids, and chiropractic is not harmless for kids – what more do we need to conclude that chiropractors should not be allowed anywhere near them?
And most experts now agree with this conclusion; except, of course, the chiropractors themselves. This recent article in THE CHRONICLE OF CHIROPRACTIC is most illuminating in this context:
It was only a matter of time before the attack on the chiropractic care of children spread to the United States from Australia and Canada and its also no surprise that insurance companies would jump on the bandwagon first. According to Blue Cross and Blue Shield Children under the age of 5 years should not receive chiropractic care (spinal manipulation) ” . . . because the skeletal system is not mature at this time.”
The Blues further contend that:
“Serious adverse events may be associated with pediatric spinal manipulation in children under the age of 5 years due to the risks of these procedures in children this age.”
The Blues claims that their determination is based on standards of care – though they do not state which ones.
“This determination was based on standards of care in pediatric medicine as well as current medical evidence.”
This is not the first time Blue Cross attacked the chiropractic care of children. In 2005 CareFirst Blue Cross claimed that:
“Spinal manipulation services to treat children 12 years of age and younger, for any condition, is considered experimental and investigational.”
The ridiculous and false claims by Blue Cross come on the heels of a ban placed on spinal manipulation of infants by the Chiropractic Board of Australia (see related story) and attacks on chiropractors who care for children in Canada by chiropractic regulatory boards there.
There is in fact plenty of evidence to support the chiropractic care of infants and children and there are practice guidelines (the highest level on the research hierarchy pyramid) that support such care.
The real issue is not whether or not evidence exists to support the chiropractic care of children – the real issue is power and the lack of any necessity for evidence for those with the power.
__________________________________________________________________
END OF QUOTE
What can we learn from this outburst?
- Chiropractors often take much-needed critique as an ‘attack’. My explanation for this phenomenon is that they sense how wrong they truly are, get defensive, and fear for their cash-flow.
- When criticised, they do not bother to address the arguments. This, I believe, is again because they know they are in the wrong.
- Chiropractors are in denial as to what they can and cannot achieve with their manipulations. My explanation for this is that they might need to be in denial – because otherwise they would have to stop practising.
- They often insult criticism as ridiculous and false without providing any evidence. The likely explanation is that they have no reasonable evidence to offer.
- All they do instead is stating things like ‘there is plenty of evidence’. They don’t like to present the ‘evidence’ because they seem to know that it is worthless.
- Lastly, in true style, they resort to conspiracy theories.
To any critical thinker their behaviour thus makes one conclusion virtually inescapable: DON’T LET A CHIROPRACTOR NEAR YOUR KIDS!
An abstract from the recent ‘2nd OFFICIAL SIPS CONFERENCE ON PLACEBO STUDIES’ caught my attention. It is not available on-line; therefore let me reproduce it here in full:
The role of placebo effects in mindfulness-based analgesia 1. Jonathan Davies. University of Sydney, Sydney, NSW, Australia. 2. Louise Sharpe. University of Sydney, Sydney, NSW, Australia. 3. Melissa Day. University of Queensland, Brisbane, QLD, Australia. 4. Ben Colagiuri. University of Sydney, Sydney, NSW, Australia.
Background: Mindfulness meditation can reduce pain both in experimental and clinical settings, though it is not known to what extent mindfulness-specific vs placebo-like expectancy effects account for these changes. This study aimed to: 1. establish whether placebo effects contribute to mindfulness-mediated analgesia; and 2. identify putative cognitive mechanisms responsible for placebo- vs mindfulness-mediated analgesia. Methods: We compared the effects of focussed-attention mindfulness training (6 x 20 min), sham mindfulness, and a no-treatment in a double-blind RCT for experimental heat pain. Sham mindfulness instructions lacked the ‘active ingredients’ of the real training but were matched on all other contextual factors. Results: Both real and sham mindfulness training led to greater pain tolerance relative to no treatment, but there was no difference between the real and sham training. This was accompanied by increased expectancy, beliefs, and pain-related cognitive processes in the two mindfulness groups relative to no treatment, but again there were no differences between real and sham training on these outcomes. There were no effects on pain intensity, pleasantness or threshold. Conclusion: These findings suggest that mindfulness training – at least those involving focused-attention – may lead to improved pain tolerance via the placebo effect rather than any specific mindfulness-related mechanisms. Potential mediators of these effects will be discussed.

I find this study remarkable in two ways:
- It shows that, with a bit of fantasy, ingenuity and will, one can design and use sham procedures even in clinical trials of mind/body therapies.
- Its results suggest that, if one does control for placebo effects, these treatments may not prove to be more than a placebo therapy.
What implications might this have for clinical practice?
Mindfulness is currently hugely popular. It would not be surprising, if the news that it might rely purely on placebo effects would calm down the enthusiasm about this treatment. Many might ask, does it matter? As long as patients benefit, the mechanism of action seems irrelevant. This, of course, is an interesting debate which we have had on this blog many times before.
What do you think?
Yesterday, I had the honour and pleasure to present to the UK press my new book entitled ‘ALTERNATIVE MEDICINE, A CRITICAL ASSESSMENT OF 150 MODALITIES’ (see also my previous post). The SCIENCE MEDIA CENTRE had invited me to do a ‘media briefing’ on the occasion of its publication. I did this by outlining the background around so-called alternative medicine (SCAM) and explaining the concept of the new book which essentially is – as its title indicates – to provide concise and critical assessments of 150 modalities.
In the course of my short presentation, I mentioned the following exotic modalities in order to show that my book goes beyond the ‘usual suspects’ of acupuncture, chiropractic, etc.:
- BERLIN WALL
- COLLOIDAL SILVER
- PALEO DIET
- PLACENTOPHAGY
- URINE THERAPY
- CUPPING
- GUA SHA
- LYMPH DRAINAGE
- SLAPPING THERAPY
- VISCERAL OSTEOPATHY
- JOHREI HEALING
- LEECH THERAPY
- NEURAL THERAPY
- ZERO BALANCE
- APPLIED KINESIOLOGY
- IRIDOLOGY
- LIVE BLOOD ANALYSIS
- PULSE DIAGNOSIS
- RADIONICS
As it turned out, the journalists present found the BERLIN WALL remedy the most fascinating aspect of my talk. And this is clearly reflected in today’s articles covering the event:
The DAILY TELEGRAPH published an article much in the same vein, and so did THE SUN and the EXPRESS (not available on line). The only UK newspaper I have seen so far going beyond the Berlin Wall topic is THE DAILY MAIL. The paper mentions several other so-called alternative medicines (SCAMs) that consumers need to be protected from, in my view.
Interestingly, none of the articles mentioned that my new book is not an exercise in debunking. During my presentation, I made the point that several of my assessments of 150 modalities do arrive at positive conclusions for therapies that demonstrably generate more good than harm.
I also tried to point out to the journalists that SCAM includes a range of diagnostic techniques. None of them are valid which means that they present a real danger to consumers through false-positive and false-negative diagnoses. In particular the latter scenario can cost lives.
All in all, I did enjoy yesterday’s press briefing very much. I am aware of the fact that, in the realm of SCAM, the press have a most important role to play. Consumers rarely consult their doctor when deciding to use SCAM; frequently they go by what they read in the papers.
In this context, I find it noteworthy that, during the last years, the UK press have become considerably more sceptical. Not so long ago, most UK journalists used to praise SCAM like the best thing since sliced bread; today this attitude has laudably shifted towards a more rational stance. I am sure that the excellent work of the SCIENCE MEDIA CENTRE has played a crucial part in this positive development.
The journal NATURE has just published an excellent article by Andrew D. Oxman and an alliance of 24 leading scientists outlining the importance and key concepts of critical thinking in healthcare and beyond. The authors state that the Key Concepts for Informed Choices is not a checklist. It is a starting point. Although we have organized the ideas into three groups (claims, comparisons and choices), they can be used to develop learning resources that include any combination of these, presented in any order. We hope that the concepts will prove useful to people who help others to think critically about what evidence to trust and what to do, including those who teach critical thinking and those responsible for communicating research findings.
Here I take the liberty of citing a short excerpt from this paper:
CLAIMS:
Claims about effects should be supported by evidence from fair comparisons. Other claims are not necessarily wrong, but there is an insufficient basis for believing them.
Claims should not assume that interventions are safe, effective or certain.
- Interventions can cause harm as well as benefits.
- Large, dramatic effects are rare.
- We can rarely, if ever, be certain about the effects of interventions.
Seemingly logical assumptions are not a sufficient basis for claims.
- Beliefs alone about how interventions work are not reliable predictors of the presence or size of effects.
- An outcome may be associated with an intervention but not caused by it.
- More data are not necessarily better data.
- The results of one study considered in isolation can be misleading.
- Widely used interventions or those that have been used for decades are not necessarily beneficial or safe.
- Interventions that are new or technologically impressive might not be better than available alternatives.
- Increasing the amount of an intervention does not necessarily increase its benefits and might cause harm.
Trust in a source alone is not a sufficient basis for believing a claim.
- Competing interests can result in misleading claims.
- Personal experiences or anecdotes alone are an unreliable basis for most claims.
- Opinions of experts, authorities, celebrities or other respected individuals are not solely a reliable basis for claims.
- Peer review and publication by a journal do not guarantee that comparisons have been fair.
COMPARISONS:
Studies should make fair comparisons, designed to minimize the risk of systematic errors (biases) and random errors (the play of chance).
Comparisons of interventions should be fair.
- Comparison groups and conditions should be as similar as possible.
- Indirect comparisons of interventions across different studies can be misleading.
- The people, groups or conditions being compared should be treated similarly, apart from the interventions being studied.
- Outcomes should be assessed in the same way in the groups or conditions being compared.
- Outcomes should be assessed using methods that have been shown to be reliable.
- It is important to assess outcomes in all (or nearly all) the people or subjects in a study.
- When random allocation is used, people’s or subjects’ outcomes should be counted in the group to which they were allocated.
Syntheses of studies should be reliable.
- Reviews of studies comparing interventions should use systematic methods.
- Failure to consider unpublished results of fair comparisons can bias estimates of effects.
- Comparisons of interventions might be sensitive to underlying assumptions.
Descriptions should reflect the size of effects and the risk of being misled by chance.
- Verbal descriptions of the size of effects alone can be misleading.
- Small studies might be misleading.
- Confidence intervals should be reported for estimates of effects.
- Deeming results to be ‘statistically significant’ or ‘non-significant’ can be misleading.
- Lack of evidence for a difference is not the same as evidence of no difference.
CHOICES:
What to do depends on judgements about the problem, the relevance (applicability or transferability) of evidence available and the balance of expected benefits, harm and costs.
Problems, goals and options should be defined.
- The problem should be diagnosed or described correctly.
- The goals and options should be acceptable and feasible.
Available evidence should be relevant.
- Attention should focus on important, not surrogate, outcomes of interventions.
- There should not be important differences between the people in studies and those to whom the study results will be applied.
- The interventions compared should be similar to those of interest.
- The circumstances in which the interventions were compared should be similar to those of interest.
Expected pros should outweigh cons.
- Weigh the benefits and savings against the harm and costs of acting or not.
- Consider how these are valued, their certainty and how they are distributed.
- Important uncertainties about the effects of interventions should be reduced by further fair comparisons.
__________________________________________________________________________
END OF QUOTE
I have nothing to add to this, except perhaps to point out how very relevant all of this, of course, is for SCAM and to warmly recommend you study the full text of this brilliant paper.
The ‘College of Medicine and Integrated Health’ (CMIH) has been the subject of several previous blog posts (see for instance here, here and here). Recently, they have come up with something new that, in my view, deserves a further comment.
The new ‘SELF CARE TOOL KIT’ began, according to the CMIH, in 2009 with a national multi-centre project commissioned by the UK Department of Health, to consider the best way to integrate self care into family practice. The project involved two large family health centres and two university departments. One output was the Self Care Library (SCL).
The Self Care Library (SCL) is an online patient resource providing free evidence-based information about self-care. The funding for the SCL did, however, not survive, and the facility was assigned to the CMIH. Thanks to funding from ‘Pukka Herbs Vitamins, Herbal Remedies & Health Supplements‘, the CMIH was able to transfer the content and to begin updating entries. Simon Mills, the coordinator of the original project who is now employed by Pukka, has led this transformation and helped the College set up the new parent portal, Our Health Directory.
The Self Care Toolkit is thus the new SCL. All concerned with this project are experienced in clinical practice and can separate the theory from real life needs. We all have academic lives as well so can be hard-nosed with the evidence base as well.
_______________________________________________________________
The above text is essentially based on the information provided by the CMIH. A few critical remarks and clarifications might therefore be in order:
- What does ‘separate the theory from real life needs’ mean? Does it mean that the scientific evidence can be interpreted liberally (see below)?
- Is it a good idea to have a commercial sponsor for such a project?
- Is it wise that the main person in charge is on the payroll of a manufacturer of dietary supplements?
- Is there any oversight to minimise undue bias and prevent the public from being misled?
- Is it really true that all people involved have academic lives? Simon Mills (who once was a member of my team) has no longer an academic appointment, as far as I know.
But, you are right, these are perhaps mere trivialities. Let’s see what the ‘Self Care Tool Kit’ actually delivers. I have chosen the entry on DEPRESSION to check its validity. Here it is:
_______________________________________________________________
It isn’t likely that taking extra vitamins will make much difference to low mood or depression. It is true that many people don’t get quite enough B, C and D vitamins in their food. And it’s also true that the brain and nervous system need these vitamins. Because they don’t get stored in the body, our daily diet has to supply them. Research has shown that people with low blood levels of the B vitamin folic acid are more likely to be depressed and less likely to do well on anti-depressant medicines. So, if you are eating a very poor diet, taking extra vitamins just might help. It’s also worth remembering that alcohol, refined sugars, nicotine and caffeine all take these vitamins out of the body. Yet most people who feel depressed probably won’t benefit from taking vitamins alone. To ensure that you get a good balance of these vitamins, try to eat more whole-foods, fruits, vegetables, nuts and seeds.
Some people say that taking high doses of vitamin C (1-2 g and more a day) helps lift their mood. There is a little research to support this and none showing that high doses of vitamin C actually help clinical depression. Vitamin C levels fall after surgery or inflammatory disease. The body needs more vitamin C when coping with stress, pregnancy and breast feeding. Aspirin, tetracycline and contraceptive pills take vitamin C out of the body. Smokers also need extra vitamin C because nicotine removes it. Fresh fruit and vegetables are the best sources of vitamin C.
Doctors are increasingly concerned about low vitamin D, especially in the Asian community. A lack of vitamin D can lead to depression. Oily fish and dairy products are good sources of vitamin D, and sunlight helps the body make vitamin D. Do you get enough sunshine and eat a good diet? It is estimated that worldwide over 1 billion people get too little vitamin D.
Evidence
Taking supplements of vitamins B and D might help some people, whose diet is poor, but more research is needed.
Safety
Very high doses of vitamins and minerals can upset the body and cause side-effects. Get medical advice if you intend to take large doses. To ensure that you get a good balance of these vitamins, try to eat more whole-foods, fruits, vegetables, nuts and seeds.
Cost
If your diet is poor and you don’t get into the sun, ask your doctor about a vitamin D blood test. If it’s normal, there’s no point in taking vitamin D. If it’s low, your GP will prescribe it for you or you can buy a vitamin D supplement.
___________________________________________________________________
In my view, this text begs several questions:
1) Am I right in thinking that phraseology such as the one below will encourage patients suffering from depression to try the supplements mentioned?
- people with low blood levels of the B vitamin folic acid are more likely to be depressed and less likely to do well on anti-depressant medicines..
- Some people say that taking high doses of vitamin C (1-2 g and more a day) helps lift their mood…
- There is a little research to support this and none showing that high doses of vitamin C actually help clinical depression…
- A lack of vitamin D can lead to depression.
- Taking supplements of vitamins B and D might help some people…
- … your GP will prescribe it for you or you can buy a vitamin D supplement.
2) How does that tally with the latest evidence? For instance:
- No significant reduction in depression was seen after vitamin D supplementation compared to placebo
- No additional effects from nutritional supplementation were detected
- Adding vitamin C to citalopram did not increase the efficacy of citalopram in MDD patients.
3) The CMIH state: ‘This site gives you information NOT medical advice.’ But, in view of the actual text above, is this true?
4) Depression is a life-threatening condition. Is there a risk that patients trust the CMHI’s (non-) advice and commit suicide because of its ineffectiveness?
5) Do Pukka, the sponsor of all this, happen to supply most of the self care remedies promoted in the ‘Self Care Tool Kit’?
The answer to the last question, I am afraid, is YES!





















