systematic review
I have seen some daft meta-analyses in my time – this one, however, takes the biscuit. Here is its unaltered abstract:
Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
___________________________
This meta-analysis has too many serious flaws to mention. Let me therefore just focus on the main two:
- Craniosacral Therapy is not an MBMBT.
- Craniosacral Therapy is not effective for NLBP. The false positive result was generated on the basis of 4 studies. All of them have serious methodological problems that prevent an overall positive conclusion about the effectiveness of this treatment. In case you don’t believe me, here are the 4 abstracts:
1) Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
2) Background: Craniosacral therapy (CST) and sensorimotor training (SMT) are two recommended interventions for nonspecific chronic low back pain (NCLBP). This study compares the effects of CST and SMT on pain, functional disability, depression and quality of life in patients with NCLBP.
Methodology: A total of 31 patients with NCLBP were randomly assigned to the CST group (n=16) and SMT (n=15). The study patients received 10 sessions of interventions during 5 weeks. Visual analogue scale (VAS), Oswestry disability index (ODI), Beck depression inventory-II (BDI-II), and Short Form-36 (SF-36) questionnaires were used at baseline (before the treatment), after the treatment, and 2 months after the last intervention session. Results were compared and analyzed statistically.
Results: Both groups showed significant improvement from baseline to after treatment (p < 0.05). In the CST group, this improvement continued during the follow-up period in all outcomes (p < 0.05), except role emotional domain of SF-36. In the SMT group, VAS, ODI and BDI-II increased during follow-up. Also, all domains of SF-36 decreased over this period. Results of group analysis indicate a significant difference between groups at the end of treatment phase (p < 0.05), except social functioning.
Conclusions: Results of our research confirm that 10 sessions of craniosacral therapy (CST) or sensorimotor training (SMT) can significantly control pain, disability, depression, and quality of life in patients with NCLBP; but the efficacy of CST is significantly better than SMT.
3) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
4) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
_______________________________
I REST MY CASE
Lumbosacral Radicular Syndrome (LSRS) is a condition characterized by pain radiating in one or more dermatomes (Radicular Pain) and/or the presence of neurological impairments (Radiculopathy). So far, different reviews have investigated the effect of HVLA (high-velocity low-amplitude) spinal manipulations in LSRS. However, these studies included ‘mixed’ population samples (LBP patients with or without LSRS) and treatments other than HVLA spinal manipulations (e.g., mobilisation, soft tissue treatment, etc.). Hence, the efficacy of HVLAT in LSRS is yet to be fully understood.
This review investigated the effect and safety of HVLATs on pain, levels of disability, and health-related quality of life in LSRS, as well as any possible adverse events.
Randomized clinical trials (RCTs) published in English in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (PubMed), EMBASE, PEDro, and Web of Science were identified. RCTs on an adult population (18-65 years) with LSRS that compared HVLATs with other non-surgical treatments, sham spinal manipulation, or no intervention were considered. Two authors selected the studies, extracted the data, and assessed the methodological quality through the ‘Risk of Bias (RoB) Tool 2.0’ and the certainty of the evidence through the ‘GRADE tool’. A meta-analysis was performed to quantify the effect of HVLA on pain levels.
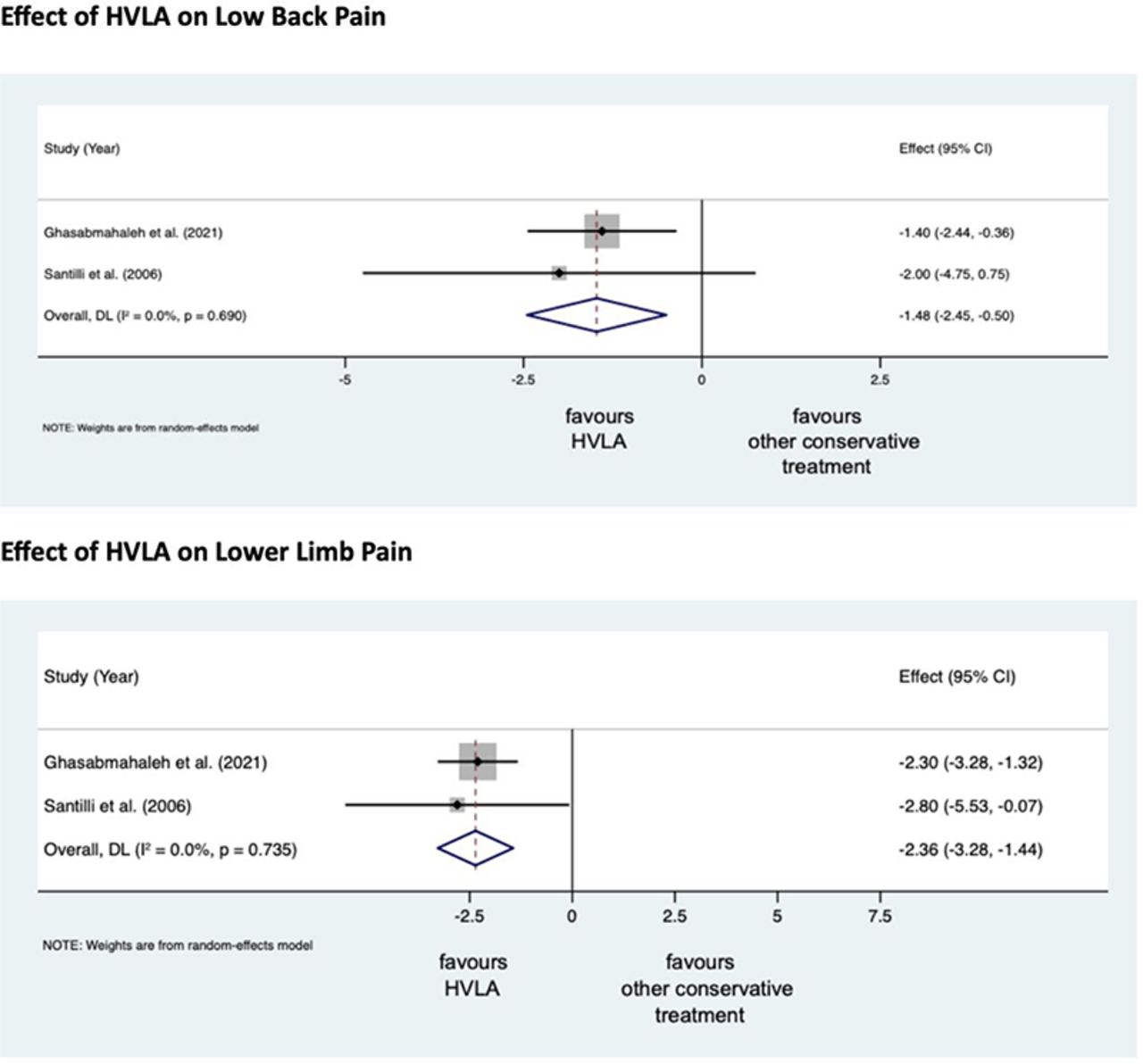
A total of 308 records were retrieved from the search strings. Only two studies met the inclusion criteria. Both studies were at high RoB. Two meta-analyses were performed for low back and leg pain levels. HVLA seemed to reduce the levels of low back (MD = -1.48; 95% CI = -2.45, -0.50) and lower limb (MD = -2.36; 95% CI = -3.28, -1.44) pain compared to other conservative treatments, at three months after treatment. However, high heterogeneity was found (I² = 0.0%, p = 0.735). Besides, their certainty of the evidence was ‘very low’. No adverse events were reported.
The authors stated that they cannot conclude whether HVLA spinal manipulations can be helpful for the treatment of LSRS or not. Future high-quality RCTs are needed to establish the actual effect of HVLA manipulation in this disease with adequate sample size and LSRS definition.
Chiropractors earn their living by applying HVLA thrusts to patients suffering from LSRS. One would therefore have assumed that the question of efficacy has been extensively researched and conclusively answered. It seems that one would have assumed wrongly!
Now that this is (yet again) in the open, I wonder whether chiropractors will, in the future, tell their patients while obtaining informed consent: “I plan to give you a treatment for which sound evidence is not available; it can also cause harm; and, of course, it will cost you – I hope you don’t mind.”
On this blog, we have some people who continue to promote conspiracy theories about Covid and Covid vaccinations. It is, therefore, time, I feel, to present them with some solid evidence on the subject (even though it means departing from our usual focus on SCAM).
This Cochrane review assessed the efficacy and safety of COVID‐19 vaccines (as a full primary vaccination series or a booster dose) against SARS‐CoV‐2. An impressive team of investigators searched the Cochrane COVID‐19 Study Register and the COVID‐19 L·OVE platform (last search date 5 November 2021). They also searched the WHO International Clinical Trials Registry Platform, regulatory agency websites, and Retraction Watch. They included randomized controlled trials (RCTs) comparing COVID‐19 vaccines to placebo, no vaccine, other active vaccines, or other vaccine schedules.
A total of 41 RCTs could be included and analyzed assessing 12 different vaccines, including homologous and heterologous vaccine schedules and the effect of booster doses. Thirty‐two RCTs were multicentre and five were multinational. The sample sizes of RCTs were 60 to 44,325 participants. Participants were aged: 18 years or older in 36 RCTs; 12 years or older in one RCT; 12 to 17 years in two RCTs; and three to 17 years in two RCTs. Twenty‐nine RCTs provided results for individuals aged over 60 years, and three RCTs included immunocompromised patients. No trials included pregnant women. Sixteen RCTs had two‐month follow-ups or less, 20 RCTs had two to six months, and five RCTs had greater than six to 12 months or less. Eighteen reports were based on preplanned interim analyses. The overall risk of bias was low for all outcomes in eight RCTs, while 33 had concerns for at least one outcome. 343 registered RCTs with results not yet available were identified.The evidence for mortality was generally sparse and of low or very low certainty for all WHO‐approved vaccines, except AD26.COV2.S (Janssen), which probably reduces the risk of all‐cause mortality (risk ratio (RR) 0.25, 95% CI 0.09 to 0.67; 1 RCT, 43,783 participants; high‐certainty evidence).High‐certainty evidence was found that BNT162b2 (BioNtech/Fosun Pharma/Pfizer), mRNA‐1273 (ModernaTx), ChAdOx1 (Oxford/AstraZeneca), Ad26.COV2.S, BBIBP‐CorV (Sinopharm‐Beijing), and BBV152 (Bharat Biotect) reduce the incidence of symptomatic COVID‐19 compared to placebo (vaccine efficacy (VE): BNT162b2: 97.84%, 95% CI 44.25% to 99.92%; 2 RCTs, 44,077 participants; mRNA‐1273: 93.20%, 95% CI 91.06% to 94.83%; 2 RCTs, 31,632 participants; ChAdOx1: 70.23%, 95% CI 62.10% to 76.62%; 2 RCTs, 43,390 participants; Ad26.COV2.S: 66.90%, 95% CI 59.10% to 73.40%; 1 RCT, 39,058 participants; BBIBP‐CorV: 78.10%, 95% CI 64.80% to 86.30%; 1 RCT, 25,463 participants; BBV152: 77.80%, 95% CI 65.20% to 86.40%; 1 RCT, 16,973 participants).Moderate‐certainty evidence was found that NVX‐CoV2373 (Novavax) probably reduces the incidence of symptomatic COVID‐19 compared to placebo (VE 82.91%, 95% CI 50.49% to 94.10%; 3 RCTs, 42,175 participants).There is low‐certainty evidence for CoronaVac (Sinovac) for this outcome (VE 69.81%, 95% CI 12.27% to 89.61%; 2 RCTs, 19,852 participants).High‐certainty evidence was found that BNT162b2, mRNA‐1273, Ad26.COV2.S, and BBV152 result in a large reduction in the incidence of severe or critical disease due to COVID‐19 compared to placebo (VE: BNT162b2: 95.70%, 95% CI 73.90% to 99.90%; 1 RCT, 46,077 participants; mRNA‐1273: 98.20%, 95% CI 92.80% to 99.60%; 1 RCT, 28,451 participants; AD26.COV2.S: 76.30%, 95% CI 57.90% to 87.50%; 1 RCT, 39,058 participants; BBV152: 93.40%, 95% CI 57.10% to 99.80%; 1 RCT, 16,976 participants).
Moderate‐certainty evidence was found that NVX‐CoV2373 probably reduces the incidence of severe or critical COVID‐19 (VE 100.00%, 95% CI 86.99% to 100.00%; 1 RCT, 25,452 participants).
Two trials reported high efficacy of CoronaVac for severe or critical disease with wide CIs, but these results could not be pooled.
mRNA‐1273, ChAdOx1 (Oxford‐AstraZeneca)/SII‐ChAdOx1 (Serum Institute of India), Ad26.COV2.S, and BBV152 probably result in little or no difference in serious adverse events (SAEs) compared to placebo (RR: mRNA‐1273: 0.92, 95% CI 0.78 to 1.08; 2 RCTs, 34,072 participants; ChAdOx1/SII‐ChAdOx1: 0.88, 95% CI 0.72 to 1.07; 7 RCTs, 58,182 participants; Ad26.COV2.S: 0.92, 95% CI 0.69 to 1.22; 1 RCT, 43,783 participants); BBV152: 0.65, 95% CI 0.43 to 0.97; 1 RCT, 25,928 participants). In each of these, the likely absolute difference in effects was fewer than 5/1000 participants.
Evidence for SAEs is uncertain for BNT162b2, CoronaVac, BBIBP‐CorV, and NVX‐CoV2373 compared to placebo (RR: BNT162b2: 1.30, 95% CI 0.55 to 3.07; 2 RCTs, 46,107 participants; CoronaVac: 0.97, 95% CI 0.62 to 1.51; 4 RCTs, 23,139 participants; BBIBP‐CorV: 0.76, 95% CI 0.54 to 1.06; 1 RCT, 26,924 participants; NVX‐CoV2373: 0.92, 95% CI 0.74 to 1.14; 4 RCTs, 38,802 participants).
The authors’ conclusions were as follows: Compared to placebo, most vaccines reduce, or likely reduce, the proportion of participants with confirmed symptomatic COVID‐19, and for some, there is high‐certainty evidence that they reduce severe or critical disease. There is probably little or no difference between most vaccines and placebo for serious adverse events. Over 300 registered RCTs are evaluating the efficacy of COVID‐19 vaccines, and this review is updated regularly on the COVID‐NMA platform (covid-nma.com).
_____________________
As some conspiratorial loons will undoubtedly claim that this review is deeply biased; it might be relevant to add the conflicts of interest of its authors:
- Carolina Graña: none known.
- Lina Ghosn: none known.
- Theodoros Evrenoglou: none known.
- Alexander Jarde: none known.
- Silvia Minozzi: no relevant interests; Joint Co‐ordinating Editor and Method editor of the Drugs and Alcohol Group.
- Hanna Bergman: Cochrane Response – consultant; WHO – grant/contract (Cochrane Response was commissioned by the WHO to perform review tasks that contribute to this publication).
- Brian Buckley: none known.
- Katrin Probyn: Cochrane Response – consultant; WHO – consultant (Cochrane Response was commissioned to perform review tasks that contribute to this publication).
- Gemma Villanueva: Cochrane Response – employment (Cochrane Response has been commissioned by WHO to perform parts of this systematic review).
- Nicholas Henschke: Cochrane Response – consultant; WHO – consultant (Cochrane Response was commissioned by the WHO to perform review tasks that contributed to this publication).
- Hillary Bonnet: none known.
- Rouba Assi: none known.
- Sonia Menon: P95 – consultant.
- Melanie Marti: no relevant interests; Medical Officer at WHO.
- Declan Devane: Health Research Board (HRB) – grant/contract; registered nurse and registered midwife but no longer in clinical practice; Editor, Cochrane Pregnancy and Childbirth Group.
- Patrick Mallon: AstraZeneca – Advisory Board; spoken of vaccine effectiveness to media (print, online, and live); works as a consultant in a hospital that provides vaccinations; employed by St Vincent’s University Hospital.
- Jean‐Daniel Lelievre: no relevant interests; published numerous interviews in the national press on the subject of COVID vaccination; Head of the Department of Infectious Diseases and Clinical Immunology CHU Henri Mondor APHP, Créteil; WHO (IVRI‐AC): expert Vaccelarate (European project on COVID19 Vaccine): head of WP; involved with COVICOMPARE P et M Studies (APHP, INSERM) (public fundings).
- Lisa Askie: no relevant interests; Co‐convenor, Cochrane Prospective Meta‐analysis Methods Group.
- Tamara Kredo: no relevant interests; Medical Officer in an Infectious Diseases Clinic at Tygerberg Hospital, Stellenbosch University.
- Gabriel Ferrand: none known.
- Mauricia Davidson: none known.
- Carolina Riveros: no relevant interests; works as an epidemiologist.
- David Tovey: no relevant interests; Emeritus Editor in Chief, Feedback Editors for 2 Cochrane review groups.
- Joerg J Meerpohl: no relevant interests; member of the German Standing Vaccination Committee (STIKO).
- Giacomo Grasselli: Pfizer – speaking engagement.
- Gabriel Rada: none known.
- Asbjørn Hróbjartsson: no relevant interests; Cochrane Methodology Review Group Editor.
- Philippe Ravaud: no relevant interests; involved with Mariette CORIMUNO‐19 Collaborative 2021, the Ministry of Health, Programme Hospitalier de Recherche Clinique, Foundation for Medical Research, and AP‐HP Foundation.
- Anna Chaimani: none known.
- Isabelle Boutron: no relevant interests; member of Cochrane Editorial Board.
___________________________
And as some might say this analysis is not new, here are two further papers just out:
Objectives To determine the association between covid-19 vaccination types and doses with adverse outcomes of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection during the periods of delta (B.1.617.2) and omicron (B.1.1.529) variant predominance.
Design Retrospective cohort.
Setting US Veterans Affairs healthcare system.
Participants Adults (≥18 years) who are affiliated to Veterans Affairs with a first documented SARS-CoV-2 infection during the periods of delta (1 July-30 November 2021) or omicron (1 January-30 June 2022) variant predominance. The combined cohorts had a mean age of 59.4 (standard deviation 16.3) and 87% were male.
Interventions Covid-19 vaccination with mRNA vaccines (BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna)) and adenovirus vector vaccine (Ad26.COV2.S (Janssen/Johnson & Johnson)).
Main outcome measures Stay in hospital, intensive care unit admission, use of ventilation, and mortality measured 30 days after a positive test result for SARS-CoV-2.
Results In the delta period, 95 336 patients had infections with 47.6% having at least one vaccine dose, compared with 184 653 patients in the omicron period, with 72.6% vaccinated. After adjustment for patient demographic and clinical characteristics, in the delta period, two doses of the mRNA vaccines were associated with lower odds of hospital admission (adjusted odds ratio 0.41 (95% confidence interval 0.39 to 0.43)), intensive care unit admission (0.33 (0.31 to 0.36)), ventilation (0.27 (0.24 to 0.30)), and death (0.21 (0.19 to 0.23)), compared with no vaccination. In the omicron period, receipt of two mRNA doses were associated with lower odds of hospital admission (0.60 (0.57 to 0.63)), intensive care unit admission (0.57 (0.53 to 0.62)), ventilation (0.59 (0.51 to 0.67)), and death (0.43 (0.39 to 0.48)). Additionally, a third mRNA dose was associated with lower odds of all outcomes compared with two doses: hospital admission (0.65 (0.63 to 0.69)), intensive care unit admission (0.65 (0.59 to 0.70)), ventilation (0.70 (0.61 to 0.80)), and death (0.51 (0.46 to 0.57)). The Ad26.COV2.S vaccination was associated with better outcomes relative to no vaccination, but higher odds of hospital stay and intensive care unit admission than with two mRNA doses. BNT162b2 was generally associated with worse outcomes than mRNA-1273 (adjusted odds ratios between 0.97 and 1.42).
Conclusions In veterans with recent healthcare use and high occurrence of multimorbidity, vaccination was robustly associated with lower odds of 30 day morbidity and mortality compared with no vaccination among patients infected with covid-19. The vaccination type and number of doses had a significant association with outcomes.
SECOND EXAMPLE Long COVID, or complications arising from COVID-19 weeks after infection, has become a central concern for public health experts. The United States National Institutes of Health founded the RECOVER initiative to better understand long COVID. We used electronic health records available through the National COVID Cohort Collaborative to characterize the association between SARS-CoV-2 vaccination and long COVID diagnosis. Among patients with a COVID-19 infection between August 1, 2021 and January 31, 2022, we defined two cohorts using distinct definitions of long COVID—a clinical diagnosis (n = 47,404) or a previously described computational phenotype (n = 198,514)—to compare unvaccinated individuals to those with a complete vaccine series prior to infection. Evidence of long COVID was monitored through June or July of 2022, depending on patients’ data availability. We found that vaccination was consistently associated with lower odds and rates of long COVID clinical diagnosis and high-confidence computationally derived diagnosis after adjusting for sex, demographics, and medical history.
_______________________________________
There are, of course, many more articles on the subject for anyone keen to see the evidence. Sadly, I have little hope that the COVID loons will be convinced by any of them. Yet, I thought I should give it nevertheless a try.
A team of French researchers assessed whether a conflict of interest (COI) might be associated with the direction of the results of meta-analyses of homoeopathy trials. Their analysis (published as a ‘letter to the editor) is complex, therefore, I present here only their main finding.
The team conducted a literature search until July 2022 on PubMed and Embase to identify meta-analyses of randomized clinical trials assessing the efficacy of homoeopathy. They then assessed the existence of potential COI, defined by the presence of at least one of the following criteria:
- affiliation of one or more authors to an academic homoeopathy research or care facility, or to the homoeopathy industry;
- research sponsored or funded by the homoeopathy industry;
- COI declared by the authors.
The researchers also evaluated and classified any spin in meta-analyses conclusions into three categories (misleading reporting, misleading interpretation and inappropriate extrapolation). Two reviewers assessed the quality of meta-analyses and the risk of bias based. Publication bias was evaluated by the funnel plot method. For all the studies included in these meta-analyses, the researchers checked whether they reported a statistically significant result in favour of homoeopathy. Further details about the methods are provided on OSF (https://osf.io/nqw7r/) and in the preregistered protocol (CRD42020206242).
Twenty meta-analyses were included in the analysis (list of references available at https://osf.io/nqw7r/).
- Among the 13 meta-analyses with COI, a significantly positive effect of homoeopathy emerged (OR=0.60 (95% CI 0.50 to 0.70)).
- There was no such effect for meta-analyses without COI (OR=0.96 (95% CI 0.75 to 1.23)).
The authors concluded that in the presence of COI, meta-analyses of homoeopathy trials are more likely
to have favourable results. This is consistent with recent research suggesting that systematic reviews with financial COI are associated with more positive outcomes.
Meta-analyses are systematic reviews (critical assessments of the totality of the available evidence) where the data from the included studies are pooled. For a range of reasons, this may not always be possible. Therefore the number of meta-analyses (20) is substantially lower than that of the existing systematic reviews (>50).
Both systematic reviews and meta-analyses are theoretically the most reliable evidence regarding the value of any intervention. I said ‘theoretically’ because, like any human endeavour, they need to be done in an unbiased fashion to produce reliable results. People with a conflict of interest by definition struggle to be free of bias. As we have seen many times, this would include homoeopaths.
This new analysis confirms what many of us have feared. If proponents of homeopathy with an overt conflict of interest conduct a meta-analysis of studies of homeopathy, the results tend to be more positive than when independent researchers do it. The question that emerges from this is the following:
Are the findings of those researchers who have an interest in producing a positive result closer to the truth than the findings of researchers who have no such conflict?
I let you decide.
In response to yesterday’s post, I received a lengthy comment from ‘Stan’. Several readers have already commented on it. Therefore, I can make my arguments short. In this post, will repeat Stan’s points each followed by my comments (in bold). Here we go:
Seven Reasons Homœopathy is Not Placebo Effect
Sorry, Stan, but your heading is not proper English; I have therefore changed it for the title of this post.
1. Homeopathic remedies work on babies, animals, plants and people in a coma. Biodynamic farmers use homeopathic remedies to repel pests and treat plant diseases. Some organic ranchers rely on homeopathic remedies to treat their herds. Some “placebo by proxy” effect has been shown for children but its doubtful that it could be shown for a herd of cattle or crops in a field. Farmers can’t rely on wishful thinking to stay in business.
As discussed ad nauseam on this blog, homeopathic remedies do not work on babies or animals better than placebos. I don’t know of any studies with “people in a coma” (if you do, Stan, please let me know). The fact that ranchers rely on homeopathy is hilarious but does not prove anything.
2. The correct curative remedy will initially cause a worsening of the condition being cured if it is given in too strong (i.e. too dilute) a dose. A placebo might only cause a temporary improvement of the condition being treated; certainly not an aggravation.
The ‘homeopathic aggravation’ is a myth created by homeopaths. It disappears if we try to systematically research it; see here, for instance.
3. One can do a “proving” of an unknown homeopathic remedy by taking it repeatedly over several days and it will temporarily cause symptoms that one has never experienced previously – symptoms it will cure in a sick person. This is a repeatable scientific experiment used to determine the scope of a new remedy, or confirm the effects of an already proven remedy. A placebo might possibly have an effect if the individual taking it has been “prepared” by being told what they are taking but it likely wouldnt match previously recorded symptoms in the literature.
Homeopathic provings are rubbish and not reproducible when done rigorously; see here.
4. One can treat simple acute (self-limiting) conditions (e.g. minor burns, minor injuries, insect bites, etc.) and see unusually rapid cures with homeopathic remedies. A placebo might only cause a temporary improvement of the condition being treated while taken. Placebos have been found mostly effective in conditions with a strong psychological component like pain.
You mean like using Arnica for cuts and bruises? Sadly, it does not work.
5. One can get homeopathic treatment for long term chronic (non self-limiting) conditions and see a deep lasting cure, as has been documented clinically for a couple centuries. A placebo might only cause a temporary partial improvement of the condition being treated while the placebo is being taken.
You mean like asthma, eczema, or insomnia?
6. There is over 200 years worth of extensive documentation from around the world, of the clinical successes of homeopathy for both acute and chronic conditions of all types. As Dr Hahn has said you have throw out 90% of the evidence to conclude that homeopathy doesnt work. The Sheng et al meta-analysis in 2005 Lancet that was supposedly the death knell of homeopathy used only 8 studies, excluding hundreds of others. Unsurprisingly homeopathy was found wanting. So-called Skeptics see what they want to see in the science. There is relatively little documentation of placebo usage. A few recent studies have been done showing the limited temporary benefits of placebos.
What Hahn wrote is understandably liked by homeopaths but it nevertheless is BS. If you don’t trust me, please rely on independent bodies from across the world.
7. Homeopathic remedies have been shown to have a very weak electromagnetic signature and contain some nano-particles. Some believe this explains their mechanism. An exciting new potential field of research is the subtle cell signalling that has been found to direct the development of stem cells. Scientists have created double-headed planeria worms and this trait has been found to be inherited by their offspring without any change in the genes or epigenetics. Until now we had no idea how a single fertilized ovum could evolve into a complex creature that is bilateral and has multiple cell types. It is possible that the very subtle electromagnetic signature or some other unknown effect of homeopathic remedies is effecting this subtle cell signalling.
The homeopathic nano-myth is nonsense. And so is the rest of your assumptions.
Every conventional drug has “side effects” that match the symptoms for which it is indicated! Aspirin can cause headaches and fever, ritalin can cause hyperactive effects, radiation can cause cancer. Conventional doctors are just practicing bad homeopathy. They are prescribing Partially similar medicines. If their drugs were homeopathic (i.e. similar) to the patients symptoms on all levels they would be curative. Radiation sometimes does cure cancer instead of just suppressing it per usual.
Even if this were true, what would it prove? Certainly not that homeopathy works!
Dr Hahneman did forbid mixing homeopathy and conventional medicine. In his day doctors commonly used extensive blood letting and extreme doses of mercury. Its not Quite as bad now.
You evidently did not read Hahnemann’s writings.
Just because we dont know how extremely dilute homeopathic remedies work, doesn’t discount that they Do work. Homeopathy seems to fly in the face of Known science. In no way is it irrational or unscientific. There are lots of phenomena in the universe that cant be explained yet, like dark energy and dark matter effects and even consciousness!
Not knowing how a treatment works has not stopped science to test whether it works (e.g. Aspirin). In the case of homeopathy, the results of these endeavors were not positive.
The assumption that the moon is made of cheese also flies in the face of science; do you perhaps think that this makes it true?
The actions of homeopathy can and have been well-explained: they are due to placebo effects.
________________________
Stan, thank you for this entertaining exercise. But, next time, please remember to supply evidence for your statements.
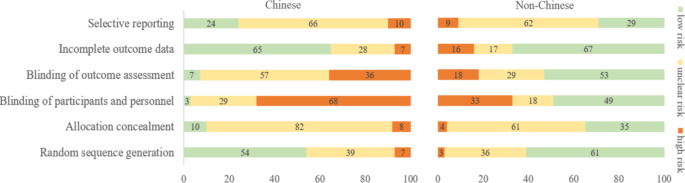
There are debates in acupuncture-related systematic reviews and meta-analyses on whether searching Chinese databases to get more Chinese-language studies may increase the risk of bias and overestimate the effect size, and whether the treatment effects of acupuncture differ between Chinese and non-Chinese populations.
For this meta-epidemiological study, a team of investigators searched the Cochrane Library from its inception until December 2021, and identified systematic reviews and meta-analyses with acupuncture as one of the interventions. Paired reviewers independently screened the reviews and extracted the information. They repeated the meta-analysis of the selected outcomes to separately pool the results of Chinese- and non-Chinese-language acupuncture studies and presented the pooled estimates as odds ratios (OR) with 95% confidence interval (CI). They calculated the Ratio of ORs (ROR) by dividing the OR of the Chinese-language trials by the OR of the non-Chinese-language trials, and the ROR by dividing the OR of trials addressing Chinese population by the OR of trials addressing non-Chinese population. The researchers thus explored whether the impact of a high risk of bias on the effect size differed between studies published in Chinese- and in non-Chinese-language, and whether the treatment effects of acupuncture differed between Chinese and non-Chinese populations.
The researchers identified 84 Cochrane acupuncture reviews involving 33 Cochrane groups, of which 31 reviews (37%) searched Chinese databases. Searching versus not searching Chinese databases significantly increased the contribution of Chinese-language literature both to the total number of included trials (54% vs. 15%) and the sample size (40% vs. 15%). When compared with non-Chinese-language trials, Chinese-language trials were associated with a larger effect size (pooled ROR 0.51, 95% CI 0.29 to 0.91). The researchers also observed a higher risk of bias in Chinese-language trials in blinding of participants and personnel (97% vs. 51%) and blinding of outcome assessment (93% vs. 47%). The higher risk of bias was associated with a larger effect estimate in both Chinese language (allocation concealment: high/unclear risk vs. low risk, ROR 0.43, 95% CI 0.21 to 0.87) and non-Chinese-language studies (blinding of participants and personnel: high/unclear risk vs. low risk, ROR 0.41, 95% CI 0.23 to 0.74). However, the team found no evidence that the higher risk of bias would increase the effect size of acupuncture in Chinese-language studies more often than in non-Chinese-language studies (the confidence intervals of all ROR in the high-risk group included 1, Table 3). The researchers further found acupuncture appeared to be more effective in Chinese than in non-Chinese populations.
The authors concluded that the findings of this study suggest the higher risk of bias may lead to an overestimation of the treatment effects of acupuncture but would not increase the treatment effects in Chinese-language studies more often than in other language studies. The difference in treatment effects of acupuncture was probably associated with differences in population characteristics.
The authors discuss that, although searching Chinese databases can substantially increase the number of eligible studies and sample size in acupuncture reviews, the potentially higher risk of bias is an argument that needs to be considered in the inclusion of Chinese-language studies. Patients, investigators, and guideline panels should be cautious when adopting evidence from acupuncture reviews where studies with a high risk of bias contributed with a high weight to the meta-analysis.
The authors observed larger treatment effects of acupuncture in Chinese-language studies than in studies published in other languages. Although the treatment effects of acupuncture tended to be greater in studies with a high risk of bias, this potential overestimation did not differ between studies published in Chinese and in other languages. In other words, the larger treatment effects in Chinese-language studies cannot be explained by a high risk of bias. Furthermore, our study found acupuncture to be more effective in Chinese populations than in other populations, which could at least partly explain the larger treatment effects observed in Chinese-language studies.
I feel that this analysis obfuscates more than it clarifies. As we have discussed often here, acupuncture studies by Chinese researchers (regardless of what language they are published in) hardly ever report negative results, and their findings are often fabricated. It, therefore, is not surprising that their effect sizes are larger than those of other trials.
The only sensible conclusion from this messy and regrettable situation, in my view, is to be very cautious and exclude them from systematic reviews.
Infant colic is a sensitive subject for chiropractors in the UK. In case you forgot, here is why. Consequently, the subject has featured regularly on this blog – and now there is new evidence:
A systematic review and meta-analysis were conducted on infantile colic studies that used SO-CALLED alternative medicine (SCAM) techniques as interventions. The outcome measures were hours spent crying and/or sleeping. The authors used the PubMed, Physiotherapy Evidence Database, Cochrane Library, Embase, Web of Science, Scopus, Osteopathic Medicine Digital Database, and Google Scholar databases from inception to 11 November 2022.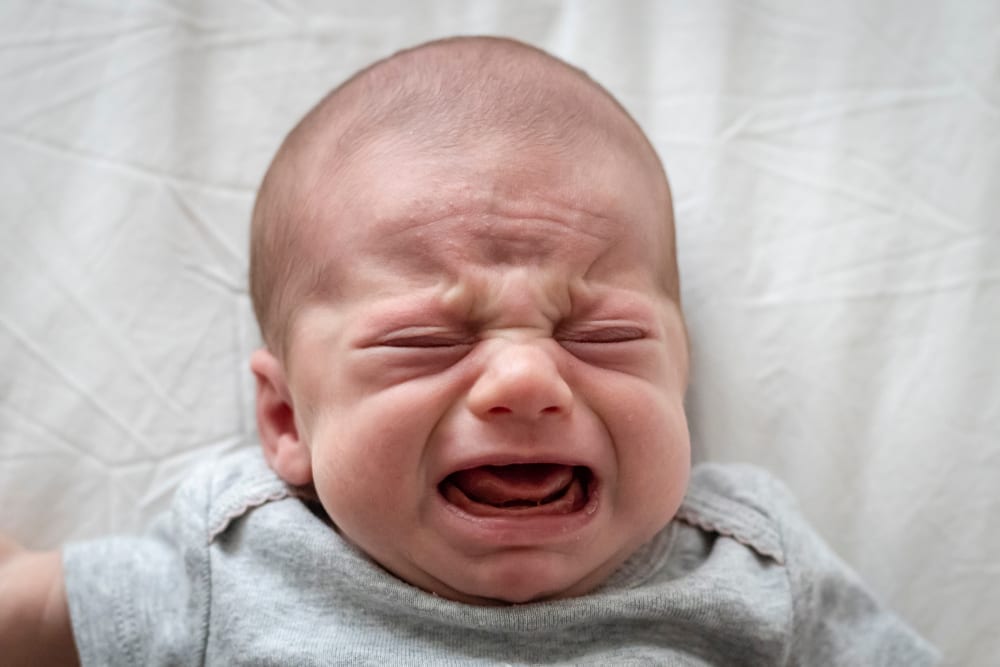
The methodological quality of the randomized control trials ranged from fair to high. The authors focused on five studies with 422 babies using the following interventions: cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization. These treatments failed to decrease the crying time (mean difference -1.08, 95% CI -2.17 to 0.01, I2 = 92%) and to increase the sleeping time (mean difference 1.11, 95% CI -0.20 to 2.41; I2: 91%), compared with no intervention. The quality of the evidence was rated as very low for both outcome measures.The authors concluded that osteopathy and chiropractic treatment failed to reduce the crying time and increase sleeping time in babies with infantile colic, compared to no additional intervention.The 5 included studies were the following:
- Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: A pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther. 2012;35(8):600–7.
- Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. A randomized controlled trial. Complement Ther Med. 2022;71(February 2021).
- Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child. 2001;84(2):138–41.
- Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Ther. 2021;29(1):1–11.
- Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract. 2006;12(2):83–90.
This means that, in recent years, several new studies have emerged. I find this surprising: there is no plausible mechanism of action and the previous reviews were negative.
Why flog a dead horse?
But – come to think of it – this is a question one might ask about most of the research into cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization.
Social prescribing (SP) has been mentioned here several times before. It seems important to so-called alternative medicine (SCAM), as some enthusiasts – not least King Charles – are trying to use it as a means to smuggle nonsensical treatments into routine healthcare.
SP is supposed to enable healthcare professionals to link patients with non-medical interventions available in the community to address underlying socioeconomic and behavioural determinants. The question, of course, is whether it has any relevant benefits.
This systematic review included all randomised controlled trials of SP among community-dwelling adults recruited from primary care or community setting, investigating any chronic disease risk factors defined by the WHO (behavioural factors: smoking, physical inactivity, unhealthy diet and excessive alcohol consumption; metabolic factors: raised blood pressure, overweight/obesity, hyperlipidaemia and hyperglycaemia). Random effect meta-analyses were performed at two time points: completion of intervention and follow-up after trial.
The researchers identified 9 reports from 8 trials totalling 4621 participants. All studies evaluated SP exercise interventions which were highly heterogeneous regarding the content, duration, frequency and length of follow-up. The majority of studies had some concerns about the risk of bias. A meta-analysis revealed that SP likely increased physical activity (completion: mean difference (MD) 21 min/week, 95% CI 3 to 39, I2=0%; follow-up ≤12 months: MD 19 min/week, 95% CI 8 to 29, I2=0%). However, SP may not improve markers of adiposity, blood pressure, glucose and serum lipid. There were no eligible studies that primarily target unhealthy diet, smoking or excessive alcohol-drinking behaviours.
The authors concluded that SP exercise interventions probably increased physical activity slightly; however, no benefits were observed for metabolic factors. Determining whether SP is effective in modifying the determinants of chronic diseases and promotes sustainable healthy behaviours is limited by the current evidence of quantification and uncertainty, warranting further rigorous studies.
Great! Regular exercise improves physical fitness.
But do we need SP for this?
Don’t get me wrong, I have nothing against connecting patients with social networks to improve their health and quality of life. I do, however, object if SP is used to smuggle unproven or disproven SCAMs into EBM. In addition, I ask myself whether we really need the new profession of a ‘link worker’ to facilitate SP. I remember being taught that a good doctor should look after his/her patients holistically, and surely that includes mentioning and facilitating social networks for those who need them.
I, therefore, fear that SP is taking something valuable out of the hands of doctors. And the irony is that SP is favoured by those who are all too quick to turn around and say: LOOK AT HOW FRIGHTFULLY REDUCTIONIST AND HEARTLESS DOCTORS HAVE BECOME. WE NEED MORE HOLISM IN MEDICINE AND THAT CAN ONLY BE PROVIDED BY SCAM PRACTITIONERS!
The claim that homeopathy has a role in oncology does not seem to go away. Some enthusiasts say it can be used as a causal therapy, while others insist it might be a helpful symptomatic adjuvant. Almost all oncologists agree that homeopathy has no place at all in cancer care.
Who is right?
This systematic review included clinical studies from 1800 until 2020 to evaluate evidence of the effectiveness of homeopathy on physical and mental conditions in patients during oncological treatment.
In February 2021 a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning use, effectiveness, and potential harm of homeopathy in cancer patients.
From all 1352 search results, 18 studies with 2016 patients were included in this SR. The patients treated with homeopathy were mainly diagnosed with breast cancer. The therapy concepts included single and combination homeopathic remedies (used systemically or as mouth rinses) of various dilutions. The outcomes assessed were:
- the influence on toxicity of cancer treatment (mostly hot flashes and menopausal symptoms),
- the time to drain removal in breast cancer patients after mastectomy,
- survival,
- quality of life,
- global health,
- subjective well-being,
- anxiety and depression,
- safety and tolerance.
The included studies reported heterogeneous results: some studies described significant differences in quality of life or toxicity of cancer treatment favoring homeopathy, whereas others did not find an effect or reported significant differences to the disadvantage of homeopathy or side effects caused by homeopathy. The majority of the studies had low methodological quality.
The authors concluded that, the results for the effectiveness of homeopathy in cancer patients are heterogeneous, mostly not significant and fail to show an advantage of homeopathy over other active or passive comparison groups. No evidence can be provided that homeopathy exceeds the placebo effect. Furthermore, the majority of the included studies shows numerous and severe methodological weaknesses leading to a high level of bias and are consequently hardly reliable. Therefore, based on the findings of this SR, no evidence for positive effectiveness of homeopathy can be verified.
This could not be clearer. Some might argue that, of course, homeopathy cannot change the natural history of cancer, but it might improve the quality of life of those patients who believe in it via a placebo response. I would still oppose this notion: there are many effective treatments in the supportive treatment of cancer, and it seems much better to use those options and tell patients the truth about homeopathy.
Irritable bowel syndrome (IBS) is a common chronic disorder associated with psychological distress and reduced health-related quality of life (HRQoL). Therefore, stress management is often employed in the hope of alleviating IBS symptoms. But does it work?
This systematic review investigated the effects of stress management for adults with IBS on typical symptoms, HRQoL, and mental health. The predefined criteria included:
- patients: adults with IBS;
- intervention: stress management;
- control: care as usual or waitlist;
- outcome: patient-relevant;
- study-type: controlled trials.
Two researchers independently reviewed the publications retrieved through electronic searches and assessed the risk of bias using the Scottish Intercollegiate Guidelines Network checklist. The researchers performed a meta-analysis with homogeneous trials of acceptable quality.
After screening 6656 publications, 10 suitable randomized trials of acceptable (n = 5) or low methodological quality (n = 5) involving 587 patients were identified. The meta-analysis showed no effect of stress management on IBS severity 1-2 months after the intervention (Hedges’ g = -0.23, 95%-CI = -0.84 to -0.38, I2 = 86.1%), and after 3-12 months (Hedges’ g = -0.77, 95%-CI = -1.77 to -0.23, I2 = 93.3%). One trial found a short-term reduction of symptoms, and one trial found symptom relief in the long term (at 6 months). One of two studies that examined HRQoL found an improvement (after 2 months). One of two studies that examined depression and anxiety found a reduction of these symptoms (after 3 weeks).
The authors concluded that stress management may be beneficial for patients with IBS regarding the short-term reduction of bowel and mental health symptoms, whereas long-term benefits are unclear. Good quality RCTs with more than 6 months follow-up are needed.
Considering the actual evidence, I find the conclusions rather odd. Would it not have been more honest to state something along the following lines?:
There is currently no convincing evidence to suggest that stress management benefits IBS patients.
So why, be not more open and less misleading?
Could some of the authors’ affiliations provide a clue?
- Department for Internal and Integrative Medicine, Sozialstiftung Bamberg Hospital, Bamberg, Germany.
- Department for Integrative Medicine, University of Duisburg-Essen, Medical Faculty, Bamberg, Germany.
Quite possibly, yes!