symptom-relief
Low back pain is the leading cause of years lived with disability globally, but most interventions have only short-lasting, small to moderate effects. Cognitive functional therapy (CFT) is an individualized approach that targets unhelpful pain-related cognitions, emotions, and behaviors that contribute to pain and disability. Movement sensor biofeedback might enhance treatment effects.
This study aimed to compare the effectiveness and economic efficiency of CFT, delivered with or without movement sensor biofeedback, with usual care for patients with chronic, disabling low back pain.
RESTORE was a randomized, three-arm, parallel-group, phase 3 trial, done in 20 primary care physiotherapy clinics in Australia. The researchers recruited adults (aged ≥18 years) with low back pain lasting more than 3 months with at least moderate pain-related physical activity limitation. Exclusion criteria were serious spinal pathology (eg, fracture, infection, or cancer), any medical condition that prevented being physically active, being pregnant or having given birth within the previous 3 months, inadequate English literacy for the study’s questionnaires and instructions, a skin allergy to hypoallergenic tape adhesives, surgery scheduled within 3 months, or an unwillingness to travel to trial sites. Participants were randomly assigned (1:1:1) via a centralized adaptive schedule to
- usual care,
- CFT only,
- CFT plus biofeedback.
The primary clinical outcome was activity limitation at 13 weeks, self-reported by participants using the 24-point Roland Morris Disability Questionnaire. The primary economic outcome was quality-adjusted life-years (QALYs). Participants in both interventions received up to seven treatment sessions over 12 weeks plus a booster session at 26 weeks. Physiotherapists and patients were not masked.
Between Oct 23, 2018, and Aug 3, 2020, the researchers assessed 1011 patients for eligibility. After excluding 519 (51·3%) ineligible patients, they randomly assigned 492 (48·7%) participants; 164 (33%) to CFT only, 163 (33%) to CFT plus biofeedback, and 165 (34%) to usual care. Both interventions were more effective than usual care (CFT only mean difference –4·6 [95% CI –5·9 to –3·4] and CFT plus biofeedback mean difference –4·6 [–5·8 to –3·3]) for activity limitation at 13 weeks (primary endpoint). Effect sizes were similar at 52 weeks. Both interventions were also more effective than usual care for QALYs, and much less costly in terms of societal costs (direct and indirect costs and productivity losses; –AU$5276 [–10 529 to –24) and –8211 (–12 923 to –3500).
The authors concluded that CFT can produce large and sustained improvements for people with chronic disabling low back pain at considerably lower societal cost than that of usual care.
This is a well-designed and well-reported study. It shows that CFT is better than usual care. The effect sizes are not huge and seem similar to many other treatments for chronic LBP, including the numerous so-called alternative medicine (SCAM) options that are available.
Faced with a situation where we have virtually dozens of therapies of similar effectiveness, what should we recommend to patients? I think this question is best and most ethically answered by accounting for two other important determinants of usefulness:
- risk
- cost.
CFT is both low in risk and cost. So is therapeutic exercise. We would therefore need a direct comparison of the two to decide which is the optimal approach.
Until we have such a study, patients might just opt for one or both of them. What seems clear, meanwhile, is this: SCAM does not offer the best solution to chronic LBP. In particular, chiropractic, osteopathy, or acupuncture – which are neither low-cost nor risk-free – are, contrary to what some try so very hard to convince us of, sensible options.
It is not only practitioners of so-called alternative medicine (SCAM) who can be fraudulent charlatans. The study of medicine does not protect you from joining in. Here is an impressive case in point:
It has been reported that a former doctor convicted of fraudulently submitting nearly $120 million in claims related to the 1-800-GET-THIN Lap-Band surgery business has been sentenced to seven years in federal prison.
Julian Omidi, 58, of West Hollywood was sentenced Monday by U.S. District Court Judge Dolly M. Gee. The judge also imposed a five-year probation period on Surgery Center Management LLC, an Omidi-controlled Beverly Hills-based company. In the coming weeks, Gee is expected to hold a separate hearing to decide on restitution and forfeiture in the case, along with setting a fine for the Beverly Hills company.
“Mr. Omidi made millions at the expense of the multiple victim companies he defrauded, and he violated his oath to ‘do no harm’ by callously misleading patients about the need for a sleep study and subsequent weight loss surgery,” said Donald Alway, the assistant director in charge of the FBI’s Los Angeles field office.
Omidi controlled several entities in the GET-THIN network. Prosecutors say Omidi incentivized employees to ensure patients underwent sleep studies and then falsified the results to show that patients had obstructive sleep apnea to help them qualify for insurance coverage for the weight loss surgery. Those results were then filed with insurance companies to pre-approve the Lap-Band weight-loss surgeries. The 1-800-GET-THIN business received approximately $41 million for those procedures, according to prosecutors. While not all patients were approved to receive the surgery, prosecutors say GET-THIN would bill the patient roughly $15,000 for each sleep study, totaling $27 million in payments from insurance providers.
Omidi and his Beverly Hills-based company, Surgery Center Management, were found guilty of 28 counts of wire fraud, three counts of mail fraud, and one count of conspiracy to commit money laundering. Omidi was also found guilty of two counts of making false statements relating to healthcare matters, one count of aggravated identity theft, and two counts of money laundering after a 48-day trial in downtown Los Angeles.
“As found by the jury, the defendant Julian Omidi deliberately and repeatedly acted with an eye towards business and profits, rather than in the interest of GET-THIN’s medical patients, by inducing patients to undergo medical treatment premised on fraud rather than medical necessity, including surgeries that carry significant risks and life-long health impacts,” said U.S. Atty. Martin Estrada. A series of Los Angeles Times columns from 2010 to 2014 detailed how five patients died after they received Lap-Band surgeries at clinics affiliated with 1-800-GET-THIN. During a 2009 inspection, the Department of Health and Human Services found unsanitary conditions, inoperative scrub sinks, one-time-only equipment being reused, and several other deficiencies. The inspector shut down the clinic for a day, but further action was not taken at the time.
Omidi’s medical license was revoked in 2009, and he was arrested. In 2014, federal agencies seized more than $110 million from the 1-800-GET-THIN network in securities and funds.
______________________________
This is a spectacular case, of course. Yet, I fail to see how it differs in principle from the many instances we see on a daily basis in the realm of SCAM. Let me give you just a few examples:
- A chiropractor diagnoses subluxation and subsequently treats his patient with a series of spinal manipulations.
- A naturopath uses iridology to diagnose a weakness of the liver and subsequently treats it with herbal remedies.
- An acupuncturist diagnoses a blockage of chi and follows it up with a series of acupuncture sessions.
- A Heilpraktiker employs bioresonance to diagnose an intoxication which he then treats with a detox program.
The strategy is always the same:
- Charlatans use bogus diagnostic methods.
- They make bogus diagnoses with them.
- They then start expensive and often dangerous treatments.
- They make good money by defrauding the system.
Could someone please explain what the difference in principle is between the case of the fraudulent surgeon and the average SCAM practitioner?
Imagine you have caught a cold. You think it is not necessary to see a doctor, but you want to take something that helps your body to get better. What is your choice of remedy? There are many options provided by conventional medicine as well as by so-called alternative medicine (SCAM).
Many people opt for SCAM to address health issues or prevent diseases. Yet, the evidence for SCAMs is either lacking or controversial due to methodological weaknesses. Thus, practitioners and patients primarily rely on subjective references rather than credible evidence from systematic research.
This study investigated whether cognitive and personality factors explain the differences in belief in SCAM and homeopathy. The researchers investigated the robustness of 21 predictors when examined together to obtain insights into some key determinants of such beliefs in a sample of 599 participants (60% female, 18-81 years). A combination of predictors explained 20% of the variance in SCAM belief. These predictors were:
- ontological confusions,
- spiritual epistemology,
- agreeableness,
- death anxiety,
- gender.
Approximately 21% of the variance in belief in homeopathy was explained by the following predictors:
- ontological confusions,
- illusory pattern perception,
- need for cognitive closure,
- need for cognition,
- honesty-humility,
- death anxiety,
- gender,
- age.
The authors concluded that some of the predictors from previous research replicated whereas others did not. Demographics and certain cognitive variables seem to be key determinants associated with beliefs in SCAM and homeopathy. Those individual differences and cognitive biases might result in a different perception of the world. However, variables related to abilities did not predict the beliefs. Thus, they might not be a result of inability but rather of ignorance.
Previous studies have shown that SCAM believers tend to believe in paranormal phenomena and conspiracies. I think that, in the discussion sections of this blog, we have ample evidence for this to be true. Paranormal beliefs are usually built on a magical worldview without reasoned review, which is shared by SCAM proponents. Such beliefs advocate emotional criteria for truth instead of data and logical considerations. Another belief, namely spirituality, is closely related to paranormal beliefs and religiosity and also associated with being a SCAM user. Lindeman found that SCAM belief could be best explained by intuitive reasoning, paranormal beliefs, and ontological confusions, defined as category mistakes in which properties of living and lifeless entities are mixed.
The authors point out that their results do not replicate previous findings that showed predictive value of certain cognitive variables such as cognitive style. An explanation could be that rather inattention to accuracy than the inability to consider empirical evidence fosters the beliefs. People might simply not be aware of the absence of evidence. Another possibility is that people are aware of the absence of evidence but are reluctant to engage with it. Practitioners and patients often claim “whatever works is good” or “the main thing is that it works”. Thus, it is ignorance rather than a lack of capacity to appropriately process the evidence.
The authors of this study are well aware of the limitations of their research:
“As with most cross-sectional studies using questionnaires, our results are based on self-reports. Additionally, single items were used for measuring belief strength. Even if multi-item measures often have advantages, single items can be advantageous in terms of practical benefits, e.g., adapting to subjects’ limited attention and time resources. There are several single item measures successfully used to measure diverse concepts including attitudes. Also, the variance on those items in our sample shows that participants were able to reflect their beliefs and rank them on the scale provided. Another limitation is that the findings are based on regression analyses, which do not provide insight into causality. Thus, the relationship remains correlational. Even if our sample was broader than in many other psychological studies—it was slightly unbalanced, especially in comparison to the German population. It over-represented educated individuals which may lead to an inadequate variation of the cognitive variables if we consider the relationship between cognition and education. However, education and the cognitive variables are only weakly correlated. Thus, it can be assumed that the unbalanced sample did not affect the distribution of cognitive variables to a great extent.”
I found this acupuncture study from the Department of Oral and Maxillofacial Sciences, “Sapienza” University of Rome, Rome, Italy. As this seems to be a respectable institution, I had a look. What I found was remarkable! Let me show you the abstract in its full beauty:
Background: Pain related to Temporomandibular Disorders (TMD) is severe, negatively affecting patients’ quality of life, and often resistant to conventional treatments. Abdominal Acupuncture (AA) is known to be particularly effective for pain, especially chronic and musculoskeletal pain, but it is still poorly studied and never investigated in TMD patients. Objectives: To analyze the efficacy of AA for the treatment of patients with subacute and chronic pain related to TMD and non-responding to previous conventional therapies (occlusal splint, medications, physical therapy).
Methods: Twenty-eight patients, 24 F and four M (mean age 49.36 years), were recruited from January 2019-February 2021. All patients underwent AA treatment: two sessions per week for four weeks, for a total of eight sessions. At the beginning of therapy (T0) and at the end of the cycle (T1) the following data were evaluated: maximum mouth opening (MMO); cranio-facial pain related to TMD (verbal numeric scale, VNS); pain interference with normal activities and quality of life of patients (Brief Pain Inventory, BPI); oral functioning (Oral Behavior Checklist, OBC); impression of treatment effectiveness (Patients’ Global Impression of Improvement, PGI-I Scale). Statistical comparison of data before and after the AA treatment was performed by Wilcoxon’s signed-rank test (significance level p < 0.05).
Results: The MMO values were significantly improved after one cycle of AA (p = 0.0002). In addition, TMD-related pain had a statistically significant decline following AA treatment (all p < 0.001). Patients’ general activity and quality of life (BPI) were described as improved following a course of AA, with statistically significant values for all aspects considered (all p < 0.05).
Conclusion: Abdominal acupuncture resulted in effective treatment of subacute/chronic resistant pain related to TMD, capable of improving mandibular function and facial pain, and reduced the interference of pain affecting patients’ quality of life.
_____________________
Shocked?
Me too!
This study did not include a control group. Such uncontrolled studies are not necessarily useless. In areas where there is no prior evidence, they can be a reasonable starting point for further research. In the case of TMD/acupuncture, however, this does not imply. Here we already have about a dozen controlled trials. This means an uncontrolled study cannot possibly contribute to our knowledge. This means that the present study is useless. And that, in turn, means it is unethical.
But even if we ignore all this, the study is very misleading. It concludes that acupuncture improved TMD. This, however, can be doubted!
- What about placebo?
- What about regression toward the mean?
- What about the natural history of the condition?
Bad science is regrettable and dangerous, as it
- wastes resources,
- misleads vulnerable patients,
- violates ethics,
- and undermines trust in science.
I fear that the Italian group has just provided us with a prime example of these points.
Social prescribing (SP) has been mentioned here several times before. It seems important to so-called alternative medicine (SCAM), as some enthusiasts – not least King Charles – are trying to use it as a means to smuggle nonsensical treatments into routine healthcare.
SP is supposed to enable healthcare professionals to link patients with non-medical interventions available in the community to address underlying socioeconomic and behavioural determinants. The question, of course, is whether it has any relevant benefits.
This systematic review included all randomised controlled trials of SP among community-dwelling adults recruited from primary care or community setting, investigating any chronic disease risk factors defined by the WHO (behavioural factors: smoking, physical inactivity, unhealthy diet and excessive alcohol consumption; metabolic factors: raised blood pressure, overweight/obesity, hyperlipidaemia and hyperglycaemia). Random effect meta-analyses were performed at two time points: completion of intervention and follow-up after trial.
The researchers identified 9 reports from 8 trials totalling 4621 participants. All studies evaluated SP exercise interventions which were highly heterogeneous regarding the content, duration, frequency and length of follow-up. The majority of studies had some concerns about the risk of bias. A meta-analysis revealed that SP likely increased physical activity (completion: mean difference (MD) 21 min/week, 95% CI 3 to 39, I2=0%; follow-up ≤12 months: MD 19 min/week, 95% CI 8 to 29, I2=0%). However, SP may not improve markers of adiposity, blood pressure, glucose and serum lipid. There were no eligible studies that primarily target unhealthy diet, smoking or excessive alcohol-drinking behaviours.
The authors concluded that SP exercise interventions probably increased physical activity slightly; however, no benefits were observed for metabolic factors. Determining whether SP is effective in modifying the determinants of chronic diseases and promotes sustainable healthy behaviours is limited by the current evidence of quantification and uncertainty, warranting further rigorous studies.
Great! Regular exercise improves physical fitness.
But do we need SP for this?
Don’t get me wrong, I have nothing against connecting patients with social networks to improve their health and quality of life. I do, however, object if SP is used to smuggle unproven or disproven SCAMs into EBM. In addition, I ask myself whether we really need the new profession of a ‘link worker’ to facilitate SP. I remember being taught that a good doctor should look after his/her patients holistically, and surely that includes mentioning and facilitating social networks for those who need them.
I, therefore, fear that SP is taking something valuable out of the hands of doctors. And the irony is that SP is favoured by those who are all too quick to turn around and say: LOOK AT HOW FRIGHTFULLY REDUCTIONIST AND HEARTLESS DOCTORS HAVE BECOME. WE NEED MORE HOLISM IN MEDICINE AND THAT CAN ONLY BE PROVIDED BY SCAM PRACTITIONERS!
The claim that homeopathy has a role in oncology does not seem to go away. Some enthusiasts say it can be used as a causal therapy, while others insist it might be a helpful symptomatic adjuvant. Almost all oncologists agree that homeopathy has no place at all in cancer care.
Who is right?
This systematic review included clinical studies from 1800 until 2020 to evaluate evidence of the effectiveness of homeopathy on physical and mental conditions in patients during oncological treatment.
In February 2021 a systematic search was conducted searching five electronic databases (Embase, Cochrane, PsychInfo, CINAHL and Medline) to find studies concerning use, effectiveness, and potential harm of homeopathy in cancer patients.
From all 1352 search results, 18 studies with 2016 patients were included in this SR. The patients treated with homeopathy were mainly diagnosed with breast cancer. The therapy concepts included single and combination homeopathic remedies (used systemically or as mouth rinses) of various dilutions. The outcomes assessed were:
- the influence on toxicity of cancer treatment (mostly hot flashes and menopausal symptoms),
- the time to drain removal in breast cancer patients after mastectomy,
- survival,
- quality of life,
- global health,
- subjective well-being,
- anxiety and depression,
- safety and tolerance.
The included studies reported heterogeneous results: some studies described significant differences in quality of life or toxicity of cancer treatment favoring homeopathy, whereas others did not find an effect or reported significant differences to the disadvantage of homeopathy or side effects caused by homeopathy. The majority of the studies had low methodological quality.
The authors concluded that, the results for the effectiveness of homeopathy in cancer patients are heterogeneous, mostly not significant and fail to show an advantage of homeopathy over other active or passive comparison groups. No evidence can be provided that homeopathy exceeds the placebo effect. Furthermore, the majority of the included studies shows numerous and severe methodological weaknesses leading to a high level of bias and are consequently hardly reliable. Therefore, based on the findings of this SR, no evidence for positive effectiveness of homeopathy can be verified.
This could not be clearer. Some might argue that, of course, homeopathy cannot change the natural history of cancer, but it might improve the quality of life of those patients who believe in it via a placebo response. I would still oppose this notion: there are many effective treatments in the supportive treatment of cancer, and it seems much better to use those options and tell patients the truth about homeopathy.
Irritable bowel syndrome (IBS) is a common chronic disorder associated with psychological distress and reduced health-related quality of life (HRQoL). Therefore, stress management is often employed in the hope of alleviating IBS symptoms. But does it work?
This systematic review investigated the effects of stress management for adults with IBS on typical symptoms, HRQoL, and mental health. The predefined criteria included:
- patients: adults with IBS;
- intervention: stress management;
- control: care as usual or waitlist;
- outcome: patient-relevant;
- study-type: controlled trials.
Two researchers independently reviewed the publications retrieved through electronic searches and assessed the risk of bias using the Scottish Intercollegiate Guidelines Network checklist. The researchers performed a meta-analysis with homogeneous trials of acceptable quality.
After screening 6656 publications, 10 suitable randomized trials of acceptable (n = 5) or low methodological quality (n = 5) involving 587 patients were identified. The meta-analysis showed no effect of stress management on IBS severity 1-2 months after the intervention (Hedges’ g = -0.23, 95%-CI = -0.84 to -0.38, I2 = 86.1%), and after 3-12 months (Hedges’ g = -0.77, 95%-CI = -1.77 to -0.23, I2 = 93.3%). One trial found a short-term reduction of symptoms, and one trial found symptom relief in the long term (at 6 months). One of two studies that examined HRQoL found an improvement (after 2 months). One of two studies that examined depression and anxiety found a reduction of these symptoms (after 3 weeks).
The authors concluded that stress management may be beneficial for patients with IBS regarding the short-term reduction of bowel and mental health symptoms, whereas long-term benefits are unclear. Good quality RCTs with more than 6 months follow-up are needed.
Considering the actual evidence, I find the conclusions rather odd. Would it not have been more honest to state something along the following lines?:
There is currently no convincing evidence to suggest that stress management benefits IBS patients.
So why, be not more open and less misleading?
Could some of the authors’ affiliations provide a clue?
- Department for Internal and Integrative Medicine, Sozialstiftung Bamberg Hospital, Bamberg, Germany.
- Department for Integrative Medicine, University of Duisburg-Essen, Medical Faculty, Bamberg, Germany.
Quite possibly, yes!
Massages are experienced as agreeable by most patients. But that does not necessarily mean that it improves our quality of life. This study tests whether it does.
This study compared three massage dosing strategies among inpatients receiving palliative care consultation. It was designed as a three-armed randomized trial examining three different doses of therapist-applied massage to test change in overall quality of life (QoL) and symptoms among hospitalized adult patients receiving palliative care consultation for any indication:
- Arm I: 10-min massage daily × 3 days;
- Arm II: 20-min massage daily × 3 days;
- Arm III: single 20-min massage.
The primary outcome measure was the single-item McGill QoL question. Secondary outcomes measured pain/symptoms, rating of peacefulness, and satisfaction with the intervention. Data were collected at baseline, pre-and post-treatment, and one-day post-last treatment (follow-up). Repeated measure analysis of variance and paired t-test were used to determine significant differences.
A total of 387 patients participated (55.7 (±15.49) years old, mostly women (61.2%) and African-American (65.6%)). All three arms demonstrated within-group improvement at follow-up for McGill QoL (all P < 0.05). No significant between-group differences were found. Finally, repeated measure analyses demonstrated time to predict immediate improvement in distress (P ≤ 0.003) and pain (P ≤ 0.02) for all study arms; however, only improvement in distress was sustained at follow-up measurement in arms with three consecutive daily massages of 10 or 20 minutes.
The authors concluded that massage therapy in complex patients with advanced illness was beneficial beyond dosage. Findings support session length (10 or 20 minutes) was predictive of short-term improvements while treatment frequency (once or three consecutive days) predicted sustained improvement at follow-up.
I like this study because it teaches us an important lesson:
IF ONE DESIGNS A SILLY STUDY, ONE IS LIKELY TO ARRIVE AT A SILLY CONCLUSION.
This study does not have a proper control group. Therefore, we cannot know whether the observed outcomes were due to the different interventions or to non-specific effects such as expectation, the passing of time, etc.
The devil’s advocate conclusion of the findings is thus dramatically different from that of the authors: the results of this trial are consistent with the notion that massage has no effect on QoL, no matter how it is dosed.
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 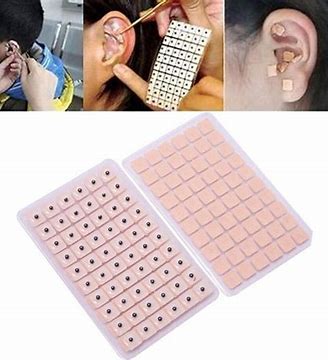
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.
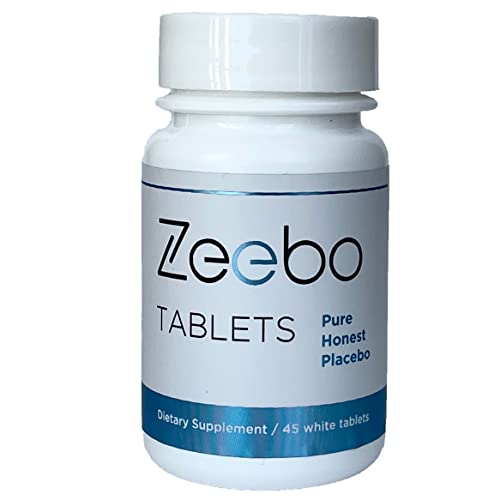
At first, I thought this was an ‘April fools’ joke. Then I looked at it a bit closer and realized that it seemed for real: Amazon is selling a placebo tablet. Here is how it is advertised:
- Honest Placebo Tablets by Zeebo Effect, inert ingredients, halal & kosher
- Focus on symptom relief, concentration, clarity, energy, calm, sleep
- Ze logo on each tablet, the original honest placebo brand trusted since 2014
- Randomized Controlled Trials with Zeebo Published in Journal for Pain, Nature, American Family Physician
- Each bottle is sealed with a transparent, tamper-proof neckband
Zeebo Tablets – Honest placebo tablets (white, round, 250mg each) are designed to help you create a safe placebo experience. Zeebo comes with the Ze logo on each tablet. Zeebo is made from an inert, natural fiber. Vegan, free of sugar or dyes. When it comes to Zeebo, You are the active ingredient. Users of Zeebo Tablets know they are taking a placebo containing only inert ingredients. Zeebo Tablets are taken intentionally obtain stress and pain relief, to release tension, irritability and nervousness, to help with calm and sleep serving as a sleep aid. Some of our customers take Zeebo Tablets to solicit placebo effects for increased mental focus, clarity, concentration, test performance and to sustain higher energy levels during physical exercise. Zeebo tablets are pure placebo, they are non-drowsy, non-homeopathic. There are no known interactions between Zeebo Placebo Tablets and other medications or supplements. Do not use Zeebo to delay or replace medical treatment. Visit zeeboeffect.com to learn about Zeebo. Look for the ebook The Placebo Cure to find out more about how to create your own Honest Placebo experience.
Take as needed. You may or may not respond to placebo. Do not use Zeebo to replace or delay medical treatment. Use Zeebo without deceit.*
* These statements have not been evaluated by the FDA. This product is not intended to diagnose, cure, treat, or prevent any disease.
Statements regarding dietary supplements have not been evaluated by the FDA and are not intended to diagnose, treat, cure, or prevent any disease or health condition.
Zeebo Tablets are an ethical placebo. People take it knowing it is a placebo. Take it without self-deceit. Zeebo is not made to look like any other ingestible. In fact, we think that the Zeebo branding can help enhance the experience. Have a look into ethical placebo or honest placebo studies. You will find a lot of research there, published in the journals Nature, Pain, for example. No need to trick yourself.
_________________________
After reading all this, I am again not entirely sure whether this is a hoax. If it is, I failed to get the fun of it. If it isn’t, there might be reasons for concern. When a placebo was marketed, a few years ago, THE GUARDIAN published opinions about the idea:
Jennifer Buettner, whose company Efficacy is marketing the placebo, says it can stimulate “the body’s ability to repair itself and the miracle power of the brain”. She said the company planned to distribute the pills, which cost £3 for 50, in the UK. “When drugs are not needed and the patient still thinks that medicine would help, we believe that the placebo effect can work,” she said.
But Dr Clare Gerada, vice-chair of the Royal College of GPs, described the pill as “medicalising love”, adding: “This placebo disempowers parents. It is telling them that unless you give your children this pill there’s nothing else.” Douglas Kamerow, associate editor of the British Medical Journal, said giving placebos to children was a “deeply bad idea”. Writing in the latest edition of the journal, he said: “The problems are numerous. Firstly, whom are we treating here, children or their parents?” He added that if parents used placebos to comfort their children they were teaching them that tablets are the answer for all life’s aches and pains.
As we have seen previously, the evidence on ‘open placebos’ is less impressive than many think. It makes me wonder whether the sale of placebo tablets is a good idea.
WHAT DO YOU THINK?