supplements
Many chiropractors seem to view the present pandemic as a business opportunity and make no end of false claims to attract customers. This has now been outlawed in the US. Medscape reported that a US district court will decide whether a chiropractor who is charged with 10 counts of making false marketing claims related to COVID-19 will be the first person convicted under a new federal law.
On his website, chiropractor ‘Dr.’ Eric Neptune advertises his services as follows:
Have you ever been told by your medical doctor that you or a member of your family had a specific disease, syndrome, or sickness? Did your doctor then recommend a drug or surgery to fix the issue, or tell you that you would have to live with it for the rest of your life? If so, you are not alone!
Nepute Wellness Center is unlike any medical clinic you may have been to. The clinic team is focused on finding and fixing the CAUSE of your problem vs. seeking out and treating only the SYMPTOMS. Nepute Wellness Center is equipped with state-of-the-art diagnostic equipment and testing, as well as medical doctors, nurses, and chiropractors who have been uniquely trained to treat your whole body, regardless of age, and return your body to a healthy balance so that it can heal itself the way God intended.
If you are tired of trying to treat your symptoms using prescription and over-the-counter pills, or even considering surgery, then Nepute Wellness Center may be right for you! Or like many, you want to be proactive with your health and prevent sickness and disease before you begin to suffer any symptoms, allowing you to live the full life you deserve, then make Nepute Wellness Center your partner in health!
Already over a year ago, Eric Nepute, the owner of Quickwork, based in St. Louis, Missouri, managed to make headlines. He had recorded a video that racked up more than 21 million views and suggested that drinking tonic water would prevent COVID-19 infections. Now, Mr. Neptune is the first person charged by the Federal Trade Commission (FTC) under the new COVID- 19 Consumer Protection Act. His company which has several locations in St. Louis County advertised its vitamin D and zinc products on social media and the internet as drugs that could treat or prevent COVID-19 claiming that their products are “more effective than the available COVID-19 vaccines”.
The FTC warned Nepute’s company in May 2020 about making unsubstantiated claims for other products regarding efficacy against COVID-19 and advised him to immediately stop making claims that were not supported by scientific evidence. However, Nepute seemed undeterred.
The FTC is seeking to fine Nepute and Quickwork up to US$43,792 for each violation of the COVID-19 Consumer Protection Act. In addition, the FTC seeks to bar the company from making health claims unless they are true and can be substantiated by scientific evidence.
Through his attorney, Neptune told the local NBC TV news affiliate, “I feel that I have not done anything wrong. I encourage everyone to live a healthy lifestyle during this unprecedented time. My attorneys are reviewing the complaint and I have no further comments at this time.”
The General Chiropractic Council’s (GCC) Registrant Survey 2020 was conducted in September and October 2020. Its aim was to gain valuable insights into the chiropractic profession to improve the GCC’s understanding of chiropractic professionals’ work and settings, qualifications, job satisfaction, responsibilities, clinical practice, future plans, the impact of the COVID-19 pandemic on practice, and optimism and pessimism about the future of the profession.
The survey involved a census of chiropractors registered with the GCC. It was administered online, with an invitation email was sent to every GCC registrant, followed by three reminders for those that had not responded to the survey. An open-access online survey was also available for registrants to complete if they did not respond to the mailings. This was promoted using the GCC website and social media channels. In total, 3,384 GCC registrants were eligible to take part in the survey. A fairly miserable response rate of 28.6% was achieved.
Here are 6 results that I found noteworthy:
- Registrants who worked in clinical practice were asked if performance was monitored at any of the clinical practices they worked at. Just over half (55%) said that it was and a third (33%) said it was not. A further 6% said they did not know and 6% preferred not to say. Of those who had their performance monitored, only 37% said that audits of clinical care were conducted.
- Registrants working in clinical practice were asked if any of their workplaces used a patient safety incident reporting system. Just under six in ten (58%) said at least one of them did, whilst 23% said none of their workplaces did. A further 12% did not know and 7% preferred not to say.
- Of the 13% who said they had a membership of a Specialist Faculty, a third (33%) said it was in paediatric chiropractic, 25% in sports chiropractic, and 16% in animal chiropractic. A further 13% said it was in pain and the same proportion (13%) in orthopaedics.
- Registrants who did not work in chiropractic research were asked if they intended to work in that setting in the next three years. Seven in ten (70%) said they did not intend to work in chiropractic research in the next three years, whilst 25% did not know or were undecided. Only 5% said they did intend to work in chiropractic research.
- Registrants were also asked how easy it is to keep up to date with recommendations and advances in clinical practice. Overall, two-thirds (67%) felt it was easy and 30% felt it was not.
- Registrants were asked in the survey whether they felt optimistic or pessimistic about the future of the profession over the next three years. Overall, half (50%) said they were optimistic and 23% were pessimistic. A further 27% said they were neither optimistic nor pessimistic.
Perhaps even more noteworthy are those survey questions and subject areas that might have provided interesting information but were not included in the survey. Here are some questions that spring into my mind:
- Do you believe in the concept of subluxation?
- Do you treat conditions other than spinal problems?
- How frequently do you use spinal manipulations?
- How often do you see adverse effects of spinal manipulation?
- Do you obtain informed consent from all patients?
- How often do you refer patients to medical doctors?
- Do you advise in favour of vaccinations?
- Do you follow the rules of evidence-based medicine?
- Do you offer advice about prescribed medications?
- Which supplements do you recommend?
- Do you recommend maintenance treatment?
I wonder why they were not included.
The Chinese have made several attempts to persuade us that their traditional remedies are effective for COVID-19 infections. Here is yet another one. This review summarised the evidence of the therapeutic effects and safety of Chinese herbal medicine (CHM) used with or without conventional western therapy for COVID-19. All clinical studies of the therapeutic effects and safety of CHM for COVID-19 were included. The authors
- summarized the general characteristics of included studies,
- evaluated the methodological quality of the randomized controlled trials (RCTs) using the Cochrane risk of bias tool,
- analyzed the use of CHM,
- used Revman 5.4 software to present the risk ratio (RR) or mean difference (MD) and their 95% confidence interval (CI) to estimate the therapeutic effects and safety of CHM.
A total of 58 clinical studies were identified including;
- 10 RCTs,
- 1 non-randomized controlled trials,
- 11 retrospective studies with a control group,
- 12 case-series,
- 24 case-reports.
All of the studies had been performed in China. No RCTs of high methodological quality were identified. The most frequently tested oral Chinese patent medicine, Chinese herbal medicine injection, or prescribed herbal decoction were:
- Lianhua Qingwen granule/capsule,
- Xuebijing injection,
- Maxing Shigan Tang.
The pooled analyses showed that there were statistical differences between the intervention group and the comparator group (RR 0.42, 95% CI 0.21 to 0.82, six RCTs; RR 0.38, 95% CI 0.23 to 0.64, five retrospective studies with a control group), indicating that CHM plus conventional western therapy appeared to be better than conventional western therapy alone in reducing aggravation rate.
In addition, compared with conventional western therapy, CHM plus conventional western therapy had the potential advantages in increasing the recovery rate and shortening the duration of fever, cough, and fatigue, improving the negative conversion rate of nucleic acid test, and increasing the improvement rate of chest CT manifestations and shortening the time from receiving the treatment to the beginning of chest CT manifestations improvement.
For adverse events, the pooled data showed that there were no statistical differences between the CHM and the control groups.
The authors concluded that current low certainty evidence suggests that there maybe a tendency that CHM plus conventional western therapy is superior to conventional western therapy alone. The use of CHM did not increase the risk of adverse events.
One of the principles to remember here is this: RUBBISH IN, RUBBISH OUT. If you meta-analyze primary data that are rubbish, your findings can only be rubbish as well.
All one needs to know about the primary data entered into the present analysis is that there were no rigorous RCTs… not one! That means the evidence is, as the authors rightly but modestly conclude of LOW CERTAINTY. My conclusions would have been a little different:
- In terms of safety, the dataset is too small and unreliable to make any judgment.
- In terms of efficacy, there is no sound data that CHM has a positive effect.
As I don’t live in the UK at present, I miss much of what the British papers report about so-called alternative medicine (SCAM). Therefore, I am a bit late to stumble over an article on the business activities of our Royals. It brought back into memory a little tiff I had with Prince Charles.
The article in the Express includes the following passage:

The UK’s first professor of complementary medicine, Edzard Ernst, dubbed the Duchy Originals detox tincture — which was being sold on the market at the time — “outright quackery”.
The product, called Duchy Herbals’ Detox Tincture, was advertised as a “natural aid to digestion and supports the body’s elimination processes” and a “food supplement to help eliminate toxins and aid digestion”.
The artichoke and dandelion mix cost £10 for a 50ml bottle.
Yet, Professor Ernst said Charles and his advisers seemed to be ignoring the science in favour of relying on “make-believe” and “superstition”, and said the suggestion that such products could remove bodily toxins was “implausible, unproven and dangerous”.
He noted: “Prince Charles thus financially exploits a gullible public in a time of financial hardship.”
This passage describes things accurately but not completely. What actually happened was this:
Unbeknown to me and with the help of some herbalists, Duchy Originals had developed the ‘detox tincture’ during a time when I was researching the evidence about ‘detox’. Eventually, my research was published as a review of the detox concept:
Background: The concept that alternative therapies can eliminate toxins and toxicants from the body, i.e. ‘alternative detox’ (AD) is popular.
Sources of data: Selected textbooks and articles on the subject of AD.
Areas of agreement: The principles of AD make no sense from a scientific perspective and there is no clinical evidence to support them.
Areas of controversy: The promotion of AD treatments provides income for some entrepreneurs but has the potential to cause harm to patients and consumers.
Growing points: In alternative medicine, simplistic but incorrect concepts such as AD abound. AREAS TIMELY FOR RESEARCH: All therapeutic claims should be scientifically tested before being advertised-and AD cannot be an exception.
When I was asked by a journalist what I thought about Charles’ new ‘detox tincture’, I told her that it was not supported by evidence which clearly makes it quackery. I also joked that Duchy Originals could thus be called ‘Dodgy Originals’. The result was this newspaper article and a subsequent media storm in the proverbial teacup.
At Exeter University, I had just fallen out of favor because of the ‘Smallwood Report’ and the complaint my involvement in it prompted by Charles’ first private secretary (full story in my memoir). After the ‘Dodgy Originals story’ had hit the papers, I was summoned ominously to my dean, Prof John Tooke, who probably had intended to give me a dressing down of major proportions. By the time we were able to meet, a few weeks later, the MHRA had already reprimanded Duchy Originals for misleading advertising which took most of the wind out of Tooke’s sail. The dressing down thus turned into something like “do you have to be so undiplomatic all the time?”.
Several months later, I was invited by the Science Media Centre, London, to give a lecture on the occasion of my retirement (Fiona Fox, the head of the SMC, had felt that, since my own University does not have the politeness to run a valedictory lecture for me, she will organize one for journalists). In that short lecture, I tried to summarize 19 years of research which inevitably meant briefly mentioning Charles and his foray into detox.
When I had finished, there were many questions from the journalists. Jenny Hope from the Daily Mail asked, “You mentioned snake-oil salesmen in your talk, and you also mentioned Prince Charles and his tinctures. Do you think that Prince Charles is a snake-oil salesman?” My answer was brief and to the point: “Yes“. The next day, this was all over the press. The Mail’s article was entitled ‘Charles? He’s just a snake-oil salesman: Professor attacks prince on ‘dodgy’ alternative remedies‘.
The advice of Tooke (who by then had left Exeter) to be more diplomatic had evidently not borne fruits (but the tinctures were discreetly taken off the market).
Diplomatic or honest?
This has been a question that I had to ask myself regularly during my 19 years at Exeter. For about 10 years, I had tried my best to walk the ‘diplomatic route’. When I realised that, in alternative medicine, the truth is much more important than diplomacy, I gradually changed … and despite all the hassle and hardship it brought me, I do not regret the decision.
As we have often discussed, proponents of so-called alternative medicine (SCAM), have an unfortunate tendency to mislead the public about vitamins and other supplements. Consequently, there is much uncertainty in many people’s minds. It is, therefore, all the more important to highlight new information that might counter this phenomenon.
This study tested whether high-dose zinc and/or high-dose ascorbic acid reduce the severity or duration of symptoms compared with usual care among ambulatory patients with SARS-CoV-2 infection. It was designed as a multicenter, single health system randomized clinical factorial open-label trial and enrolled 214 adult patients with a diagnosis of SARS-CoV-2 infection confirmed with a polymerase chain reaction assay who received outpatient care in sites in Ohio and Florida. The trial was conducted from April 27, 2020, to October 14, 2020.
Patients were randomized in a 1:1:1:1 allocation ratio to receive either:
- zinc gluconate (50 mg),
- ascorbic acid (8000 mg),
- both of these agents,
- standard care only.
The treatments lasted 10 days.
The primary endpoint was the number of days required to reach a 50% reduction in symptoms, including the severity of fever, cough, shortness of breath, and fatigue (rated on a 4-point scale for each symptom). Secondary endpoints included days required to reach a total symptom severity score of 0, cumulative severity score at day 5, hospitalizations, deaths, adjunctive prescribed medications, and adverse effects of the study supplements.
A total of 214 patients were randomized, with a mean (SD) age of 45.2 (14.6) years and 132 (61.7%) women. The study was stopped for a low conditional power for benefit with no significant difference among the 4 groups for the primary endpoint. Patients who received usual care without supplementation achieved a 50% reduction in symptoms at a mean (SD) of 6.7 (4.4) days compared with 5.5 (3.7) days for the ascorbic acid group, 5.9 (4.9) days for the zinc gluconate group, and 5.5 (3.4) days for the group receiving both (overall P = .45). There was no significant difference in secondary outcomes among the treatment groups.
The authors concluded that, in this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
This study has several limitations (and its authors are laudably frank about them):
- Its sample size is small.
- It has no placebo control group.
- It is open-label.
- Patients were not masked to which therapy they received.
The trial nevertheless adds important information about the value of using zinc or vitamin C or both in the management of COVID patients.
On Twitter, the hype had begun even before its text was available. Priti Gandhi, for instance, tweeted:
Yet another feather in India’s cap!! 1st evidence-based, CoPP-WHO GMP certified medicine for Covid-19 released today. Congratulations to @yogrishiramdev ji, @Ach_Balkrishna ji & the team of scientists at Patanjali Research Institute. Your efforts have been successful!! #Ayurveda
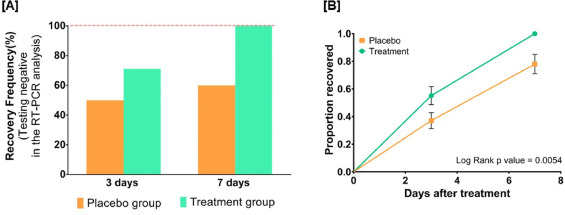
So, what is it all about? This study included 100 patients and was designed to evaluate the impact of traditional Indian Ayurvedic treatment on asymptomatic patients with COVID-19 infection. It is a placebo-controlled randomized double-blind pilot clinical trial that was conducted at the Department of Medicine in the National Institute of Medical Sciences and Research, Jaipur, India.
- 1 g of Giloy Ghanvati (Tinospora cordifolia)
- 2 g of Swasari Ras (traditional herbo-mineral formulation)
- 0.5 g of Ashwagandha (Withania somnifera)
- 0.5 g of Tulsi Ghanvati (Ocimum sanctum)
The treatment was given orally to the patients in the treatment group twice per day for 7 days. Medicines were given in the form of tablets and each tablet weighed 500 mg. While Swasari Ras was administered in powdered form, 30 min before breakfasts and dinners, rest were scheduled for 30 min post-meals. Patients in the treatment group also received 4 drops of Anu taila (traditional nasal drop) in each nostril every day 1 h before breakfast. Patients in the placebo group received identical-looking tablets and drops, post-randomization, and double-blinded assortments. 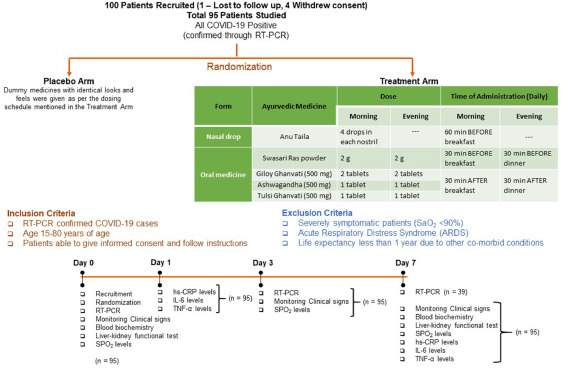 The RT-qPCR test was used for the detection of viral load in the nasopharyngeal and oropharyngeal swab samples of study participants during the study. Chemiluminescent immunometric assay was used to quantify serum levels of interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), and high sensitivity C-reactive protein (hs-CRP) on day 1 and day 7 of the study. Patient testing negative for SARS-CoV-2 in the RT-PCR analysis was the primary outcome of this study.
The RT-qPCR test was used for the detection of viral load in the nasopharyngeal and oropharyngeal swab samples of study participants during the study. Chemiluminescent immunometric assay was used to quantify serum levels of interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), and high sensitivity C-reactive protein (hs-CRP) on day 1 and day 7 of the study. Patient testing negative for SARS-CoV-2 in the RT-PCR analysis was the primary outcome of this study.
By day three, 71.1 % and 50.0 % of patients recovered in the treatment and placebo groups, respectively. The treatment group witnessed 100 % recovery by day 7, while it was 60.0 % in the placebo group. Average fold changes in serum levels of hs-CRP, IL-6, and TNF-α in the treatment group were respectively, 12.4, 2.5 and 20 times lesser than those in the placebo group at day 7. There was a 40 % absolute reduction in the risk of delayed recovery from infection in the treatment group.
The authors concluded that Ayurvedic treatment can expedite virological clearance, help in faster recovery and concomitantly reduce the risk of viral dissemination. Reduced inflammation markers suggested less severity of SARS-CoV-2 infection in the treatment group. Moreover, there was no adverse effect observed to be associated with this treatment.
I have the following concerns or questions about this trial:
- Why do the authors call it a pilot study? A pilot study is merely for testing the feasibility of a trial design and is not meant to yield definitive efficacy results.
- The authors state that the patients were asymptomatic yet in the discussion they claim they were asymptomatic or mildly symptomatic.
- Some of the effect sizes reported here are extraordinary and seem almost too good to be true.
- The claim of no adverse effect is implausible; even placebos would cause perceived adverse effects in a percentage of patients.
- If the study is solid and withstands the scrutiny of the raw data, it is of huge relevance for public health. So, why did the authors publish it in PHYTOMEDICINE, a relatively minor and little-known journal?
An article in The Economic Times’ reported this:
Patanjali Ayurved released what it called the first “evidence-based” medicine for Covid-19 on Friday. It claimed it has been “recognised by the WHO (World Health Organization) as an ayurvedic medicine for corona”.
Patanjali promoter, yoga guru Baba Ramdev, released a scientific research paper in this regard at the launch, presided over by Union health minister Harsh Vardhan and transport minister Nitin Gadkari.
The Ayurveda products maker said it has received a certification from the Ayush ministry. “Coronil has received the Certificate of Pharmaceutical Product (CoPP) from the Ayush section of Central Drugs Standard Control Organisation (CDSCO) as per the WHO certification scheme,” it said in a statement.
Under the CoPP, Coronil can be exported to 158 countries, the company said, adding that based on the presented data, the ministry has recognised Coronil as medicine for “supporting measure in Covid-19”.
Am I the only one who fears that something is not entirely kosher about the study? (This is an honest question, and I would be pleased to receive answers from my readers)
“Today, scientists note that the glycyrrhizic acid contained in this plant prevents the development of a new coronavirus, which the whole world is fighting against. Moreover, even a small concentration of an aqueous extract of licorice root has a neutralizing effect.”

These are the words of President Gurbanguly Berdymukhamedov of Turkmenistan. The plant he referred to is licorice. With is the promotion of a herbal solution for the pandemic, he is in good company:
- Thailand’s health ministry approved the use of Andrographis Paniculata, commonly known as green chiretta, to treat patients who are in the early stages of a Covid-19 infection.
- The health authorities of Tamil Nadu distributed herbal medicine to the general public as a preventive measure against Coronavirus disease.
- Madagascar claims to have a cure for Covid-19, the herbal tea named Covid-Organics has the plant artemisia as an ingredient.
- China has been using TCM alongside conventional treatment methods to treat Covid-19 patients. Some of the herbal formulations used in the treatment are:
- Jinhua Qinggan Granule
- Sheganmahuang decoction
- Lianhuaqingwen capsule
- Maxingshigan decoction
- Xuebijing Injection
- Indonesia is testing two herbal medicines: Cordyceps militaris, a fungus common in the Himalayas, and a herbal formulation comprising Ginger, gripeweed, Ngai camphor, and Andrographis paniculata.
And what about some evidence? In 2020, Medline listed 302 articles on herbal medicine for COVID-19. Here I selected just 10 of them to give you a flavor:
COVID-19 is the most recently discovered coronavirus infectious disease and leads to pandemic all over the world. The clinical continuum of COVID-19 varies from mild illness with non-specific signs and symptoms of acute respiratory disease to extreme respiratory pneumonia and septic shock. It can transmit from animal to human in the form of touch, through the air, water, utensils, fomite and feco-oral route blood. The pathogenesis and clinical features of COVID-19 be the same as the clinical manifestation associated epidemic Fever. In Unani medicine, various herbal drugs are described under the caption of epidemic disease. Great Unani scholar also Avicenna (980-1037 AD) recommended that during epidemic condition movement should be restricted, self-isolation, fumigation around the habitant with perfumed herbs (Ood, Kafoor, Sumbuluttib, Saad Kofi, Loban, etc.), and use of appropriate antidotes (Tiryaqe Wabai) and vinegar (Sirka) as prophylaxis. Herbal approach is based on single (Unnab-Ziziphus jujuba, Sapistan-Cordia myxa, Bahidana-Cydonia oblonga, Khatmi-Althea officinalis, Khubazi-Malva sylvestris, Zafran-Crocus sativus, Sibr-Aloe barbedensis, Murmuki-Commiphora myrrha, Darchini-Cinnamomum zeylanicum, Qaranfal-Syzygium aromaticum, Rihan-Oscimum sanctum, Habtus Sauda-Nigella sativa, Aslus Sus-Glycyrrhiza glabra, Maghze Amaltas-Cassia fistula and Adusa-Adhatoda vasica) and compound drugs (Habbe Bukhar, Sharbat Khaksi, Sharbat Zanjabeel, Naqu Nazla, Majoon Chobchini, Jawrish Jalinus and Khamira Marvareed) most of them are claimed for anti-viral, anti-pyretic, blood purifier, cardioprotective and expectorant activities. Traditionally most of the herbal practitioners are using it.
According to the World Health Organization (WHO), viral diseases continue to rise, and pose a significant public health problem. Novel coronavirus disease (COVID-19) is an infectious disease caused by SARS-CoV-2. The pathogenesis and clinical manifestations of COVID-19 is close to Amraz-e-Wabai (epidemic diseases) which was described by Hippocrates, Galen, Aristotle, Razes, Haly Abbas, Avicenna, Jurjani etc. Presently, there is no specific or challenging treatment available for COVID-19. Renowned Unani Scholars recommended during epidemic situation to stay at home, and fumigate the shelters with aromatics herbs like Ood kham (Aquilaria agallocha Roxb.), Kundur (Boswellia serrata Roxb), Kafoor (Cinnamomum camphora L.), Sandal (Santalum album L), Hing (Ferula foetida L.) etc. Use of specific Unani formulations are claimed effective for the management of such epidemic or pandemic situation like antidotes (Tiryaqe Wabai, Tiryaqe Arba, Tiryaqe Azam, Gile Armani), Herbal Decoction (Joshandah), along with Sharbate Khaksi, Habbe Bukhar, Sharbate Zanjabeel, Khamira Marwareed, Jawarish Jalinus, and Sirka (vinegar). Such drugs are claimed for use as antioxidant, immunomodulatory, cardiotonic, and general tonic actions. The study enumerates the literature regarding management of epidemics in Unani medicine and attempts to look the same in the perspective of COVID-19 prevention and management.
Unani system of medicine is based on the humoral theory postulated by Hippocrates, according to him the state of body health and disease are regulated by qualitative and quantitative equilibrium of four humours. Amraz-e-Waba is an umbrella term which is used in Unani medicine for all types of epidemics (smallpox, measles, plague, Hameer Saifi, influenza, Nipaha, Ebola, Zika, and 2019 novel coronavirus, etc.) mostly fatal in nature. The coronavirus disease 2019 (COVID-19) is a severe acute respiratory infection, and the pathogenesis and clinical features resemble with those of Nazla-e-Wabaiya (influenza) and Zatul Riya (pneumonia) which were well described many years ago in Unani text such as high-grade fever, headache, nausea and vomiting, running nose, dry cough, respiratory distress, alternate and small pulse, asthenia, foul smell from breath, insomnia, frothy stool, syncope, coldness in both upper and lower extremities, etc. The World Health Organization declared COVID-19 as a global emergency pandemic. Unani scholars like Hippocrates (370-460 BC), Galen (130-200 AD), Rhazes (865-925 AD), and Avicenna (980-1037 AD) had described four etiological factors for Amraz-e-Waba viz., change in quality of air, water, Earth, and celestial bodies, accordingly mentioned various preventive measures to be adopted during epidemics such as restriction of movement, isolation or “quarantena”, and fumigation with loban (Styrax benzoin W. G. Craib ex Hartwich.), sandalwood (Santalum album L.), Zafran (Crocus sativus L.), myrtle (Myrtus communis L.), and roses (Rosa damascena Mill.) and use of vinegar (sirka) and antidotes (Tiryaq) as prophylaxis, and avoiding consumption of milk, oil, sweet, meat, and alcohol. This review focuses and elaborates on the concept, prevention, and probable management of COVID-19 in the light of Amraz-e-Waba.
Background: Current recommendations for the self-management of SARS-Cov-2 disease (COVID-19) include self-isolation, rest, hydration, and the use of NSAID in case of high fever only. It is expected that many patients will add other symptomatic/adjuvant treatments, such as herbal medicines.
Aims: To provide a benefits/risks assessment of selected herbal medicines traditionally indicated for “respiratory diseases” within the current frame of the COVID-19 pandemic as an adjuvant treatment.
Method: The plant selection was primarily based on species listed by the WHO and EMA, but some other herbal remedies were considered due to their widespread use in respiratory conditions. Preclinical and clinical data on their efficacy and safety were collected from authoritative sources. The target population were adults with early and mild flu symptoms without underlying conditions. These were evaluated according to a modified PrOACT-URL method with paracetamol, ibuprofen, and codeine as reference drugs. The benefits/risks balance of the treatments was classified as positive, promising, negative, and unknown.
Results: A total of 39 herbal medicines were identified as very likely to appeal to the COVID-19 patient. According to our method, the benefits/risks assessment of the herbal medicines was found to be positive in 5 cases (Althaea officinalis, Commiphora molmol, Glycyrrhiza glabra, Hedera helix, and Sambucus nigra), promising in 12 cases (Allium sativum, Andrographis paniculata, Echinacea angustifolia, Echinacea purpurea, Eucalyptus globulus essential oil, Justicia pectoralis, Magnolia officinalis, Mikania glomerata, Pelargonium sidoides, Pimpinella anisum, Salix sp, Zingiber officinale), and unknown for the rest. On the same grounds, only ibuprofen resulted promising, but we could not find compelling evidence to endorse the use of paracetamol and/or codeine.
Conclusions: Our work suggests that several herbal medicines have safety margins superior to those of reference drugs and enough levels of evidence to start a clinical discussion about their potential use as adjuvants in the treatment of early/mild common flu in otherwise healthy adults within the context of COVID-19. While these herbal medicines will not cure or prevent the flu, they may both improve general patient well-being and offer them an opportunity to personalize the therapeutic approaches.
Recently, the novel life-threatening coronavirus infection (COVID-19) was reported at the end of 2019 in Wuhan, China, and spread throughout the world in little time. The effective antiviral activities of natural products have been proved in different studies. In this review, regarding the effective herbal treatments on other coronavirus infections, promising natural products for COVID-19 treatment are suggested. An extensive search in Google Scholar, Science Direct, PubMed, ISI, and Scopus was done with search words include coronavirus, COVID-19, SARS, MERS, natural product, herb, plant, and extract. The consumption of herbal medicine such as Allium sativum, Camellia sinensis, Zingiber officinale, Nigella sativa, Echinacea spp. Hypericum perforatum, and Glycyrrhiza glabra, Scutellaria baicalensis can improve the immune response. It seems that different types of terpenoids have promising effects in viral replication inhibition and could be introduced for future studies. Additionally, some alkaloid structures such as homoharringtonine, lycorine, and emetine have strong anti-coronavirus effects. Natural products can inhibit different coronavirus targets such as S protein (emodin, baicalin) and viral enzymes replication such as 3CLpro (Iguesterin), PLpro (Cryptotanshinone), helicase (Silvestrol), and RdRp (Sotetsuflavone). Based on previous studies, natural products can be introduced as preventive and therapeutic agents in the fight against coronavirus.
Background: The aim of the present review is to provide basic knowledge about the treatment of Coronavirus via medicinal plants. Coronavirus (COVID-19, SARS-CoV, and MERS-CoV) as a viral pneumonia causative agent, infects thousands of people in China and worldwide. There is currently no specific medicine or vaccine available and it is considered a threat to develop effective novel drug or anti-coronavirus vaccine treatment. However, natural compounds to treat coronaviruses are the most alternative and complementary therapies due to their diverse range of biological and therapeutic properties.
Methods: We performed an open-ended, English restricted search of Scopus database, Web of Science, and Pubmed for all available literature from Jan-March, 2020, using terms related to phytochemical compounds, medicinal plants and coronavirus.
Results: The view on anti-coronavirus (anti-CoV) activity in the plant derived phytochemicals and medicinal plants give the strong base to develop a novel treatment of corona virus activity. Various phytochemicals and medicinal plant extracts have been revised and considered to be the potential anti-CoV agents for effective control and future drug development. We discuss some important plants (Scutellaria baicalensis, Psorothamnus arborescens, Glycyrrhiza radix, Glycyrrhiza uralensis , Lycoris radiate, Phyllanthus emblica, Camellia sinensis, Hyptis atrorubens Poit, Fraxinus sieboldiana, Erigeron breviscapus, Citri Reticulatae Pericarpium, Amaranthus tricolor, Phaseolus vulgaris, Rheum palmatum, Curcuma longa and Myrica cerifera) emerged to have broad spectrum antiviral activity.
Conclusion: Nigella sativa has potent anti-SARS-CoV activity and it might be useful souce for developing novel antiviral therapies for coronaviruses.
COVID-19 has been declared a pandemic by WHO on March 11, 2020. No specific treatment and vaccine with documented safety and efficacy for the disease have been established. Hence it is of utmost importance to identify more therapeutics such as Chinese medicine formulae to meet the urgent need. Qing Fei Pai Du Tang (QFPDT), a Chinese medicine formula consisting of 21 herbs from five classical formulae has been reported to be efficacious on COVID-19 in 10 provinces in mainland China. QFPDT could prevent the progression from mild cases and shorten the average duration of symptoms and hospital stay. It has been recommended in the 6th and 7th versions of Clinical Practice Guideline on COVID-19 in China. The basic scientific studies, supported by network pharmacology, on the possible therapeutic targets of QFPDT and its constituent herbs including Ephedra sinica, Bupleurum chinense, Pogostemon cablin, Cinnamomum cassia, Scutellaria baicalensis were reviewed. The anti-oxidation, immuno-modulation and antiviral mechanisms through different pathways were collated. Two clusters of actions identified were cytokine storm prevention and angiotensin converting enzyme 2 (ACE2) receptor binding regulation. The multi-target mechanisms of QFPDT for treating viral infection in general and COVID-19 in particular were validated. While large scale clinical studies on QFPDT are being conducted in China, one should use real world data for exploration of integrative treatment with inclusion of pharmacokinetic, pharmacodynamic and herb-drug interaction studies.
In December 2019, a novel coronavirus SARS-CoV-2, causing the disease COVID-19, spread from Wuhan throughout China and has infected people over 200 countries. Thus far, more than 3,400,000 cases and 240,000 deaths have occurred worldwide, and the coronavirus pandemic continues to grip the globe. While numbers of cases in China have been steadying, the number of infections outside China is increasing at a worrying pace. We face an urgent need to control the spread of the COVID-19 epidemic, which is currently expanding to a global pandemic. Efforts have focused on testing antiviral drugs and vaccines, but there is currently no treatment specifically approved. Traditional Chinese medicine (TCM) is grounded in empirical observations and the Chinese people use TCM to overcome these sorts of plagues many times in thousands of years of history. Currently, the Chinese National Health Commission recommended a TCM prescription of Qing-Fei-Pai-Du-Tang (QFPDT) in the latest version of the “Diagnosis and Treatment guidelines of COVID-19” which has been reported to provide reliable effects for COVID-19. While doubts about TCM still exist today, this review paper will describe the rationalities that QFPDT is likely to bring a safe and effective treatment of COVID-19.
The fight against the novel coronavirus pneumonia (namely COVID-19) that seriously harms human health is a common task for all mankind. Currently, development of drugs against the novel coronavirus (namely SARS-CoV-2) is quite urgent. Chinese medical workers and scientific researchers have found some drugs to play potential therapeutic effects on COVID-19 at the cellular level or in preliminary clinical trials. However, more fundamental studies and large sample clinical trials need to be done to ensure the efficacy and safety of these drugs. The adoption of these drugs without further testing must be careful. The relevant articles, news, and government reports published on the official and Preprint websites, PubMed and China National Knowledge Infrastructure (CNKI) databases from December 2019 to April 2020 were searched and manually filtered. The general pharmacological characteristics, indications, adverse reactions, general usage, and especially current status of the treatment of COVID-19 of those potentially effective drugs, including chemical drugs, traditional Chinese medicines (TCMs), and biological products in China were summarized in this review to guide reasonable medication and the development of specific drugs for the treatment of COVID-19.
Objective: To analysis the medication characteristics of the prescriptions issued via open channel by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine in treating coronavirus disease 2019 (COVID-19).
Methods: We collected the data of traditional Chinese medicine related to treatment plans published by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine from the start of COVID-19 outbreak to February 19, 2020. The frequency analysis, cluster analysis and association analysis were performed.
Results: The study collected 4 national and 34 regional prevention and treatment plans, 578 items, 84 traditional Chinese formulations, 60 Chinese patent medicines, and 230 Chinese herbs. The high frequently used herbs were Liquorice, Scutellariabaicalensis, Semen armeniacaeamarae, and Gypsum. The commonly used traditional formulations included Maxing Shigan decoction, Yin Qiao powder, and Xuanbai Chengqi decoction. The Chinese patent drugs included Angong Niuhuang pill, Xuebijing injection, and Lianhua Qingwen capsule. The most common paired medications were Ephedra and Semen armeniacaeamarae, Fructusforsythiae and Liquorice. Two core combinations and one novel formula were discovered in the study.
Conclusions: Yin Qiao powder and Huopo Xialing decoction are the basic formulations for Weifen syndrome of COVID-19. In addition, Maxing Shigan decoction, Liang Ge powder, Qingwen Baidu decoction and Da Yuan decoction are the basic formulations for Qifen syndrome of COVID-19. The main medication characteristics are clearing heat, entilating lung, removing toxicity and removing turbidity. It shows that removing toxicity and eliminating evil are the prescription thought in treating epidemic disease of traditional Chinese medicine.
Confused?
Me too!
What seems to emerge is this:
- ‘Herbalists and Co’ did not wait long to jump on the corona bandwagon.
- They managed to confuse not just you and me, but even politicians, presidents, and their advisers.
- They produced a plethora of articles implying that an endless array of herbs might be effective.
- In doing so, no clear consensus emerged as to which herbs are the most promising.
- Sound evidence seems to be not available.
- Clinical trials are slow to start or not even planned.
- Everything is based on more or less wild extrapolation.
- Much of what is being published is borderline irresponsible.
- YET, IT MUST BE GOOD FOR BUSINESS!
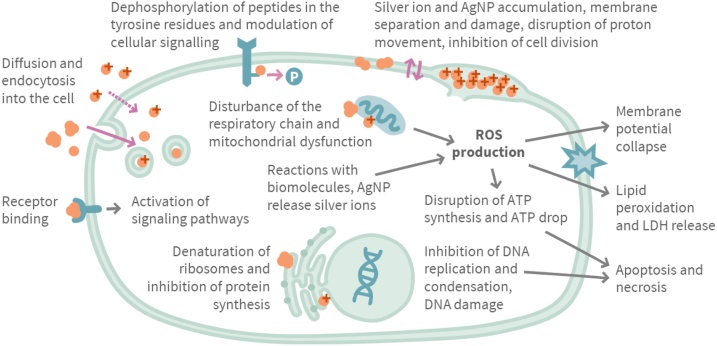
The aim of this investigation was to evaluate the marketing practices, beliefs and health claims regarding the use of colloidal silver in Finland. Contents of three company websites selling colloidal silver were reviewed, and the claims used in the marketing of colloidal silver were compared to the scientific information about silver. In Facebook posts and discussion about colloidal silver were analyzed.
In Finland, the marketing of colloidal silver products on websites selling the products did not follow the regulations of authorities; several scientifically unfounded claims about the efficacy and medical use of colloidal silver were found. After the Finnish Broadcasting Company (Yle) documentary and an intervention by authorities, contents of the websites were changed, but still questionable information and misleading claims could be found. In the analyzed Facebook groups attitudes towards medical use of colloidal silver were uncritically positive, internal use was highly promoted and the restrictions of use were considered unjustified.
The authors concluded that the use of quackery products such as colloidal silver can be dangerous, and their use and marketing should be controlled and restricted.
The authors stress that silver nanoparticles (AgNPs) are potentially toxic due to their small size and Ag+-release capabilities, and the use of colloidal silver products containing AgNPs can cause a wide variety of adverse effects such as argyria.
WebMD cautions that despite promoters’ claims, silver has no known function in the body and is not an essential mineral supplement. Colloidal silver products were once available as over-the-counter drug products. In 1999 the U.S. Food and Drug Administration (FDA) ruled that these colloidal silver products were not considered safe or effective. Colloidal silver products marketed for medical purposes or promoted for unproven uses are now considered “misbranded” under the law without appropriate FDA approval as a new drug. There are currently no FDA-approved over-the-counter or prescription drugs containing silver that are taken by mouth. However, there are still colloidal silver products being sold as homeopathic remedies and dietary supplements.
On this blog, we have discussed that colloidal silver is nevertheless marketed aggressively by crooks (see here and here). The message that emerges from all this seems clear: do not fall for the plethora of false claims made by irresponsible entrepreneurs who want your money and risk your health. Keep your money and health by staying away from colloidal silver and similar SCAMs.
We live in truly grim times! Let me therefore try to cheer you up a little. Here is a story that might make you smile.
In 1981, I moved back from London to Munich. While still in London, I had written an article on garlic for a German medical journal. It was published just as we arrived in our new home. Here is it’s English abstract:
Garlic has had a firm place in folk medicine since ancient times. More recent results are summarized here which show that extracts of the plant have an antimicrobial action, they are capable of lowering blood cholesterol and of reducing secondary vascular changes. They raise fibrinolytic activity and inhibit thrombocyte aggregation. Therefore the plant contains highly active therapeutic principles which appear to be particularly suitable for prophylaxis of arteriosclerosis.
Yes, you are quite right, this paper is nothing to write home about. So, why do I consider it ‘most consequential‘? Here is what happened:
My wife and I had barely arrived in our new home, when a man phoned (he had gone to a lot of trouble to find my number) and said: “I know you are the leading expert on garlic; I urgently need to talk to you”. Never correct a man’s mistake, if it’s in your favour, I thought, and we made an appointment for a meeting at the Munich train station hotel.
When I met him a few days later, he ordered me a coffee (which later I had to pay for) and explained that he had worked his whole life (he was about 50, I guessed) for the pharmaceutical industry and had now decided that this was enough. He thus planned to set up his own pharmaceutical company. He already had a photocopy machine in his basement, he proudly told me, and a wife who was willing to work as hard as he was. Specifically, his plan was to launch a garlic pill, and for that he needed my advice. I told him what he wanted to know, and we parted after about two hours promising to stay in contact.
The man’s name was Kuno Lichtwer.
During the weeks that followed, he often phoned me to pick my brain. One day, he told me that he had everything in place: he had found a supplier of the materials, a manufacturer to produce the pills and even registered a name for it:
KWAI

Then he popped the question that was foremost on his mind: ‘What do you think, Dr Ernst, should I risk it and go ahead with this or not?’. I had started to like that man; he was going to lose all his savings on a crazy idea, I felt. So, I told him: ‘If I were you, I would not do it. There are already plenty of garlic pills on the market. You are risking to lose everything.’ Then there was a long pause; eventually, he thanked me for my honest advice and hung up.
Weeks later he phoned again to tell me that he had truly appreciated my brutally direct advice, thought long and hard about it, but went ahead with his plan anyway. Would I now accept the position of ‘medical advisor’ to Lichwer Pharma? I was surprised, but accepted this new post. Thereafter, I advised him the best I could. We even conducted and published the very first clinical trial with his product. It was a rather flimsy study (we had no funds at all), but did suggest a positive result.
Each time Mr Lichtwer called me, he was elated; things were not just going well, they were booming! He was evidently hugely gifted in promoting KWAI. Then he invited me several times to come to Berlin where Lichtwer Pharma was based for business meetings. Proudly, he showed me that meanwhile his firm had moved out of his basement into a proper building. The next I knew was that he had a dozen employees. Lichtwer seemed unstoppable. This went on for 2 or 3 years, if I remember correctly.
During all this time, we had never talked about money, and my work for him had always been unpaid – that is, until one day just before Christmas he phoned and explained that he had moved his firm to yet a bigger building and hired yet more staff. He also realised that I deserved some renumeration for my advice; therefore, he had put a cheque in the post. When I told my wife about it, we both celebrated in anticipation of the substantial windfall. Two days later, his letter arrived. He very kindly thanked me for years of work and included a cheque of 500 DM (about 150 DM per year of work). A few months later, his firm had grown so big that a full time medical and research director was badly needed. He informed me that he had found a highly experienced expert and invited me to meet the new man, Prof Schulz.
No, I did not feel hard done by! On the contrary, I was happy that my prediction had been grossly wrong and that my friend Kuno was doing so well. In addition, I was also relieved, because my research at the University did not give me nearly enough time to look adequately after the now substantial firm of Lichtwer Pharma.
Thereafter, Lichtwer’s garlic pill went from strength to strength. Several larger studies confirmed our initial results that garlic positively influenced blood lipids (in 2000, our systematic review concluded: The available data suggest that garlic is superior to placebo in reducing total cholesterol levels. However, the size of the effect is modest, and the robustness of the effect is debatable. The use of garlic for hypercholesterolemia is therefore of questionable value). One day, I read somewhere that KWAI had become the most consumed pill in Germany (even beating Aspirin). Then Lichtwer Pharma went international and added several further herbal products to its portfolio. In 1991, Lichtwer Pharma was estimated to be worth 100 Million DM. Several years later, the firm had almost 400 employees and a yearly turnover of 353 Million DM.
To his credit, Kuno Lichtwer never entirely forgot me. When I had moved to the UK, he even came to Exeter, was entertained by my University, and made a donation of £100 000 towards a ‘Lichtwer Research Fellowship’ for my department. I am not sure whether Kuno Lichtwer is still alive. If he is, he would probably agree that, had I offered him 10 000 DM of my savings during our 1st meeting in 1981 (he did hint at that possibility), he would have gladly made me a partner in his enterprise.
But, as they say: money is not everything.
And a good story to tell is also not bad.
Hesperidin is a flavonoid found in citrus fruits, especially orange and grapefruit. It is said to have antioxidant and anti-inflammatory effects. Research into hesperidin began in the 1940s but only recently interest turned buoyant, and all sorts of benefits have been suggested. Here are just three recent clinical studies:
- This study investigated the effects of chronic intake of an orange extract (2S-hesperidin) or placebo on non-oxidative/glycolytic and oxidative metabolism markers and performance markers in amateur cyclists. A double-blind, randomized, placebo-controlled trial was carried out between late September and December 2018. Forty amateur cyclists were randomized into two groups: one taking 500 mg/day 2S-hesperidin and the other taking 500 mg/day placebo (microcellulose) for eight weeks. All participants completed the study. An incremental test was used to evaluate performance, and a step test was used to measure oxygen consumption, carbon dioxide, efficiency and oxidation of carbohydrates and fat by indirect calorimetry. The anaerobic power (non-oxidative) was determined using Wingate tests (30 s). After eight weeks supplementation, there was an increase in the incremental test in estimated functional threshold power (FTP) (3.2%; p ≤ 0.05) and maximum power (2.7%; p ≤ 0.05) with 2S-hesperdin compared to placebo. In the step test, there was a decrease in VO2 (L/min) (-8.3%; p ≤ 0.01) and VO2R (mL/kg/min) (-8.9%; p ≤ 0.01) at VT2 in placebo. However, there were no differences between groups. In the Wingate test, there was a significant increase (p ≤ 0.05) in peak and relative power in both groups, but without differences between groups. Supplementation with an orange extract (2S-hesperdin) 500 mg/day improves estimated FTP and maximum power performance in amateur cyclists.
- In this clinical trial with a parallel-group design, 49 patients with MetS received either 500-mg hesperidin or placebo, twice daily, for 12 weeks. Number of participants with treated MetS was considered as a primary end point. Anthropometric parameters, dietary intake, physical activity, lipid profile, glucose homeostasis parameter, tumor necrosis factor alpha (TNF-α), high-sensitivity C-reactive protein (hs-CRP) were assessed at the beginning and at the end of the study. Compared with the placebo group, hesperidin decreased fasting glucose level (- 6.07 vs. – 13.32 mg/dL, P = 0.043), triglyceride (- 8.83 vs. – 49.09 mg/dL, P = 0.049), systolic blood pressure (- 0.58 vs. – 2.68 mmHg, P = 0.048) and TNF-α (- 1.29 vs. – 4.44 pg/mL, P = 0.009). Based on the within-group analysis, hesperidin led to significant decrease in serum levels of glucose, insulin, triglyceride, total cholesterol, low density lipoprotein cholesterol, TNF-α and hs-CRP, while in control group only glucose and insulin significantly decreased. The results indicate that hesperidin supplementation can improve metabolic abnormalities and inflammatory status in patients with MetS.
- In this study, 64 patients were randomly allocated to receive 500 mg/day hesperidin or placebo capsules for 6 weeks. Data on systolic blood pressure (SBP), diastolic blood pressure, serum total antioxidant capacity (TAC), tumor necrosis factor alpha, interleukin 6 (IL-6), and high-sensitivity C-reactive protein (hs-CRP) were collected at the baseline and at the end of the study. In the hesperidin group, SBP (122.7 ± 8.5 vs. 119.0 ± 7.4; p = .005), mean arterial blood pressure (94.2 ± 5.5 vs. 91.8 ± 5.5; p = .009), IL-6 (8.3 ± 2.1 vs. 7.4 ± 1.8; p = .001), and hs-CRP (1.9 ± 1.2 vs. 1.1 ± 0.9; p < .000) decreased whereas TAC increased (0.74 ± 0.1 vs. 0.82 ± 0.1; p < .000) in comparison to the baseline values. There was a significant difference in mean percent change of SBP, diastolic blood pressure, mean arterial blood pressure, serum TAC, and inflammatory markers (tumor necrosis factor alpha, IL-6, and hs-CRP) between hesperidin and control groups following intervention in adjusted models (p < .05). These results suggest that hesperidin may have antihypertensive and anti-inflammatory effects in type 2 diabetes.

The latest suggestion for Hesperidin is – how could be be otherwise? – that it helps against COVID-19: Hesperidin can block coronavirus from entering host cells through ACE2 receptors which can prevent the infection. Anti-viral activity of hesperidin might constitute a treatment option for COVID-19 through improving host cellular immunity against infection and its good anti-inflammatory activity may help in controlling cytokine storm. Hesperidin mixture with diosmin co-administrated with heparin protect against venous thromboembolism which may prevent disease progression. Based on that, hesperidin might be used as a meaningful prophylactic agent and a promising adjuvant treatment option against SARS-CoV-2 infection.
According to one source, Hesperidin can cause several problems:
- abdominal pain,
- diarrhea,
- contact dermatitis,
- nausea,
- interactions with medications (including anticoagulants, blood pressure drugs, and calcium channel blockers),
- increased risk of bleeding.
No doubt, Hesperidin is an interesting substance. Yet, I feel that much more research is needed until we can be reasonably sure that it is clinically effective for any condition, particularly COVID-19.