study design
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 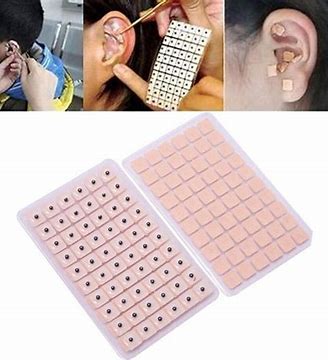
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.
This single-blind, randomized, clinical trial was aimed at determining the long-term clinical effects of spinal manipulative therapy (SMT) or mobilization (MOB) as an adjunct to neurodynamic mobilization (NM) in the management of individuals with Lumbar Disc Herniation with Radiculopathy (DHR).
Forty participants diagnosed as having a chronic DHR (≥3 months) were randomly allocated into two groups with 20 participants each in the SMT and MOB groups.
Participants in the SMT group received high-velocity, low-amplitude manipulation, while those in the MOB group received Mulligans’ spinal mobilization with leg movement. Each treatment group also received NM as a co-intervention, administered immediately after the SMT and MOB treatment sessions. Each group received treatment twice a week for 12 weeks.
The following outcomes were measured at baseline, 6, 12, 26, and 52 weeks post-randomization; back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
The results indicate that the MOB group improved significantly better than the SMT group in all outcomes (p < 0.05), and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks. These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups. The risk of being improved at 12 weeks post-randomization was 40% lower (RR = 0.6, CI = 0.4 to 0.9, p = 0.007) in the SMT group compared to the MOB group.
The authors concluded that this study found that individuals with DHR demonstrated better improvements when treated with MOB plus NM than when treated with SMT plus NM. These improvements were also clinically meaningful for activity limitation, functional mobility, and quality of life outcomes at long-term follow-up.
Yet again, I find it hard to resist playing the devil’s advocate: had the researchers added a third group with sham-MOB, they would have perhaps found that this group would have recovered even faster. In other words, this study might show that SMT is no good for DHR (which I find unsurprising), but it does NOT demonstrate MOB to be an effective therapy.
Guided imagery is said to distract patients from disturbing feelings and thoughts, positively affects emotional well-being, and reduce pain by producing pleasing mental images.
This study aimed to determine the effects of guided imagery on postoperative pain management in patients undergoing lower extremity surgery. This randomized controlled study was conducted between April 2018 and May 2019. It included 60 patients who underwent lower extremity surgery. After using guided imagery, the posttest mean Visual Analog Scale score of patients in the intervention group was found to be 2.56 (1.00 ± 6.00), whereas the posttest mean score of patients in the control group was 4.10 (3.00 ± 6.00), and the difference between the groups was statistically significant (p <.001).
The authors concluded that guided imagery reduces short-term postoperative pain after lower extremity surgery.
I did not want to spend $52 to access the full article. Therefore, I can only comment on what the abstract tells me – and that is regrettably not a lot.
In fact, we don’t even learn what treatment was given to the control group. I guess that both groups receive standard post-op care and the control group received nothing in addition. This would mean that the observed effect might be entirely due to placebo and other non-specific effects. If that is so, the authors’ conclusion is not accurate.
I happen to think that guided imagery is a promising albeit under-researched therapy. Therefore, I am particularly frustrated to see that the few trials that do emerge of this option are woefully inadequate to determine its value.
Menopausal symptoms are a domaine of so-called alternative medicine (SCAM), not least because many women are worried about hormone treatments and therefore want ‘something natural’. TCM practitioners are only too keen to offer their services. But do their treatments really work?
This study aimed to analyze the effectiveness of acupuncture combined with Chinese herbal medicine (CHM) on mood disorder symptoms for menopausal women.
A total of 95 qualified Chinese participants were randomly assigned to one of three groups:
- 31 in the acupuncture combined with CHM group (combined group),
- 32 in the acupuncture combined with CHM placebo group (acupuncture group),
- 32 in the CHM combined with sham acupuncture group (CHM group).
The patients were treated for 8 weeks and followed up for 4 weeks. The data were collected using the Greene Climacteric Scale (GCS), self-rating depression scale (SDS), self-rating anxiety scale (SAS), and safety index.
The three groups each showed significant decreases in the GCS, SDS, and SAS after treatment (p < 0.05). Furthermore, the effect on the GCS total score and the anxiety domain lasted until the follow-up period in the combined group (p < 0.05). Within the three groups, there was no difference in GCS and SAS between the three groups after treatment (p > 0.05). However, the combined group showed significant improvement in the SDS, compared with both the acupuncture group and the CHM group at 8 weeks and 12 weeks (p < 0.05). No obvious abnormal cases were found in any of the safety indexes.
The authors concluded that the results suggest that either acupuncture, or CHM or combined therapy offer safe improvement of mood disorder symptoms for menopausal women. However, the combination therapy was associated with more stable effects in the follow-up period and a superior effect on improving depression symptoms.
Previous reviews have drawn conclusions that are far less positive, e.g.:
- the observed clinical benefit associated with acupuncture may be due, in part, or in whole to nonspecific effects.
- the evidence gathered was not sufficient to affirm the effectiveness of traditional acupuncture compared with sham acupuncture.
- For natural menopause, one large study has shown acupuncture to be superior to self-care alone in reducing the number of hot flushes and improving the quality of life; five small studies have been unable to demonstrate that the effect of acupuncture is limited to any particular points, as traditional theory would suggest; and one study showed acupuncture was superior to blunt needle for flash frequency but not intensity.
- Sham-controlled RCTs fail to show specific effects of acupuncture for control of menopausal hot flushes.
It seems therefore wise to take the conclusions of the new study with a pinch of salt. The intergroup difference observed in this trial may well be due to residual biases, multiple testing, or coincidence. And the reported intragroup differences are in complete accord with the fact that the employed therapies are mere placebos.
This, of course, begs the question of whether SCAM has anything else to offer for women suffering from menopausal symptoms. To answer it, I can refer you to one of our systematic reviews:
Some evidence exists in favour of phytosterols and phytostanols for diminishing LDL and total cholesterol in postmenopausal women. Similarly, regular fiber intake is effective in reducing serum total cholesterol in hypercholesterolemic postmenopausal women. Clinical evidence also exists on the effectiveness of vitamin K, a combination of calcium and vitamin D or a combination of walking with other weight-bearing exercise in reducing bone mineral density loss and the incidence of fractures in postmenopausal women. Black cohosh appears to be effective therapy for relieving menopausal symptoms, primarily hot flashes, in early menopause. Phytoestrogen extracts, including isoflavones and lignans, appear to have only minimal effect on hot flashes but have other positive health effects, e.g. on plasma lipid levels and bone loss. For other commonly used CAMs, e.g. probiotics, prebiotics, acupuncture, homeopathy and DHEA-S, randomized, placebo-controlled trials are scarce and the evidence is unconvincing. More and better RCTs testing the effectiveness of these treatments are needed.
Hemiparesis is a severe impairment following a stroke that affects the majority of stroke patients. Rehabilitation is usually at least partly successful. But might results be improved with homeopathy?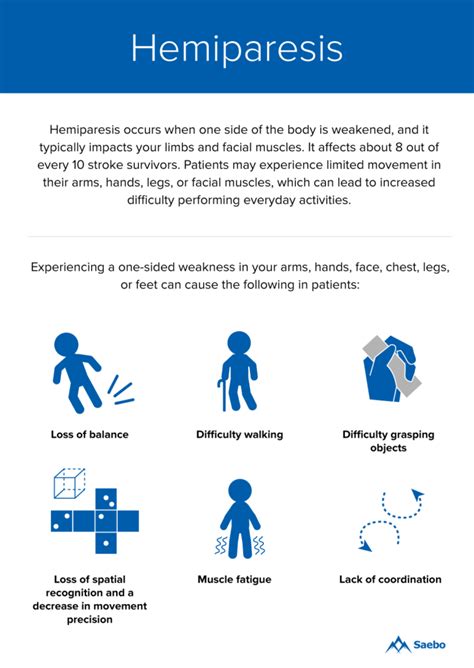
This trial tested the efficacy of individualized homeopathic medicines (IHMs) in comparison with identical-looking placebos in the treatment of post-stroke hemiparesis (PSH) in the mutual context of standard physiotherapy (SP).
A 3-months, open-label, randomized, placebo-controlled trial (n = 60) was conducted at the Organon of Medicine outpatient departments of the ‘National Institute of Homoeopathy’, West Bengal, India. Patients were randomized to receive IHMs plus SP (n = 30) or identical-looking placebos plus SP (n = 30). The primary outcome measure was Medical Research Council (MRC) muscle strength grading scale; secondary outcomes were Stroke Impact Scale (SIS) version 2.0, Modified Ashworth Scale (MAS), and stroke recovery 0-100 visual analog scale (VAS) scores; all measured at baseline and 3 months after the intervention. Group differences and effect sizes (Cohen’s d) were calculated on the intention-to-treat sample.
Although overall improvements were higher in the IHMs group than in the placebo group with small to medium effect sizes, the group differences were statistically non-significant (all P>0.05, unpaired t-tests). Improvement in SIS physical problems was significantly higher with IHM than with placebo (mean difference 2.0, 95% confidence interval 0.3 to 3.8, P = 0.025, unpaired t-test). Causticum, Lachesis mutus, and Nux vomica were the most frequently prescribed medicines. No harms, unintended effects, homeopathic aggravations, or any serious adverse events were reported from either group.
The authors concluded that there was a small, but non-significant direction of effect favoring homeopathy against placebos in treatment of post-stroke hemiparesis.
Considering the fact that homeopathy has become the holy cow of India which led to the phenomenon that almost no negative homeopathy trials are being reported by Indian researchers, this article is a happy surprise. Its authors clearly report that IHM had no effect on the primary outcome measure.
Bravo!
But who had the bizarre idea that it might?
I have heard many outlandish claims by homeopaths but the one about PSH was a new one to me.
Equally puzzling is, in my view, the design of this study: it was an “open-label, randomized, placebo-controlled trial”. The reason for having a placebo group is to blind the patients, i.e. not let them know whether they receive the verum or the placebo. In an open-label trial, however, the patient is given exactly that information. I totally fail to understand the logic of this. Can someone enlighten me, please?
Atopic dermatitis (AD) is a common condition that often frustrates all attempts of treatment. This is an ideal situation for homeopaths who claim to have the solution. Yet the evidence fails to support their optimism. The two systematic reviews on the subject are not encouraging:
- There was insufficient evidence to make recommendations on maternal allergen avoidance for disease prevention, oral antihistamines, Chinese herbs, dietary restriction in established atopic eczema, homeopathy, house dust mite reduction, massage therapy, hypnotherapy, evening primrose oil, emollients, topical coal tar and topical doxepin.
- The evidence from controlled clinical trials therefore fails to show that homeopathy is an efficacious treatment for eczema.
But now, a new study has emerged and it seems to contradict the previous conclusions. This study compared the efficacy of individualized homeopathic medicines (IHMs) against placebos in the treatment of AD.
In this double-blind, randomized, placebo-controlled trial of 6 months duration (n = 60), adult patients were randomized to receive either IHMs (n = 30) or identical-looking placebos (n = 30). All participants received concomitant conventional care, which included the application of olive oil and maintaining local hygiene. The primary outcome measure was disease severity using the Patient-Oriented Scoring of Atopic Dermatitis (PO-SCORAD) scale; secondary outcomes were the Atopic Dermatitis Burden Scale for Adults (ADBSA) and Dermatological Life Quality Index (DLQI) – all were measured at baseline and every month, up to 6 months. Group differences were calculated on the intention-to-treat sample.
After 6 months of intervention, inter-group differences became statistically significant on PO-SCORAD, the primary outcome (−18.1; 95% confidence interval, −24.0 to −12.2), favoring IHMs against placebos (F 1, 52 = 14.735; p <0.001; two-way repeated measures analysis of variance). Inter-group differences for the secondary outcomes favored homeopathy, but were overall statistically non-significant (ADBSA: F 1, 52 = 0.019; p = 0.891; DLQI: F 1, 52 = 0.692; p = 0.409).
The authors concluded that IHMs performed significantly better than placebos in reducing the severity of AD in adults, though the medicines had no overall significant impact on AD burden or DLQI.
I was unable to access the full paper, or more precisely unwilling to pay for it (in case someone has access, please post the link in the comments section below). From what can be gleaned from the abstract, this study is rigorous and clearly reported.
So, why is the outcome positive?
Pehaps one clue lies in the origin of the study. Here are the affiliations of the authors:
- 1Department of Materia Medica, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Howrah, West Bengal, India.
- 2Department of Pathology and Microbiology, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 3Department of Pathology and Microbiology, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Govt. of West Bengal, Howrah, West Bengal, India.
- 4Department of Repertory, JIMS Homoeopathic Medical College and Hospital, Shamshabad, Telangana, India.
- 5Department of Repertory, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Govt. of West Bengal, Howrah, West Bengal, India.
- 6Department of Health and Family Welfare, Homoeopathic Medical Officer, Rajganj State Homoeopathic Dispensary, Rajganj Government Medical College and Hospital, Uttar Dinajpur, West Bengal, India.
- 7Department of Pathology and Microbiology, National Tuberculosis Elimination Program Wing, Imambara Sadar Hospital, Hooghly, Govt. of West Bengal, India.
- 8Department of Organon of Medicine and Homoeopathic Philosophy, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 9Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 10Department of Health and Family Welfare, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Govt. of West Bengal, India.
- 11Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
I have previously noted that Indian studies of homeopathy (almost) never report a negative result. Why? Are the Indian homeopaths better than those elsewhere, or are they just less honest?
Acupuncture is a panacea, we are often told.
But is it true?
Of course not!
This study was aimed at evaluating the effect of acupuncture on myelosuppression and quality of life in women with breast cancer during treatment with anthracyclines (ANT).
Women with an indication for ANT chemotherapy were randomized into two groups:
- the acupuncture group (AG) was submitted to an acupuncture intervention, starting before the first chemotherapy infusion, and continuing throughout the treatment;
- the control group (CG) received no acupuncture.
A quality of life questionnaire (FACT-G) and peripheral blood levels of the participants were evaluated before and at the end of treatment.
A total of 26 women were randomized into 2 groups: AG (10) and CG (16). Of these, 26.9% had a dense dose indication according to the service’s protocol for the administration of granulocyte-stimulating factor (G-CSF) from the first cycle, not participating in the analysis. The need for secondary prophylaxis with G-CSF occurred in 72.7% in the control group versus 12% in the acupuncture group. Regarding quality of life (QoL), it was observed that the groups did not initially differ from each other. At the end of the treatment, there was a significant difference in the AG for the physical (GP) (p-value=0.011), social/family (GS) (p-value=0.018), and functional (GF) (p-value=0.010) domains, regarding the initial and final FACT-G showed a difference between the groups, where the GA average at the end rose from 80.68 to 90.12 (p-value = 0.004) and in the CG the average dropped from 81.95 to 70.59 (p-value=0.003).
The authors concluded that acupuncture was efficient in the secondary prophylaxis of myelosuppression during chemotherapy and the quality of life of women during treatment has increased.
My interpretation of these results is quite different from that of the authors.
Please let me explain.
The improvement of the quality of life can easily be explained via a placebo effect; acupuncture itself has not necessarily any part in it. But what about the effect on the bone marrow? Might it too be due to a placebo response, or the additional attention? Probably not.
Does that mean that this study proves a definite positive effect of acupuncture?
No!
Why not?
Because firstly the study was far too small for allowing such a far-reaching conclusion, and secondly one would need independent confirmation before accepting such a far-reaching conclusion.
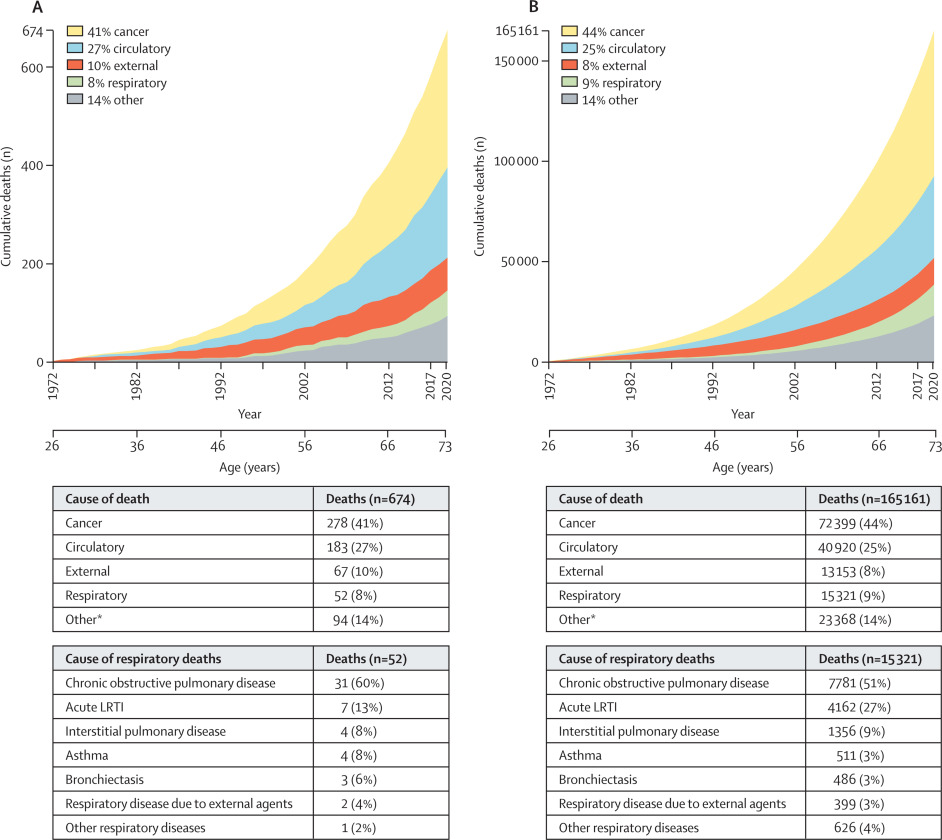
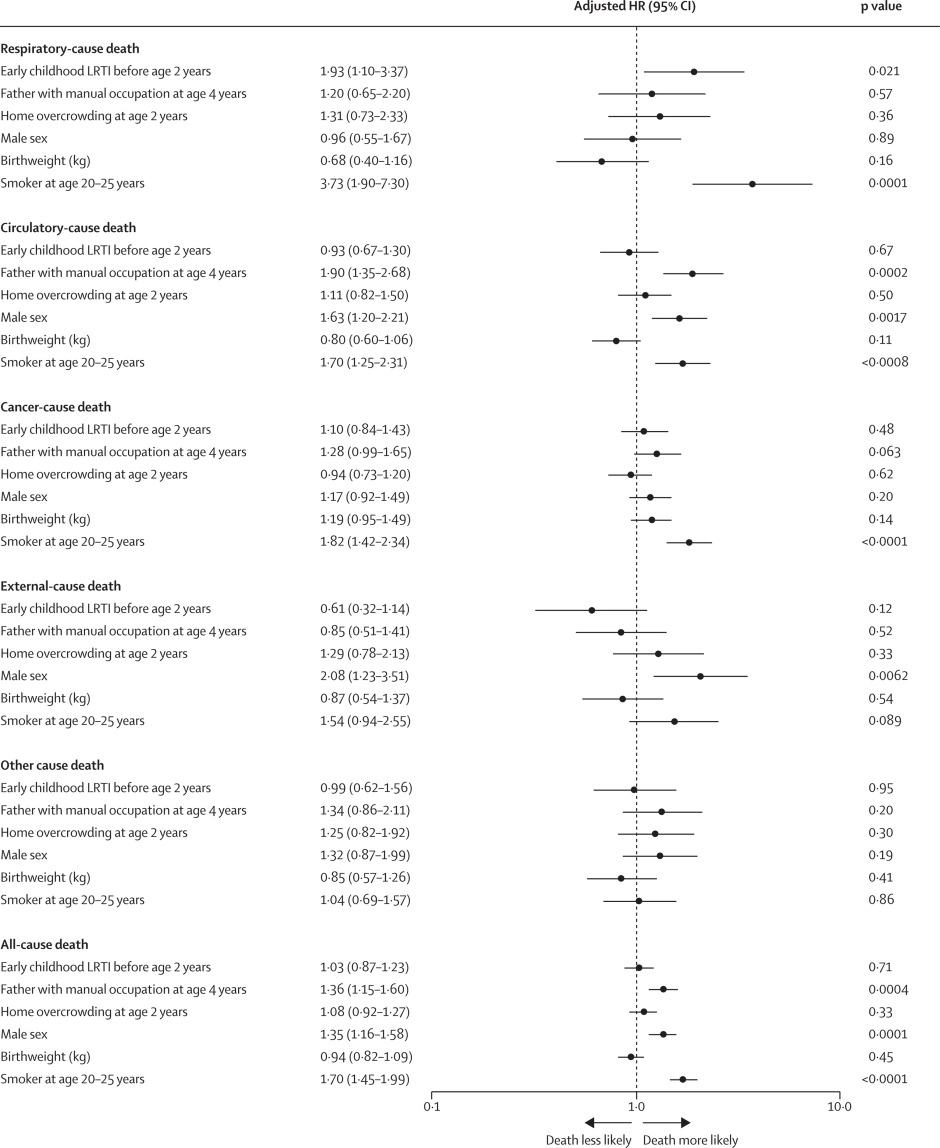
Lower respiratory tract infections (LRTIs) in early childhood are known to influence lung development and lifelong lung health, but their link to premature adult death from respiratory disease is unclear. This analysis aimed to estimate the association between early childhood LRTI and the risk and burden of premature adult mortality from respiratory disease.
This longitudinal observational cohort study used data collected prospectively by the Medical Research Council National Survey of Health and Development in a nationally representative cohort recruited at birth in March 1946, in England, Scotland, and Wales. It evaluated the association between LRTI during early childhood (age <2 years) and death from respiratory disease from age 26 through 73 years. Early childhood LRTI occurrence was reported by parents or guardians. Cause and date of death were obtained from the National Health Service Central Register. Hazard ratios (HRs) and population attributable risk associated with early childhood LRTI were estimated using competing risks Cox proportional hazards models, adjusted for childhood socioeconomic position, childhood home overcrowding, birthweight, sex, and smoking at age 20–25 years. The researchers compared mortality within the cohort studied with national mortality patterns and estimated corresponding excess deaths occurring nationally during the study period.
5362 participants were enrolled in March, 1946, and 4032 (75%) continued participating in the study at age 20–25 years. 443 participants with incomplete data on early childhood (368 [9%] of 4032), smoking (57 [1%]), or mortality (18 [<1%]) were excluded. 3589 participants aged 26 years (1840 [51%] male and 1749 [49%] female) were included in the survival analyses from 1972 onwards. The maximum follow-up time was 47·9 years. Among 3589 participants, 913 (25%) who had an LRTI during early childhood were at greater risk of dying from respiratory disease by age 73 years than those with no LRTI during early childhood (HR 1·93, 95% CI 1·10–3·37; p=0·021), after adjustment for childhood socioeconomic position, childhood home overcrowding, birthweight, sex, and adult smoking. This finding corresponded to a population attributable risk of 20·4% (95% CI 3·8–29·8) and 179 188 (95% CI 33 806–261 519) excess deaths across England and Wales between 1972 and 2019.
The authors concluded that, in this perspective, life-spanning, nationally representative cohort study, LRTI during early childhood was associated with almost a two times increased risk of premature adult death from respiratory disease, and accounted for one-fifth of these deaths.
What has that got to do with so-called alternative medicine?
Nothing!
Yet, I feel that this study is so remarkable that I need to report on it nonetheless.
What do the findings indicate?
I am not sure. Perhaps they confirm that our genetic makeup is hugely important in determining our health. Thus even the earliest signs of weakness can provide an indication of what might happen in later life.
Whatever the meaning, I find this study fascinating and hope you agree.
The ‘keto diet’ is a currently popular high-fat, low-carbohydrate diet; it limits the intake of glucose which results in the production of ketones by the liver and their uptake as an alternative energy source by the brain. It is said to be an effective treatment for intractable epilepsy. In addition, it is being promoted as a so-called alternative medicine (SCAM) for a wide range of conditions, including:
- weight loss,
- cognitive and memory enhancement,
- type II diabetes,
- cancer,
- neurological and psychiatric disorders.
Now, it has been reported that the ‘keto diet’ may be linked to higher levels of cholesterol and double the risk of cardiovascular events. In the study, researchers defined a low-carb, high-fat (LCHF) diet as 45% of total daily calories coming from fat and 25% coming from carbohydrates. The study, which has so far not been peer-reviewed, was presented Sunday at the American College of Cardiology’s Annual Scientific Session Together With the World Congress of Cardiology.
“Our study rationale came from the fact that we would see patients in our cardiovascular prevention clinic with severe hypercholesterolemia following this diet,” said Dr. Iulia Iatan from the Healthy Heart Program Prevention Clinic, St. Paul’s Hospital, and University of British Columbia’s Centre for Heart Lung Innovation in Vancouver, Canada, during a presentation at the session. “This led us to wonder about the relationship between these low-carb, high-fat diets, lipid levels, and cardiovascular disease. And so, despite this, there’s limited data on this relationship.”
The researchers compared the diets of 305 people eating an LCHF diet with about 1,200 people eating a standard diet, using health information from the United Kingdom database UK Biobank, which followed people for at least a decade. They found that people on the LCHF diet had higher levels of low-density lipoprotein and apolipoprotein B. Apolipoprotein B is a protein that coats LDL cholesterol proteins and can predict heart disease better than elevated levels of LDL cholesterol can. The researchers also noticed that the LCHF diet participants’ total fat intake was higher in saturated fat and had double the consumption of animal sources (33%) compared to those in the control group (16%). “After an average of 11.8 years of follow-up – and after adjustment for other risk factors for heart disease, such as diabetes, high blood pressure, obesity, and smoking – people on an LCHF diet had more than two times higher risk of having several major cardiovascular events, such as blockages in the arteries that needed to be opened with stenting procedures, heart attack, stroke, and peripheral arterial disease.” Their press release also cautioned that their study “can only show an association between the diet and an increased risk for major cardiac events, not a causal relationship,” because it was an observational study, but their findings are worth further investigation, “especially when approximately 1 in 5 Americans report being on a low-carb, keto-like or full keto diet.”
I have to say that I find these findings not in the slightest bit surprising and would fully expect the relationship to be causal. The current craze for this diet is concerning and we need to warn consumers that they might be doing themselves considerable harm.
Other authors have recently pointed out that, within the first 6-12 months of initiating the keto diet, transient decreases in blood pressure, triglycerides, and glycosylated hemoglobin, as well as increases in HDL and weight loss may be observed. However, the aforementioned effects are generally not seen after 12 months of therapy. Despite the diet’s favorable effect on HDL-C, the concomitant increases in LDL-C and very-low-density lipoproteins (VLDL) may lead to increased cardiovascular risks. And another team of researchers has warned that “given often-temporary improvements, unfavorable effects on dietary intake, and inadequate data demonstrating long-term safety, for most individuals, the risks of ketogenic diets may outweigh the benefits.”
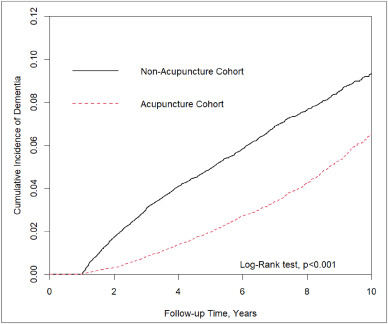
In this retrospective matched-cohort study, Chinese researchers investigated the association of acupuncture treatment for insomnia with the risk of dementia. They collected data from the National Health Insurance Research Database (NHIRD) of Taiwan to analyze the incidence of dementia in patients with insomnia who received acupuncture treatment.
The study included 152,585 patients, selected from the NHIRD, who were newly diagnosed with insomnia between 2000 and 2010. The follow-up period ranged from the index date to the date of dementia diagnosis, date of withdrawal from the insurance program, or December 31, 2013. A 1:1 propensity score method was used to match an equal number of patients (N = 18,782) in the acupuncture and non-acupuncture cohorts. The researchers employed Cox proportional hazards models to evaluate the risk of dementia. The cumulative incidence of dementia in both cohorts was estimated using the Kaplan–Meier method, and the difference between them was assessed through a log-rank test.
Patients with insomnia who received acupuncture treatment were observed to have a lower risk of dementia (adjusted hazard ratio = 0.54, 95% confidence interval = 0.50–0.60) than those who did not undergo acupuncture treatment. The cumulative incidence of dementia was significantly lower in the acupuncture cohort than in the non-acupuncture cohort (log-rank test, p < 0.001).
The researchers concluded that acupuncture treatment significantly reduced or slowed the development of dementia in patients with insomnia.
They could be correct, of course. But, then again, they might not be. Nobody can tell!
As many who are reading these lines know: CORRELATION IS NOT CAUSATION.
But if acupuncture was not the cause for the observed differences, what could it be? After all, the authors used clever statistics to make sure the two groups were comparable!
The problem here is, of course, that they can only make the groups comparable for variables that were measured. These were about 20 parameters mostly related to medication intake and concomitant diseases. This leaves a few hundred potentially relevant variables that were not quantified and could thus not be accounted for.
My bet would be lifestyle: it is conceivable that the acupuncture group had acupuncture because they were generally more health-conscious. Living a relatively healthy life might reduce the dementia risk entirely unrelated to acupuncture. According to Occam’s razor, this explanation is miles more likely that the one about acupuncture.
So, what this study really demonstrates or implies is, I think, this:
- The propensity score method can never be perfect in generating completely comparable groups.
- The JTCM publishes rubbish.
- Correlation is not causation.
- To establish causation in clinical medicine, RCTs are usually the best option.
- Occam’s razor can be useful when interpreting research findings.