study design
This trial investigated the effect of osteopathic visceral manipulation (OVM) on disability and pain intensity in individuals with functional constipation and chronic nonspecific low back pain. It was designed as a randomized controlled trial with a blinded assessor. Seventy-six volunteers with functional constipation and chronic nonspecific low back pain were randomized to two groups: OVM and sham OVM. The primary clinical outcome was pain intensity measured using a numeric rating scale (NRS) and disability measured using the Oswestry Disability Index (ODI). The secondary outcomes were electromyographic signals measured during the flexion-extension cycle, the finger-to-floor distance during complete flexion of the trunk, and the Fear-Avoidance Beliefs Questionnaire (FABQ). All outcomes were determined after six weeks of treatment as well as three months after randomization.
The OVM group reported a reduction in pain intensity after six weeks of treatment and at the three-month evaluation (p < .0002) and the sham group reported a reduction in pain intensity after three-month evaluation (p < .007). For the ODI was also found in the OVM group six weeks after the end of treatment (treatment effect = -6.59, 95% CI: -12.01 to -1.17, p = .01) and at the three-month evaluation (treatment effect = -6.02, 95% CI: -11.55 to -0.49, p = .03). Significant differences were also found for paravertebral muscle activity during the dynamic phases (flexion and extension) six-week evaluations.
The authors concluded that the OVM group demonstrated a reduction in pain intensity and improvement in disability after six-weeks and three-month follow-up while the sham group reduction in pain three-month follow-up.
I have no access to the full paper (if someone can send me the paper, I would update my post accordingly), but from reading the abstract, it seems the reported findings are based on within-group changes. The whole point of having a control group is to compare verum and control. The other point of importance is that it would have been crucial to verify whether patients were able to tell the verum from the sham intervention. If patients were able to tell, they would no longer be blinded and the placebo effect would have not been accounted for. A third point of relevance might be that the study seems tiny and far too small for drawing general conclusions about the value of OVM.
_________________________
I have now seen the protocol of the paper – thanks for making it available – and might add the following points to the discussion:
- The sham treatment consisted of “light touches over the different parts of the abdomen, without any deep mobilization or movement. The osteopath applied her hands over the same points with the
same duration as in OVM to give the patient the perception of being treated.” It is likely that patients in the control group could have guessed that they were sham-treated. - The stats issue cannot be resolved on the basis of just the protocol.
- “To assess patients’ blinding to treatment allocation, patients are asked post treatment (six weeks after
the start of treatment) to report which study treatment they think that they received (OVM/SOVM). The effect of their reports on outcome will be examined in explorative analysis.” As I have no
access to the results, I still do not know whether blinding was successful.
Psoriasis is a chronic inflammatory skin disorder, affecting the trunk and extensor surfaces of limbs and scalp predominantly. Its prevalence ranges between 0.1 and 11.4% and in India between 0.4 and 2.8%. Psoriasis remains a frequently encountered condition in homeopathy practice, but there is a dearth of evidence supporting its use. 
This 6-month, double-blind, randomized trial was conducted on 51 patients suffering from psoriasis at the National Institute of Homoeopathy, India. Patients were randomized to receive either individualized homeopathic medicines (IHMs; n = 25) in LM potencies or identical-looking placebos (n=26). Psoriasis area and severity index (PASI; primary), psoriasis disability index (PDI), and dermatological life quality index (DLQI; secondary) were measured at baseline, and every 2 months, up to 6 months. The intention-to-treat sample was analyzed using a two-way repeated measure analysis of variance.
Although intra-group changes were significant in both groups, improvements were significantly greater in the IHMs group than in the placebo group regarding the PASI scores after 6 months (F1, 49 = 10.448, P = 0.002). DLQI daily activity subscale scores also yielded similar significant results favoring IHMs against placebos after 6 months (F1, 49 = 5.480, P = 0.023). Improvement in PDI total (F1, 49 = 0.063, P = 0.803), DLQI total (F1, 49 = 1.371, P = 0.247), and all remaining subscales were higher in the IHMs group than placebos after 6 months, but non-significant statistically. Calcarea carbonica, Mercurius solubilis, Arsenicum album, and Petroleum were the most frequently prescribed medicines.
The authors concluded that IHMs exhibited better results than placebos in the treatment of psoriasis. Further research is warranted.
I am unable to access the full text of this paper [in case someone can, please send it to me for further scrutiny]. Judging from just the abstract, I see the following problems with this trial:
- Psoriasis is a genetically determined condition, and I find it hard to believe that homeopathy can change its natural history.
- The symptoms of psoriasis fluctuate and can be influenced by a range of factors, including stress.
- We learn nothing about any concomitant interventions which are always necessary, e.g. creams, or compliance with them.
- It is conceivable that patients in the verum group received inadvertent reassurance which, in turn, reduced stress and improved compliance with external treatments.
- It is unclear whether patients were successfully blinded or whether inadvertent de-blinding occurred.
In any case, I would caution that this trial needs independent replications before we can take its findings seriously.
__________________________
Thanks to several readers, I now have the full text and can add the following points:
- The authors report adverse events as follows: ” No adverse events were reported during the treatment period from either group that could be attributed causally to either IHMs or placebos. Some minor events unrelated to study medications, like common cold and injury occurring in both groups were treated with acute homeopathic medicines irrespective of allocated codes, and once those acute phases were over, the patients were returned to originally allocated groups again.” This is odd because homeopaths would expect aggravations in a high percentage of cases.
- I am not sure that I understand the blinding procedure; it is described as follows: “Double-blinding method was adopted by masking the trial participants, investigators, outcome assessors, pharmacists, and data entry operators throughout the trial. Identical-looking vials were coded as either “1” or “2” and contained either medicines or placebos. The codes remained the same for all the randomized participants. Codes were assigned randomly and confidentially by another independent third party. Both medicines and placebos were repacked in identical glass bottles and labeled with code, name of medicine, and potency, and were dispensed according to the random number list. The vials were destined for each patient by the random number chart. The participants got the medicines dispensed personally at the hospital pharmacy. Codes were broken at the end of the trial after the dataset was frozen.”
- The affiliations of the authors are interesting:1 Dept. of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector 3, Salt Lake, Kolkata 700106, West Bengal, India; affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India
2 Dept. of Repertory, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE,
Sector 3, Salt Lake, Kolkata 700106, West Bengal, India; affiliated to The West Bengal University of
Health Sciences, Govt. of West Bengal, India 3 Dept. of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, 265, 266, Acharya Prafulla Chandra Road, Kolkata 700009, West Bengal; affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India
4 East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre,
Village and Post Office: Dakshin Gouripur, Police Station Bishnupur, South 24 Parganas 743503, West
Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India 5 Dept. of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, 12, Gobinda Khatick Road, Tangra, Kolkata 700046, West Bengal; affiliated to The West Bengal University
of Health Sciences, Govt. of West Bengal, India.
I think it is safe to repeat that independent replications would be essential.
This study investigated the potential benefits of auricular point acupressure on cerebrovascular function and stroke prevention among adults with a high risk of stroke.
A randomized controlled study was performed with 105 adults at high risk for stroke between March and July 2021. Participants were randomly allocated to receive either
- auricular point acupressure with basic lifestyle interventions (n = 53) or
- basic lifestyle interventions alone (n = 52) for 2 weeks.
The primary outcome was the kinematic and dynamic indices of cerebrovascular function, as well as the CVHP score at week 2, measured by the Doppler ultrasonography and pressure transducer on carotids.
Of the 105 patients, 86 finished the study. At week 2, the auricular point acupressure therapy with lifestyle intervention group had higher kinematic indices, cerebrovascular hemodynamic parameters score, and lower dynamic indices than the lifestyle intervention group.
The authors concluded that ccerebrovascular function and cerebrovascular hemodynamic parameters score were greater improved among the participants undergoing auricular point acupressure combined with lifestyle interventions than lifestyle interventions alone. Hence, the auricular point acupressure can assist the stroke prevention.
Acupuncture is a doubtful therapy.
Acupressure is even more questionable.
Ear acupressure is outright implausible.
The authors discuss that the physiological mechanism underlying the effect of APA therapy on cerebrovascular hemodynamic function is not fully understood at present. There may be two possible explanations.
- First, a previous study has demonstrated that auricular acupuncture can directly increase mean blood flow velocity in the middle cerebral artery.
- Second, cerebrovascular hemodynamic function is indirectly influenced by the effect of APA therapy on blood pressure.
I think there is a much simpler explanation: the observed effects are directly or indirectly due to placebo. As regular listeners of this blog know only too well by now, the A+B versus B study design cannot account for placebo effects. Sadly, the authors of this study hardly discuss this explanation – that’s why they had to publish their findings in just about the worst SCAM journal of them all: EBCAM.
Previous research revealed that cognitive abilities are negatively related to right-wing and prejudiced attitudes. No study has, however, investigated if emotional abilities also show such a relationship, although this can be expected based on both classic and recent literature. The aim of the present study was 2-fold:
(a) to investigate the relationship between emotional abilities and right-wing and prejudiced attitudes, and
(b) to pit the effects of emotional and cognitive abilities on these attitudes against each other.
Results from 2 adult samples (n = 409 and 574) in which abilities scores were collected in individual testing sessions, revealed that emotional abilities are significantly and negatively related to social-cultural and economic-hierarchical right-wing attitudes, as well as to blatant ethnic prejudice. These relationships were as strong as those found for cognitive abilities. For economic-hierarchical right-wing attitudes, emotional abilities were even the only significant correlate.
The authors concluded that the study of emotional abilities has the potential to significantly advance our understanding of right-wing and prejudiced attitudes.
__________
The researchers found that individuals with weaker emotional abilities — particularly emotional understanding and management — tended to score higher on a measure of right-wing authoritarianism and social dominance orientation. Right-wing authoritarianism is a personality trait that describes the tendency to submit to political authority and be hostile towards other groups, while social dominance orientation is a measure of a person’s preference for inequality among social groups.
The results of this study were univocal. People who endorse authority and strong leaders and who do not mind inequality — the two basic dimensions underlying right-wing political ideology — show lower levels of emotional abilities,” said Van Hiel, the lead author of the study. “Those with lower emotional and cognitive abilities were also more likely to agree with blatantly prejudiced statements such as “The White race is superior to all other races.”
Of course, the study only collected correlational data, preventing inferences of causality from being made. “Caution should be exercised in the interpretation of such results,” Van Hiel said. “One cannot discredit any ideology on the basis of such results as those presently obtained. Only in a distant future, we will be able to look back upon our times, and then we can maybe judge which ideologies were the best. Cognitively and emotionally smart people can make wrong decisions as well. The results have been obtained in one particular context. Would similar results be obtained in other contexts besides in a Western country with a long-standing stable democracy? Whether these tendencies are universal, or limited to particular contexts, is very intriguing.”
A team of French researchers assessed whether a conflict of interest (COI) might be associated with the direction of the results of meta-analyses of homoeopathy trials. Their analysis (published as a ‘letter to the editor) is complex, therefore, I present here only their main finding.
The team conducted a literature search until July 2022 on PubMed and Embase to identify meta-analyses of randomized clinical trials assessing the efficacy of homoeopathy. They then assessed the existence of potential COI, defined by the presence of at least one of the following criteria:
- affiliation of one or more authors to an academic homoeopathy research or care facility, or to the homoeopathy industry;
- research sponsored or funded by the homoeopathy industry;
- COI declared by the authors.
The researchers also evaluated and classified any spin in meta-analyses conclusions into three categories (misleading reporting, misleading interpretation and inappropriate extrapolation). Two reviewers assessed the quality of meta-analyses and the risk of bias based. Publication bias was evaluated by the funnel plot method. For all the studies included in these meta-analyses, the researchers checked whether they reported a statistically significant result in favour of homoeopathy. Further details about the methods are provided on OSF (https://osf.io/nqw7r/) and in the preregistered protocol (CRD42020206242).
Twenty meta-analyses were included in the analysis (list of references available at https://osf.io/nqw7r/).
- Among the 13 meta-analyses with COI, a significantly positive effect of homoeopathy emerged (OR=0.60 (95% CI 0.50 to 0.70)).
- There was no such effect for meta-analyses without COI (OR=0.96 (95% CI 0.75 to 1.23)).
The authors concluded that in the presence of COI, meta-analyses of homoeopathy trials are more likely
to have favourable results. This is consistent with recent research suggesting that systematic reviews with financial COI are associated with more positive outcomes.
Meta-analyses are systematic reviews (critical assessments of the totality of the available evidence) where the data from the included studies are pooled. For a range of reasons, this may not always be possible. Therefore the number of meta-analyses (20) is substantially lower than that of the existing systematic reviews (>50).
Both systematic reviews and meta-analyses are theoretically the most reliable evidence regarding the value of any intervention. I said ‘theoretically’ because, like any human endeavour, they need to be done in an unbiased fashion to produce reliable results. People with a conflict of interest by definition struggle to be free of bias. As we have seen many times, this would include homoeopaths.
This new analysis confirms what many of us have feared. If proponents of homeopathy with an overt conflict of interest conduct a meta-analysis of studies of homeopathy, the results tend to be more positive than when independent researchers do it. The question that emerges from this is the following:
Are the findings of those researchers who have an interest in producing a positive result closer to the truth than the findings of researchers who have no such conflict?
I let you decide.
‘Spagyric’ is a so-called alternative medicine (SCAM) based on the alchemy of Paracelsus (1493-1541). Paracelsus borrowed the term from “separate” (spao) and “combine” (ageiro) to indicate that spagyric preparations are based on the “separation”, “extraction” and “recombination” of the active ingredients of a substance. Plant, mineral as well as animal source materials are used.
The production of spagyric remedies is based on a complex process of maceration and fermentation of a plant extract in alcohol. It takes place in dark, thick-walled glass flasks that are hermetically sealed and kept at a controlled temperature of 37 °C for 28 days. The tincture thus obtained is then decanted and the drug residue is removed from the solution, completely dried, and burned to ash to recover the inorganic components of the plant material. The ash is subsequently dissolved in the alcoholic solution of maceration, and the finished spagyric preparation is left for 12 days before use.
Spagyric is not the most popular of all SCAMs but it certainly does have a significant following. One enthusiast claims that “spagyric essences work on a vibrational level in their action upon the emotional/mind and physical spheres and can be employed in numerous situations. Most people seek help to relieve physical symptoms. Even so, it is often necessary to address the emotional and psychological aspects which may predispose the illness or imbalance. In an era where many people are experiencing life-changing events, the ability to transition smoothly is essential for well-being and vitality. Guidance and help are required to maintain homeostasis. These medicines can help the patient to understand the root cause of their illness and learn to regain control of their lives. Some medicine systems appear to be less effective than in previous times. It has been suggested that the energetic frequency of both the earth and human organism are changing. Therefore these systems may no longer be a vibrational match for the changing frequencies. Spagyric Medicine is designed to ‘tune in with’ these current frequencies. Research suggests that the Spagyric essences may instigate improved health by energetically influencing DNA.”
After reading such weird statements, I ask myself, is there any evidence that spagyric remedies work? In my search for robust studies, I was unsuccessful. There does not seem to be a single controlled study on the subject. However, there are fragmentary reports of a study initiated and conducted by a now largely unknown healer named Karl Hann von Weyhern.
Von Weyhern (1882 – 1954) had taken a few semesters of pharmacy and medicine in Freiburg but remained without a degree. In 1930, he became a member of the NSDAP (Hitler’s Nazi party) and in 1940 he joined the SS. Around 1935, he settled in Munich as a non-medical practitioner (Heilpraktiker), and Heinrich Himmler who has a soft spot for SCAM enlisted as one of his patients. By then von Weyhern had by then made a steep career in the Nazi hierarchy, and he managed to convince Himmler that his spagyric remedies could cure tuberculosis, which was still rampant at the time. They decided to carry out experiments in this regard in the Dachau concentration camp.
Thus, von Weyhern was allowed to test spagyric remedies on forcibly recruited concentration camp prisoners. These experiments lasted for about one year and included around 150 patients who, according to von Weyhern’s iridology diagnosis, suffered from tuberculosis. Half of them were treated with spagyric remedies and the others with conventional treatments. At the end of the experiment, 27 persons were reportedly released into everyday concentration camp life as ‘fit for work’. How many of the 150 prisoners lost their lives due to these experiments is not known. Von Weyhern never filed a final report. It is to be feared that the death toll was considerable. [1]
After the war, von Weyhern denied belonging to the SS, claimed that he had ‘sacrificed himself’ for his patients in the concentration camp, merely had to pay a fine, and was ‘denazified’ in 1948. Subsequently, he resumed his work as a ‘Heilpraktiker’ in Olching, a village near Dachau. [1]
Of course, these infamous experiments cannot be blamed on spagyric medicine. Yet, I feel they are nevertheless important, not least because they seem to reveal the only thing remotely resembling something like evidence.
[1] Die Ärzte der Nazi-Führer: Karrieren und Netzwerke : Mathias Schmidt (Hg.), Dominik Groß (Hg.), Jens Westemeier (Hg.): Amazon.de: BooksThere are debates in acupuncture-related systematic reviews and meta-analyses on whether searching Chinese databases to get more Chinese-language studies may increase the risk of bias and overestimate the effect size, and whether the treatment effects of acupuncture differ between Chinese and non-Chinese populations.
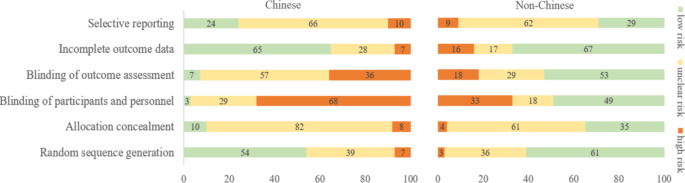
For this meta-epidemiological study, a team of investigators searched the Cochrane Library from its inception until December 2021, and identified systematic reviews and meta-analyses with acupuncture as one of the interventions. Paired reviewers independently screened the reviews and extracted the information. They repeated the meta-analysis of the selected outcomes to separately pool the results of Chinese- and non-Chinese-language acupuncture studies and presented the pooled estimates as odds ratios (OR) with 95% confidence interval (CI). They calculated the Ratio of ORs (ROR) by dividing the OR of the Chinese-language trials by the OR of the non-Chinese-language trials, and the ROR by dividing the OR of trials addressing Chinese population by the OR of trials addressing non-Chinese population. The researchers thus explored whether the impact of a high risk of bias on the effect size differed between studies published in Chinese- and in non-Chinese-language, and whether the treatment effects of acupuncture differed between Chinese and non-Chinese populations.
The researchers identified 84 Cochrane acupuncture reviews involving 33 Cochrane groups, of which 31 reviews (37%) searched Chinese databases. Searching versus not searching Chinese databases significantly increased the contribution of Chinese-language literature both to the total number of included trials (54% vs. 15%) and the sample size (40% vs. 15%). When compared with non-Chinese-language trials, Chinese-language trials were associated with a larger effect size (pooled ROR 0.51, 95% CI 0.29 to 0.91). The researchers also observed a higher risk of bias in Chinese-language trials in blinding of participants and personnel (97% vs. 51%) and blinding of outcome assessment (93% vs. 47%). The higher risk of bias was associated with a larger effect estimate in both Chinese language (allocation concealment: high/unclear risk vs. low risk, ROR 0.43, 95% CI 0.21 to 0.87) and non-Chinese-language studies (blinding of participants and personnel: high/unclear risk vs. low risk, ROR 0.41, 95% CI 0.23 to 0.74). However, the team found no evidence that the higher risk of bias would increase the effect size of acupuncture in Chinese-language studies more often than in non-Chinese-language studies (the confidence intervals of all ROR in the high-risk group included 1, Table 3). The researchers further found acupuncture appeared to be more effective in Chinese than in non-Chinese populations.
The authors concluded that the findings of this study suggest the higher risk of bias may lead to an overestimation of the treatment effects of acupuncture but would not increase the treatment effects in Chinese-language studies more often than in other language studies. The difference in treatment effects of acupuncture was probably associated with differences in population characteristics.
The authors discuss that, although searching Chinese databases can substantially increase the number of eligible studies and sample size in acupuncture reviews, the potentially higher risk of bias is an argument that needs to be considered in the inclusion of Chinese-language studies. Patients, investigators, and guideline panels should be cautious when adopting evidence from acupuncture reviews where studies with a high risk of bias contributed with a high weight to the meta-analysis.
The authors observed larger treatment effects of acupuncture in Chinese-language studies than in studies published in other languages. Although the treatment effects of acupuncture tended to be greater in studies with a high risk of bias, this potential overestimation did not differ between studies published in Chinese and in other languages. In other words, the larger treatment effects in Chinese-language studies cannot be explained by a high risk of bias. Furthermore, our study found acupuncture to be more effective in Chinese populations than in other populations, which could at least partly explain the larger treatment effects observed in Chinese-language studies.
I feel that this analysis obfuscates more than it clarifies. As we have discussed often here, acupuncture studies by Chinese researchers (regardless of what language they are published in) hardly ever report negative results, and their findings are often fabricated. It, therefore, is not surprising that their effect sizes are larger than those of other trials.
The only sensible conclusion from this messy and regrettable situation, in my view, is to be very cautious and exclude them from systematic reviews.
Infant colic is a sensitive subject for chiropractors in the UK. In case you forgot, here is why. Consequently, the subject has featured regularly on this blog – and now there is new evidence:
A systematic review and meta-analysis were conducted on infantile colic studies that used SO-CALLED alternative medicine (SCAM) techniques as interventions. The outcome measures were hours spent crying and/or sleeping. The authors used the PubMed, Physiotherapy Evidence Database, Cochrane Library, Embase, Web of Science, Scopus, Osteopathic Medicine Digital Database, and Google Scholar databases from inception to 11 November 2022.
The methodological quality of the randomized control trials ranged from fair to high. The authors focused on five studies with 422 babies using the following interventions: cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization. These treatments failed to decrease the crying time (mean difference -1.08, 95% CI -2.17 to 0.01, I2 = 92%) and to increase the sleeping time (mean difference 1.11, 95% CI -0.20 to 2.41; I2: 91%), compared with no intervention. The quality of the evidence was rated as very low for both outcome measures.The authors concluded that osteopathy and chiropractic treatment failed to reduce the crying time and increase sleeping time in babies with infantile colic, compared to no additional intervention.The 5 included studies were the following:
- Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: A pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther. 2012;35(8):600–7.
- Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. A randomized controlled trial. Complement Ther Med. 2022;71(February 2021).
- Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child. 2001;84(2):138–41.
- Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Ther. 2021;29(1):1–11.
- Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract. 2006;12(2):83–90.
This means that, in recent years, several new studies have emerged. I find this surprising: there is no plausible mechanism of action and the previous reviews were negative.
Why flog a dead horse?
But – come to think of it – this is a question one might ask about most of the research into cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization.
I found this acupuncture study from the Department of Oral and Maxillofacial Sciences, “Sapienza” University of Rome, Rome, Italy. As this seems to be a respectable institution, I had a look. What I found was remarkable! Let me show you the abstract in its full beauty:
Background: Pain related to Temporomandibular Disorders (TMD) is severe, negatively affecting patients’ quality of life, and often resistant to conventional treatments. Abdominal Acupuncture (AA) is known to be particularly effective for pain, especially chronic and musculoskeletal pain, but it is still poorly studied and never investigated in TMD patients. Objectives: To analyze the efficacy of AA for the treatment of patients with subacute and chronic pain related to TMD and non-responding to previous conventional therapies (occlusal splint, medications, physical therapy).
Methods: Twenty-eight patients, 24 F and four M (mean age 49.36 years), were recruited from January 2019-February 2021. All patients underwent AA treatment: two sessions per week for four weeks, for a total of eight sessions. At the beginning of therapy (T0) and at the end of the cycle (T1) the following data were evaluated: maximum mouth opening (MMO); cranio-facial pain related to TMD (verbal numeric scale, VNS); pain interference with normal activities and quality of life of patients (Brief Pain Inventory, BPI); oral functioning (Oral Behavior Checklist, OBC); impression of treatment effectiveness (Patients’ Global Impression of Improvement, PGI-I Scale). Statistical comparison of data before and after the AA treatment was performed by Wilcoxon’s signed-rank test (significance level p < 0.05).
Results: The MMO values were significantly improved after one cycle of AA (p = 0.0002). In addition, TMD-related pain had a statistically significant decline following AA treatment (all p < 0.001). Patients’ general activity and quality of life (BPI) were described as improved following a course of AA, with statistically significant values for all aspects considered (all p < 0.05).
Conclusion: Abdominal acupuncture resulted in effective treatment of subacute/chronic resistant pain related to TMD, capable of improving mandibular function and facial pain, and reduced the interference of pain affecting patients’ quality of life.
_____________________
Shocked?
Me too!
This study did not include a control group. Such uncontrolled studies are not necessarily useless. In areas where there is no prior evidence, they can be a reasonable starting point for further research. In the case of TMD/acupuncture, however, this does not imply. Here we already have about a dozen controlled trials. This means an uncontrolled study cannot possibly contribute to our knowledge. This means that the present study is useless. And that, in turn, means it is unethical.
But even if we ignore all this, the study is very misleading. It concludes that acupuncture improved TMD. This, however, can be doubted!
- What about placebo?
- What about regression toward the mean?
- What about the natural history of the condition?
Bad science is regrettable and dangerous, as it
- wastes resources,
- misleads vulnerable patients,
- violates ethics,
- and undermines trust in science.
I fear that the Italian group has just provided us with a prime example of these points.
Massages are experienced as agreeable by most patients. But that does not necessarily mean that it improves our quality of life. This study tests whether it does.
This study compared three massage dosing strategies among inpatients receiving palliative care consultation. It was designed as a three-armed randomized trial examining three different doses of therapist-applied massage to test change in overall quality of life (QoL) and symptoms among hospitalized adult patients receiving palliative care consultation for any indication:
- Arm I: 10-min massage daily × 3 days;
- Arm II: 20-min massage daily × 3 days;
- Arm III: single 20-min massage.
The primary outcome measure was the single-item McGill QoL question. Secondary outcomes measured pain/symptoms, rating of peacefulness, and satisfaction with the intervention. Data were collected at baseline, pre-and post-treatment, and one-day post-last treatment (follow-up). Repeated measure analysis of variance and paired t-test were used to determine significant differences.
A total of 387 patients participated (55.7 (±15.49) years old, mostly women (61.2%) and African-American (65.6%)). All three arms demonstrated within-group improvement at follow-up for McGill QoL (all P < 0.05). No significant between-group differences were found. Finally, repeated measure analyses demonstrated time to predict immediate improvement in distress (P ≤ 0.003) and pain (P ≤ 0.02) for all study arms; however, only improvement in distress was sustained at follow-up measurement in arms with three consecutive daily massages of 10 or 20 minutes.
The authors concluded that massage therapy in complex patients with advanced illness was beneficial beyond dosage. Findings support session length (10 or 20 minutes) was predictive of short-term improvements while treatment frequency (once or three consecutive days) predicted sustained improvement at follow-up.
I like this study because it teaches us an important lesson:
IF ONE DESIGNS A SILLY STUDY, ONE IS LIKELY TO ARRIVE AT A SILLY CONCLUSION.
This study does not have a proper control group. Therefore, we cannot know whether the observed outcomes were due to the different interventions or to non-specific effects such as expectation, the passing of time, etc.
The devil’s advocate conclusion of the findings is thus dramatically different from that of the authors: the results of this trial are consistent with the notion that massage has no effect on QoL, no matter how it is dosed.