study design
The aim of this systematic review was to update the current level of evidence for spinal manipulation in influencing various biochemical markers in healthy and/or symptomatic population.
Various databases were searched (inception till May 2023) and fifteen trials (737 participants) that met the inclusion criteria were included in the review. Two authors independently screened, extracted and assessed the risk of bias in included studies. Outcome measure data were synthesized using standard mean differences and meta-analysis for the primary outcome (biochemical markers). The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) was used for assessing the quality of the body of evidence for each outcome of interest.
There was low-quality evidence that spinal manipulation influenced various biochemical markers (not pooled). There was low-quality evidence of significant difference that spinal manipulation is better (SMD -0.42, 95% CI – 0.74 to -0.1) than control in eliciting changes in cortisol levels immediately after intervention. Low-quality evidence further indicated (not pooled) that spinal manipulation can influence inflammatory markers such as interleukins levels post-intervention. There was also very low-quality evidence that spinal manipulation does not influence substance-P, neurotensin, oxytocin, orexin-A, testosterone and epinephrine/nor-epinephrine.
The authors concluded that spinal manipulation may influence inflammatory and cortisol post-intervention. However, the wider prediction intervals in most outcome measures point to the need for future research to clarify and establish the clinical relevance of these changes.
The majority of the studies were of low or very low quality. This means that the collective evidence is less than reliable. In turn, this means, I think, that the conclusions are misleading. A more honest conclusion would be this:
There is no reliable evidence that spinal manipulation influences inflammatory and cortisol levels.
As for the clinical relevance, I would like to point out that it would not be surprising if chiropractors could one day convincingly show that spinal manipulation do influence various biochemical markers. Many things do! If you fall down a staircase, for instance, plenty of biochemical markers will be affected. This, however, does not mean that throwing our patients down the stairs is of therapeutic value.
This study aimed to compare the effects of cognitive functional therapy (CFT) and movement system impairment (MSI)-based treatment on pain intensity, disability, Kinesiophobia, and gait kinetics in patients with chronic non-specific low back pain (CNSLBP).
In a single-blind randomized clinical trial, the researchers randomly assigned 91 patients with CNSLBP into CFT (n = 45) and MSI-based treatment (n = 46) groups. An 8-week training intervention was given to both groups. The researchers measured the primary outcome, which was pain intensity (Numeric rating scale), and the secondary outcomes, including disability (Oswestry disability index), Kinesiophobia (Tampa Kinesiophobia Scale), and vertical ground reaction force (VGRF) parameters at self-selected and faster speed (Force distributor treadmill). They evaluated patients at baseline, at the end of the 8-week intervention (post-treatment), and six months after the first treatment. Mixed-model ANOVA was used to evaluate the effects of the interaction between time (baseline vs. post-treatment vs. six-month follow-up) and group (CFT vs. MSI-based treatment) on each measure.
CFT showed superiority over MSI-based treatment in reducing pain intensity (P < 0.001, Effect size (ES) = 2.41), ODI (P < 0.001, ES = 2.15), and Kinesiophobia (P < 0.001, ES = 2.47) at eight weeks. The CFT also produced greater improvement in VGRF parameters, at both self-selected (FPF[P < 0.001, ES = 3], SPF[P < 0.001, ES = 0.5], MSF[P < 0.001, ES = 0.67], WAR[P < 0.001, ES = 1.53], POR[P < 0.001, ES = 0.8]), and faster speed, FPF(P < 0.001, ES = 1.33, MSF(P < 0.001, ES = 0.57), WAR(P < 0.001, ES = 0.67), POR(P < 0.001, ES = 2.91)] than the MSI, except SPF(P < 0.001, ES = 0.0) at eight weeks.
The authors concluded that this study suggests that the CFT is associated with better results in clinical and cognitive characteristics than the MSI-based treatment for CNSLBP, and the researchers maintained the treatment effects at six-month follow-up. Also, This study achieved better improvements in gait kinetics in CFT. CTF seems to be an appropriate and applicable treatment in clinical setting.
To understand this study, we need to know what CFT and MSI exactly entailed. Here is the information that the authors provide:
Movement system impairment-based treatment
The movement system impairment-based treatment group received 11 sessions of MSI-based treatment over the 8 weeks for 60 min per session with a supervision of a native speaker experienced (above 5 years) physical therapist with the knowledge of MSI-based treatment. The researchers designed the MSI-based treatment uniquely for each patient based on the interview, clinical examination, and questionnaires, just like they did with the CFT intervention. First, they administered standardized tests to characterize changes in the patient’s low back pain symptoms, and then they modified the treatment to make it more specific based on the participant’s individual symptoms. Depending on the participant’s direction-specific low back pain classification, they performed the intervention following one of the five MSI subgroups namely [1] rotation, [2] extension, [3] flexion, [4] rotation with extension, and [5] rotation with flexion. Finally, Patients treated using the standardized MSI protocol as follows: [1] education regarding normal postures and movements such as sitting, walking, bending, standing, and lying down; [2] education regarding exercises to perform trunk movements as painlessly as possible; and [3] prescription of functional exercises to improve trunk movement [32].
Cognitive functional therapy
Cognitive functional therapy was prescribed for each patient in CFT group based the CFT protocol conducted by O’Sullivan et al. (2015). Patients received supervised 12 sessions of training over the 8-week period with 60 min per session provided with another physical therapist who had been trained in CFT treatment. In this protocol, a physical therapist with more than 5 years of experience conducted an interview and physical examination of the patients to determine their own unique training programs, considering modifiable cognitive, biopsychosocial, functional, and lifestyle behavior factors. The intervention consists of the following 3 main stages: [1] making sense of pain that is completely reflective, where physical therapist could use the context of the patient’s own story to provide a new understanding of their condition and question their old beliefs [2] exposure with control which is designed to normalize maladaptive or provocative movement and posture related to activities of daily living that is integrated into each patient’s functional impairments, including teaching how to relax trunk muscles, how to have normal body posture while sitting, lying, bending, lifting, moving, and standing, and how to avoid pain behaviors, which aims to break poor postural habits; and [3] lifestyle change which is investigating the influence of unhealthy lifestyles in the patient’s pain context. Assessing the individual’s body mass, nutrition, quality of sleep, levels of physical activity or sedentary lifestyle, smoking, and other factors via video calls. Identifying such lifestyle factors helped us to individually advise and design exercise programs, rebuild self-confidence and self-efficacy, promote changes in lifestyle, and design coping strategies.
I must admit that I am not fully convinced.
Firstly, the study was not large and we need – as the authors state – more evidence. Secondly, I am not sure that the results show CFT to be more effective that MSI. They might merely indicate 1) that the bulk of the improvement is due to non-specific effects (e.g. reression towards the mean, natural history of the condition, placebo) and 2) that CFT is less harmful than MSI.
My conclusion:
we need not just more but better evidence.
This study aimed to compare the effectiveness of three distinct interventions – Yoga, Naturopathy, and Conventional medical management – in alleviating pain, reducing disability, enhancing spinal mobility, and improving the quality of life in individuals with low back pain. Ninety participants were recruited and randomly divided into three groups.
- The first group (group 1) received Yoga,
- the second group (group 2) received Naturopathy treatments,
- the third group served as the control and received conventional medications.
Visual Analogue Scale (VAS) scores, Oswestry Disability Index (ODI), Flexion Test-Finger to Floor Test (FTFT) results, and Quality of Life (QOL) were assessed at baseline and after a 10-day intervention period for all groups.
Overall comparisons between the groups, utilizing ANOVA, revealed marked differences in pain severity, disability index, daily functional capacity, and Quality of Life (QoL) improvements following respective interventions. Substantial improvements were also noted within the yoga and naturopathic medicine groups across multiple variables.
The authors concluded that the results of this comparative analysis emphasize the effectiveness of Yoga, Naturopathy, and Conventional Medical Treatment in managing low back pain. All three interventions demonstrated significant improvements in pain intensity, disability, spinal mobility, and quality of life. This study contributes valuable insights into the diverse therapeutic approaches for low back pain management, highlighting the potential of holistic and alternative treatments to enhance patients’ well-being.
__________________
This is a remarkably poor study. Its flaws are too numerous to account for them all here. Let me focus on just a three that stand out.
- All we learn about the 3 treatment regimen is this (and it clearly not enough to do an independent replication of this trial):
Yoga Group:
Participants in the Yoga Group underwent a specifically designed integrated approach of Yoga therapy (IAYT) for back pain, incorporating relaxation techniques, spinal movements, breathing exercises, pranayama, and deep relaxation techniques. The intervention was conducted by qualified yoga instructors at SDM College of Naturopathy and Yogic Sciences.
Naturopathy Group:
Participants in the Naturopathy Group received neutral spinal baths and partial massages. The spinal bath was administered at Government Yoga & Nature Cure Out Patient Center, Puttur, and massages were performed by trained naturopathy therapists.
Conventional Medicine Group:
Participants in the Conventional Medicine Group received standard medical treatments for low back pain as recommended by orthopedic physicians from S.D.M Medical College, Dharward
- As an equivalence trial, the sample size of this study is far too small. This means that its findings are most likely caused by coincidence and not by the interventions applied.
- There was no attempt of blinding the patients. Therefore, the results – if they were otherwise trustworthy – would be dominated by expectations and not by the effects of the treatments.
Altogether, this study is, I think, a good example for the fact that
poor research often is worse than no research at all.
Women experience more problems in their sexual functioning after childbirth. Due to the high prevalence of sexual problems during the lactation period, the World Health Organization suggests that measures are needed to improve women’s sexual functioning during breastfeeding. This study investigated the effect of auricular acupressure on sexual functioning among lactating women.
A randomized, sham-controlled trial was conducted between October 2019 to March 2020 in urban comprehensive health centers of Qazvin, Iran. Seventy-six women who had been lactating between six months and one year postpartum were randomly assigned to auricular acupressure group (n=38) or sham control group (n=38) using a balanced block randomization method. The intervention group received ear acupressure in 10 sessions (at four-day intervals) and control group received the sham intervention at the same intervals. Sexual functioning was the primary outcome of the study (assessed using the Female Sexual Function Index) before and at three time points post-intervention (immediately after, one month after, and two months after). The secondary outcome was sexual quality of life assessed using Sexual Quality of Life-Female Version.
Auricular acupressure had a large effect on female sexual functioning at all three post-intervention time points:
- immediately after the intervention (adjusted mean difference [95% CI]: 8.37 [6.27; 10.46] with Cohen’s d [95% CI]: 1.81[1.28; 2.34]),
- one month after the intervention (adjusted mean difference [95% CI]: 8.44 [6.41; 10.48] with Cohen’s d [95% CI]: 2.01 [1.46; 2.56]),
- two months after the intervention (adjusted mean difference [95% CI]: 7.43 [5.12; 9.71] with Cohen’s d [95% CI]: 1.57 [1.06; 2.08]).

Acupressure significantly increased participants’ sexual quality of life on the Sexual Quality of Life-Female scale by 13.73 points in the intervention group compared to the control group (p<0.001). The effect size of intervention for female sexual quality was large (adjusted Cohen’s d [95% CI]: 1.09 [0.58; 1.59]). Weekly frequency of sexual intercourse in the intervention group significantly increased compared to sham control group (p<0.001). These changes were clinically significant for sexual functioning and sexual quality of life.
The authors concluded that auricular acupressure was effective in increasing quality of sexual life and sexual functioning among lactating women. Although further research is needed to confirm the efficacy of auricular acupressure, based on the present study’s findings, the use of auricular acupressure by women’s healthcare providers after childbirth is recommended.
One possible explanation for this result is that the study was de-blinded; the sham treatment might not have been distinguished from the verum, or the verbal and/or non-verbal communications between the therapist and the patients contributed to a de-blinding effect. As the sucess of blinding was not reported and probably not even tested, we cannot know. The authors explain that auricular acupressure might improve both endocrine function (increased sex hormones including androgens and estrogens) and its physiological consequences (e.g., vaginal dryness, and vaginal epithelial atrophy), as well as reducing fatigue and insomnia problems (which might increase sexual desire).
Personally, I find this VERY hard to believe. Auricular acupressure or auriculotherapy, as it is also called, was invented by Paul Nogier in the 1950s. Its assumptions are not in line with our knowledge of anatomy and physiology. The different maps used by proponents of auriculotherapy show embarrassing disagreements. The therapy is being promoted as a treatment for many conditions. However, the clinical evidence that it might be effective is weak, not least because many of the clinical trials are of low quality and thus unreliable. One of the first rigorous tests of auriculotherapy was published in 1984 by one of the most prominent researchers of pain, R. Melzack. Here is the abstract[2]:
Enthusiastic reports of the effectiveness of electrical stimulation of the outer ear for the relief of pain (“auriculotherapy”) have led to increasing use of the procedure. In the present study, auriculotherapy was evaluated in 36 patients suffering from chronic pain, using a controlled crossover design. The first experiment compared the effects of stimulation of designated auriculotherapy points, and of control points unrelated to the painful area. A second experiment compared stimulation of designated points with a no-stimulation placebo control. Pain-relief scores obtained with the McGill Pain Questionnaire failed to show any differences in either experiment. It is concluded that auriculotherapy is not an effective therapeutic procedure for chronic pain.
Today we have an abundance of clinical trials of this therapy. Their results are by no means uniform. It is therefore best not to rely on single studies but on systematic reviews that include the evidence from all reliable trials. Our review concluded that “because of the paucity and of the poor quality of the data, the evidence for the effectiveness of auricular therapy for the symptomatic treatment of insomnia is limited. Further, rigorously designed trials are warranted to confirm these results.”[3] Other, less rigorous reviews arrive at more positive conclusions; due to the often poor quality of the primary studies, they should, however, be interpreted with great caution.[4]
The most frequently reported adverse events of auriculotherapy include local skin irritation and discomfort, mild tenderness or pain, and dizziness. Most of these events were transient, mild, and tolerable, and no serious adverse events were identified.[5]
In view of all this, I think that we need much more and much better evidence for auricular acupressure to be recommended for ANY condition.
[1] Wirz-Ridolfi A. The History of Ear Acupuncture and Ear Cartography: Why Precise Mapping of Auricular Points Is Important. Med Acupunct. 2019 Jun 1;31(3):145-156. doi: 10.1089/acu.2019.1349.
[2] Melzack, R., & Katz, J. (1984). Auriculotherapy fails to relieve chronic pain. A controlled crossover study. JAMA, 251(8), 1041–1043.
[3] Lee MS, Shin BC, Suen LK, Park TY, Ernst E (2008) Auricular acupuncture for insomnia: a systematic review. Int J Clin Pract 62(11):1744–1752.
[4] Usichenko, T. I., Hua, K., Cummings, M., Nowak, A., Hahnenkamp, K., Brinkhaus, B., & Dietzel, J. (2022). Auricular stimulation for preoperative anxiety – A systematic review and meta-analysis of randomized controlled clinical trials. Journal of clinical anesthesia, 76, 110581.
[5] Tan JY, Molassiotis A, Wang T, Suen LK (2014) Adverse events of auricular therapy: a systematic review. Evid Based Complement Alternat Med 2014:506758
A ‘pragmatic, superiority, open-label, randomised controlled trial’ of sleep restriction therapy versus sleep hygiene has just been published in THE LANCET. Adults with insomnia disorder were recruited from 35 general practices across England and randomly assigned (1:1) using a web-based randomisation programme to either four sessions of nurse-delivered sleep restriction therapy plus a sleep hygiene booklet or a sleep hygiene booklet only. There was no restriction on usual care for either group. Outcomes were assessed at 3 months, 6 months, and 12 months. The primary endpoint was self-reported insomnia severity at 6 months measured with the insomnia severity index (ISI). The primary analysis included participants according to their allocated group and who contributed at least one outcome measurement. Cost-effectiveness was evaluated from the UK National Health Service and personal social services perspective and expressed in terms of incremental cost per quality-adjusted life year (QALY) gained. The trial was prospectively registered (ISRCTN42499563).
Between Aug 29, 2018, and March 23, 2020 the researchers randomly assigned 642 participants to sleep restriction therapy (n=321) or sleep hygiene (n=321). Mean age was 55·4 years (range 19–88), with 489 (76·2%) participants being female and 153 (23·8%) being male. 580 (90·3%) participants provided data for at least one outcome measurement. At 6 months, mean ISI score was 10·9 (SD 5·5) for sleep restriction therapy and 13·9 (5·2) for sleep hygiene (adjusted mean difference –3·05, 95% CI –3·83 to –2·28; p<0·0001; Cohen’s d –0·74), indicating that participants in the sleep restriction therapy group reported lower insomnia severity than the sleep hygiene group. The incremental cost per QALY gained was £2076, giving a 95·3% probability that treatment was cost-effective at a cost-effectiveness threshold of £20 000. Eight participants in each group had serious adverse events, none of which were judged to be related to intervention.
The authors concluded that brief nurse-delivered sleep restriction therapy in primary care reduces insomnia symptoms, is likely to be cost-effective, and has the potential to be widely implemented as a first-line treatment for insomnia disorder.
I am frankly amazed that this paper was published in a top journal, like THE LANCET. Let me explain why:
The verum treatment was delivered over four consecutive weeks, involving one brief session per week (two in-person sessions and two sessions over the phone). Session 1 introduced the rationale for sleep restriction therapy alongside a review of sleep diaries, helped participants to select bed and rise times, advised on management of daytime sleepiness (including implications for driving), and discussed barriers to and facilitators of implementation. Session 2, session 3, and session 4 involved reviewing progress, discussion of difficulties with implementation, and titration of the sleep schedule according to a sleep efficiency algorithm.
This means that the verum group received fairly extensive attention, while the control group did not. In other words, a host of non-specific effects are likely to have significantly influenced or even entirely determined the outcome. Despite this rather obvious limitation, the authors fail to discuss any of it. On the contrary, that claim that “we did a definitive test of whether brief sleep restriction therapy delivered in primary care is clinically effective and cost-effective.” This is, in my view, highly misleading and unworthy of THE LANCET. I suggest the conclusions of this trial should be re-formulated as follows:
The brief nurse-delivered sleep restriction, or the additional attention provided exclusively to the patients in the verum group, or a placebo-effect or some other non-specific effect reduced insomnia symptoms.
Alternatively, one could just conclude from this study that poor science can make it even into the best medical journals – a problem only too well known in the realm of so-called alternative medicine (SCAM).
This systematic review evaluated all available randomized controlled trials (RCTs) investigating the clinical effects of hydrotherapy according to Kneipp which is characterized by cold water applications. All RCTs on therapy and prevention with Kneipp hydrotherapy were included. Study participants were patients and healthy volunteers of all age groups. MEDLINE (via PubMed), Scopus, Central, CAMbase, and opengrey.eu were systematically searched through April 2021 without language restrictions and updated by searching PubMed until April 6th 2023. The risk of bias was assessed using the Cochrane tool version 1.
Twenty RCTs (N=4247) were included. Due to the high heterogeneity of the RCTs, no meta-analysis was performed. The risk of bias was rated as unclear in most of the domains. Of 132 comparisons, 46 showed significant positive effects in favor of hydrotherapy on chronic venous insufficiency, menopausal symptoms, fever, cognition, emotional function, and sickness absenteeism. However, 81 comparisons showed no differences between groups, and 5 were in favor of the respective control group. Only half of the studies reported safety issues.
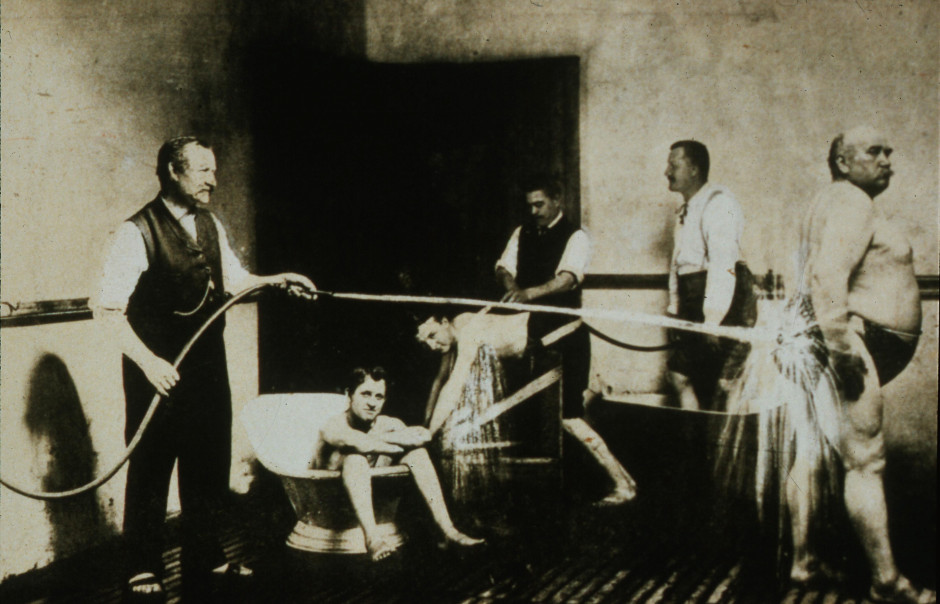
The authors concluded that although RCTs on Kneipp hydrotherapy seem to show positive effects in some conditions and outcomes, it remains difficult to ascertain treatment effects due to the high risk of bias and heterogeneity of most of the considered studies. Further high-quality RCTs on Kneipp hydrotherapy are urgently warranted.
This is certainly the best review of the subject so far. It makes it very clear that the evidence for Kneipp hydrotherapy is weak, mostly because of the many flaws in the primary studies. One needs to add, I think, that 20 RCTs are an absurdly small amount considering that many indications this type of therapy is advocated for – many enthusiasts even consider it a panacea.
It follows, I fear, that Kneipp hydrotherapy is almost entirely not evidence-based. This should be bad news for the numerous institutions and Spa towns (mostly in Germany) that live on employing this treatment and telling patients that it is effective. They usually claim that experience shows this to be true. But this was the mantra of medicine ~100 years ago. Since then, we have learned that experience is a very poor guide that regularly leads us up the garden path.
Kneippians will counter that clinical trials are difficult to conduct and expensive to finance. Both arguments are of course true but, considering that an entire industry lives on telling patients something that essentially amounts to a lie (i.e. the claim that it works), it surely is obligatory to overcome these obstacles.
Cervical artery dissection (CeAD), which includes both vertebral artery dissection (VAD) and carotid artery dissection (CAD), is the most serious safety concern associated with cervical spinal manipulation (CSM). This study evaluated the association between CSM and CeAD among US adults.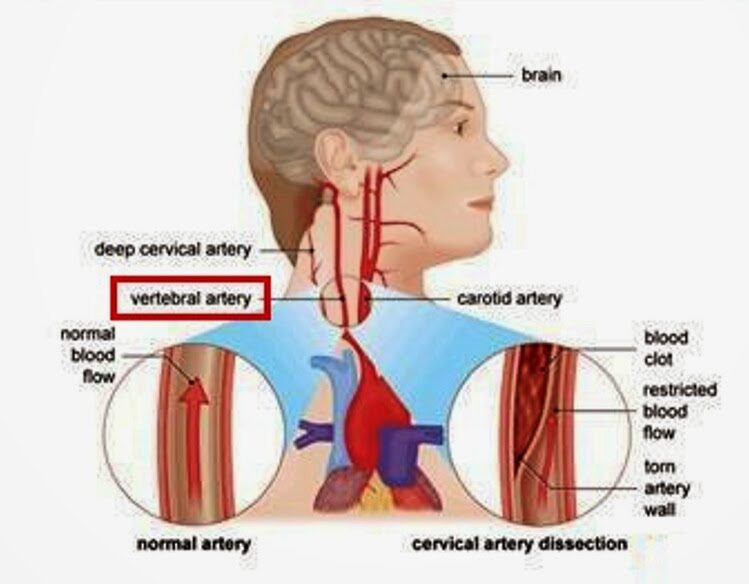
Through analysis of health claims data, the researchers employed a case-control study with matched controls, a case-control design in which controls were diagnosed with ischemic stroke, and a case-crossover design in which recent exposures were compared to exposures in the same case that occurred 6-7 months earlier. The researchers evaluated the association between CeAD and the 3-level exposure, CSM versus office visit for medical evaluation and management (E&M) versus neither, with E&M set as the referent group.
2337 VAD cases and 2916 CAD cases were identified. Compared to population controls, VAD cases were 0.17 (95% CI 0.09 to 0.32) times as likely to have received CSM in the previous week as compared to E&M. In other words, E&M was about 5 times more likely than CSM in the previous week in cases, relative to controls. CSM was 2.53 (95% CI 1.71 to 3.68) times as likely as E&M in the previous week among individuals with VAD than among individuals experiencing a stroke without CeAD. In the case-crossover study, CSM was 0.38 (95% CI 0.15 to 0.91) times as likely as E&M in the week before a VAD, relative to 6 months earlier. In other words, E&M was approximately 3 times more likely than CSM in the previous week in cases, relative to controls. Results for the 14-day and 30-day timeframes were similar to those at one week.
The authors concluded that, among privately insured US adults, the overall risk of CeAD is very low. Prior receipt of CSM was more likely than E&M among VAD patients as compared to stroke patients. However, for CAD patients as compared to stroke patients, as well as for both VAD and CAD patients in comparison with population controls and in case-crossover analysis, prior receipt of E&M was more likely than CSM.
What seems fairly clear from this and a previous similar analysis by the same authors is, I think, this: retrospective studies of this type can unfortunately not provide us with much reliable information about the risks of spinal manipulation. The reasons for this are manyfold, e.g.: less than exact classifications in patients’ records, or the fact that multiple types of spinal manipulations exist of which only some might be dangerous.
I have seen some daft meta-analyses in my time – this one, however, takes the biscuit. Here is its unaltered abstract:
Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
___________________________
This meta-analysis has too many serious flaws to mention. Let me therefore just focus on the main two:
- Craniosacral Therapy is not an MBMBT.
- Craniosacral Therapy is not effective for NLBP. The false positive result was generated on the basis of 4 studies. All of them have serious methodological problems that prevent an overall positive conclusion about the effectiveness of this treatment. In case you don’t believe me, here are the 4 abstracts:
1) Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
2) Background: Craniosacral therapy (CST) and sensorimotor training (SMT) are two recommended interventions for nonspecific chronic low back pain (NCLBP). This study compares the effects of CST and SMT on pain, functional disability, depression and quality of life in patients with NCLBP.
Methodology: A total of 31 patients with NCLBP were randomly assigned to the CST group (n=16) and SMT (n=15). The study patients received 10 sessions of interventions during 5 weeks. Visual analogue scale (VAS), Oswestry disability index (ODI), Beck depression inventory-II (BDI-II), and Short Form-36 (SF-36) questionnaires were used at baseline (before the treatment), after the treatment, and 2 months after the last intervention session. Results were compared and analyzed statistically.
Results: Both groups showed significant improvement from baseline to after treatment (p < 0.05). In the CST group, this improvement continued during the follow-up period in all outcomes (p < 0.05), except role emotional domain of SF-36. In the SMT group, VAS, ODI and BDI-II increased during follow-up. Also, all domains of SF-36 decreased over this period. Results of group analysis indicate a significant difference between groups at the end of treatment phase (p < 0.05), except social functioning.
Conclusions: Results of our research confirm that 10 sessions of craniosacral therapy (CST) or sensorimotor training (SMT) can significantly control pain, disability, depression, and quality of life in patients with NCLBP; but the efficacy of CST is significantly better than SMT.
3) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
4) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
_______________________________
I REST MY CASE
This article by a Postgraduate Trainee (Dept. of Case Taking and Repertory, National Institute of Homoeopathy, Govt. of India) an Assistant Professor (Dept. of Surgery, National Institute of Homoeopathy Govt. of India) and another Assistant Professor (Dept. of Obstetrics & Gynaecology, Midnapore Homoeopathic Medical College & Hospital, Govt. of West Bengal) might not be available online (Clinical Medicine and Health Research Journal, Volume 03, Issue 03, May – June 2023 Page No. 444-446) but it is I think worth discussing. Here is its abstract:
Warts are one of the common dermatological disorders caused by human papilloma viruses encountered in our day to day life. These are cutaneous or mucosal infection needs proper care and treatment to prevent its transmission and complete healing. Although mostly warts are dealt with the therapeutic approach, i.e. on the basis of its peculiar type and location but it can even be successfully treated by constitutional approach. This article is regarding a case of warts treated successfully with Rhus Tox followed by Ferrum Met selected as the simillimum and proved its effectiveness in a short period of time.
As the abstract is not very informative, let me show you also some sections from the paper itself:
The patient presented with warts on right wrist for 1 year. There were plane warts at back of wrist, which was smooth, slightly elevated and skin coloured. There was no history of warts or other benign skin disease in the family. This case treated with individualized homoeopathic medicine showed complete resolution of the warts. There is no cure for wart in conventional medicine except removal of them with various methods. Although it does not rule out the chance of recurrence, later on may deep organic disease. That is why a substantial number of warts patients resort to Complementary and Alternative Medicine (CAM), especially homoeopathy.
In this case, Ferrum Metallicum 0/1 was selected as a ‘similimum’ based on totality of symptoms, repertorial analysis and consultation with Homoeopathic Materia Medica, which was given more priority in this case. After seeing improvement, succeeding potency was prescribed. After Ferrum Met 0/4 all her complaints including warts disappeared. Thus, the outcome of this case of Plane Warts of the lady shows the success of individualized homoeopathic medicine in treatment of wart.
Conclusion:
This case report suggests homoeopathic treatment as a promising complementary or alternative therapy and emphasizes the need of repertorisation in individualized homoeopathic prescription. This case shows a positive role of homoeopathic in treating Warts. However, this is a single case study and requires well designed studies which may be taken up for future scientific validation.
This case report reminded me of an exciting and quite lovely story: at Exeter, we once conducted a wart study. It was a placebo-controlled, double-blind trial where the verum group received distant healing and the controls nothing at all. After planning the study, I was no longer involved in its running. As I happened to have a wart at the time, I offered myself to my team as a patient. They checked me out and admitted me into the study. For the next weeks, I either received the distant healing energy or nothing; neither I nor my team knew which. My wart was photographed and measured regularly.
And then it happened: shortly after the treatment period was over, my wart had gone. Everyone was excited, especially the UK healing scene. But we had to wait until the trial was finished, the results were calculated, and the random code was opened. The result: no difference between verum and placebo! We concluded that distant healing from experienced healers had no effect on the number or size of patients’ warts.
And my own, very personal wart?
It had disappeared spontaneously – I had been in the control group!
I know Indian homeopaths have a thing about healing warts (we discussed this before) but I am afraid the conclusions of this new paper ought to be re-written:
This case report does not suggest that homeopathic treatment is a promising complementary or alternative therapy. It shows the natural history of the condition in the disappearance of warts.
Maintenance of cognitive abilities is of critical importance to older adults, yet only a few effective strategies to slow down cognitive decline currently exist. Multivitamin supplementation is used to promote general health; however, it is unclear whether it favorably affects cognition in older age. This study aimed to examine the effect of daily multivitamin/multimineral supplementation on memory in older adults.
The Cocoa Supplement and Multivitamin Outcomes Study Web (COSMOS-Web) ancillary study (NCT04582617) included 3562 older adults. Participants were randomly assigned to a daily multivitamin supplement (Centrum Silver) or placebo and evaluated annually with an Internet-based battery of neuropsychological tests for 3 y. The prespecified primary outcome measure was change in episodic memory, operationally defined as immediate recall performance on the ModRey test, after 1 y of intervention. Secondary outcome measures included changes in episodic memory over 3 y of follow-up and changes in performance on neuropsychological tasks of novel object recognition and executive function over 3 y.
Compared with placebo, participants randomly assigned to multivitamin supplementation had significantly better ModRey immediate recall at 1 y, the primary endpoint (t(5889) = 2.25, P = 0.025), as well as across the 3 y of follow-up on average (t(5889) = 2.54, P = 0.011). Multivitamin supplementation had no significant effects on secondary outcomes. Based on a cross-sectional analysis of the association between age and performance on the ModRey, it was estimated that the effect of the multivitamin intervention improved memory performance above placebo by the equivalent of 3.1 y of age-related memory change.
The authors concluded that daily multivitamin supplementation, compared with placebo, improves memory. Multivitamin supplementation holds promise as a safe and accessible approach to maintaining cognitive health in older age.
These findings are surprising, not least because similar studies have thus far failed to demonstrate such effects. A 2013 trial, for instance, concluded that, in male physicians aged 65 years or older, long-term use of a daily multivitamin did not provide cognitive benefits.
Judging from the abstract alone (unfortunately, I have no access to the full paper), this seems to be a rigorous trial. It was conducted by multiple researchers of high standing. One is therefore inclined to believe the results.
Yet, one might be wise to be cautious.
Provided that a full analysis of the study does not identify major flaws, I would still want to 1) have a plausible explanation as to the mode of action and 2) see an independent replication before I accept the findings.
PS
The study was partly funded by the National Institutes of Health. The vitamins were provided by Pfizer Inc. and Haleon, the makers of the supplement used in the study.
PPS
I have now seen the full paper [thank you Dan] and can confirm that the study was of high quality. Yet, it also has limitations, of course, e.g.:
- the effect size is modest;
- the study population is selected and thus the results are not generalizable;
- the outcome measures were assessed remotely;
- the success of blinding was not checked [I find it conceivable that some trial participants tried to find out what they were taking, e.g. by tasting the pills].
