spinal manipulation
The website of the World Federation of Chiropractic (WFC) points out that public health is defined by the WHO as follows:
“Activities to strengthen public health capacities and service aim to provide conditions under which people can maintain to be healthy, improve their health and wellbeing, or prevent the deterioration of their health. Public health focuses on the entire spectrum of health and wellbeing, not only the eradication of particular diseases.”
The WFC then continues stating this:
As primary contact health professionals, chiropractors can play an important role as public health advocates. This can range from providing support and advice on health matters such as physical activity, diet, and fitness as well as lifestyle choices such as injury prevention and avoiding tobacco use. Chiropractors can also play a role in counselling patients and communities on the benefits of public health measures, especially as this relates to immediate health needs of each region.
I think that this might merit a few comments.
- Physical activity is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Diet is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Fitness is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Lifestyle choice is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Injury prevention is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Avoiding tobacco use is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
- Counseling is undoubtedly an important issue for public health; however, there are clearly healthcare professionals who are in a better-informed position to advise on it than chiropractors.
So, what is the real contribution of chiropractors to public health?
- Chiropractors tend to advise their clients against vaccinations.
- Some mislead the public by claiming they boost immunity and prevent serious infections.
- Many undermine evidence-based medicine by promoting obsolete myths such as ‘the innate’ or subluxations.
- Many sell supplements that could interact with prescription drugs.
- Many make bogus health claims for profit.
I would therefore argue that, on balance, the contribution of chiropractors to public health might be considerable …
sadly, however, it goes in the wrong direction.
In a video, Mr.Darkmoore speaks from a hospital bed and says the cause behind his visit to the emergency room stemmed from a chiropractor’s work on him. Three days ago, he had a ringing in his ear due to a long-term condition he knew as tinnitus. Thus, he decided to visit a chiropractor. “I figured $100 to a chiro, let them adjust a few things, if all else fails, I’ll go to a doctor,” explains Darkmoore.
This $100 visit led to several other complications and doctor’s bills worth thousands of dollars. The day after he was treated by the chiropractor, he experienced a headache that eventually led to dizzy spells. He decided to visit the emergency room where a CT scan was ordered which showed that the chiropractor had dissected an artery in his neck.
Next, Darkmoore was put on blood thinners to avoid blood clots that could result in a stroke or worse. Darkmoore explains that he will be on two blood thinners for the next three months to prevent clotting. If the dissection heals partially, he says he will need to take aspirin every day for the rest of his life. If it doesn’t heal, he claims that he will need surgery.
Many viewers of the video claimed they have had the same “chiropractor gone wrong” experience as Darkmoore.
- “Wow. How scary. I had a similar thing happen to me. Extremely bad headache after going one time. Haven’t gone since,” one commenter wrote.
- “I’m so sorry this happened to u,” another user echoed. “My chiropractor also caused an injury which required emergency surgery & I have permanent damage. I’m glad u survived.”
Darkmore captioned his last update video, “I appreciate the thoughts and prayers. Hopefully, I’ll be okay after 3 months of recovery.”
__________________
Let’s hope that he is correct and that he will make a speedy and full recovery.
Of course, chiros will queue up to stress that important details are missing in this case report. To them, I would merely say this:
THERE IS NO GOOD EVIDENCE THAT NECK MANIPULATIONS BRING ANY BENEFIT AND QUITE A BIT OF EVIDENCE THAT THEY CAN CAUSE SERIOUS HARM.
SO, WHY NOT JUST STOP OFFERING THE PROCEDURE?
An impressive article by John Mac Ghlionn caught my attention. Allow me to quote a few passages from it:
The U.S. House of Representatives and the U.S. Senate recently reintroduced legislation to increase access to Medicare-covered services provided by chiropractors. Last year, the US chiropractic market size was worth $13.13 Billion. By the end of the decade, it will be worth over $18 billion. Each year, a whopping 35 million Americans seek chiropractic care.
But why? It’s a questionable science full of questionable characters.
Last year, a Georgia woman was left paralyzed and unable to speak after receiving a neck adjustment from a chiropractor. She’s not the first person to have had her life utterly ruined by a chiropractor, and chances are she won’t be the last. Many patients who visit chiropractors suffer severe side effects; some lose their lives…
As Dr. Steven Novella has noted, what used to be fraud is now known as holistic medicine. Dr. Edzard Ernst, a retired British-German physician and researcher, has expertly demonstrated the many ways in which chiropractic treatments are rooted not in science, but in mystical concepts…
Spinal adjustments, also known as “subluxations,” are also common. A dangerous practice that has been heavily criticized, spinal manipulations are associated with a number of adverse effects, including the risk of stroke. As Dr. Ernst has noted, the cost-effectiveness of this particular treatment “has not been demonstrated beyond reasonable doubt.”
Not content with spinal and neck manipulations, some chiropractors offer to treat other conditions — like diabetes, for example. They are not trained to treat diabetes. Other chiropractors appear to take joy in torturing infants. In August of 2018, a chiropractor made headlines for all the wrong reasons when a video emerged showing him hanging a two-week-old newborn upside down by the ankles…
Finally, as I alluded to earlier, the chiropractic community is full of fraudsters. In 2019, in the US, 15 chiropractors were charged in an insurance fraud and illegal kickback operation. More recently, in February of this year, a New York federal judge sentenced Patrick Khaziran to 30 months in prison after he pleaded guilty to being part of a widespread scheme that defrauded the NBA out of at least $5 million. In recent times, the chiropractic community has come under scrutiny for abusive care and illegal billing practices. When it comes to instances of healthcare fraud, chiropractic medicine is unrivaled.
None of this should come as a surprise. After all, the entire chiropractic community was constructed on a foundation of lies. As the aforementioned Dr. Ernst told me, we should be skeptical of what chiropractors are offering, largely because the whole practice was founded “by a deluded charlatan, who insisted that all human diseases are due to subluxations of the spine. Today, we know that chiropractic subluxations are mere figments of Palmer’s imagination. Yet, the chiropractic profession is unable to separate itself from the myth. It is easy to see why: without it, they would at best become poorly trained physiotherapists without any raison d’etre.”
… Dr. William T. Jarvis famously referred to chiropractic as “the most significant nonscientific health-care delivery system in the United States.” Comparing the chiropractic community to a cult, Dr. Jarvis wondered, somewhat incredulously, why chiropractors are licensed to practice in all 50 US states. The entire profession, he warned, “should be viewed as a societal problem, not simply as a competitor of regular health-care.”
___________________________
In my view, this is an impressive article, not least because it is refreshingly devoid of the phenomenon known as ‘false balance, e.g. a chiropractor being invited to add his self-interested views at the end of the paper claiming, for instance, “we have years of experience and cause far less harm than real doctors”.
Cervical artery dissection (CeAD), which includes both vertebral artery dissection (VAD) and carotid artery dissection (CAD), is the most serious safety concern associated with cervical spinal manipulation (CSM). This study evaluated the association between CSM and CeAD among US adults.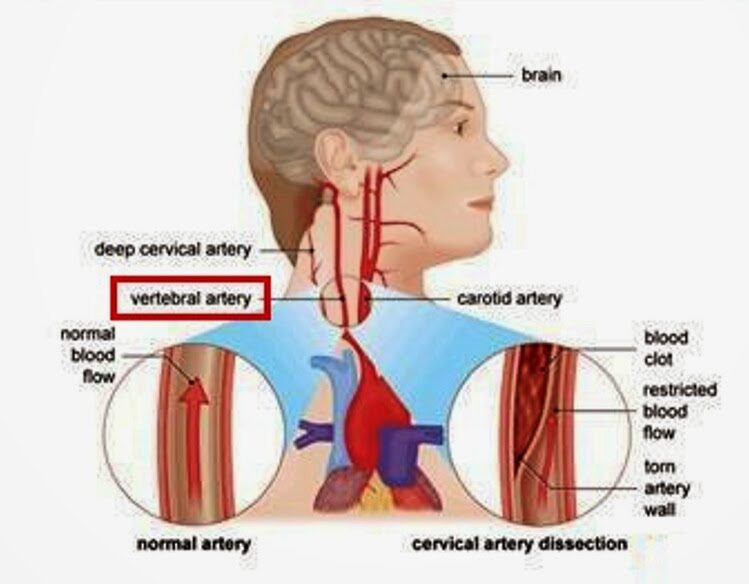
Through analysis of health claims data, the researchers employed a case-control study with matched controls, a case-control design in which controls were diagnosed with ischemic stroke, and a case-crossover design in which recent exposures were compared to exposures in the same case that occurred 6-7 months earlier. The researchers evaluated the association between CeAD and the 3-level exposure, CSM versus office visit for medical evaluation and management (E&M) versus neither, with E&M set as the referent group.
2337 VAD cases and 2916 CAD cases were identified. Compared to population controls, VAD cases were 0.17 (95% CI 0.09 to 0.32) times as likely to have received CSM in the previous week as compared to E&M. In other words, E&M was about 5 times more likely than CSM in the previous week in cases, relative to controls. CSM was 2.53 (95% CI 1.71 to 3.68) times as likely as E&M in the previous week among individuals with VAD than among individuals experiencing a stroke without CeAD. In the case-crossover study, CSM was 0.38 (95% CI 0.15 to 0.91) times as likely as E&M in the week before a VAD, relative to 6 months earlier. In other words, E&M was approximately 3 times more likely than CSM in the previous week in cases, relative to controls. Results for the 14-day and 30-day timeframes were similar to those at one week.
The authors concluded that, among privately insured US adults, the overall risk of CeAD is very low. Prior receipt of CSM was more likely than E&M among VAD patients as compared to stroke patients. However, for CAD patients as compared to stroke patients, as well as for both VAD and CAD patients in comparison with population controls and in case-crossover analysis, prior receipt of E&M was more likely than CSM.
What seems fairly clear from this and a previous similar analysis by the same authors is, I think, this: retrospective studies of this type can unfortunately not provide us with much reliable information about the risks of spinal manipulation. The reasons for this are manyfold, e.g.: less than exact classifications in patients’ records, or the fact that multiple types of spinal manipulations exist of which only some might be dangerous.
There is widespread agreement amongst clinicians that people with non-specific low back pain (NSLBP) comprise a heterogeneous group and that their management should be individually tailored. One treatment known by its tailored design is the McKenzie method (e.g. an individualized program of exercises based on clinical clues observed during assessment) used mostly but not exclusively by physiotherapists.
A recent Cochrane review evaluated the effectiveness of the McKenzie method in people with (sub)acute non-specific low back pain. Randomized clinical trials (RCTs) investigating the effectiveness of the McKenzie method in adults with (sub)acute (less than 12 weeks) NSLBP.
Five RCTs were included with a total of 563 participants recruited from primary or tertiary care. Three trials were conducted in the USA, one in Australia, and one in Scotland. Three trials received financial support from non-commercial funders and two did not provide information on funding sources. All trials were at high risk of performance and detection bias. None of the included trials measured adverse events.
McKenzie method versus minimal intervention (educational booklet; McKenzie method as a supplement to other intervention – main comparison) There is low-certainty evidence that the McKenzie method may result in a slight reduction in pain in the short term (MD -7.3, 95% CI -12.0 to -2.56; 2 trials, 377 participants) but not in the intermediate term (MD -5.0, 95% CI -14.3 to 4.3; 1 trial, 180 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -2.5, 95% CI -7.5 to 2.0; 2 trials, 328 participants) nor in the intermediate term (MD -0.9, 95% CI -7.3 to 5.6; 1 trial, 180 participants).
McKenzie method versus manual therapy There is low-certainty evidence that the McKenzie method may not reduce pain in the short term (MD -8.7, 95% CI -27.4 to 10.0; 3 trials, 298 participants) and may result in a slight increase in pain in the intermediate term (MD 7.0, 95% CI 0.7 to 13.3; 1 trial, 235 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -5.0, 95% CI -15.0 to 5.0; 3 trials, 298 participants) nor in the intermediate term (MD 4.3, 95% CI -0.7 to 9.3; 1 trial, 235 participants).
McKenzie method versus other interventions (massage and advice) There is very low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD 4.0, 95% CI -15.4 to 23.4; 1 trial, 30 participants) nor in the intermediate term (MD 10.0, 95% CI -8.9 to 28.9; 1 trial, 30 participants).
The authors concluded that, based on low- to very low-certainty evidence, the treatment effects for pain and disability found in our review were not clinically important. Thus, we can conclude that the McKenzie method is not an effective treatment for (sub)acute NSLBP.
The hallmark of the McKenzie method for back pain involves the identification and classification of nonspecific spinal pain into homogenous subgroups. These subgroups are based on the similar responses of a patient’s symptoms when subjected to mechanical forces. The subgroups include postural syndrome, dysfunction syndrome, derangement syndrome, or “other,” with treatment plans directed to each subgroup. The McKenzie method emphasizes the centralization phenomenon in the assessment and treatment of spinal pain, in which pain originating from the spine refers distally, and through targeted repetitive movements the pain migrates back toward the spine. The clinician will then use the information obtained from this assessment to prescribe specific exercises and advise on which postures to adopt or avoid. Through an individualized treatment program, the patient will perform specific exercises at home approximately ten times per day, as opposed to 1 or 2 physical therapy visits per week. According to the McKenzie method, if there is no restoration of normal function, tissue healing will not occur, and the problem will persist.
Classification:
The postural syndrome is pain caused by mechanical deformation of soft tissue or vasculature arising from prolonged postural stresses. These may affect the joint surfaces, muscles, or tendons, and can occur in sitting, standing, or lying. Pain may be reproducible when such individuals maintain positions or postures for sustained periods. Repeated movements should not affect symptoms, and relief of pain typically occurs immediately following the correction of abnormal posture.
The dysfunction syndrome is pain caused by the mechanical deformation of structurally impaired soft tissue; this may be due to traumatic, inflammatory, or degenerative processes, causing tissue contraction, scarring, adhesion, or adaptive shortening. The hallmark is a loss of movement and pain at the end range of motion. Dysfunction has subsyndromes based upon the end-range direction that elicits this pain: flexion, extension, side-glide, multidirectional, adherent nerve root, and nerve root entrapment subsyndromes. Successful treatment focuses on patient education and mobilization exercises that focus on the direction of the dysfunction/direction of pain. The goal is on tissue remodeling which can be a prolonged process.
The derangement syndrome is the most commonly encountered pain syndrome, reported in one study to have a prevalence as high as 78% of patients classified by the McKenzie method. It is caused by an internal dislocation of articular tissue, causing a disturbance in the normal position of affected joint surfaces, deforming the capsule, and periarticular supportive ligaments. This derangement will both generate pain and obstruct movement in the direction of the displacement. There are seven different subsyndromes which are classified by the location of pain and the presence, or absence, of deformities. Pain is typically elicited by provocative assessment movements, such as flexion or extension of the spine. The centralization and peripheralization of symptoms can only occur in the derangement syndrome. Thus the treatment for derangement syndrome focuses on repeated movement in a single direction that causes a gradual reduction in pain. Studies have shown approximately anywhere between 58% to 91% prevalence of centralization of lower back pain. Studies have also shown that between 67% to 85% of centralizers displayed the directional preference for a spinal extension. This preference may partially explain why the McKenzie method has become synonymous with spinal extension exercises. However, care must be taken to accurately diagnose the direction of pain, as one randomized controlled study has shown that giving the ‘wrong’ direction of exercises can actually lead to poorer outcomes.
Other or Nonmechanical syndrome refers to any symptom that does not fit in with the other mechanical syndromes, but exhibits signs and symptoms of other known pathology; Some of these examples include spinal stenosis, sacroiliac disorders, hip disorders, zygapophyseal disorders, post-surgical complications, low back pain secondary to pregnancy, spondylolysis, and spondylolisthesis.
CONCLUSION:
“Internationally researched” and found to be ineffective!
This study allegedly evaluated the efficacy of osteopathic manipulative therapy (OMT) compared to that of the Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) for patients with chronic LBP.
It included 68 participants of both genders, aged 30 to 60, with chronic LBP. Participants were randomly assigned to one of two parallel groups, each with 34 members. The OMT group received, as a direct technique, a high-velocity/low-amplitude (HVLA) impulse, and as indirect techniques, strain counterstrain (SCS), myofascial release (MFR), and visceral mobilization therapy (VMT). The KEOMT group received lumbar segmental traction and lumbar segmental mobilization-flexion and gliding therapy grade 3. The participants in both groups received 10 treatments, two per week for five weeks. The primary outcome was pain severity, using a numeric pain rating scale (NPRS). The secondary outcome was the measurement of functional disability, using the Oswestry Disability Index (ODI).
The OMT and KEOMT both decreased pain and disability; however, the changes on the NPRS and ODI postintervention were statistically greater for the OMT group compared to the KEOMT group (P < .05).
The authors concluded that the OMT was better at reducing pain and improving quality of life. It reduced functional disability more than KEOMT in patients with chronic LBP.
The Kaltenborn-Evjenth Orthopedic Manipulative Therapy (KEOMT) concept is a treatment and training system based upon a comprehensive biomechanical evaluation of the arthro-neuro-muscular system and an individual’s functional abilities. This system of diagnosis and patient management applies to both patients with acute, subacute and chronic conditions of the spine and extremities and to athletes seeking to improve performance. It offers a reliable and practical approach that focuses on optimal physical health and function.
Has the KEOMT concept been tested and shown to be effective for LBP?
No!
So, what we have here is an equivalence trial of two manual techniques. As such it is FAR too small to yield a meaningful result. If the findings were meaningful, would they show that OMT is effective?
No!
As we have no proof that KEOMT does not impede recovery from LBP, the result could merely be due to the fact that OMT does not influence the natural history of LBP, while KEOMT has a detrimental effect.
Last question: which journal publishes such rubbish?
Ahh, it’s the remarkable Alternative therapies in health and medicine. That explains a lot!
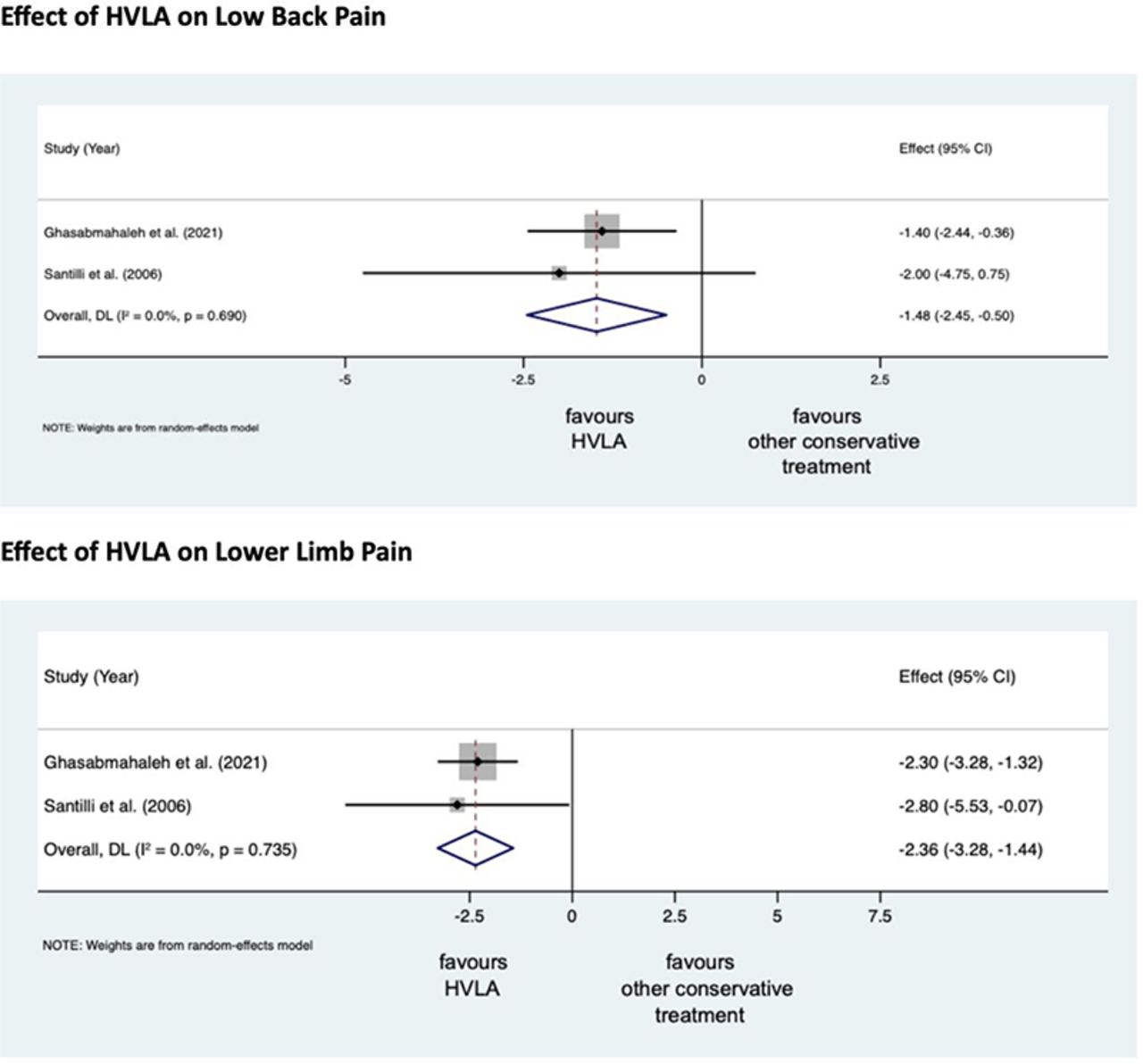
Lumbosacral Radicular Syndrome (LSRS) is a condition characterized by pain radiating in one or more dermatomes (Radicular Pain) and/or the presence of neurological impairments (Radiculopathy). So far, different reviews have investigated the effect of HVLA (high-velocity low-amplitude) spinal manipulations in LSRS. However, these studies included ‘mixed’ population samples (LBP patients with or without LSRS) and treatments other than HVLA spinal manipulations (e.g., mobilisation, soft tissue treatment, etc.). Hence, the efficacy of HVLAT in LSRS is yet to be fully understood.
This review investigated the effect and safety of HVLATs on pain, levels of disability, and health-related quality of life in LSRS, as well as any possible adverse events.
Randomized clinical trials (RCTs) published in English in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (PubMed), EMBASE, PEDro, and Web of Science were identified. RCTs on an adult population (18-65 years) with LSRS that compared HVLATs with other non-surgical treatments, sham spinal manipulation, or no intervention were considered. Two authors selected the studies, extracted the data, and assessed the methodological quality through the ‘Risk of Bias (RoB) Tool 2.0’ and the certainty of the evidence through the ‘GRADE tool’. A meta-analysis was performed to quantify the effect of HVLA on pain levels.
A total of 308 records were retrieved from the search strings. Only two studies met the inclusion criteria. Both studies were at high RoB. Two meta-analyses were performed for low back and leg pain levels. HVLA seemed to reduce the levels of low back (MD = -1.48; 95% CI = -2.45, -0.50) and lower limb (MD = -2.36; 95% CI = -3.28, -1.44) pain compared to other conservative treatments, at three months after treatment. However, high heterogeneity was found (I² = 0.0%, p = 0.735). Besides, their certainty of the evidence was ‘very low’. No adverse events were reported.
The authors stated that they cannot conclude whether HVLA spinal manipulations can be helpful for the treatment of LSRS or not. Future high-quality RCTs are needed to establish the actual effect of HVLA manipulation in this disease with adequate sample size and LSRS definition.
Chiropractors earn their living by applying HVLA thrusts to patients suffering from LSRS. One would therefore have assumed that the question of efficacy has been extensively researched and conclusively answered. It seems that one would have assumed wrongly!
Now that this is (yet again) in the open, I wonder whether chiropractors will, in the future, tell their patients while obtaining informed consent: “I plan to give you a treatment for which sound evidence is not available; it can also cause harm; and, of course, it will cost you – I hope you don’t mind.”
An explanatory sequential mixed methods study with three separate phases was conducted in Danish patients with lumbar radiculopathy receiving a standardized chiropractic care package (SCCP). Lumbar radiculopathy is pain and other neurological symptoms caused by the pinching of nerve roots where they leave your spinal cord in the lumbar region. 
Phase one of the study was a quantitative analysis based on a survey in a prospective cohort of patients with lumbar radiculopathy in an SCCP from 2018 to 2020. Patients rated their satisfaction with the examination, information, treatment effect, and overall management of their problem on a 0–10 scale. In phase two, six semi-structured interviews conducted in 2021 were used to gain further explanatory insights into the findings from phase one. Data were analyzed using systematic text condensation. In phase three, the quantitative and qualitative data were merged in a narrative joint display to obtain a deeper understanding of the overall results.
Here I am only interested in the patients’ perception of the treatment effect. Of 303 eligible patients, 238 responded to the survey. Of these, 50% were very satisfied with the treatment effect.
The authors stated that patients in their study expected a rapid and persistent decrease in symptoms, which, unfortunately, does not match the prognosis of lumbar radiculopathy. Although the prognosis is considered good, the improvement happens gradually and often with fluctuating pain patterns, and it is not unusual to have milder symptoms for three months or longer.
So, only half of the patients who had chosen to consult chiropractors for their lumbar radiculopathy were very satisfied with the treatment results. In most patients, the symptoms decreased only gradually often with fluctuating pain patterns, and the authors comment that symptoms frequently last for three months or longer with a SCCP.
Impressive?
Might I point out that what is being described here looks to me very much like the natural history of lumbar radiculopathy? About 90% of patients with back pain caused by disc herniation see improvements within three months without therapy. Are the authors aware that their observational study is in accordance with the notion that the SCCP does nothing or very little to help patients suffering from lumbar radiculopathy?
Infant colic is a sensitive subject for chiropractors in the UK. In case you forgot, here is why. Consequently, the subject has featured regularly on this blog – and now there is new evidence:
A systematic review and meta-analysis were conducted on infantile colic studies that used SO-CALLED alternative medicine (SCAM) techniques as interventions. The outcome measures were hours spent crying and/or sleeping. The authors used the PubMed, Physiotherapy Evidence Database, Cochrane Library, Embase, Web of Science, Scopus, Osteopathic Medicine Digital Database, and Google Scholar databases from inception to 11 November 2022.
The methodological quality of the randomized control trials ranged from fair to high. The authors focused on five studies with 422 babies using the following interventions: cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization. These treatments failed to decrease the crying time (mean difference -1.08, 95% CI -2.17 to 0.01, I2 = 92%) and to increase the sleeping time (mean difference 1.11, 95% CI -0.20 to 2.41; I2: 91%), compared with no intervention. The quality of the evidence was rated as very low for both outcome measures.The authors concluded that osteopathy and chiropractic treatment failed to reduce the crying time and increase sleeping time in babies with infantile colic, compared to no additional intervention.The 5 included studies were the following:
- Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: A pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther. 2012;35(8):600–7.
- Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. A randomized controlled trial. Complement Ther Med. 2022;71(February 2021).
- Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child. 2001;84(2):138–41.
- Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Ther. 2021;29(1):1–11.
- Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract. 2006;12(2):83–90.
This means that, in recent years, several new studies have emerged. I find this surprising: there is no plausible mechanism of action and the previous reviews were negative.
Why flog a dead horse?
But – come to think of it – this is a question one might ask about most of the research into cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization.
Low back pain is the leading cause of years lived with disability globally, but most interventions have only short-lasting, small to moderate effects. Cognitive functional therapy (CFT) is an individualized approach that targets unhelpful pain-related cognitions, emotions, and behaviors that contribute to pain and disability. Movement sensor biofeedback might enhance treatment effects.
This study aimed to compare the effectiveness and economic efficiency of CFT, delivered with or without movement sensor biofeedback, with usual care for patients with chronic, disabling low back pain.
RESTORE was a randomized, three-arm, parallel-group, phase 3 trial, done in 20 primary care physiotherapy clinics in Australia. The researchers recruited adults (aged ≥18 years) with low back pain lasting more than 3 months with at least moderate pain-related physical activity limitation. Exclusion criteria were serious spinal pathology (eg, fracture, infection, or cancer), any medical condition that prevented being physically active, being pregnant or having given birth within the previous 3 months, inadequate English literacy for the study’s questionnaires and instructions, a skin allergy to hypoallergenic tape adhesives, surgery scheduled within 3 months, or an unwillingness to travel to trial sites. Participants were randomly assigned (1:1:1) via a centralized adaptive schedule to
- usual care,
- CFT only,
- CFT plus biofeedback.
The primary clinical outcome was activity limitation at 13 weeks, self-reported by participants using the 24-point Roland Morris Disability Questionnaire. The primary economic outcome was quality-adjusted life-years (QALYs). Participants in both interventions received up to seven treatment sessions over 12 weeks plus a booster session at 26 weeks. Physiotherapists and patients were not masked.
Between Oct 23, 2018, and Aug 3, 2020, the researchers assessed 1011 patients for eligibility. After excluding 519 (51·3%) ineligible patients, they randomly assigned 492 (48·7%) participants; 164 (33%) to CFT only, 163 (33%) to CFT plus biofeedback, and 165 (34%) to usual care. Both interventions were more effective than usual care (CFT only mean difference –4·6 [95% CI –5·9 to –3·4] and CFT plus biofeedback mean difference –4·6 [–5·8 to –3·3]) for activity limitation at 13 weeks (primary endpoint). Effect sizes were similar at 52 weeks. Both interventions were also more effective than usual care for QALYs, and much less costly in terms of societal costs (direct and indirect costs and productivity losses; –AU$5276 [–10 529 to –24) and –8211 (–12 923 to –3500).
The authors concluded that CFT can produce large and sustained improvements for people with chronic disabling low back pain at considerably lower societal cost than that of usual care.
This is a well-designed and well-reported study. It shows that CFT is better than usual care. The effect sizes are not huge and seem similar to many other treatments for chronic LBP, including the numerous so-called alternative medicine (SCAM) options that are available.
Faced with a situation where we have virtually dozens of therapies of similar effectiveness, what should we recommend to patients? I think this question is best and most ethically answered by accounting for two other important determinants of usefulness:
- risk
- cost.
CFT is both low in risk and cost. So is therapeutic exercise. We would therefore need a direct comparison of the two to decide which is the optimal approach.
Until we have such a study, patients might just opt for one or both of them. What seems clear, meanwhile, is this: SCAM does not offer the best solution to chronic LBP. In particular, chiropractic, osteopathy, or acupuncture – which are neither low-cost nor risk-free – are, contrary to what some try so very hard to convince us of, sensible options.