spinal manipulation
Mr William Harvey Lillard was the janitor contracted to clean the Ryan Building where D. D. Palmer’s magnetic healing office was located. In 1895, he became Palmer’s very first chiropractic patient and thus entered the history books. The very foundations of chiropractic are based on this story.
[Testimony of Harvey Lillard regarding the events surrounding the first chiropractic adjustment, printed in the January 1897 issue of the Chiropractor]To call the ‘Chiropractor’ a reliable source would probably be stretching it a bit, and there are various versions of the event, even one where BJ Palmer, DD’s son, changed significant details of the story. Nevertheless, it’s a nice story, if there ever was one. But, like many nice stories, it’s just that: a tall tale, a story that might be not based on reality. In this case, the reality getting in the way of a good story is human anatomy.
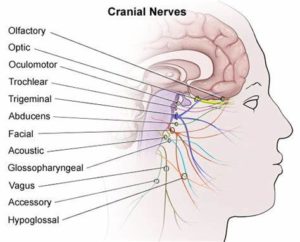
The nerve supply of the inner ear, the bit that enables us to hear, does not, like most other nerves of our body, run through the spine; it comes directly from the brain: the acoustic nerve is one of the 12 cranial nerves.
But chiropractors never let the facts get in the way of a good story! Thus they still tell it and presumably even believe it. Take this website, for instance, as an example of hundreds of similar sources:
… the very first chiropractic patient in history was named William Harvey Lillard, who experienced difficulty hearing due to compression of the nerves leading to his ears. He was treated by “the founder of chiropractic care,” David. D. Palmer, who gave Lillard spinal adjustments in order to reduce destructive nerve compressions and restore his hearing. After doing extensive research about physiology, Palmer believed that Lillard’s hearing loss was due to a misalignment that blocked the spinal nerves that controlled the inner ear (an example of vertebral subluxation). Palmer went on to successfully treat other patients and eventually trained other practitioners how to do the same.
How often have we been told that chiropractors receive a medical training that is at least as thorough as that of proper doctors? But that’s just another tall story, I guess.
Here is the abstract of a paper that makes even the most senior assessor of quackery shudder:
Objective:
The purpose of this report is to describe the manipulation under anesthesia (MUA) treatment of 6 infants with newborn torticollis with a segmental dysfunction at C1/C2.
Clinical Features:
Six infants aged 4 1/2 to 15 months previously diagnosed with newborn torticollis were referred to a doctor of chiropractic owing to a failure to respond adequately to previous conservative therapies. Common physical findings were limited range of motion of the upper cervical spine. Radiographs demonstrated rotational malpositions and translation of atlas on axis in all 6 infants, and 1 had a subluxation of the C1/C2 articulation.
Interventions and Outcome:
Selection was based on complexity and variety of different clinical cases qualifying for MUA. Treatment consisted of 1 mobilization and was performed in the operating room of a children’s hospital by a certified chiropractic physician with the author assisting. Along with the chiropractor and his assistant, a children’s anesthesiologist, 1 to 2 operating nurses, a children’s radiologist, and in 1 case a pediatric surgeon were present. Before the mobilization, plain radiographs of the cervico-occipital area were taken. Three infants needed further investigation by a pediatric computed tomography scan of the area because of asymmetric bony conditions on the plain radiographs. Follow-up consultations at 2, 3, 5, or 6 weeks were done. Patient records were analyzed for restriction at baseline before MUA compared with after MUA treatment for active rotation, passive rotation, and passive rotation in full flexion of the upper cervical spine. All 3 measurements showed significant differences. The long-term outcome data was collected via phone calls to the parents at 6 to 72 months. The initial clinical improvements were maintained.
Conclusion:
These 6 infants with arthrogenic newborn torticollis, who did not respond to previous conservative treatment methods, responded to MUA.
___________________________________________________________________
After reading the full text, I see many very serious problems and questions with this paper; here are 14 of the most obvious ones.
1. A congenital torticollis (that’s essentially what these kids were suffering from) has a good prognosis and does not require such invasive treatments. There is thus no plausible reason to conduct a case series of this nature.
2. A retrospective case series does not allow conclusions about therapeutic effectiveness, yet in the article the author does just that.
3. The same applies to her conclusions about the safety of the interventions.
4. It is unclear how the 6 cases were selected; it seems possible or even likely that they are, in fact, 6 cases of many more treated over a long period of time.
5. If so, this paper is hardly a ‘retrospective case series’; at best it could be called a ‘best case series’.
6. The X-rays or CT scans are unnecessary and potentially harmful.
7. The anaesthesia is potentially very harmful and unjustifiable.
8. The outcome measure is unreliable, particularly if performed by the chiropractor who has a vested interest in generating a positive result.
9. The follow-up by telephone is inadequate.
10. The range of the follow-up period (6-72 months) is unacceptable.
11. The exact way in which informed consent was obtained is unclear. In particular, we would need to know whether the parents were fully informed about the futility of the treatment and its considerable risks.
12. The chiropractor who administered the treatments is not named. Why not?
13. Similarly, it is unclear why the other healthcare professionals involved in these treatments are not named as co-authors of the paper.
14. It is unclear whether ethical approval was obtained for these treatments.
The author seems inexperienced in publishing scientific articles; the present one is poorly written and badly constructed. A Medline research reveals that she has only one other publication to her name. So, perhaps one should not be too harsh in judging her. But what about her supervisors, the journal, its reviewers, its editor and the author’s institution? The author comes from the Department of Chiropractic Medicine, Medical Faculty University, Zurich, Switzerland. On their website, they state:
The Faculty of Medicine of the University of Zurich is committed to high quality teaching and continuing research-based education of students in health care professions. Excellent and internationally recognised scientists and clinically outstanding physicians are at the Faculty of Medicine devoted to patients and public health, to teaching, to the support of young researchers and to academic medicine. The interaction between research and teaching, and their connection to clinical practice play a central role for us…
The Faculty of Medicine of the University of Zurich promotes innovative research in the basic fields of medicine, in the clinical application of knowledge, in personalised medicine, in health care, and in the translational connection between all these research areas. In addition, it encourages the cooperation between primary care and specialised health care.
It seems that, with the above paper, the UZH must have made an exception. In my view, it is a clear case of scientific misconduct and child abuse.
I am being told to educate myself and rethink the subject of NAPRAPATHY by the US naprapath Dr Charles Greer. Even though he is not very polite, he just might have a point:
Edzard, enough foolish so-called scientific, educated assesments from a trained Allopathic Physician. When asked, everything that involves Alternative Medicine in your eyesight is quackery. Fortunately, every Medically trained Allopathic Physician does not have your points of view. I have partnered with Orthopaedic Surgeons, Medical Pain Specialists, General practitioners, Thoracic Surgeons, Forensic Pathologists and Others during the course, whom appreciate the Services that Naprapaths provide. Many of my current patients are Medical Physicians. Educate yourself. Visit a Naprapath to learn first hand. I expect your outlook will certainly change.
I have to say, I am not normally bowled over by anyone who calls me an ‘allopath’ (does Greer not know that Hahnemann coined this term to denigrate his opponents? Is he perhaps also in favour of homeopathy?). But, never mind, perhaps I was indeed too harsh on naprapathy in my previous post on this subject.
So, let’s try again.
Just to remind you, naprapathy was developed by the chiropractor Oakley Smith who had graduated under D D Palmer in 1899. Smith was a former Iowa medical student who also had investigated Andrew Still’s osteopathy in Kirksville, before going to Palmer in Davenport. Eventually, Smith came to reject Palmer’s concept of vertebral subluxation and developed his own concept of “the connective tissue doctrine” or naprapathy.
Dr Geer published a short article explaining the nature of naprapathy:
Naprapathy- A scientific, Evidence based, integrative, Alternative form of Pain management and nutritional assessment that involves evaluation and treatment of Connective tissue abnormalities manifested in the entire human structure. This form of Therapeutic Regimen is unique specifically to the Naprapathic Profession. Doctors of Naprapathy, pronounced ( nuh-prop-a-thee) also referred to as Naprapaths or Neuromyologists, focus on the study of connective tissue and the negative factors affecting normal tissue. These factors may begin from external sources and latently produce cellular changes that in turn manifest themselves into structural impairments, such as irregular nerve function and muscular contractures, pulling its’ bony attachments out of proper alignment producing nerve irritability and impaired lymphatic drainage. These abnormalities will certainly produce a pain response as well as swelling and tissue congestion. Naprapaths, using their hands, are trained to evaluate tissue tension findings and formulate a very specific treatment regimen which produces positive results as may be evidenced in the patients we serve. Naprapaths also rely on information obtained from observation, hands on physical examination, soft tissue Palpatory assessment, orthopedic evaluation, neurological assessment linked with specific bony directional findings, blood and urinalysis laboratory findings, diet/ Nutritional assessment, Radiology test findings, and other pertinent clinical data whose information is scrutinized and developed into a individualized and specific treatment plan. The diagnostic findings and results produced reveal consistent facts and are totally irrefutable. The deductions that formulated these concepts of theory of Naprapathic Medicine are rationally believable, and have never suffered scientific contradiction. Discover Naprapathic Medicine, it works.
What interests me most here is that naprapathy is evidence-based. Did I perhaps miss something? As I cannot totally exclude this possibility, I did another Medline search. I found several trials:
1st study (2007)
Four hundred and nine patients with pain and disability in the back or neck lasting for at least 2 weeks, recruited at 2 large public companies in Sweden in 2005, were included in this randomized controlled trial. The 2 interventions were naprapathy, including spinal manipulation/mobilization, massage, and stretching (Index Group) and support and advice to stay active and how to cope with pain, according to the best scientific evidence available, provided by a physician (Control Group). Pain, disability, and perceived recovery were measured by questionnaires at baseline and after 3, 7, and 12 weeks.
RESULTS:
At 7-week and 12-week follow-ups, statistically significant differences between the groups were found in all outcomes favoring the Index Group. At 12-week follow-up, a higher proportion in the naprapathy group had improved regarding pain [risk difference (RD)=27%, 95% confidence interval (CI): 17-37], disability (RD=18%, 95% CI: 7-28), and perceived recovery (RD=44%, 95% CI: 35-53). Separate analysis of neck pain and back pain patients showed similar results.
DISCUSSION:
This trial suggests that combined manual therapy, like naprapathy, might be an alternative to consider for back and neck pain patients.
2nd study (2010)
Subjects with non-specific pain/disability in the back and/or neck lasting for at least two weeks (n = 409), recruited at public companies in Sweden, were included in this pragmatic randomized controlled trial. The two interventions compared were naprapathic manual therapy such as spinal manipulation/mobilization, massage and stretching, (Index Group), and advice to stay active and on how to cope with pain, provided by a physician (Control Group). Pain intensity, disability and health status were measured by questionnaires.
RESULTS:
89% completed the 26-week follow-up and 85% the 52-week follow-up. A higher proportion in the Index Group had a clinically important decrease in pain (risk difference (RD) = 21%, 95% CI: 10-30) and disability (RD = 11%, 95% CI: 4-22) at 26-week, as well as at 52-week follow-ups (pain: RD = 17%, 95% CI: 7-27 and disability: RD = 17%, 95% CI: 5-28). The differences between the groups in pain and disability considered over one year were statistically significant favoring naprapathy (p < or = 0.005). There were also significant differences in improvement in bodily pain and social function (subscales of SF-36 health status) favoring the Index Group.
CONCLUSIONS:
Combined manual therapy, like naprapathy, is effective in the short and in the long term, and might be considered for patients with non-specific back and/or neck pain.
3rd study (2016)
Participants were recruited among patients, ages 18-65, seeking care at the educational clinic of Naprapathögskolan – the Scandinavian College of Naprapathic Manual Medicine in Stockholm. The patients (n = 1057) were randomized to one of three treatment arms a) manual therapy (i.e. spinal manipulation, spinal mobilization, stretching and massage), b) manual therapy excluding spinal manipulation and c) manual therapy excluding stretching. The primary outcomes were minimal clinically important improvement in pain intensity and pain related disability. Treatments were provided by naprapath students in the seventh semester of eight total semesters. Generalized estimating equations and logistic regression were used to examine the association between the treatments and the outcomes.
RESULTS:
At 12 weeks follow-up, 64% had a minimal clinically important improvement in pain intensity and 42% in pain related disability. The corresponding chances to be improved at the 52 weeks follow-up were 58% and 40% respectively. No systematic differences in effect when excluding spinal manipulation and stretching respectively from the treatment were found over 1 year follow-up, concerning minimal clinically important improvement in pain intensity (p = 0.41) and pain related disability (p = 0.85) and perceived recovery (p = 0.98). Neither were there disparities in effect when male and female patients were analyzed separately.
CONCLUSION:
The effect of manual therapy for male and female patients seeking care for neck and/or back pain at an educational clinic is similar regardless if spinal manipulation or if stretching is excluded from the treatment option.
_________________________________________________________________
I don’t know about you, but I don’t call this ‘evidence-based’ – especially as all the three trials come from the same research group (no, not Greer; he seems to have not published at all on naprapathy). Dr Greer does clearly not agree with my assessment; on his website, he advertises treating the following conditions:
Anxiety
Back Disorders
Back Pain
Cervical Radiculopathy
Cervical Spondylolisthesis
Cervical Sprain
Cervicogenic Headache
Chronic Headache
Chronic Neck Pain
Cluster Headache
Cough Headache
Depressive Disorders
Fibromyalgia
Headache
Hip Arthritis
Hip Injury
Hip Muscle Strain
Hip Pain
Hip Sprain
Joint Clicking
Joint Pain
Joint Stiffness
Joint Swelling
Knee Injuries
Knee Ligament Injuries
Knee Sprain
Knee Tendinitis
Lower Back Injuries
Lumbar Herniated Disc
Lumbar Radiculopathy
Lumbar Spinal Stenosis
Lumbar Sprain
Muscle Diseases
Musculoskeletal Pain
Neck Pain
Sciatica (Not Due to Disc Displacement)
Sciatica (Not Due to Disc Displacement)
Shoulder Disorders
Shoulder Injuries
Shoulder Pain
Sports Injuries
Sports Injuries of the Knee
Stress
Tendonitis
Tennis Elbow (Lateral Epicondylitis)
Thoracic Disc Disorders
Thoracic Outlet Syndrome
Toe Injuries
Odd, I’d say! Did all this change my mind about naprapathy? Not really.
But nobody – except perhaps Dr Greer – can say I did not try.
And what light does this throw on Dr Greer and his professionalism? Since he seems to be already quite mad at me, I better let you answer this question.
 Chiropractic may be nonsense, but it nevertheless earns chiros very good money. Chiropractors tend to treat their patients for unnecessarily long periods of time. This, of course, costs money, and even if the treatment in question ever was indicated (which, according to the best evidence, is more than doubtful), this phenomenon would significantly inflate healthcare expenditure. It was reported that over 80% of the money that the US Medicare paid to chiropractors in 2013 went for medically unnecessary procedures. The federal insurance program for senior citizens thus spent roughly $359 million on unnecessary chiropractic care that year.
Chiropractic may be nonsense, but it nevertheless earns chiros very good money. Chiropractors tend to treat their patients for unnecessarily long periods of time. This, of course, costs money, and even if the treatment in question ever was indicated (which, according to the best evidence, is more than doubtful), this phenomenon would significantly inflate healthcare expenditure. It was reported that over 80% of the money that the US Medicare paid to chiropractors in 2013 went for medically unnecessary procedures. The federal insurance program for senior citizens thus spent roughly $359 million on unnecessary chiropractic care that year.
Such expenditure may not benefit patients, but it surely benefits the chiropractors. A recent article in Forbes informed us that, according to the US Bureau of Labor Statistics’ Occupational Outlook Handbook, the employment of chiropractors is expected to grow 12% from 2016 to 2026, faster than the average for all occupations.
According to the latest data from the Bureau Occupational Employment Statistics, as of 2017, the average income of an US chiropractor amounts to US $ 85,870. However, chiropractors’ salaries aren’t this high in every US state. The lowest average income (US$ 45 000) per year is in the state of Wyoming.
Below you’ll find a breakdown of where chiropractors’ incomes are the highest.
| 1 | Rhode Island | $147,900 |
| 2 | Tennessee | $122,620 |
| 3 | Connecticut | $113,130 |
| 4 | Alaska | $106,600 |
| 5 | Colorado | $99,350 |
| 6 | New Hampshire | $99,330 |
| 7 | Nevada | $99,140 |
| 8 | Delaware | $97,650 |
| 9 | Massachusetts | $96,110 |
| 10 | Maryland | $95,190 |
These are tidy sums indeed – remember, they merely depict the averages. Individual chiropractors will earn substantially more than the average, of course. And there are hundreds of websites, books, etc. to teach chiros how to maximise their cash-flow. Some of the most popular ‘tricks of the chiro trade’ include:
- maintenance therapy,
- treatment of children,
- making unsupported therapeutic claims,
- disregarding the risks of spinal manipulation,
- selling useless dietary supplements.
Considering the sums of money that are at stake, I am beginning to understand why chiropractors tend to get so nervous, often even furious and aggressive, when I point out that they might be causing more harm than good to their patients.
Its the money, stupid!
An impressive 17% of US chiropractic patients are 17 years of age or younger. This figure increases to 39% among US chiropractors who have specialized in paediatrics. Data for other countries can be assumed to be similar. But is chiropractic effective for children? All previous reviews concluded that there is a paucity of evidence for the effectiveness of manual therapy for conditions within paediatric populations.
This systematic review is an attempt to shed more light on the issue by evaluating the use of manual therapy for clinical conditions in the paediatric population, assessing the methodological quality of the studies found, and synthesizing findings based on health condition.
Of the 3563 articles identified through various literature searches, 165 full articles were screened, and 50 studies (32 RCTs and 18 observational studies) met the inclusion criteria. Only 18 studies were judged to be of high quality. Conditions evaluated were:
- attention deficit hyperactivity disorder (ADHD),
- autism,
- asthma,
- cerebral palsy,
- clubfoot,
- constipation,
- cranial asymmetry,
- cuboid syndrome,
- headache,
- infantile colic,
- low back pain,
- obstructive apnoea,
- otitis media,
- paediatric dysfunctional voiding,
- paediatric nocturnal enuresis,
- postural asymmetry,
- preterm infants,
- pulled elbow,
- suboptimal infant breastfeeding,
- scoliosis,
- suboptimal infant breastfeeding,
- temporomandibular dysfunction,
- torticollis,
- upper cervical dysfunction.
Musculoskeletal conditions, including low back pain and headache, were evaluated in seven studies. Only 20 studies reported adverse events.
The authors concluded that fifty studies investigated the clinical effects of manual therapies for a wide variety of pediatric conditions. Moderate-positive overall assessment was found for 3 conditions: low back pain, pulled elbow, and premature infants. Inconclusive unfavorable outcomes were found for 2 conditions: scoliosis (OMT) and torticollis (MT). All other condition’s overall assessments were either inconclusive favorable or unclear. Adverse events were uncommonly reported. More robust clinical trials in this area of healthcare are needed.
There are many things that I find remarkable about this review:
- The list of indications for which studies have been published confirms the notion that manual therapists – especially chiropractors – regard their approach as a panacea.
- A systematic review evaluating the effectiveness of a therapy that includes observational studies without a control group is, in my view, highly suspect.
- Many of the RCTs included in the review are meaningless; for instance, if a trial compares the effectiveness of two different manual therapies none of which has been shown to work, it cannot generate a meaningful result.
- Again, we find that the majority of trialists fail to report adverse effects. This is unethical to a degree that I lose faith in such studies altogether.
- Only three conditions are, according to the authors, based on evidence. This is hardly enough to sustain an entire speciality of paediatric chiropractors.
Allow me to have a closer look at these three conditions.
- Low back pain: the verdict ‘moderate positive’ is based on two RCTs and two observational studies. The latter are irrelevant for evaluating the effectiveness of a therapy. One of the two RCTs should have been excluded because the age of the patients exceeded the age range named by the authors as an inclusion criterion. This leaves us with one single ‘medium quality’ RCT that included a mere 35 patients. In my view, it would be foolish to base a positive verdict on such evidence.
- Pulled elbow: here the verdict is based on one RCT that compared two different approaches of unknown value. In my view, it would be foolish to base a positive verdict on such evidence.
- Preterm: Here we have 4 RCTs; one was a mere pilot study of craniosacral therapy following the infamous A+B vs B design. The other three RCTs were all from the same Italian research group; their findings have never been independently replicated. In my view, it would be foolish to base a positive verdict on such evidence.
So, what can be concluded from this?
I would say that there is no good evidence for chiropractic, osteopathic or other manual treatments for children suffering from any condition.
And why do the authors of this new review arrive at such dramatically different conclusion? I am not sure. Could it perhaps have something to do with their affiliations?
- Palmer College of Chiropractic,
- Canadian Memorial Chiropractic College,
- Performance Chiropractic.
What do you think?
A new update of the current Cochrane review assessed the benefits and harms of spinal manipulative therapy (SMT) for the treatment of chronic low back pain. The authors included all randomised controlled trials (RCTs) examining the effect of spinal manipulation or mobilisation in adults (≥18 years) with chronic low back pain with or without referred pain. Studies that exclusively examined sciatica were excluded.
The effect of SMT was compared with recommended therapies, non-recommended therapies, sham (placebo) SMT, and SMT as an adjuvant therapy. Main outcomes were pain and back specific functional status, examined as mean differences and standardised mean differences (SMD), respectively. Outcomes were examined at 1, 6, and 12 months.
Forty-seven RCTs including a total of 9211 participants were identified. Most trials compared SMT with recommended therapies. In 16 RCTs, the therapists were chiropractors, in 14 they were physiotherapists, and in 5 they were osteopaths. They used high velocity manipulations in 18 RCTs, low velocity manipulations in 12 studies and a combination of the two in 20 trials.
Moderate quality evidence suggested that SMT has similar effects to other recommended therapies for short term pain relief and a small, clinically better improvement in function. High quality evidence suggested that, compared with non-recommended therapies, SMT results in small, not clinically better effects for short term pain relief and small to moderate clinically better improvement in function.
In general, these results were similar for the intermediate and long term outcomes as were the effects of SMT as an adjuvant therapy.
Low quality evidence suggested that SMT does not result in a statistically better effect than sham SMT at one month. Additionally, very low quality evidence suggested that SMT does not result in a statistically better effect than sham SMT at six and 12 months. Low quality evidence suggested that SMT results in a moderate to strong statistically significant and clinically better effect than sham SMT at one month. Additionally, very low quality evidence suggested that SMT does not result in a statistically significant better effect than sham SMT at six and 12 months.
(Mean difference in reduction of pain at 1, 3, 6, and 12 months (0-100; 0=no pain, 100 maximum pain) for spinal manipulative therapy (SMT) versus recommended therapies in review of the effects of SMT for chronic low back pain. Pooled mean differences calculated by DerSimonian-Laird random effects model.)
About half of the studies examined adverse and serious adverse events, but in most of these it was unclear how and whether these events were registered systematically. Most of the observed adverse events were musculoskeletal related, transient in nature, and of mild to moderate severity. One study with a low risk of selection bias and powered to examine risk (n=183) found no increased risk of an adverse event or duration of the event compared with sham SMT. In one study, the Data Safety Monitoring Board judged one serious adverse event to be possibly related to SMT.
The authors concluded that SMT produces similar effects to recommended therapies for chronic low back pain, whereas SMT seems to be better than non-recommended interventions for improvement in function in the short term. Clinicians should inform their patients of the potential risks of adverse events associated with SMT.
This paper is currently being celebrated (mostly) by chiropractors who think that it vindicates their treatments as being both effective and safe. However, I am not sure that this is entirely true. Here are a few reasons for my scepticism:
- SMT is as good as other recommended treatments for back problems – this may be so but, as no good treatment for back pain has yet been found, this really means is that SMT is as BAD as other recommended therapies.
- If we have a handful of equally good/bad treatments, it stand to reason that we must use other criteria to identify the one that is best suited – criteria like safety and cost. If we do that, it becomes very clear that SMT cannot be named as the treatment of choice.
- Less than half the RCTs reported adverse effects. This means that these studies were violating ethical standards of publication. I do not see how we can trust such deeply flawed trials.
- Any adverse effects of SMT were minor, restricted to the short term and mainly centred on musculoskeletal effects such as soreness and stiffness – this is how some naïve chiro-promoters already comment on the findings of this review. In view of the fact that more than half the studies ‘forgot’ to report adverse events and that two serious adverse events did occur, this is a misleading and potentially dangerous statement and a good example how, in the world of chiropractic, research is often mistaken for marketing.
- Less than half of the studies (45% (n=21/47)) used both an adequate sequence generation and an adequate allocation procedure.
- Only 5 studies (10% (n=5/47)) attempted to blind patients to the assigned intervention by providing a sham treatment, while in one study it was unclear.
- Only about half of the studies (57% (n=27/47)) provided an adequate overview of withdrawals or drop-outs and kept these to a minimum.
- Crucially, this review produced no good evidence to show that SMT has effects beyond placebo. This means the modest effects emerging from some trials can be explained by being due to placebo.
- The lead author of this review (SMR), a chiropractor, does not seem to be free of important conflicts of interest: SMR received personal grants from the European Chiropractors’ Union (ECU), the European Centre for Chiropractic Research Excellence (ECCRE), the Belgian Chiropractic Association (BVC) and the Netherlands Chiropractic Association (NCA) for his position at the Vrije Universiteit Amsterdam. He also received funding for a research project on chiropractic care for the elderly from the European Centre for Chiropractic Research and Excellence (ECCRE).
- The second author (AdeZ) who also is a chiropractor received a grant from the European Chiropractors’ Union (ECU), for an independent study on the effects of SMT.
After carefully considering the new review, my conclusion is the same as stated often before: SMT is not supported by convincing evidence for back (or other) problems and does not qualify as the treatment of choice.
Osteopathy is a tricky subject:
- Osteopathic manipulations/mobilisations are advocated mainly for spinal complaints.
- Yet many osteopaths use them also for a myriad of non-spinal conditions.
- Osteopathy comprises two entirely different professions; in the US, osteopaths are very similar to medically trained doctors, and many hardly ever employ osteopathic manual techniques; outside the US, osteopaths are alternative practitioners who use mainly osteopathic techniques and believe in the obsolete gospel of their guru Andrew Taylor Still (this post relates to the latter type of osteopathy).
- The question whether osteopathic manual therapies are effective is still open – even for the indication that osteopaths treat most, spinal complaints.
- Like chiropractors, osteopaths now insist that osteopathy is not a treatment but a profession; the transparent reason for this argument is to gain more wriggle-room when faced with negative evidence regarding they hallmark treatment of osteopathic manipulation/mobilisation.
A new paper authored by osteopaths is an attempt to shed more light on the effectiveness of osteopathy. The aim of this systematic review evaluated the impact of osteopathic care for spinal complaints. Only randomized controlled trials conducted in high-income Western countries were considered. Two authors independently screened the titles and abstracts. Primary outcomes included ‘pain’ and ‘functional status’, while secondary outcomes included ‘medication use’ and ‘health status’.
Nineteen studies were included and qualitatively synthesized. Nine studies were from the US, followed by Germany with 7 studies. The majority of studies (n = 13) focused on low back pain.
In general, mixed findings related to the impact of osteopathic care on primary and secondary outcomes were observed. For the primary outcomes, a clear distinction between US and European studies was found, where the latter RCTs reported positive results more frequently. Studies were characterized by substantial methodological differences in sample sizes, number of treatments, control groups, and follow-up.
The authors concluded that “the findings of the current literature review suggested that osteopathic care may improve pain and functional status in patients suffering from spinal complaints. A clear distinction was observed between studies conducted in the US and those in Europe, in favor of the latter. Today, no clear conclusions of the impact of osteopathic care for spinal complaints can be drawn. Further studies with larger study samples also assessing the long-term impact of osteopathic care for spinal complaints are required to further strengthen the body of evidence.”
Some of the most obvious weaknesses of this review include the following:
- In none of the studies employed blinding of patients, care provider or outcome assessor occurred, or it was unclear. Blinding of outcome assessors is easily implemented and should be standard in any RCT.
- In three studies, the study groups differed to some extent at baseline indicating that randomisation was not successful..
- Five studies were derived from the ‘grey literature’ and were therefore not peer-reviewed.
- One study (the UK BEAM trial) employed not just osteopaths but also chiropractors and physiotherapists for administering the spinal manipulations. It is therefore hardly an adequate test of osteopathy.
- The study was funded by an unrestricted grant from the GNRPO, the umbrella organization of the ‘Belgian Professional Associations for Osteopaths’.
Considering this last point, the authors’ honesty in admitting that no clear conclusions of the impact of osteopathic care for spinal complaints can be drawn is remarkable and deserves praise.
Considering that the evidence for osteopathy is even far worse for non-spinal conditions (numerous trials exist for all sorts of other conditions, but they tend to be flimsy and usually lack independent replications), it is fair to conclude that osteopathy is NOT an evidence-based therapy.
Excellent journals always publish excellent science!
If this is what you believe, you might want to read a study of chiropractic just published in the highly respected SCIENTIFIC REPORTS.
The objective of this study was to investigate whether a single session of chiropractic care could increase strength in weak plantar flexor muscles in chronic stroke patients. Maximum voluntary contractions (strength) of the plantar flexors, soleus evoked V-waves (cortical drive), and H-reflexes were recorded in 12 chronic stroke patients, with plantar flexor muscle weakness, using a randomized controlled crossover design. Outcomes were assessed pre and post a chiropractic care intervention and a passive movement control. Repeated measures ANOVA was used to asses within and between group differences. Significance was set at p < 0.05. Following the chiropractic care intervention there was a significant increase in strength (F (1,11) = 14.49, p = 0.002; avg 64.2 ± 77.7%) and V-wave/Mmax ratio (F(1,11) = 9.67, p = 0.009; avg 54.0 ± 65.2%) compared to the control intervention. There was a significant strength decrease of 26.4 ± 15.5% (p = 0.001) after the control intervention. There were no other significant differences. Plantar flexor muscle strength increased in chronic stroke patients after a single session of chiropractic care. An increase in V-wave amplitude combined with no significant changes in H-reflex parameters suggests this increased strength is likely modulated at a supraspinal level. Further research is required to investigate the longer term and potential functional effects of chiropractic care in stroke recovery.
In the article we find the following further statements (quotes in bold, followed by my comments in normal print):
- Data were collected by a team of researchers from the Centre for Chiropractic Research at the New Zealand College of Chiropractic. These researchers can be assumed to be highly motivated in generating a positive finding.
- The entire spine and both sacroiliac joints were assessed for vertebral subluxations, and chiropractic adjustments were given where deemed necessary, by a New Zealand registered chiropractor. As there is now near-general agreement that such subluxations are a myth, the researchers treated a non-existing entity.
- The chiropractor did not contact on a segment deemed to be subluxated during the control set-up and no adjustive thrusts were applied during any control intervention. The patients therefore were clearly able to tell the difference between real and control treatments. Participants were not checked for blinding success.
- Maximum isometric plantarflexion force was measured using an isometric strain gauge. Such measurements crucially depend on the motivation of the patient.
- The grant proposal for this study was reviewed by the Australian Spinal Research Foundation to support facilitation of funding from the United Chiropractic Association. Does this not mean the researchers had a conflict of interest?
- The authors declare no competing interests. Really? They were ardent subluxationists supported by the United Chiropractic Association, an organisation stating that chiropractic is concerned with the preservation and restoration of health, and focuses particular attention on the subluxation, and subscribes to to the obsolete concept of vitalism: we ascribe to the idea that all living organisms are sustained by an innate intelligence, which is both different from and greater than physical and chemical forces. Further, we believe innate intelligence is an expression of universal intelligence.
So, in essence, what we have here is an under-powered study sponsored by vitalists and conducted by subluxationists treating a mythical entity with dubious interventions without controlling for patients’ expectation pretending their false-positive findings are meaningful.
I cannot help wondering what possessed the SCIENTIFIC REPORTS to publish such poor science.
So-called alternative medicine (SCAM) for animals is popular. A recent survey suggested that 76% of US dog and cat owners use some form of SCAM. Another survey showed that about one quarter of all US veterinary medical schools run educational programs in SCAM. Amazon currently offers more that 4000 books on the subject.
The range of SCAMs advocated for use in animals is huge and similar to that promoted for use in humans; the most commonly employed practices seem to include acupuncture, chiropractic, energy healing, homeopathy (as discussed in the previous post) and dietary supplements. In this article, I will briefly discuss the remaining 4 categories.
ACUPUNCTURE
Acupuncture is the insertion of needles at acupuncture points on the skin for therapeutic purposes. Many acupuncturists claim that, because it is over 2 000 years old, acupuncture has ‘stood the test of time’ and its long history proves acupuncture’s efficacy and safety. However, a long history of usage proves very little and might even just demonstrate that acupuncture is based on the pre-scientific myths that dominated our ancient past.
There are many different forms of acupuncture. Acupuncture points can allegedly be stimulated not just by inserting needles (the most common way) but also with heat, electrical currents, ultrasound, pressure, bee-stings, injections, light, colour, etc. Then there is body acupuncture, ear acupuncture and even tongue acupuncture. Traditional Chinese acupuncture is based on the Taoist philosophy of the balance between two life-forces, ‘yin and yang’. In contrast, medical acupuncturists tend to cite neurophysiological theories as to how acupuncture might work; even though some of these may appear plausible, they nevertheless are mere theories and constitute no proof for acupuncture’s validity.
The therapeutic claims made for acupuncture are legion. According to the traditional view, acupuncture is useful for virtually every condition. According to ‘Western’ acupuncturists, acupuncture is effective mostly for chronic pain. Acupuncture has, for instance, been used to improve mobility in dogs with musculoskeletal pain, to relieve pain associated with cervical neurological disease in dogs, for respiratory resuscitation of new-born kittens, and for treatment of certain immune-mediated disorders in small animals.
While the use of acupuncture seems to gain popularity, the evidence fails to support this. Our systematic review of acupuncture (to the best of my knowledge the only one on the subject) in animals included 14 randomized controlled trials and 17 non-randomized controlled studies. The methodologic quality of these trials was variable but, on average, it was low. For cutaneous pain and diarrhoea, encouraging evidence emerged that might warrant further investigation. Single studies reported some positive inter-group differences for spinal cord injury, Cushing’s syndrome, lung function, hepatitis, and rumen acidosis. However, these trials require independent replication. We concluded that, overall, there is no compelling evidence to recommend or reject acupuncture for any condition in domestic animals. Some encouraging data do exist that warrant further investigation in independent rigorous trials.
Serious complications of acupuncture are on record and have repeatedly been discussed on this blog: acupuncture needles can, for instance, injure vital organs like the lungs or the heart, and they can introduce infections into the body, e. g. hepatitis. About 100 human fatalities after acupuncture have been reported in the medical literature – a figure which, due to lack of a monitoring system, may disclose just the tip of an iceberg. Information on adverse effects of acupuncture in animals is currently not available.
Given that there is no good evidence that acupuncture works in animals, the risk/benefit balance of acupuncture cannot be positive.
CHIROPRACTIC
Chiropractic was created by D D Palmer (1845-1913), an American magnetic healer who, in 1895, manipulated the neck of a deaf janitor, allegedly curing his deafness. Chiropractic was initially promoted as a cure-all by Palmer who claimed that 95% of diseases were due to subluxations of spinal joints. Subluxations became the cornerstone of chiropractic ‘philosophy’, and chiropractors who adhere to Palmer’s gospel diagnose subluxation in nearly 100% of the population – even in individuals who are completely disease and symptom-free. Yet subluxations, as understood by chiropractors, do not exist.
There is no good evidence that chiropractic spinal manipulation might be effective for animals. A review of the evidence for different forms of manual therapies for managing acute or chronic pain syndromes in horses concluded that further research is needed to assess the efficacy of specific manual therapy techniques and their contribution to multimodal protocols for managing specific somatic pain conditions in horses. For other animal species or other health conditions, the evidence is even less convincing.
In humans, spinal manipulation is associated with serious complications (regularly discussed in previous posts), usually caused by neck manipulation damaging the vertebral artery resulting in a stroke and even death. Several hundred such cases have been documented in the medical literature – but, as there is no system in place to monitor such events, the true figure is almost certainly much larger. To the best of my knowledge, similar events have not been reported in animals.
Since there is no good evidence that chiropractic spinal manipulations work in animals, the risk/benefit balance of chiropractic fails to be positive.
ENERGY HEALING
Energy healing is an umbrella term for a range of paranormal healing practices, e. g. Reiki, Therapeutic Touch, Johrei healing, faith healing. Their common denominator is the belief in an ‘energy’ that can be used for therapeutic purposes. Forms of energy healing have existed in many ancient cultures. The ‘New Age’ movement has brought about a revival of these ideas, and today ‘energy’ healing systems are amongst the most popular alternative therapies in many countries.
Energy healing relies on the esoteric belief in some form of ‘energy’ which refers to some life force such as chi in Traditional Chinese Medicine, or prana in Ayurvedic medicine. Some proponents employ terminology from quantum physics and other ‘cutting-edge’ science to give their treatments a scientific flair which, upon closer scrutiny, turns out to be little more than a veneer of pseudo-science.
Considering its implausibility, energy healing has attracted a surprisingly high level of research activity in the form of clinical trials on human patients. Generally speaking, the methodologically best trials of energy healing fail to demonstrate that it generates effects beyond placebo. There are few studies of energy healing in animals, and those that are available are frequently less than rigorous (see for instance here and here). Overall, there is no good evidence to suggest that ‘energy’ healing is effective in animals.
Even though energy healing is per se harmless, it can do untold damage, not least because it can lead to neglect of effective treatments and it undermines rationality in our societies. Its risk/benefit balance therefore fails to be positive.
DIETARY SUPPLEMENTS
Dietary supplements for veterinary use form a category of remedies that, in most countries, is a regulatory grey area. Supplements can contain all sorts of ingredients, from minerals and vitamins to plants and synthetic substances. Therefore, generalisations across all types of supplements are impossible. The therapeutic claims that are being made for supplements are numerous and often unsubstantiated. Although they are usually promoted as natural and safe, dietary supplements do not have necessarily either of these qualities. For example, in the following situations, supplements can be harmful:
- Combining one supplement with another supplement or with prescribed medicines
- Substituting supplements for prescription medicines
- Overdosing some supplements, such as vitamin A, vitamin D, or iron
Examples of currently most popular supplements for use in animals include chondroitin, glucosamine, probiotics, vitamins, minerals, lutein, L-carnitine, taurine, amino acids, enzymes, St John’s wort, evening primrose oil, garlic and many other herbal remedies. For many supplements taken orally, the bioavailability might be low. There is a paucity of studies testing the efficacy of dietary supplements in animals. Three recent exceptions (all of which require independent replication) are:
- A trial showing that the dietary supplementation with Maca increased sperm production in stallions.
- A study demonstrating that curcumin supplementation appeared to reduce arthritis pain in dogs.
- An investigation suggesting that royal jelly supplementation can improve the egg quality of hens.
Dietary supplements are promoted as being free of direct risks. On closer inspection, this notion turns out to be little more than an advertising slogan. As discussed repeatedly on this blog, some supplements contain toxic materials, contaminants or adulterants and thus have the potential to do harm. A report rightly concluded that many challenges stand in the way of determining whether or not animal dietary supplements are safe and at what dosage. Supplements considered safe in humans and other cross-species are not always safe in horses, dogs, and cats. An adverse event reporting system is badly needed. And finally, regulations dealing with animal dietary supplements are in disarray. Clear and precise regulations are needed to allow only safe dietary supplements on the market.
It is impossible to generalise about the risk/benefit balance of dietary supplements; however, caution is advisable.
CONCLUSION
SCAM for animals is an important subject, not least because of the current popularity of many treatments that fall under this umbrella. For most therapies, the evidence is woefully incomplete. This means that most SCAMs are unproven. Arguably, it is unethical to use unproven medicines in routine veterinary care.
PS
I was invited several months ago to write this article for VETERINARY RECORD. It was submitted to peer review and subsequently I withdrew my submission. The above post is a slightly revised version of the original (in which I used the term ‘alternative medicine’ rather than ‘SCAM’) which also included a section on homeopathy (see my previous post). The reason for the decision to withdraw this article was the following comment by the managing editor of VETERINARY RECORD: A good number of vets use these therapies and a more balanced view that still sets out their efficacy (or otherwise) would be more useful for the readership.
Pertussis (whooping-cough) is a serious condition. Today, we have vaccinations and antibiotics against it and therefore it is rarely a fatal disease. A century or so, the situation was different. Then all sorts of quacks claimed to be able to treat pertussis and many patients, particularly children, died.
This article starts with this amazing introduction: Osteopathic physicians may want to consider using osteopathic manipulative treatment (OMT) as an adjunctive treatment modality for pertussis; however, suitable OMT techniques are not specified in the research literature.
For the paper, the author then searched the historical osteopathic literature to identify OMT techniques that were used in the management of pertussis in the pre-antibiotic era. The 24 identified sources included 8 articles and 16 book contributions from the years 1886 to 1958. Most sources were published within the first quarter of the 20th century. Commonly identified OMT techniques included mobilization techniques, lymphatic pump techniques, and other manipulative techniques predominantly in the cervical and thoracic regions.
The author concluded that the wealth of OMT techniques for patients with pertussis that were identified suggests that pertussis was commonly treated by early osteopaths. Further research is necessary to identify or establish the evidence base for these techniques so that in case of favorable outcomes, their use by osteopathic physicians is justified as adjunctive modalities when encountering a patient with pertussis.
I found it hard to decide whether to laugh or to cry after reading this. One could easily have a good giggle about the silliness of the idea to revive obsolete techniques for treating a potentially serious infection. One the other hand, I cannot help but ask myself:
- Is there any suggestion at all that OMT was successful in treating pertussis?
- If the answer is negative (and I fear it is), why would anyone spend considerable resources to establish the evidence base for these techniques?
- Do osteopaths believe in progress at all?
- Do they really think that there is even a remote chance that mobilization techniques, lymphatic pump techniques, and other manipulative techniques will, one day, come back as adjunctive therapies for pertussis?
- Do they not believe in a rational approach to prioritising medical research such that scarce resources are spent ethically and wisely?
You may think that none of this really matters. The author of this paper is just a lone loon! That may well be so, but even lone loons can do a lot of harm, if they convince consumers of their bizarre ideas.
But surely, the profession of osteopathy would not tolerate this, you say. I am not convinced. The article was published in the Journal of the American Osteopathic Association. This seems significant to me. It is comparable to the JAMA or the BMJ publishing an article calling for a programme of research into the possible benefits of blood-letting as a treatment of pneumonia!