risk/benefit
The increasing demand for fertility treatments has led to the rise of private clinics offering so-called alternative medicine (SCAM) treatments. Even King Charles has recently joined in with this situalion. One of the most frequently offered SCAM infertility treatment is acupuncture. However, there is no good evidence to support the effectiveness of acupuncture in treating infertility.
This study evaluated the scope of information provided by SCAM fertility clinics in the UK. A content analysis was conducted on 200 websites of SCAM fertility clinics in the UK that offer acupuncture as a treatment for infertility. Of the 48 clinics that met the eligibility criteria, the majority of the websites did not provide sufficient information on:
- the efficacy,
- the risks,
- the success rates
of acupuncture for infertility.
The authors concluded that this situation has the potential to infringe on patient autonomy, provide false hope and reduce the chances of pregnancy ever being achieved as fertility declines during the time course of ineffective acupuncture treatment.
The authors are keen to point out that their investigation has certain limitations. The study only analysed the information provided on the clinics’ websites and did not assess the quality of the treatment provided by the clinics.
Therefore, the study’s fndings cannot be generalized to the quality of the acupuncture treatment provided by the clinics.
Nonetheless the paper touches on very important issues: far too many health clinics that offer SCAM for this or that indication operate way outside the ethically (and legally) acceptable norm. They advertise their services without making it clear that they are neither effective nor safe. Desperate consumers thus fall for their promises. In the case of infertility, this might result merely in frustration and loss of (often substantial amounts of) money. In the case of serious disease, such as cancer, this often results in premature death.
It is time, I think, that this entire sector is regualted in a way that it does not endanger the well-being, health, or life of consumers.
We discussed the 2015 Australian NHMRC report on homeopathy many times before, e.g.:
- Homeopathy: the 2015 NHMRC report and its criticism re-analysed
- HOMEOPATHY: the NHMRC report revisited
- Ombudsman investigates ‘flawed’ homeopathic study
- The final verdict on homeopathy: it’s a placebo
In a nutshell, the report was an hugely influential analysis of the effectiveness of homeopathy which came to squarely negative conclusions. Thus it was celebrated as a thorough and conclusive piece evidence demonstrating the madness of homeopathy. Unsurprisingly, homeopaths did not like it at all and produced various criticisms claiming that it was neither thorough nor conclusive.
Now the final evaluation of what has been going on was finally published (ISSUED BY THE COMMONWEALTH OMBUDSMAN, IAIN ANDERSON, ON 4 AUGUST 2023):
The Office of the Commonwealth Ombudsman (the Office) has finalised an investigation relating to the National Health and Medical Research Council’s (NHMRC) review of the evidence for the effectiveness of homeopathy, conducted between 2010 and 2015. We commenced this investigation in September 2017 in response to concerns raised with us about how the NHMRC review had proceeded.
The Office conducts its investigations in private, and the Ombudsman generally does not make a public statement in the absence of a formal report. In the circumstances of this matter, including that the then-Ombudsman released a public statement on 4 June 2021 which acknowledged the Office was investigating, we believe it is important to share publicly the information we can, now that the investigation is complete.
Our investigation was finalised in July 2023. We acknowledge the length of time the investigation has taken. This is in part due to the extensive efforts the Office made to source independent scientific expertise to advise us on some detailed and specific questions of scientific methodology that were raised with our Office, including some that were only brought to our attention as our investigation progressed. Despite our best efforts, it was not possible to engage an expert (or experts) to provide independent advice to our Office on this subject. In the absence of independent, expert scientific expertise we have not been able to conclusively determine those matters of scientific methodology. This did not prevent our Office from forming a view on other aspects of the matter.
Our investigation did not result in any adverse findings about the review or the NHMRC. When finalising investigations, we may offer comments and suggestions to an agency about areas for future improvement. In this instance, we offered comments and suggestions to the NHMRC about how it records and publicly explains decisions about its activities. The NHMRC also independently made several improvements to its processes during the course of our investigation.
________________
In essence, this means that the conclusions of the report stand:
Homeopathy should not be used to treat health conditions that are chronic, serious, or could become serious. People who choose homeopathy may put their health at risk if they reject or delay treatments for which there is good evidence for safety and effectiveness. People who are considering whether to use homeopathy should first get advice from a registered health practitioner. Those who use homeopathy should tell their health practitioner and should keep taking any prescribed treatments.
Thus the matter is closed – that is closed for rational thinkers. For irrationalists, the matter will no doubt continue to be a stone of contention. No, homeopath will be able to accept these conclusions simply because a member of a cult ceases to be a cultist once he/she accepts the criticism agaist the cult.
Massage is frequently used for recovery and increased performance. This review, aimed to search and systemize current literature findings relating to massages’ effects on sports and exercise performance concerning its effects on motor abilities and neurophysiological and psychological mechanisms.
One hundred and fourteen articles were included. The data revealed that massages, in general, do not affect motor abilities, except flexibility. However, several studies demonstrated that positive muscle force and strength changed 48 h after the massage was given. Concerning neurophysiological parameters, massage did not change blood lactate clearance, muscle blood flow, muscle temperature, or activation. However, many studies indicated a reduction of pain and delayed onset muscle soreness, which are probably correlated with the reduction of the level of creatine kinase enzyme and psychological mechanisms. In addition, massage treatment led to a decrease in depression, stress, anxiety, and the perception of fatigue and an increase in mood, relaxation, and the perception of recovery.
The authors concluded that the direct usage of massages just for gaining results in sport and exercise performance seems questionable. However, it is indirectly connected to performance as an important tool when an athlete should stay focused and relaxed during competition or training and recover after them.
The evidence about the value of massage therapy is limited through the mostly poor quality of the primary studies. Unfortunately, the review authors did not bother to address this issue. Another recent and in my opinion more rigorous review identified 29 eligible studies recruiting 1012 participants, representing the largest examination of the effects of massage. Its authors found no evidence that massage improves measures of strength, jump, sprint, endurance, or fatigue, but massage was associated with small but statistically significant improvements in flexibility and DOMS. Massage therapy has the additional advantage that it is agreeable and nearly free of adverse effects. So, on balance, I think massage therapy might be worth considering for athletes.
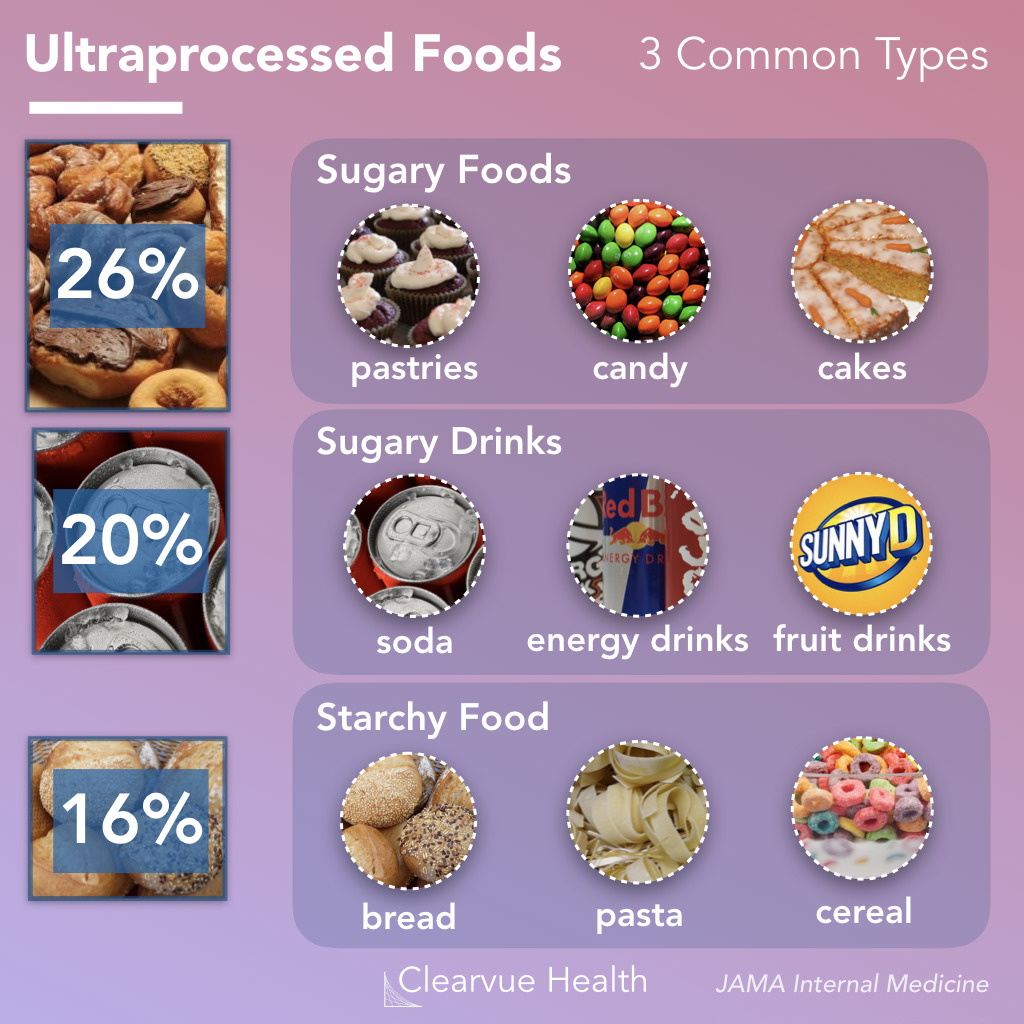
Like ultra-processed food (UPF) itself, the subject of UPF is everywhere – radio, TV, Twitter, you name it, the topic crops up. I too could not resist writing a post on it a few months ago. And now I am publishing another one but one in a slightly more irritated mood.
Why do these endless discussions on UPF irritate me?
To start with, there is no uniform definition of UPF, and many commentators seem more than a little confused about what UPF actually is. One definition holds that Ultra-processed foods are foods that have been altered to include fats, starches, sugars, salts and hydrogenated oils extracted from other foods. They contain ingredients, additives, and preservatives that are not normally used in home cooking. It seems obvious that discussions on UPF without a clear and understandable definition of the term are merely generating confusion in the general public.
But there are, of course, lists of UPF that might render the subject a bit clearer. The trouble, however, is that these lists reveal disagreement among each other. Thus they are prone to generate even more confusion.
Next, there is the evidence – and there is lots of it. It suggests that the regular consumption of UPF is bad for virtually every aspect of health. And if there is no evidence that it is detrimental for a given condition, it probably is merely because nobody has yet bothered to do the analyses. The trouble is, however, that all the relevant research comes from either basic science or epidemiology. This means that causality is unproven.
A further problem is that even the experts don’t know what the alleged causal factors in UPF are.
- Is it the processing?
- The additives?
- The sugar?
- The fats?
- If so, which fats exactly?
- Is it perhaps a complex inter-play of some of these factors?
If we want to make progress, we need to know! If not, we cannot possibly begin to avoid the health-threatening effects of UPF.
The final and arguably biggest problem is that UPF is everywhere. Nobody living in an industrialized country and earning a regular living can avoid consuming UPF. This means, I fear, that all the current hype about UPF is not just irritating but possibly counter-productive.
Imagine an average person trying to make sense of these discussions. She would soon give up and conclude that all these ‘clever’ experts know nothing at all. Her foremost concern is to make ends meet. In the end, she will carry on as before. Alternatively, she might even conclude that, as the even experts do not make sense, UPF cannot be all that bad after all.
After reading about and listening to the arguments around UPF, I ask myself this: would it not be more productive to apply more common sense and focus on a few nutritional messages that are 1) solidly based on evidence and 2) an average person can actually follow?
In a video, Mr.Darkmoore speaks from a hospital bed and says the cause behind his visit to the emergency room stemmed from a chiropractor’s work on him. Three days ago, he had a ringing in his ear due to a long-term condition he knew as tinnitus. Thus, he decided to visit a chiropractor. “I figured $100 to a chiro, let them adjust a few things, if all else fails, I’ll go to a doctor,” explains Darkmoore.
This $100 visit led to several other complications and doctor’s bills worth thousands of dollars. The day after he was treated by the chiropractor, he experienced a headache that eventually led to dizzy spells. He decided to visit the emergency room where a CT scan was ordered which showed that the chiropractor had dissected an artery in his neck.
Next, Darkmoore was put on blood thinners to avoid blood clots that could result in a stroke or worse. Darkmoore explains that he will be on two blood thinners for the next three months to prevent clotting. If the dissection heals partially, he says he will need to take aspirin every day for the rest of his life. If it doesn’t heal, he claims that he will need surgery.
Many viewers of the video claimed they have had the same “chiropractor gone wrong” experience as Darkmoore.
- “Wow. How scary. I had a similar thing happen to me. Extremely bad headache after going one time. Haven’t gone since,” one commenter wrote.
- “I’m so sorry this happened to u,” another user echoed. “My chiropractor also caused an injury which required emergency surgery & I have permanent damage. I’m glad u survived.”
Darkmore captioned his last update video, “I appreciate the thoughts and prayers. Hopefully, I’ll be okay after 3 months of recovery.”
__________________
Let’s hope that he is correct and that he will make a speedy and full recovery.
Of course, chiros will queue up to stress that important details are missing in this case report. To them, I would merely say this:
THERE IS NO GOOD EVIDENCE THAT NECK MANIPULATIONS BRING ANY BENEFIT AND QUITE A BIT OF EVIDENCE THAT THEY CAN CAUSE SERIOUS HARM.
SO, WHY NOT JUST STOP OFFERING THE PROCEDURE?
We have discussed dental amalgam and its risks to human health before. Finally, there is new legislation in sight. The European Commission has revised the EU Mercury Regulation to protect EU citizens and the environment from toxic mercury. Among other things, this will completely ban the use of dental amalgam, for which 40 tons of mercury are currently consumed annually in the EU. The revised mercury ordinance provides for the following:
– No more use of dental amalgam from January 1, 2025; viable mercury-free alternatives are available.
– Ban on the manufacture and export of dental amalgam from the EU from January 1, 2025;
– Ban on the manufacture and export of six mercury-containing lamps from January 1, 2026 and January 1, 2028 (depending on lamp type).
The delegated act adopted under the Mercury Regulation transposes into EU law the decisions taken at the fourth Conference of the Parties (2022) to the Minamata Convention by introducing a ban on the production, import, and export of eight additional mercury-containing products, including mercury-containing lamps and non-electrical equipment.
The Minamata Convention is the main international legal framework for the protection of human health and the environment from anthropogenic emissions and releases of mercury to air, water, and soil. Like the Mercury Regulation, it addresses the entire life cycle of mercury, from primary mercury mining to mercury waste management.
The revised Mercury Regulation must now be approved by the European Parliament and the Council under the ordinary legislative procedure. The delegated act will be sent to the European Parliament and the Council for consideration.
Mercury is a highly toxic chemical that poses a threat to both human health and the environment. When released into the environment, it enters the food chain where it accumulates (mainly in fish). High mercury exposure can damage the brain, lungs, kidneys, and immune system.
Historically, mercury has been used in a wide range of applications, including gold mining, batteries, fluorescent tubes, thermometers, and barometers. Over the last twenty years, the EU has developed a comprehensive body of legislation, in particular the Mercury Regulation, which protects human health and the environment from anthropogenic emissions and releases of mercury, taking into account the entire life cycle of mercury from primary mercury mining to final disposal of mercury waste. It also includes measures on trade in mercury-containing products and mercury pollution.
The Minamata Convention entered into force on August 16, 2017, and has so far been ratified by the European Union and 143 countries, including all EU Member States. The fifth session of the Conference of the Parties to the Minamata Convention on Mercury (COP-5) will be held in Geneva, Switzerland, from October 30 to November 3, 2023.
_____________________________
An impressive article by John Mac Ghlionn caught my attention. Allow me to quote a few passages from it:
The U.S. House of Representatives and the U.S. Senate recently reintroduced legislation to increase access to Medicare-covered services provided by chiropractors. Last year, the US chiropractic market size was worth $13.13 Billion. By the end of the decade, it will be worth over $18 billion. Each year, a whopping 35 million Americans seek chiropractic care.
But why? It’s a questionable science full of questionable characters.
Last year, a Georgia woman was left paralyzed and unable to speak after receiving a neck adjustment from a chiropractor. She’s not the first person to have had her life utterly ruined by a chiropractor, and chances are she won’t be the last. Many patients who visit chiropractors suffer severe side effects; some lose their lives…
As Dr. Steven Novella has noted, what used to be fraud is now known as holistic medicine. Dr. Edzard Ernst, a retired British-German physician and researcher, has expertly demonstrated the many ways in which chiropractic treatments are rooted not in science, but in mystical concepts…
Spinal adjustments, also known as “subluxations,” are also common. A dangerous practice that has been heavily criticized, spinal manipulations are associated with a number of adverse effects, including the risk of stroke. As Dr. Ernst has noted, the cost-effectiveness of this particular treatment “has not been demonstrated beyond reasonable doubt.”
Not content with spinal and neck manipulations, some chiropractors offer to treat other conditions — like diabetes, for example. They are not trained to treat diabetes. Other chiropractors appear to take joy in torturing infants. In August of 2018, a chiropractor made headlines for all the wrong reasons when a video emerged showing him hanging a two-week-old newborn upside down by the ankles…
Finally, as I alluded to earlier, the chiropractic community is full of fraudsters. In 2019, in the US, 15 chiropractors were charged in an insurance fraud and illegal kickback operation. More recently, in February of this year, a New York federal judge sentenced Patrick Khaziran to 30 months in prison after he pleaded guilty to being part of a widespread scheme that defrauded the NBA out of at least $5 million. In recent times, the chiropractic community has come under scrutiny for abusive care and illegal billing practices. When it comes to instances of healthcare fraud, chiropractic medicine is unrivaled.
None of this should come as a surprise. After all, the entire chiropractic community was constructed on a foundation of lies. As the aforementioned Dr. Ernst told me, we should be skeptical of what chiropractors are offering, largely because the whole practice was founded “by a deluded charlatan, who insisted that all human diseases are due to subluxations of the spine. Today, we know that chiropractic subluxations are mere figments of Palmer’s imagination. Yet, the chiropractic profession is unable to separate itself from the myth. It is easy to see why: without it, they would at best become poorly trained physiotherapists without any raison d’etre.”
… Dr. William T. Jarvis famously referred to chiropractic as “the most significant nonscientific health-care delivery system in the United States.” Comparing the chiropractic community to a cult, Dr. Jarvis wondered, somewhat incredulously, why chiropractors are licensed to practice in all 50 US states. The entire profession, he warned, “should be viewed as a societal problem, not simply as a competitor of regular health-care.”
___________________________
In my view, this is an impressive article, not least because it is refreshingly devoid of the phenomenon known as ‘false balance, e.g. a chiropractor being invited to add his self-interested views at the end of the paper claiming, for instance, “we have years of experience and cause far less harm than real doctors”.
There is widespread agreement amongst clinicians that people with non-specific low back pain (NSLBP) comprise a heterogeneous group and that their management should be individually tailored. One treatment known by its tailored design is the McKenzie method (e.g. an individualized program of exercises based on clinical clues observed during assessment) used mostly but not exclusively by physiotherapists.
A recent Cochrane review evaluated the effectiveness of the McKenzie method in people with (sub)acute non-specific low back pain. Randomized clinical trials (RCTs) investigating the effectiveness of the McKenzie method in adults with (sub)acute (less than 12 weeks) NSLBP.
Five RCTs were included with a total of 563 participants recruited from primary or tertiary care. Three trials were conducted in the USA, one in Australia, and one in Scotland. Three trials received financial support from non-commercial funders and two did not provide information on funding sources. All trials were at high risk of performance and detection bias. None of the included trials measured adverse events.
McKenzie method versus minimal intervention (educational booklet; McKenzie method as a supplement to other intervention – main comparison) There is low-certainty evidence that the McKenzie method may result in a slight reduction in pain in the short term (MD -7.3, 95% CI -12.0 to -2.56; 2 trials, 377 participants) but not in the intermediate term (MD -5.0, 95% CI -14.3 to 4.3; 1 trial, 180 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -2.5, 95% CI -7.5 to 2.0; 2 trials, 328 participants) nor in the intermediate term (MD -0.9, 95% CI -7.3 to 5.6; 1 trial, 180 participants).
McKenzie method versus manual therapy There is low-certainty evidence that the McKenzie method may not reduce pain in the short term (MD -8.7, 95% CI -27.4 to 10.0; 3 trials, 298 participants) and may result in a slight increase in pain in the intermediate term (MD 7.0, 95% CI 0.7 to 13.3; 1 trial, 235 participants). There is low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD -5.0, 95% CI -15.0 to 5.0; 3 trials, 298 participants) nor in the intermediate term (MD 4.3, 95% CI -0.7 to 9.3; 1 trial, 235 participants).
McKenzie method versus other interventions (massage and advice) There is very low-certainty evidence that the McKenzie method may not reduce disability in the short term (MD 4.0, 95% CI -15.4 to 23.4; 1 trial, 30 participants) nor in the intermediate term (MD 10.0, 95% CI -8.9 to 28.9; 1 trial, 30 participants).
The authors concluded that, based on low- to very low-certainty evidence, the treatment effects for pain and disability found in our review were not clinically important. Thus, we can conclude that the McKenzie method is not an effective treatment for (sub)acute NSLBP.
The hallmark of the McKenzie method for back pain involves the identification and classification of nonspecific spinal pain into homogenous subgroups. These subgroups are based on the similar responses of a patient’s symptoms when subjected to mechanical forces. The subgroups include postural syndrome, dysfunction syndrome, derangement syndrome, or “other,” with treatment plans directed to each subgroup. The McKenzie method emphasizes the centralization phenomenon in the assessment and treatment of spinal pain, in which pain originating from the spine refers distally, and through targeted repetitive movements the pain migrates back toward the spine. The clinician will then use the information obtained from this assessment to prescribe specific exercises and advise on which postures to adopt or avoid. Through an individualized treatment program, the patient will perform specific exercises at home approximately ten times per day, as opposed to 1 or 2 physical therapy visits per week. According to the McKenzie method, if there is no restoration of normal function, tissue healing will not occur, and the problem will persist.
Classification:
The postural syndrome is pain caused by mechanical deformation of soft tissue or vasculature arising from prolonged postural stresses. These may affect the joint surfaces, muscles, or tendons, and can occur in sitting, standing, or lying. Pain may be reproducible when such individuals maintain positions or postures for sustained periods. Repeated movements should not affect symptoms, and relief of pain typically occurs immediately following the correction of abnormal posture.
The dysfunction syndrome is pain caused by the mechanical deformation of structurally impaired soft tissue; this may be due to traumatic, inflammatory, or degenerative processes, causing tissue contraction, scarring, adhesion, or adaptive shortening. The hallmark is a loss of movement and pain at the end range of motion. Dysfunction has subsyndromes based upon the end-range direction that elicits this pain: flexion, extension, side-glide, multidirectional, adherent nerve root, and nerve root entrapment subsyndromes. Successful treatment focuses on patient education and mobilization exercises that focus on the direction of the dysfunction/direction of pain. The goal is on tissue remodeling which can be a prolonged process.
The derangement syndrome is the most commonly encountered pain syndrome, reported in one study to have a prevalence as high as 78% of patients classified by the McKenzie method. It is caused by an internal dislocation of articular tissue, causing a disturbance in the normal position of affected joint surfaces, deforming the capsule, and periarticular supportive ligaments. This derangement will both generate pain and obstruct movement in the direction of the displacement. There are seven different subsyndromes which are classified by the location of pain and the presence, or absence, of deformities. Pain is typically elicited by provocative assessment movements, such as flexion or extension of the spine. The centralization and peripheralization of symptoms can only occur in the derangement syndrome. Thus the treatment for derangement syndrome focuses on repeated movement in a single direction that causes a gradual reduction in pain. Studies have shown approximately anywhere between 58% to 91% prevalence of centralization of lower back pain. Studies have also shown that between 67% to 85% of centralizers displayed the directional preference for a spinal extension. This preference may partially explain why the McKenzie method has become synonymous with spinal extension exercises. However, care must be taken to accurately diagnose the direction of pain, as one randomized controlled study has shown that giving the ‘wrong’ direction of exercises can actually lead to poorer outcomes.
Other or Nonmechanical syndrome refers to any symptom that does not fit in with the other mechanical syndromes, but exhibits signs and symptoms of other known pathology; Some of these examples include spinal stenosis, sacroiliac disorders, hip disorders, zygapophyseal disorders, post-surgical complications, low back pain secondary to pregnancy, spondylolysis, and spondylolisthesis.
CONCLUSION:
“Internationally researched” and found to be ineffective!
I missed this paper when it first came out in 2022. Yet, it seems potentially quite important and I, therefore, feel like discussing it here:
President of the UNESCO Committee on Bioethics Stefan Semplici called on the governments of all countries to ensure free and wider access of their citizens to alternative medicine and pay for this therapy through health insurance. Alternative medicine based on tradition – traditional medicine, in many poor countries is the only treatment option for the population. In developed countries, and especially in China and India, it enjoys well-deserved prestige (for example, acupuncture and herbal medicine) and is often integrated into the public health system.
The International Committee on Bioethics of UNESCO announced the recognition of these alternative therapies as an option for medical practice and, at the same time, as part of the identity of the cultural traditions of various nations. The UNESCO Universal Declaration on Bioethics and Human Rights includes the right to the highest attainable standard of health (Article 14), the right to respect for pluralism and cultural diversity (Article 12) and traditional knowledge (Article 17). The purpose of this document is to establish criteria for the respect and acceptability of different types of medicine without compromising the assurance of quality and patient safety that is essential in all treatments.
In order to adapt the traditions of traditional therapies to advances in medicine, this international organization calls on governments and the scientific community to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety and develop therapeutic standards and protocols for integrating traditional medicine into healthcare system. The UNESCO International Bioethics Committee believes that these methods should be seen as complementary to modern medicine, and not just an alternative to it.
_________________________
The United Nations Educational, Scientific and Cultural Organization (UNESCO) is an agency of the United Nations aimed at promoting world peace and security through international cooperation in education, arts, sciences, and culture. UNESCO’s International Bioethics Committee (IBC) is a body of 36 independent experts that follows progress in the life sciences and its applications in order to ensure respect for human dignity and freedom.
I have to say that I rarely have seen an announcement in so-called alternative medicine (SCAM) that is more confusing and less well thought through. The UNESCO Committee on Bioethics wants:
- alternative therapies as an option for medical practice,
- the highest attainable standard of health,
- to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety.
When I first read these lines, I asked myself: who on earth wrote such nonsense? It was certainly not written by someone who understands healthcare, SCAM, and evidence-based medicine.
As discussed almost permanently on this blog, most forms of SCAM have not been shown to generate more good than harm. This means that employing them ‘as an option in medical practice’ cannot possibly produce ‘the highest attainable standards of health’. In fact, the UNESCO plan would lead to lower not higher standards. How can a committee on bioethics not realize that this is profoundly unethical?
Collaboration with practitioners of alternative therapies to evaluate SCAM’s effectiveness and safety sounds a bit more reasonable. It ignores, however, that tons of evidence already exist but fail to be positive. Why do these experts in bioethics not advocate to first make a sober assessment of the published literature?
I must say that the initiative of the UNESCO Committee on Bioethics puzzles me a lot and disturbs me even more.
I’d be keen to learn what you think of it.
The current secondary analysis based on the WHO database (VigiBase) of individual case safety reports (ICSRs) focuses on the suspected cutaneous adverse drug reactions (ADRs) linked to traditional medicines (TMs).
All the ICSRs reported between 1st January 2016 and 30th June 2021 from the UN Asia region in VigiBase where at least one TM was suspected to cause cutaneous ADRs were included in the study. Data regarding demographic details, suspected drug, adverse reaction as per MedDRA term, the seriousness of the reaction, de-challenge, re-challenge, and clinical outcome for suspected cutaneous ADRs associated with TM were obtained from VigiBase and analyzed for frequency of reported events and suspected medicines.
A total of 3,523 ICSRs with 5,761 ADRs related to “skin and subcutaneous tissue disorders” were included in the analysis. Amongst these, 6.8% of ICSRs were reported as serious.
The most common ADRs were:
- pruritus (29.6%),
- rash (20.3%),
- urticaria (18.9%),
- hyperhidrosis (3.3%).
Artemisia argyi H.Lév. and Vaniot. (14.9%), Ginkgo biloba L. (5.1%), Vitis vinifera L. (4%), Vitex agnus-castus L. (3.8%), Silybum marianum (L.), Gaertn (3.5%), and Viscus album L. (2.7%) were some commonly suspected TMs for cutaneous ADRs. There were 46 cases of Stevens-Johnson syndrome and toxic epidermal necrolysis reported with TMs during the study period. Death was reported in 5 ICSRs.
The authors concluded that TMs are linked with various cutaneous ADRS ranging from pruritus to toxic epidermal necrolysis which may have serious consequences. TMs listed as suspected offending agents in this analysis, should be kept in mind while dealing with suspected cutaneous ADRs. Clinicians should be more vigilant in detecting and reporting events associated with TMs.
Herbal remedies have a reputation for being time-tested, gentle, harmless, and benign. Reports such as this one might make us doubt this cliche. More importantly, they should force us to ask whether the remedy we are tempted to try truly does generate more good than harm. In most instances, I fear, the answer is not positive.