risk/benefit
- COVID vaccinations are not 100% harmless but they generate much more good than harm.
- They are certainly far less dangerous than the disease.
- COVID infections are not ‘just a flu’ but have serious consequences.
The last point was well-documented in a recent Lancet paper. Here is its abstract in full
Mortality statistics are fundamental to public health decision making. Mortality varies by time and location, and its measurement is affected by well known biases that have been exacerbated during the COVID-19 pandemic. This paper aims to estimate excess mortality from the COVID-19 pandemic in 191 countries and territories, and 252 subnational units for selected countries, from Jan 1, 2020, to Dec 31, 2021.
Methods
All-cause mortality reports were collected for 74 countries and territories and 266 subnational locations (including 31 locations in low-income and middle-income countries) that had reported either weekly or monthly deaths from all causes during the pandemic in 2020 and 2021, and for up to 11 year previously. In addition, we obtained excess mortality data for 12 states in India. Excess mortality over time was calculated as observed mortality, after excluding data from periods affected by late registration and anomalies such as heat waves, minus expected mortality. Six models were used to estimate expected mortality; final estimates of expected mortality were based on an ensemble of these models. Ensemble weights were based on root mean squared errors derived from an out-of-sample predictive validity test. As mortality records are incomplete worldwide, we built a statistical model that predicted the excess mortality rate for locations and periods where all-cause mortality data were not available. We used least absolute shrinkage and selection operator (LASSO) regression as a variable selection mechanism and selected 15 covariates, including both covariates pertaining to the COVID-19 pandemic, such as seroprevalence, and to background population health metrics, such as the Healthcare Access and Quality Index, with direction of effects on excess mortality concordant with a meta-analysis by the US Centers for Disease Control and Prevention. With the selected best model, we ran a prediction process using 100 draws for each covariate and 100 draws of estimated coefficients and residuals, estimated from the regressions run at the draw level using draw-level input data on both excess mortality and covariates. Mean values and 95% uncertainty intervals were then generated at national, regional, and global levels. Out-of-sample predictive validity testing was done on the basis of our final model specification.
Findings
Although reported COVID-19 deaths between Jan 1, 2020, and Dec 31, 2021, totalled 5·94 million worldwide, we estimate that 18·2 million (95% uncertainty interval 17·1–19·6) people died worldwide because of the COVID-19 pandemic (as measured by excess mortality) over that period. The global all-age rate of excess mortality due to the COVID-19 pandemic was 120·3 deaths (113·1–129·3) per 100 000 of the population, and excess mortality rate exceeded 300 deaths per 100 000 of the population in 21 countries. The number of excess deaths due to COVID-19 was largest in the regions of south Asia, north Africa and the Middle East, and eastern Europe. At the country level, the highest numbers of cumulative excess deaths due to COVID-19 were estimated in India (4·07 million [3·71–4·36]), the USA (1·13 million [1·08–1·18]), Russia (1·07 million [1·06–1·08]), Mexico (798 000 [741 000–867 000]), Brazil (792 000 [730 000–847 000]), Indonesia (736 000 [594 000–955 000]), and Pakistan (664 000 [498 000–847 000]). Among these countries, the excess mortality rate was highest in Russia (374·6 deaths [369·7–378·4] per 100 000) and Mexico (325·1 [301·6–353·3] per 100 000), and was similar in Brazil (186·9 [172·2–199·8] per 100 000) and the USA (179·3 [170·7–187·5] per 100 000).
Interpretation
The full impact of the pandemic has been much greater than what is indicated by reported deaths due to COVID-19 alone. Strengthening death registration systems around the world, long understood to be crucial to global public health strategy, is necessary for improved monitoring of this pandemic and future pandemics. In addition, further research is warranted to help distinguish the proportion of excess mortality that was directly caused by SARS-CoV-2 infection and the changes in causes of death as an indirect consequence of the pandemic.
I am posting this in the hope that the many proponents of so-called alternative medicine (SCAM) who deny proven facts about COVID might learn and stop falling victim to proctophasia.
Chronic low back pain (CLBP) is among the most common types of pain in adults. It is also the domain for many types of so-called alternative medicine (SCAM). However, their effectiveness remains questionable, and the optimal approach to CLBP remains elusive. Meditation-based therapies constitute a form of SCAM with high potential for widespread availability.
This systematic review and meta-analysis of randomized clinical trials evaluated the efficacy of meditation-based therapies for CLBP management. The primary outcomes were pain intensity, quality of life, and pain-related disability; the secondary outcomes were the experienced distress or anxiety and pain bothersomeness in the patients. The PubMed, Embase, and Cochrane databases were searched for studies published from their inception until July 2021, without language restrictions.
A total of 12 randomized clinical trials with 1153 patients were included. In 10 trials, meditation-based therapies significantly reduced the CLBP pain intensity compared with nonmeditation therapies (standardized mean difference [SMD] -0.27, 95% CI = -0.43 to – 0.12, P = 0.0006). In 7 trials, meditation-based therapies also significantly reduced CLBP bothersomeness compared with nonmeditation therapies (SMD -0.21, 95% CI = -0.34 to – 0.08, P = 0.002). In 3 trials, meditation-based therapies significantly improved patient quality of life compared with nonmeditation therapies (SMD 0.27, 95% CI = 0.17 to 0.37, P < 0.00001).
The authors concluded that meditation-based therapies constitute a safe and effective alternative approach for CLBP management.
The problem with this conclusion is that the primary studies are mostly of poor quality. For instance, they do not control for placebo effects (which is obviously not easy in this case). Thus, we need to take the conclusion with a pinch of salt.
However, since the same limitations apply to chiropractic and osteopathy, and since meditation has far fewer risks than these approaches, I would gladly recommend meditation over manipulative therapies. Or, to put it plainly: in terms of risk/benefit balance, meditation seems preferable to spinal manipulation.
Yesterday I received the following interesting email: 
Pfizer your God father has now officially released the list ofAdverse events.. it’s huge.. and it’s official…If you guys had half a brainYou would have seen this coming.. calling others quacks..Pfizer clowns need to be hung on a tree just like Judas..
Is this a death threat?
Probably!
Never mind, I am getting used to them.
The first one that I remember came when I was still working at my department in Exeter. We had to call the police who instructed my secretaries how to identify letter bombs without opening them. We had reason to believe that such a device had been posted to me. Not a nice experience!
Since then, death threats have arrived with some regularity.
The one above, however, seems special.
I do not recall advertising the Pfizer vaccine on this blog and elsewhere. It seems therefore that the author (who used the following email address: John <[email protected]>) is more than mildly deranged.
Am I worried? No, not about my safety (but a little about John, I must admit). I have long learned that such aggressions of this nature are a sign that I am probably on the right path. They are, in other words, a victory of reason over unreason.
So, maybe I will start advertising the Pfizer vaccine after all?
The new issue of the BMJ carries an article on acupuncture that cries out for a response. Here, I show you the original article followed by my short comments. For clarity, I have omitted the references from the article and added references that refer to my comments.
_________________________________________
Conventional allopathic medicine [1]—medications and surgery [2] used in conventional systems of medicine to treat or prevent disease [3]—is often expensive, can cause side effects and harm, and is not always the optimal treatment for long term conditions such as chronic pain [4]. Where conventional treatments have not been successful, acupuncture and other traditional and complementary medicines have potential to play a role in optimal patient care [5].
According to the World Health Organisation (WHO) 2019 global report, acupuncture is widely used across the world. [6] In some countries acupuncture is covered by health insurance and established regulations. [7] In the US, practitioners administer over 10 million acupuncture treatments annually. [6] In the UK, clinicians administer over 4 million acupuncture treatments annually, and it is provided on the NHS. [6]
Given the widespread use of acupuncture as a complementary therapy alongside conventional medicine, there has been an increase in global research interest and funding support over recent decades. In 2009, the European Commission launched a Good Practice in Traditional Chinese Medicine Research (GP-TCM) funding initiative in 19 countries. [7] The GP-TCM grant aimed to investigate the safety and efficacy of acupuncture as well as other traditional Chinese medicine interventions.
In China, acupuncture is an important focus of the national research agenda and receives substantial research funding. [8] In 2016, the state council published a national strategy supporting universal access to acupuncture by 2020. China has established more than 79 evidence-based traditional Chinese medicine or integrative medicine research centers. [9]
Given the broad clinical application and rapid increase in funding support for acupuncture research, researchers now have additional opportunities to produce high-quality studies. However, for this to be successful, acupuncture research must address both methodological limitations and unique research challenges.
This new collection of articles, published in The BMJ, analyses the progress of developing high quality research studies on acupuncture, summarises the current status, and provides critical methodological guidance regarding the production of clinical evidence on randomised controlled trials, clinical practice guidelines and health economic evidence. It also assesses the number and quality of systematic reviews of acupuncture. [10] We hope that the collection will help inform the development of clinical practice guidelines, health policy, and reimbursement decisions. [11]
The articles document the progress of acupuncture research. In our view, the emerging evidence base on the use of acupuncture warrants further integration and application of acupuncture into conventional medicine. [12] National, regional, and international organisations and health systems should facilitate this process and support further rigorous acupuncture research.
Footnotes
This article is part of a collection funded by the special purpose funds for the belt and road, China Academy of Chinese Medical Sciences, National Natural Science Foundation of China, the National Center for Complementary and Integrative Health, the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine, the Special Project of “Lingnan Modernization of Traditional Chinese Medicine” of the 2019 Guangdong Key Research and Development Program, and the Project of First Class Universities and High-level Dual Discipline for Guangzhou University of Chinese Medicine. The BMJ commissioned, peer reviewed, edited, and made the decision to publish. Kamran Abbasi was the lead editor for The BMJ. Yu-Qing Zhang advised on commissioning for the collection, designed the topic of the series, and coordinated the author teams. Gordon Guyatt provided valuable advice and guidance. [13]
1. Allopathic medicine is the term Samuel Hahnemann coined for defaming conventional medicine. Using it in the first sentence of the article sets the scene very well.
2. Medicine is much more than ‘medications and surgery’. To imply otherwise is a strawman fallacy.
3. What about rehabilitation medicine?
4. ‘Conventional medicine is not always the optimal treatment’? This statement is very confusing and wrong. It is true that conventional medicine is not always effective. However, it is by definition the best we currently have and therefore it IS optimal.
5. Another fallacy: non sequitur
6. Another fallacy: appeal to popularity.
7. Yet another fallacy: appeal to authority.
8. TCM is heavily promoted by China not least because it is a most lucrative source of income.
9. Several research groups have shown that 100% of acupuncture research coming out of China report positive results. This casts serious doubt on the reliability of these studies (see, for instance, here, here, and here).
10. It has been noted that more than 80 percent of clinical data from China is fabricated.
11. Based on the points raised above, it seems to me that the collection’s aim is not to provide objective information but uncritical promotion.
12. I find it telling that the authors do not even consider the possibility that rigorous research might demonstrate that acupuncture cannot generate more good than harm.
13. This statement essentially admits that the series of articles constitutes paid advertising for TCM. The BMJ’s peer-review process must have been less than rigorous in this case.
On 27 January 2022, I conducted a very simple Medline search using the search term ‘Chinese Herbal Medicine, Review, 2022’. Its results were remarkable; here are the 30 reviews I found:
- Zhu, S. J., Wang, R. T., Yu, Z. Y., Zheng, R. X., Liang, C. H., Zheng, Y. Y., Fang, M., Han, M., & Liu, J. P. (2022). Chinese herbal medicine for myasthenia gravis: A systematic review and meta-analysis of randomized clinical trials. Integrative medicine research, 11(2), 100806.
- Lu, J., Li, W., Gao, T., Wang, S., Fu, C., & Wang, S. (2022). The association study of chemical compositions and their pharmacological effects of Cyperi Rhizoma (Xiangfu), a potential traditional Chinese medicine for treating depression. Journal of ethnopharmacology, 287, 114962.
- Su, F., Sun, Y., Zhu, W., Bai, C., Zhang, W., Luo, Y., Yang, B., Kuang, H., & Wang, Q. (2022). A comprehensive review of research progress on the genus Arisaema: Botany, uses, phytochemistry, pharmacology, toxicity and pharmacokinetics. Journal of ethnopharmacology, 285, 114798.
- Nanjala, C., Ren, J., Mutie, F. M., Waswa, E. N., Mutinda, E. S., Odago, W. O., Mutungi, M. M., & Hu, G. W. (2022). Ethnobotany, phytochemistry, pharmacology, and conservation of the genus Calanthe R. Br. (Orchidaceae). Journal of ethnopharmacology, 285, 114822.
- Li, M., Jiang, H., Hao, Y., Du, K., Du, H., Ma, C., Tu, H., & He, Y. (2022). A systematic review on botany, processing, application, phytochemistry and pharmacological action of Radix Rehmnniae. Journal of ethnopharmacology, 285, 114820.
- Mutinda, E. S., Mkala, E. M., Nanjala, C., Waswa, E. N., Odago, W. O., Kimutai, F., Tian, J., Gichua, M. K., Gituru, R. W., & Hu, G. W. (2022). Traditional medicinal uses, pharmacology, phytochemistry, and distribution of the Genus Fagaropsis (Rutaceae). Journal of ethnopharmacology, 284, 114781.
- Xu, Y., Liu, J., Zeng, Y., Jin, S., Liu, W., Li, Z., Qin, X., & Bai, Y. (2022). Traditional uses, phytochemistry, pharmacology, toxicity and quality control of medicinal genus Aralia: A review. Journal of ethnopharmacology, 284, 114671.
- Peng, Y., Chen, Z., Li, Y., Lu, Q., Li, H., Han, Y., Sun, D., & Li, X. (2022). Combined therapy of Xiaoer Feire Kechuan oral liquid and azithromycin for mycoplasma Pneumoniae pneumonia in children: A systematic review & meta-analysis. Phytomedicine : international journal of phytotherapy and phytopharmacology, 96, 153899.
- Xu, W., Li, B., Xu, M., Yang, T., & Hao, X. (2022). Traditional Chinese medicine for precancerous lesions of gastric cancer: A review. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 146, 112542.
- Wang, Y., Greenhalgh, T., Wardle, J., & Oxford TCM Rapid Review Team (2022). Chinese herbal medicine (“3 medicines and 3 formulations”) for COVID-19: rapid systematic review and meta-analysis. Journal of evaluation in clinical practice, 28(1), 13–32.
- Chen, X., Lei, Z., Cao, J., Zhang, W., Wu, R., Cao, F., Guo, Q., & Wang, J. (2022). Traditional uses, phytochemistry, pharmacology and current uses of underutilized Xanthoceras sorbifolium bunge: A review. Journal of ethnopharmacology, 283, 114747.
- Liu, X., Li, Y., Bai, N., Yu, C., Xiao, Y., Li, C., & Liu, Z. (2022). Updated evidence of Dengzhan Shengmai capsule against ischemic stroke: A systematic review and meta-analysis. Journal of ethnopharmacology, 283, 114675.
- Chen, J., Zhu, Z., Gao, T., Chen, Y., Yang, Q., Fu, C., Zhu, Y., Wang, F., & Liao, W. (2022). Isatidis Radix and Isatidis Folium: A systematic review on ethnopharmacology, phytochemistry and pharmacology. Journal of ethnopharmacology, 283, 114648.
- Tian, J., Shasha, Q., Han, J., Meng, J., & Liang, A. (2022). A review of the ethnopharmacology, phytochemistry, pharmacology and toxicology of Fructus Gardeniae (Zhi-zi). Journal of ethnopharmacology, 114984. Advance online publication.
- Wong, A. R., Yang, A., Li, M., Hung, A., Gill, H., & Lenon, G. B. (2022). The Effects and Safety of Chinese Herbal Medicine on Blood Lipid Profiles in Placebo-Controlled Weight-Loss Trials: A Systematic Review and Meta-Analysis. Evidence-based complementary and alternative medicine : eCAM, 2022, 1368576.
- Lu, C., Ke, L., Li, J., Wu, S., Feng, L., Wang, Y., Mentis, A., Xu, P., Zhao, X., & Yang, K. (2022). Chinese Medicine as an Adjunctive Treatment for Gastric Cancer: Methodological Investigation of meta-Analyses and Evidence Map. Frontiers in pharmacology, 12, 797753.
- Niu, L., Xiao, L., Zhang, X., Liu, X., Liu, X., Huang, X., & Zhang, M. (2022). Comparative Efficacy of Chinese Herbal Injections for Treating Severe Pneumonia: A Systematic Review and Bayesian Network Meta-Analysis of Randomized Controlled Trials. Frontiers in pharmacology, 12, 743486.
- Zhang, L., Huang, J., Zhang, D., Lei, X., Ma, Y., Cao, Y., & Chang, J. (2022). Targeting Reactive Oxygen Species in Atherosclerosis via Chinese Herbal Medicines. Oxidative medicine and cellular longevity, 2022, 1852330.
- Zhou, X., Guo, Y., Yang, K., Liu, P., & Wang, J. (2022). The signaling pathways of traditional Chinese medicine in promoting diabetic wound healing. Journal of ethnopharmacology, 282, 114662.
- Yang, M., Shen, C., Zhu, S. J., Zhang, Y., Jiang, H. L., Bao, Y. D., Yang, G. Y., & Liu, J. P. (2022). Chinese patent medicine Aidi injection for cancer care: An overview of systematic reviews and meta-analyses. Journal of ethnopharmacology, 282, 114656.
- Liu, H., & Wang, C. (2022). The genus Asarum: A review on phytochemistry, ethnopharmacology, toxicology and pharmacokinetics. Journal of ethnopharmacology, 282, 114642.
- Lin, Z., Zheng, J., Chen, M., Chen, J., & Lin, J. (2022). The Efficacy and Safety of Chinese Herbal Medicine in the Treatment of Knee Osteoarthritis: An Updated Systematic Review and Meta-Analysis of 56 Randomized Controlled Trials. Oxidative medicine and cellular longevity, 2022, 6887988.
- Yu, R., Zhang, S., Zhao, D., & Yuan, Z. (2022). A systematic review of outcomes in COVID-19 patients treated with western medicine in combination with traditional Chinese medicine versus western medicine alone. Expert reviews in molecular medicine, 24, e5.
- Mo, X., Guo, D., Jiang, Y., Chen, P., & Huang, L. (2022). Isolation, structures and bioactivities of the polysaccharides from Radix Hedysari: A review. International journal of biological macromolecules, 199, 212–222.
- Yang, L., Chen, X., Li, C., Xu, P., Mao, W., Liang, X., Zuo, Q., Ma, W., Guo, X., & Bao, K. (2022). Real-World Effects of Chinese Herbal Medicine for Idiopathic Membranous Nephropathy (REACH-MN): Protocol of a Registry-Based Cohort Study. Frontiers in pharmacology, 12, 760482.
- Zhang, R., Zhang, Q., Zhu, S., Liu, B., Liu, F., & Xu, Y. (2022). Mulberry leaf (Morus alba L.): A review of its potential influences in mechanisms of action on metabolic diseases. Pharmacological research, 175, 106029.
- Yuan, J. Y., Tong, Z. Y., Dong, Y. C., Zhao, J. Y., & Shang, Y. (2022). Research progress on icariin, a traditional Chinese medicine extract, in the treatment of asthma. Allergologia et immunopathologia, 50(1), 9–16.
- Zeng, B., Wei, A., Zhou, Q., Yuan, M., Lei, K., Liu, Y., Song, J., Guo, L., & Ye, Q. (2022). Andrographolide: A review of its pharmacology, pharmacokinetics, toxicity and clinical trials and pharmaceutical researches. Phytotherapy research : PTR, 36(1), 336–364.
- Zhang, L., Xie, Q., & Li, X. (2022). Esculetin: A review of its pharmacology and pharmacokinetics. Phytotherapy research : PTR, 36(1), 279–298.
- Wang, D. C., Yu, M., Xie, W. X., Huang, L. Y., Wei, J., & Lei, Y. H. (2022). Meta-analysis on the effect of combining Lianhua Qingwen with Western medicine to treat coronavirus disease 2019. Journal of integrative medicine, 20(1), 26–33. https://doi.org/10.1016/j.joim.2021.10.005
The amount of reviews alone is remarkable, I think: more than one review per day! Apart from their multitude, the reviews are noteworthy for other reasons as well.
- Their vast majority arrived at positive or at least encouraging conclusions.
- Most of the primary studies are from China (and we have often discussed how unreliable these trials are).
- Many of the primary studies are not accessible.
- Those that are accessible tend to be of lamentable quality.
I fear that all this is truly dangerous. The medical literature is being swamped with reviews of Chinese herbal medicine and other TCM modalities. Collectively they give the impression that these treatments are supported by sound evidence. Yet, the exact opposite is the case.
The process that is happening in front of our very eyes is akin to that of money laundering. Unreliable and often fraudulent data is being white-washed and presented to us as evidence.
The result:
WE ARE BEING SYSTEMATICALLY MISLED!
Enthusiasts of so-called alternative medicine (SCAM) seem remarkably often those who deny the evidence related to the dire consequences of a COVID-19 infection. Consequently, they also deny the value of COVID vaccinations. Because on this blog we have had so many examples of this phenomenon, let me today show an interesting study that might give them food for thought.
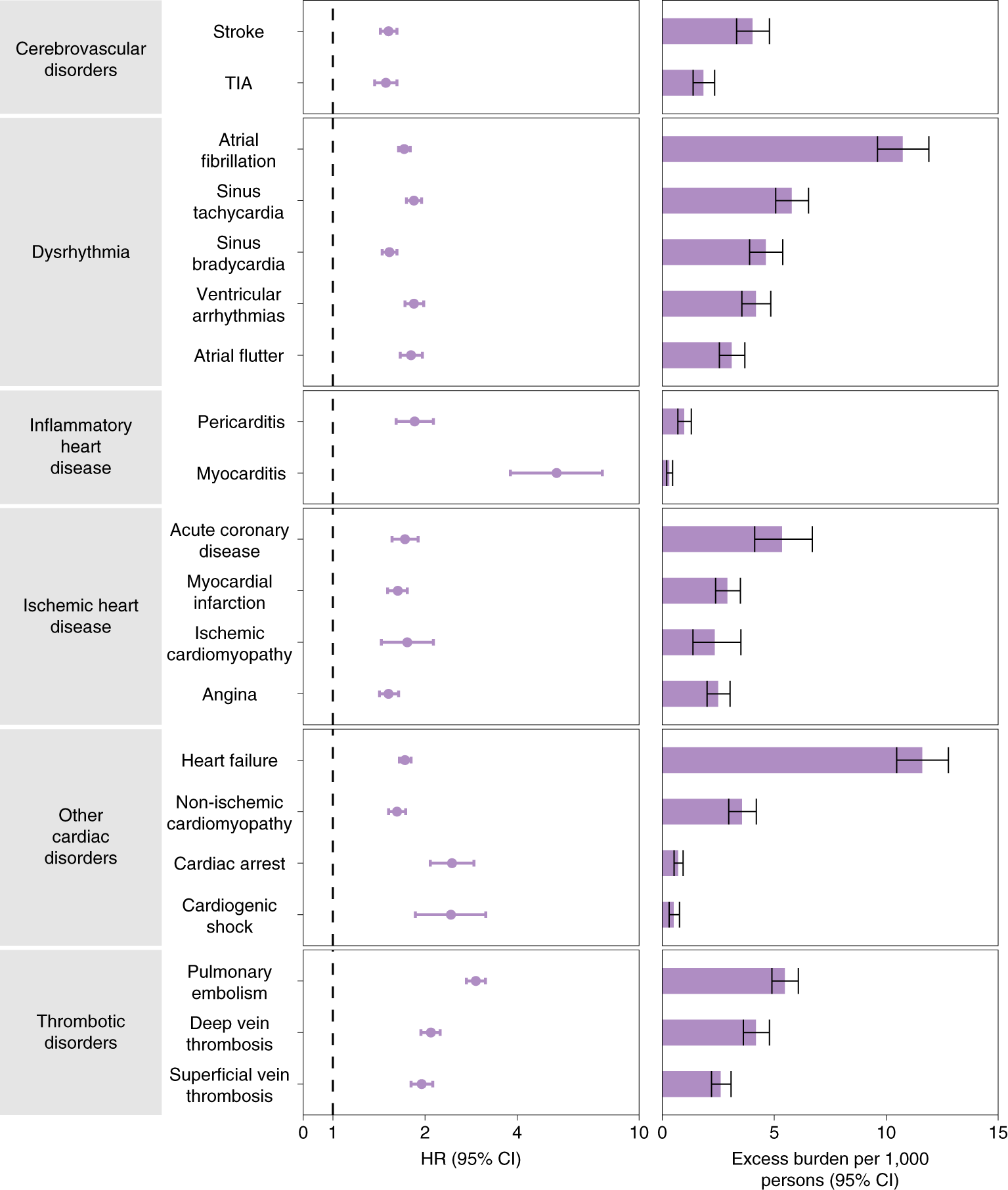
The cardiovascular complications of acute coronavirus disease 2019 (COVID-19) are well described, but the post-acute cardiovascular manifestations of COVID-19 have not yet been comprehensively characterized. The authors of this study used national healthcare databases from the US Department of Veterans Affairs to build a cohort of 153,760 individuals with COVID-19, as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) individuals, to estimate risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.
The results show that beyond the first 30 d after infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease. These risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized, and admitted to intensive care).
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
The authors concluded that the results provide evidence that the risk and 1-year burden of cardiovascular disease in survivors of acute COVID-19 are substantial. Care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
I know, this is a case-control study and correlation is not causation. But to investigate the possibility of a causal link further, the authors also tested the robustness of results in several sensitivity analyses involving the outcomes of MACE and any cardiovascular outcome. The sensitivity analyses were performed in comparisons involving COVID-19 versus the contemporary control and COVID-19 versus the historical control and, additionally, COVID-19 by care setting versus both controls.
(1) To test whether the inclusion of additional algorithmically selected covariates would challenge the robustness of study results, they selected and used 300 high-dimensional variables (instead of the 100 used in the primary analyses) to construct the inverse probability weighting.
(2) They then also tested the results in models specified to include only pre-defined covariates (that is, without the inclusion of algorithmically selected covariates) to build the inverse probability weighting.
(3) They changed the analytic approach by using the doubly robust method (instead of the inverse weighting method used in primary analyses) to estimate the magnitude of the associations between COVID-19 exposure and the pre-specified outcomes.
All sensitivity analyses yielded results consistent with those produced using the primary approach. This means that it is likely that the cause of the outcomes was the COVID-19 exposure.
How often have we seen advocates of SCAM argue against vaccination by pointing to the risk of myocarditis and other cardiovascular conditions, no matter how minuscule that risk truly is? This study quantifies the relative risk of several different cardiovascular outcomes after COVID-19 infection and the risk of myocarditis clearly stands out. I hope that the findings of this important study will make the COVID deniers reconsider their attitude.
Vertebral artery dissection is an uncommon, but potentially fatal, vascular event. This case aimed to describe the pathogenesis and clinical presentation of vertebral artery dissection in a term pregnant patient. Moreover, the authors focused on the differential diagnosis, reviewing the available evidence.
A 39-year-old Caucasian woman presented at 38 + 4 weeks of gestation with a short-term history of vertigo, nausea, and vomiting. Symptoms appeared a few days after cervical spine manipulation by an osteopathic specialist. Urgent magnetic resonance imaging of the head was obtained and revealed an ischemic lesion of the right posterolateral portion of the brain bulb. A subsequent computed tomography angiographic scan of the head and neck showed a right vertebral artery dissection. Based on the correlation of the neurological manifestations and imaging findings, a diagnosis of vertebral artery dissection was established. The patient started low-dose acetylsalicylic acid and prophylactic enoxaparin following an urgent cesarean section.
Right vertebral artery dissection with ischemia in the posterolateral medulla oblongata. In DWI (a) and ADC map (b) the arrow shows a punctate, shiny ischemic lesion, with typical reduction of ADC in the right posterolateral medulla oblongata. c and d CT angiography (axial and 3D reformat, c and d, respectively) showing a focal dissection of the V2 distal segment of the right vertebral artery, with the arrow in figure c pointing to the dissection. e MRI angiography (time of flight, TOF) showing the absence of visualization of right PICA.
The authors concluded that vertebral artery dissection is a rare but potential cause of neurologic impairments in pregnancy and during the postpartum period. It should be considered in the differential diagnosis for women who present with headache and/or vertigo. Women with a history of migraines, hypertension, or autoimmune disorders in pregnancy are at higher risk, as well as following cervical spine manipulations. Prompt diagnosis and management of vertebral artery dissection are essential to ensure favorable outcomes.
In the discussion section, the authors point out that the incidence of VAD in pregnancy is twice as common as in the rest of the female population. They also mention that a review of the literature regarding adverse effects of spinal manipulation in the pregnant and postpartum periods identified adverse events in five pregnant women and two postpartum women. The authors also include a table that summarizes all cases of VAD reported both prior and after delivery, with 24 cases distributed with a prevalence during the postpartum period (19 of the 24 cases). The clinical presentation of these cases is varied, with a higher frequency of headaches, vertigo, and diplopia, and the risk factors most represented are hypertension and migraines.
The authors finish with this advice: practitioners who do spinal manipulations should be aware of the possible complications of neck manipulation in pregnancy and the postpartum period, particularly in mothers with underlying medical disorders that may predispose to vessel fragility and VAD.
I would add advice of a different nature: consumers should always question whether the risks of any intervention outweigh its benefit. In the case of neck manipulations, the answer is not positive.
The ‘Society of Physicians and Scientists for Health, Freedom and Democracy’ (Gesellschaft der Mediziner und Wissenschaftler für Gesundheit, Freiheit und Demokratie e.V. MWGFD) recently held a press coference where they presented its 10-point plan for a Corona phase-out concept. Here are their 10 demands (my translation):
- Immediate cessation of COVID vaccinations and in particular compulsory COVID vaccination.
- End all non-evidence-based non-pharmaceutical measures (NPI’s), such as lockdowns, school closures, mandatory masks in public spaces, isolation, quarantine, contact tracing, stand-off rules, as well as RT-PCR and rapid antigen testing of people without symptoms of disease, and immediately open sports venues, restaurants, churches and cultural institutions to all without access conditions
- Pandemic management must be sensibly controlled on the basis of science and evidence, including correct testing of the genuinely ill and correct recording of the epidemic situation. Since this has been neglected for two years, we demand the resignation of the previous advisory experts.
- Drawing up easily applicable concepts for the prevention and early treatment of COVID-19 and also for the inpatient and, if necessary, intensive medical treatment of severe courses.
- The dominance of one single logic, namely the virological logic, must be ended. Other aspects, such as economic, social, psychological, educational and holistic medical considerations must be included.
- Reassuring the population about sufficient medical care for all
- The media should provide wide-ranging comprehensive information, according to the ethical guidelines for journalists formulated in the Press Code, without creating fear and panic.
- Provide programmes to treat the physical and psychological trauma caused by the operations, especially for children and adolescents
- Ending the care crisis through appropriate measures
- Separation of powers, justice and freedom
Who would put their name to such complete idiocy?
You may well ask!
The members of the MWGFD are:
- Prof. Dr. med. Sucharit Bhakdi, Facharzt für Mikrobiologie und Infektionsepidemiologie, ehem. Direktor des Instituts für Medizinische Mikrobiologie und Hygiene der Johannes Gutenberg-Universität Mainz
- Dr. med. Thomas Binder, Kardiologe, Vorstand Aletheia – Medizin und Wissenschaft für Verhältnismässigkeit, Wettingen, Schweiz
- Prof. Dr. med. Arne Burkhardt, Facharzt für Pathologie, Reutlingen
- Prof. Dr.-Ing. Aris Christidis, ehem. Technische Hochschule Mittelhessen, Giessen Fachbereich Mathematik, Naturwissenschaften und Informatik
- Andreas Diemer, Arzt für Allgemeinmedizin und Naturheilverfahren, Diplom- Physiker, Musiker, Leiter der Akademie Lebenskunst und Gesundheit, Gernsbach
- Dr. med. univ. Dr. phil. Christian Fiala, Facharzt für Frauenheilkunde und Geburtshilfe, Arzt für Allgemeinmedizin, Tropenmedizin, Wien
- Dr. med. Heinrich Fiechtner, Hämatologe und Internistischer Onkologe, Stuttgart
- Daniela Folkinger, Psychologische Beraterin, Lehrerin, Thurmansbang
- Dr. med. Margareta Griesz-Brisson, Neurologin, London und Müllheim, BW
- Prof. Dr. med. Dr. phil. Martin Haditsch, Facharzt für Mikrobiologie, Virologie und Infektionsepidemiologie, Hannover
- Dr. Dr. Renate Holzeisen, Rechtsanwältin, Bozen
- Prof. Dr. rer. hum. biol. Ulrike Kämmerer, Humanbiologin, Universitätsklinikum Würzburg
- Prof. Dr. Christian Kreiß, Volkswirtschaftler, Hochschule Aalen
- Prof. Dr. Christof Kuhbandner, Pädagogische Psychologie, Universität Regensburg
- Prof. Dr. med. Walter Lang, Pathologe, Hannover
- Werner Möller, Intensivpfleger und Atmungstherapeut, Stuttgart, Gründer der Initiative „Pflege für Aufklärung“
- Prof. Dr. Werner Müller, Rechnungswesen, Controlling, Steuern, Fachbereich Wirtschaft der Hochschule Mainz
- Cornelia Reichl, Heilpraktikerin, Passau
- Prof. Dr. rer. nat. Karina Reiß, Mikrobiologie, Quincke-Forschungszentrum der Christian-Albrechts-Universität zu Kiel
- Dr. med. Konstantina Rösch, Allgemeinärztin, Graz
- Prof. Dr. phil. Franz Ruppert, Psychotraumatologie, psychologische Psychotherapie, Psychologie, Katholische Stiftungshochschule München
- Heiko Schöning, Arzt, Hamburg
- Univ.-Prof. Dr. med. Dr. rer. nat. M. Sc. Christian Schubert, Klinik für Medizinische Psychologie, Medizinische Universität Innsbruck.
- Prof. Dr. Martin Schwab, Lehrstuhl für Bürgerliches Recht, Verfahrens- und Unternehmensrecht, Universität Bielefeld
- Univ.-Prof. Dr. med. Andreas Sönnichsen, Abteilung für Allgemeinmedizin und Familienmedizin, Medizinische Universität Wien, bis Januar 2021 Vorsitzender des Deutschen Netzwerks Evidenzbasierte Medizin,
- Priv. Doz. Dr. med. Josef Thoma, HNO-Arzt, Berlin.
- Prof. Dr. Hans-Werner Vohr, Immunologie und Immuntoxikologie, Universität Düsseldorf.
- Prof. Dr. Dr. Daniel von Wachter, Professor für Philosophie an der Internationalen Akademie für Philosophie im Fürstentum Liechtenstein
- Prof. Dr. Harald Walach, klinischer Psychologe, Gesundheits-wissenschaftler, Leiter des Change Health Science Instituts, Berlin
- Dr. med. Ronald Weikl, Facharzt für Frauenheilkunde und Geburtshilfe, Praktischer Arzt, Naturheilverfahren, Passau
- Ernst Wolff, Autor, Finanzexperte und freier Journalist, Berlin
As we see, the ‘Society of Physicians and Scientists for Health, Freedom and Democracy’ does not just contain physicians and scientists but also – contrary to its name – simple non-academic loons. And, of course, an important member – the main reason for today blogging about it – it includes SCAM practitioners and – most importantly – Prof Harald Walach who has featured so regularly on this blog.
There has been much discussion recently about the best way to persuade anti-vaxxers to change their minds. As they seem completely resistant to the scientific consensus, this has so far not been an easy task. Many experts tell us that we foremost must not ridicule them. I think the ’10 demands’ show that this is also not necessary because they are so very efficient in doing that themselves.
My second entry into this competition is so special that I will show you its complete, unadulterated abstract. Here it is:
Objective
To compare the safety differences between Chinese medicine (CM) and Western medicine (WM) based on Chinese Spontaneous Reporting Database (CSRD).
Methods
Reports of adverse events (AEs) caused by CM and WM in the CSRD between 2010 and 2011 were selected. The following assessment indicators were constructed: the proportion of serious AEs (PSE), the average number of AEs (ANA), and the coverage rate of AEs (CRA). Further comparisons were also conducted, including the drugs with the most reported serious AEs, the AEs with the biggest report number, and the 5 serious AEs of interest (including death, anaphylactic shock, coma, dyspnea and abnormal liver function).
Results
The PSE, ANA and CRA of WM were 1.09, 8.23 and 2.35 times higher than those of CM, respectively. The top 10 drugs with the most serious AEs were mainly injections for CM and antibiotics for WM. The AEs with the most reports were rash, pruritus, nausea, dizziness and vomiting for both CM and WM. The proportions of CM and WM in anaphylactic shock and coma were similar. For abnormal liver function and death, the proportions of WM were 5.47 and 3.00 times higher than those of CM, respectively.
Conclusion
Based on CSRD, CM was safer than WM at the average level from the perspective of adverse drug reactions.
__________________
Perhaps there will be readers who do not quite understand why I find this paper laughable. Let me try to answer their question by suggesting a few other research subjects of similar farcicality.
- A comparison of the safety of vitamins and chemotherapy.
- A study of the relative safety of homeopathic remedies and antibiotics.
- An investigation into the risks of sky diving in comparison with pullover knitting.
- A study of the pain caused by an acupuncture needle compared to molar extraction.
In case my point is still not clear: comparing the safety of one intervention to one that is fundamentally different in terms of its nature and efficacy does simply make no sense. If one wanted to conduct such an investigation, it would only be meaningful, if one would consider the risk-benefit balance of both treatments.
The fact that this is not done here discloses the above paper as an embarrassing attempt at promoting Traditional Chinese Medicine.
PS
In case you wonder about the affiliations of the authors and their support:
- School of Management, Nanjing University of Posts and Telecommunications, Nanjing, 210003, China
Jian-xiang Wei - School of Internet of Things, Nanjing University of Posts and Telecommunications, Nanjing, 210003, China
Zhi-qiang Lu, Guan-zhong Feng & Yun-xia Zhu
The review was supported by the Major Project of Philosophy and Social Science Research in Jiangsu Universities and the Postgraduate Research & Practice Innovation Program of Jiangsu Province, China.
Yesterday, my new book arrived on my doorstep.
WHAT JOY!
Its full title is CHARLES, THE ALTERNATIVE PRINCE. AN UNAUTHORISED BIOGRAPHY. I guess that it also clarifies its contents. In case you want to know more, here is the full list of topics:
Foreword by Nick Ross v 
1. Why this Book? 1
2. Why this Author? 5
3. Words and Meanings 10
4. How Did It All Start? 13
5. Laurens van der Post 17
6. The British Medical Association 25
7. Talking Health 31
8. Osteopathy 37
9. Chiropractic 43
10. The Foundation of Integrated Health 50
11. Open Letter to The Times 56
12. The Model Hospital 62
13. Integrated Medicine 66
14. The Gerson Therapy 73
15. Herbal Medicine 77
16. The Smallwood Report 82
17. World Health Organisation 90
18. Traditional Chinese Medicine 96
19. The ‘GetWellUK’ Study 100
20. Bravewell 106
21. Duchy Originals Detox Tincture 110
22. Charles’ Letters to Health Politicians 115
23. The College of Medicine and Integrated Health 120
24. The Enemy of Enlightenment 126
25. Harmony 132
26. Antibiotic Overuse 142
27. Ayurvedic Medicine 147
28. Social Prescribing 154
29. Homeopathy 160
30. Final Thoughts 169
Glossary 180
End Notes 187
Index 202
In case you want to know more, here is chapter 1 of my book:
Over the past two decades, I have supported efforts to focus healthcare on the particular needs of the individual patient, employing the best and most appropriate forms of treatment from both orthodox and complementary medicine in a more integrated way.[1]
The Prince of Wales 1997
This is a charmingly British understatement, indeed! Charles has been the most persistent champion of alternative medicine in the UK and perhaps even in the world. Since the early 1980s, he has done everything in his power
- to boost the image of alternative medicine,
- to improve the status of alternative practitioners,
- to make alternative therapies more available to the general public,
- to lobby that it should be paid for by the National Health Service (NHS),
- to ensure the press reported favourably about the subject,
- to influence politicians to provide more support for alternative medicine.
He has fought for these aims on a personal, emotional, political, and societal level. He has used his time, his intuition, his influence, and occasionally his money to achieve his goals. In 2010, he even wrote a book, ‘Harmony’, in which he explains his ideas in some detail[2] (discussed in chapter 25, arguably the central chapter of this biography). Charles has thus become the undisputed champion of the realm of alternative medicine. For that he is admired by alternative practitioners across the globe.
Yet, his relentless efforts are not appreciated by everyone (another British understatement!). There are those who view his interventions as counter-productive distractions from the important and never-ending task to improve modern healthcare. There are those who warn that integrating treatments of dubious validity into our medical routine will render healthcare less efficient. There are those who claim that the Prince’s preoccupation with matters that he is not qualified to fully comprehend is a disservice to public health. And there are those who insist that the role of the heir to the throne does not include interfering with health politics.
- So, are Charles’ ideas new and exciting?
- Or are they obsolete and irrational?
- Has Charles become the saviour of UK healthcare?
- Or has he hindered progress?
- Is he a role model for medical innovators?
- Or the laughing stock of the experts?
- Is he a successful reformer of healthcare?
- Or are his concepts doomed to failure?
Charles appears to evade critical questions of this nature. Relying on his intuition, he unwaveringly pursues and promotes his personal beliefs, regardless of the evidence (Box 1). He believes strongly in his mission and is, as most observers agree, full of good intentions. If he even notices any criticism, it is merely to reaffirm his resolve and redouble his efforts. He is reported to work tirelessly, and one could easily get the impression that he is obsessed with his idea of integrating alternative medicine into conventional healthcare.
I have observed Charles’ efforts around alternative medicine for the last 30 years. Occasionally, I was involved in some of them. For 19 years, I have headed the world’s most productive team of researchers in alternative medicine. This background puts me in a unique position to write this account of Charles’ ‘love affair’ with alternative medicine. It is not just a simple outline of Charles’ views and actions but also a critical analysis of the evidence that does or does not support them. In writing it, I pursue several aims:
-
- I want to summarise this part of medical history, as it amounts to an important contribution to the recent development of alternative medicine in the UK and beyond.
- I hope to explain how Charles and other enthusiasts of alternative medicine think, what motivates them and what logic they follow.
- I will contrast Charles’ beliefs with the published evidence as it pertains to each of the alternative modalities (treatments and diagnostic methods) he supports.
- I want to stimulate my readers’ ability to think critically about health in general and alternative medicine in particular.
My book will thus provide an opportunity to weigh the arguments for and against alternative medicine. In that way, it might even provide Charles with a substitute for a discussion about his thoughts on alternative medicine which, during almost half a century, he so studiously managed to avoid.
In pursuing these aims there are also issues that I hope to avoid. From the start, I should declare an interest. Charles and I once shared a similar enthusiasm for alternative medicine. But, as new evidence emerged, I changed my mind and he did not. This led to much-publicised tensions and conflicts. Yet it would be too easy to dismiss this book as an act of vengeance. It isn’t. I have tried hard to be objective and dispassionate, setting out Charles’ claims as fairly as I can and comparing them with the most reliable evidence. As much as possible:
-
- I do not want my personal discords with Charles to get in the way of objectivity.
- I do not want to be unfairly dismissive of Charles and his ambitions.
- I do not want to be disrespectful about anyone’s deeply felt convictions.
- I do not aim to weaken the standing of our royal family.
My book follows Charles’ activities in roughly chronological order. Each time we encounter a new type of alternative medicine, I will try to contrast Charles’ perceptions with the scientific evidence that was available at the time. Most chapters of this book are thus divided into four parts
-
- A short introduction
- Charles’ views
- An outline of the evidence
- A comment about the consequences
While writing this book, one question occurred to me regularly: Why has nobody so far written a detailed history of Charles’s passion for alternative medicine? Surely, the account of Charles ‘love affair’ with alternative medicine is fascinating, diverse, revealing, and important!
I hope you agree.
BOX 1
The nature of evidence in medicine and science
- Evidence is the body of facts, often created through experiments under controlled conditions, that lead to a given conclusion.
- Evidence must be neutral and give equal weight to data that fail to conform to our expectations.
- Evidence is normally used towards rejecting or supporting a hypothesis.
- In alternative medicine, the most relevant hypotheses often relate to the efficacy of a therapy.
- Such hypotheses are best tested with controlled clinical trials where a group of patients is divided into two subgroups and only one is given the therapy to be tested; subsequently the results of both groups are compared.
- Experience does not amount to evidence and is a poor indicator of efficacy; it can be influenced by several phenomena, e.g. placebo effects, natural history of the condition, regression towards the mean.
- If the results of clinical studies are contradictory, the best available evidence is usually a systematic review of the totality of rigorous trials.
- Systematic reviews are methods to minimise random and selection biases. The most reliable systematic reviews are, according to a broad consensus, those from the Cochrane Collaboration.
[1] https://www.princeofwales.gov.uk/speech/article-hrh-prince-wales-titled-science-and-homeopathy-must-work-harmony-daily-telegraph
[2] https://www.amazon.co.uk/Harmony-New-Way-Looking-World/dp/0007348037