risk/benefit
Today, a 3-day conference is starting on ‘INTEGRATIVE MEDICINE’ (IM) in London. Dr. Michael Dixon, claims that it is going to be the biggest such conference ever and said that it ‘will make history’. Dixon is an advisor to Prince Charles, chair of the College of Medicine and Integrated Health (CoMIH, of which Charles is a patron), and joint-chair of the congress. The other co-chair is Elizabeth Thompson. Both have been the subject of several previous posts on this blog.
Dixon advertised the conference by commenting: “I am seeing amongst by younger colleagues, the newly trained GPs, that they have a new attitude towards healthcare. They are not interested in whether something is viewed as conventional, complementary, functional or lifestyle, they are just looking at what works for their patients. Through this conference, we aim to capture that sense of hope, open-mindedness, and patient-centred care”. I believe that this ‘history-making’ event is a good occasion to yet again review the concept of IM.
The term IM sounds appealing, yet it is also confusing and misleading. The confusion starts with the fact that our American friends call it integrative medicine, while we in the UK normally call it integrated medicine, and it ends with different people understanding different things by IM. In conventional healthcare, for instance, people use the term to mean the integration of social and medical care. In the bizarre world of alternative medicine, IM is currently used to signify the parallel use of alternative and conventional therapies on an equal footing.
Today, there are many different definitions of the latter version of IM. Prince Charles, one of the world’s most ardent supporter of IM, used to simply call it ‘the best of both worlds’. A recent, more detailed definition is a ‘healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies’. This seems to imply that conventional medicine is not healing-orientated, does not account for the whole person, excludes aspects of lifestyle, neglects the therapeutic relationship, is not informed by evidence, and does not employ all appropriate therapies. This, I would argue is a bonanza of strawman fallacies, i.e. the misrepresentation of an opponent’s qualities with a view of defeating him more easily and making one’s own position look superior. Perhaps this is unsurprising – after all, Dixon has been once named ‘a pyromaniac in a field of (integrative) strawmen’.
Perhaps definitions are too theoretical and it is more productive to look at what IM stands for in real life. If you surf the Internet, you can find thousands of clinics that carry the name IM. It will take you just minutes to discover that there is not a single alternative therapy, however ridiculous, that they don’t offer. What is more, there is evidence to show that doctors who are into IM are also often against public health measures such as vaccinations.
The UK ‘Integrated Medicine Alliance’, a grouping within the CoMIH, offers information sheets on all of the following treatments: Acupuncture, Alexander Technique, Aromatherapy, Herbal Medicine, Homeopathy, Hypnotherapy, Massage, ,Naturopathy, Reflexology, Reiki, Tai Chi, Yoga Therapy. The one on homeopathy, for example, tells us that “homeopathy … can be used for almost any condition either alone or in a complementary manner.” Compare this to what the NHS says about it: “homeopathic remedies perform no better than placebos (dummy treatments)”.
This evidently grates with the politically correct definition above: IM is not well-informed about the evidence, and it does use inappropriate treatments. In fact, it is little more than a clumsy attempt to smuggle unproven and disproven alternative therapies into the mainstream of healthcare. It does render medicine not better but will inevitably make it worse, and this is surely not in the best interest of vulnerable patients who, I would argue, have a right to be treated with the most effective therapies currently available.
The conference can perhaps be characterized best by having a look at its sponsors. ‘Gold sponsor’ is WELEDA, and amongst the many further funders of the meeting are several other manufacturers of mistletoe medications for cancer. I just hope that the speakers at this meeting – Dixon has managed to persuade several reputable UK contributors – do not feel too embarrassed when they pass their exhibitions.
I came across an interesting case report recently published in an Austrian magazine. Here is my translation for non-German speakers:
A 42-year-old woman from Vienna has suffered from endometriosis since the age of 13. But it was only 8 years later that she found out what made the first two days of her menstruation so unbearable. She was not allowed to take painkillers to help herself during all that time. Her parents listened to medical “gurus” who distrusted conventional medicine.
“I grew up in a household where almost all illnesses were treated with homeopathy,” she wrote on Twitter. That’s exactly what became the IT expert’s undoing. In a recent interview, she looked back bitterly: “All infections and illnesses were treated with Bach flower remedies or homeopathics. Only in case of accidents or broken bones did my parents drive me to the hospital.” Her father suffered from an auto-immune disease. Because conventional medicine could not help him, he tried alternative approaches. “My parents slowly drifted more and more into this scene. At some point, they stopped listening to ‘normal’ doctors. It went downhill from there.”
As a girl, the Viennese had little chance of standing up to her parents’ “whisperers,” as she calls their esoteric advice. “When I got my period, I was in the worst pain. I fainted every month, even falling off my chair when I did it, once even at school. I vomited until I was so exhausted that I fell asleep.”
She begged her family to finally be allowed to consult a gynecologist. But he didn’t take the teenager seriously at the time and simply wanted to prescribe her the pill without a thorough examination. “I then went to my parents’ homeopathic ‘pill pusher’, who gave me homeopathics against my complaints. I wasn’t allowed to take painkillers because they ‘damage the liver’.” The guru persuaded the young woman that her health problems were her fault. “He said I just didn’t accept myself as a woman and that’s why I was in pain. I thought for a long time that I was just not strong and good enough.”
It wasn’t until she was already in her early 20s that her then-boyfriend took her to a gynecologist who finally took her condition seriously. “The ultrasound showed that I had quite a few cysts in my abdomen.” The diagnosis was also finally certain: she was now officially suffering from endometriosis. She was given the right medicine, and most of the endometriotic growths regressed. But a cyst had wrapped itself tightly around her right ovary, damaging it irrevocably over the years. It had died. “Homeopathy cost me my ovary,” the Viennese woman laments.
The fact that she nevertheless was able to become the mother of two children is thanks to her other ovary, which fortunately remained intact. But the feeling of having been treated wrongly, or not treated at all, for such a long time makes her angry. “I don’t blame my parents today. They have apologized and found their own way out of the gurus’ world of thought and out of the scene,” she emphasizes. “But I blame the people who pretend to be able to cure the majority of all diseases with homeopathy. Yet most of the time they can’t even find the right diagnosis and just give patients some stuff that has no side effects.” She now calls for an end to homeopathy.
_________________________
How many times have I said it?
His remedy might be risk-free, but the homeopath certainly isn’t!
Prof. Fabricio Benedetti is one of the world’s leading experts in the study of placebo effects. I have mentioned his excellent work before, for instance, here where he cautioned that quackery has today one more weapon on its side, which is paradoxically represented by the hard science–supported placebo mechanisms. Now he has expressed his concerns even more clearly in an article entitled “Alternative and natural medicine quackery is on the rise. Here’s why the placebo effect is part of the problem”. Here are a few excerpts from this excellent paper:
For several decades now, many scientists, including me, have been working hard to reveal the full power and scope of the placebo effect — the amazing ability of a simple sugar pill or other non-pharmaceutical “fake intervention” to improve someone’s quality of life. This research has been crucial to giving scientific credibility to a powerful psychological effect. But the advances of science have also backfired, spawning an alternative industry that preys on the vulnerable…
All this means that some alternative medicines can indeed have positive outcomes for patients, though not necessarily through the mechanisms that the therapy’s inventors supposed, but rather through a placebo effect. This holds true for treatments ranging from strange talismans to acupuncture — studies have shown that pain relief is about the same for patients receiving true acupuncture with needles, for example, as for those receiving sham acupuncture with trick needles.
The scientific advances in understanding placebo are fascinating. But one unfortunate outcome of all this work is that profit-seeking companies and individuals now have a new weapon: It is no longer necessary to demonstrate the effectiveness of their proposed therapies; it is enough to assert that these work because of the placebo effect. I receive myriad eccentric proposals for new therapies, ranging from talismans and concoctions to mascots and weird rituals. Their inventors claim that these are capable of inducing substantial health benefits and often seek my endorsement. These proposals have stepped up sharply in recent years. Sadly, the science of the placebo effect is fueling this new breed of pseudoscience…
So, if a salesperson says: “This concoction (or ritual or talisman) will reduce your pain,” it is not necessarily a lie, as the placebo effect may indeed stimulate pain-relieving circuits in the brain. But anyone could truthfully use these words, within limits.
These marketers often overstate the size of the possible response, claim to provide a “cure” rather than pain relief or incorrectly suggest that only their own expensive products will have this effect. Even worse, they may present the products as an alternative to more effective traditional medications for serious conditions such as cancer. In other words, they prey on the vulnerable by making undeliverable promises, purportedly backed by the science of placebo.
Even if taking a placebo can reduce symptoms such as pain, this isn’t always the best course of action. An apparently trivial pain may, for example, be the first sign of something far more serious. Treating the pain alone may prevent diagnosis by a physician or delay important medical treatments…
…Education, communication and honesty are the best friends of medical practice. Patients and health care professionals deserve to know what placebos can and cannot do.
The research and medical communities must be more transparent about the efficacy of many conventional pharmacological and nonpharmacological treatments, by acknowledging that some of them are useful whereas some others are not. Many over-the-counter products have doubtful efficacy, for example. Honesty will boost patients’ trust and confidence in medicine, which are the best antidotes to quackery.
BRAVO PROF BENEDETTI!
Bee venom acupuncture (BVA) is a bizarre form of acupuncture where bee venom is applied via a bee sting or an injection into acupuncture points. The paper below starts with the sentence: “BVA is an effective treatment method for various diseases.” This clearly is not true. In fact, there is no convincing evidence that it is effective for any condition. In addition, it can cause serious harm, even life-threatening anaphylaxis.
With this review, Korean authors tried to estimate the incidence rate of anaphylaxis in response to BVA. 
The investigators searched eight databases (MEDLINE (Pubmed), EMBASE, Cochrane Central Register of Controlled, KISS, KMBASE, Koreamed, OASIS, and NDSL) and systematically reviewed the articles that met the inclusion/exclusion criteria.
Among 225 potentially relevant articles, 49 were selected for this study. The overall incidence rate of anaphylaxis in response to BVA was 0.045% (95% CI 0.028-0.062). Women (0.083%, 95% CI 0.010-0.157) showed a higher incidence rate than men (0.019%, 95% CI -0.018 to 0.055), while the incidence for patients who had a skin test conducted (0.041%, 95% CI 0.011-0.072) was not significantly different compared to that obtained for patients for which there was no information about a skin test (0.047%, 95% CI 0.026-0.067). The publication year affected the incidence rate: it was highest before 1999 (1.099%, 95% CI -1.043 to 3.241), lower between 2000 and 2009 (0.049%, 95% CI 0.025-0.073), and lowest between 2010 and 2021 (0.037% 95% CI 0.014-0.060).
The authors concluded that, in this study, we provide reference data about risk size and factors of BVA-related anaphylaxis, which is essentially required for BVA application in clinics.
I fail to understand why this review included only observational studies and RCTs. Why not case reports? We would need a proper post-marketing surveillance system to obtain reliable incidence figures. Yet, such a system does not exist. Therefore, the data generated by this paper are next to worthless.
All this article does, is confirm that anaphylactic reactions after BVA are a reality. As the treatment has not been proven to be effective for any condition, its risk/benefit balance turns out to be negative. In other words, we should therefore not use BVA.
Many systematic reviews have summarized the evidence on spinal manipulative therapy (SMT) for low back pain (LBP) in adults. Much less is known about the older population regarding the effects of SMT. This paper assessed the effects of SMT on pain and function in older adults with chronic LBP in an individual participant data (IPD) meta-analysis.
Electronic databases were searched from 2000 until June 2020; reference lists of eligible trials and related reviews were also searched. Randomized controlled trials (RCTs) were considered if they examined the effects of SMT in adults with chronic LBP compared to interventions recommended in international LBP guidelines. The authors of trials eligible for the IPD meta-analysis were contacted and invited to share data. Two review authors conducted a risk of bias assessment. Primary results were examined in a one-stage mixed model, and a two-stage analysis was conducted in order to confirm the findings. The main outcomes and measures were pain and functional status examined at 4, 13, 26, and 52 weeks.
A total of 10 studies were retrieved, including 786 individuals; 261 were between 65 and 91 years of age. There was moderate-quality evidence that SMT results in similar outcomes at 4 weeks (pain: mean difference [MD] – 2.56, 95% confidence interval [CI] – 5.78 to 0.66; functional status: standardized mean difference [SMD] – 0.18, 95% CI – 0.41 to 0.05). Second-stage and sensitivity analysis confirmed these findings.
The authors concluded that SMT provides similar outcomes to recommended interventions for pain and functional status in the older adult with chronic LBP. SMT should be considered a treatment for this patient population.
This is a fine analysis. Unfortunately, its results are less than fine. Its results confirm what I have been saying ad nauseam: we do not currently have a truly effective therapy for back pain, and most options are as good or as bad as the rest. This is most frustrating for everyone concerned, but it is certainly no reason to promote SMT as usually done by chiropractors or osteopaths.
The only logical solution, in my view, is to use those options that:
- are associated with the least risks,
- are the least expensive,
- are widely available.
However you twist and turn the existing evidence, the application of these criteria does not come up with chiropractic or osteopathy as an optimal solution. The best treatment is therapeutic exercise initially taught by a physiotherapist and subsequently performed as a long-term self-treatment by the patient at home.
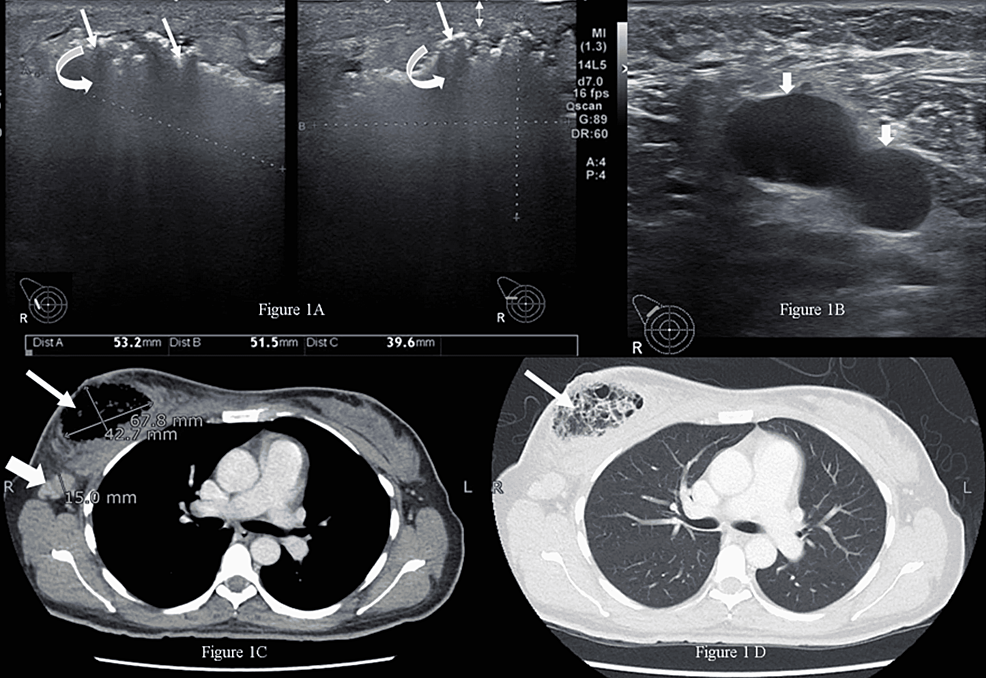
Necrotizing infection (NI) of the breast associated with underlying malignancy is a rare phenomenon characterized by necrosis of breast parenchyma. It can cause a delay in diagnosis and even lead to sepsis. Researchers from the Aga Khan University Hospital in Karachi, PAK, present a case of a 42-year-old woman with NI of the right breast, while on homeopathic treatment for a right breast lump for six months. Tissue culture showed a polymicrobial infection and histopathology established the diagnosis of breast carcinoma. After treating the NI, her breast cancer was managed as per standard guidelines.
The married, nulliparous, diabetic, hypertensive patient was a non-smoker and presented to the emergency room with complaints of fever, severe pain, and foul-smelling bloody discharge from her right breast for two weeks. She had a history of a right breast lump for six months, for which she had been taking oral homeopathic remedies, the names of which were not recorded. On examination, she had a blood pressure of 132/76 mmHg, a pulse of 84 bpm, a temperature of 99 °F, and a respiratory rate of 14 breaths per minute. The right breast was tender and hard, with a 4 x 3-cm necrotic skin patch on the upper half with bleeding and a palpable right axillary lymph node. The rest of the examination was unremarkable.
The patient was advised to undergo a metastatic workup in the emergency room, which included a contrast-enhanced CT (CECT) of the chest, abdomen, and pelvis and a bone scan. The CT confirmed the presence of an air-filled cavity in the right breast with thin septations and enlarged right axillary lymph nodes; however, there was no enhancing mass to suggest neoplasm in either breast. The CT and bone scans were negative for metastasis. The presence of severely tender breast on clinical examination and air within the breast on ultrasound suggested the possibility of NI, which warranted an early surgical intervention to prevent impending sepsis.
Microscopic examination of the debrided tissue revealed an invasive breast carcinoma of no special type [invasive ductal carcinoma (IDC), NST grade III] along with extensive necrosis and dense acute and chronic inflammation. The right axillary node biopsy was positive for nodal metastasis, and the patient was staged as cT4N1MO. A tissue culture showed a few colonies of Staphylococcus aureus and Enterococcus species suggestive of NI. After a discussion at a multidisciplinary tumor board meeting, the patient underwent a right modified radical mastectomy. Her postoperative course was unremarkable.
____________________
I have said it often but I am afraid I need to say it again: the homeopathic remedy might be harmless, but that does not mean that homeopathy is not dangerous.
During their cancer treatment path, cancer patients use numerous drugs,e.g.:
- anticancer medications,
- supportive drugs,
- other prescribed medications,
- herbal remedies,
- other OTC products.
This puts them at risk of significant drug interactions (DIs).
This study describes potential DIs in cancer patients and their prevalence and predictors.
A cross-sectional study was carried out in two centers in the northern West Bank, Palestine. The Lexicomp® Drug Interactions tool (Lexi-Comp, Hudson OH, USA) was applied to check the potential DIs. In addition, the Statistical Package for the Social Sciences (SPSS) was used to show the results and find the associations.
The final analysis included 327 patients. Most of the participants were older than 50 years (61.2%), female (68.5%), and had a solid tumor (74.6%). The total number of potential DIs was 1753, including 1510 drug-drug interactions (DDIs), 24 drug-herb interactions, and 219 drug-food interactions. Importantly, the prevalence of DDIs was 88.1%. In multivariate analysis, the number of potential DDIs significantly decreased with the duration of treatment (p = 0.007), while it increased with the number of comorbidities (p < 0.001) and the number of drugs used (p < 0.001).
The authors concluded that they found a high prevalence of DIs among cancer patients. This required health care providers to develop a comprehensive protocol to monitor and evaluate DIs by improving doctor-pharmacist communication and supporting the role of clinical pharmacists.
What the investigators did not study was the possibility of herb-herb and herb-non-herbal supplement interactions. The reason for this is probably simple: we know too little about these areas to make reasonable judgments. But even in the absence of such considerations, the prevalence of DDIs among cancer patients was high (88.1%). This means that the vast majority of cancer patients had at least one potential DDI. Over half of them were classified as moderately severe or worse.
The lessons seem to be to:
- use only truly necessary drugs and omit all remedies that are of doubtful value,
- educate the public about the risks of interactions,
- be skeptical about the messages of integrative medicine,
- consult a healthcare professional who is competent to make such judgments,
- conduct more rigorous research to increase our knowledge in this complex area.
Osteopathic visceral manipulation (VM) is a bizarre so-called alternative medicine (SCAM) that has been featured on this blog with some regularity, e.g.:
- Osteopathic visceral manipulation: a new study fails to convince anyone
- Visceral manipulation…you couldn’t make it up
- Intravaginal manipulations by (German) osteopaths: a new low point for clinical research into alternative medicine?
- Visceral osteopathy is implausible and does not work … SO, LET’S FORGET ABOUT IT ONCE AND FOR ALL
Rigorous trials fail to show that it works for anything. So, the obvious solution to this dilemma is to conduct dodgy trials!
This study tested the effects of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with polycystic ovary syndrome (PCOS), with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group that received the same hypocaloric diet added to VM to the pelvic organs and their related structures for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months from interventions. Data were described as mean, standard deviation, range, and percentage whenever applicable.
Of 60 Egyptian women with PCOS, 30 patients were included, with baseline mean age, weight, BMI, and a menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Out of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
WHERE TO START?
- Tiny sample size.
- A trail design (A+B vs B) which will inevitably generate a positive result.
- Questionable ethics.
VM is a relatively invasive and potentially embarrassing intervention for any woman; I imagine that this is all the more true in Egypt. In such circumstances, it is mandatory to ask whether a planned study is ethically justifiable. I would answer this question related to an implausible treatment like VM with a straight NO!
I realize that there may be people who disagree with me. But even those guys should accept that, at the very minimum, such a study must be designed such that it leads to a clear answer – is VM effective or not? The present trial merely suggests that the placebo effect associated with VM is powerful (which is hardly surprising for a therapy like VM).
Practitioners of so-called alternative medicine (SCAM) often argue against treating back problems with drugs. They also frequently defend their own therapy by claiming it is backed by published guidelines. So, what should we think about guidelines for the management of back pain?
This systematic review was aimed at:
- systematically evaluating the literature for clinical practice guidelines (CPGs) that included the pharmaceutical management of non-specific LBP;
- appraising the methodological quality of the CPGs;
- qualitatively synthesizing the recommendations with the intent to inform non-prescribing providers who manage LBP.
The authors searched PubMed, Cochrane Database of Systematic Review, Index to Chiropractic Literature, AMED, CINAHL, and PEDro to identify CPGs that described the management of mechanical LBP in the prior five years. Two investigators independently screened titles and abstracts and potentially relevant full text were considered for eligibility. Four investigators independently applied the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument for critical appraisal. Data were extracted for pharmaceutical intervention, the strength of recommendation, and appropriateness for the duration of LBP.
Only nine guidelines with global representation met the eligibility criteria. These CPGs addressed pharmacological treatments with or without non-pharmacological treatments. All CPGs focused on the management of acute, chronic, or unspecified duration of LBP. The mean overall AGREE II score was 89.3% (SD 3.5%). The lowest domain mean score was for applicability, 80.4% (SD 5.2%), and the highest was Scope and Purpose, 94.0% (SD 2.4%). There were ten classifications of medications described in the included CPGs: acetaminophen, antibiotics, anticonvulsants, antidepressants, benzodiazepines, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, oral corticosteroids, skeletal muscle relaxants (SMRs), and atypical opioids.
The authors concluded that nine CPGs, included ten medication classes for the management of LBP. NSAIDs were the most frequently recommended medication for the treatment of both acute and chronic LBP as a first line pharmacological therapy. Acetaminophen and SMRs were inconsistently recommended for acute LBP. Meanwhile, with less consensus among CPGs, acetaminophen and antidepressants were proposed as second-choice therapies for chronic LBP. There was significant heterogeneity of recommendations within many medication classes, although oral corticosteroids, benzodiazepines, anticonvulsants, and antibiotics were not recommended by any CPGs for acute or chronic LBP.
Oddly, this review was published by chiros in a chiro journal. The authors mention that nearly all guidelines the included CPGs recommended non-pharmacological treatments for non-specific LBP, however it was not always delineated as to precede or be used in conjunction with pharmacological intervention.
I find the review interesting because I think it suggests that:
- CPGs are not the most reliable form of evidence. Their guidance depends on how up-to-date they are and on the identity and purpose of the authors.
- Guidelines are therefore often contradictory.
- Back pain is a symptom for which currently no optimal treatment exists.
- The most reliable evidence will rarely come from CPGs but from rigorous, up-to-date, independent systematic reviews such as those from the Cochrane Collaboration.
So, the next time chiropractors osteopaths, acupuncturists, etc. tell you “BUT MY THERAPY IS RECOMMENDED IN THE GUIDELINES”, please take it with a pinch of salt.
Ayush-64 is an Ayurvedic formulation, developed by the Central Council for Research in Ayurvedic Sciences (CCRAS), the apex body for research in Ayurveda under the Ministry of Ayush. Originally developed in 1980 for the management of Malaria, this drug has now been repurposed for COVID-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic properties. Its ingredients are:
| Alstonia scholaris R. Br. Aqueous extract of (Saptaparna) | Bark-1 part |
| Picrorhiza Kurroa Royle Aqueous extract of (Kutki) | Rhizome-1 part |
| Swertia chirata Buch-Ham. Aqueous extract of (Chirata) | Whole plant-1 part |
| Caesalphinia crista, Linn. Fine powder of seed (Kuberaksha) | Pulp-2 parts |
The crucial question, of course, is does AYUSH-64 work?
An open-label randomized controlled parallel-group trial was conducted at a designated COVID care centre in India with 80 patients diagnosed with mild to moderate COVID-19 and randomized into two groups. Participants in the AYUSH-64 add-on group (AG) received AYUSH-64 two tablets (500 mg each) three times a day for 30 days along with standard conventional care. The control group (CG) received standard care alone.
The outcome measures were:
- the proportion of participants who attained clinical recovery on days 7, 15, 23, and 30,
- the proportion of participants with negative RT-PCR assay for COVID-19 at each weekly time point,
- change in pro-inflammatory markers,
- metabolic functions,
- HRCT chest (CO-RADS category),
- the incidence of Adverse Drug Reaction (ADR)/Adverse Event (AE).
Out of 80 participants, 74 (37 in each group) contributed to the final analysis. A significant difference was observed in clinical recovery in the AG (p < 0.001 ) compared to CG. The mean duration for clinical recovery in AG (5.8 ± 2.67 days) was significantly less compared to CG (10.0 ± 4.06 days). Significant improvement in HRCT chest was observed in AG (p = 0.031) unlike in CG (p = 0.210). No ADR/SAE was observed or reported in AG.
The authors concluded that AYUSH-64 as adjunct to standard care is safe and effective in hastening clinical recovery in mild to moderate COVID-19. The efficacy may be further validated by larger multi-center double-blind trials.
I do object to these conclusions for several reasons:
- The study cannot possibly determine the safety of AYUSH-64.
- Even for assessing its efficacy, it was too small.
- The trial design followed the often-discussed A+B vs B concept and is thus prone to generate false-positive results.
I believe that it is highly irresponsible, during a medical crisis like ours, to conduct studies that can only produce unreliable findings. If there is a real possibility that a therapy might work, we do need to test it, but we should take great care that the test is rigorous enough to generate reliable results. This, I think, is all the more true, if – like in the present case – the study was done with governmental support.