risk/benefit
It is not often that I publish a paper with a philosopher in a leading journal of philosophy. In fact, it is the first time, and I am rather proud of it – so much so that I must show my readers (the article is freely available via the link below and I encourage everyone to read the full text) the abstract of our article entitled WHY HOMOEOPATHY IS PSEUDOSCIENCE (Synthese (2022) 200:394):
Homoeopathy is commonly recognised as pseudoscience. However, there is, to date, no systematic discussion that seeks to establish this view. In this paper, we try to fill this gap. We explain the nature of homoeopathy, discuss the notion of pseudoscience, and provide illustrative examples from the literature indicating why homoeopathy fits the
bill. Our argument contains a conceptual and an empirical part.
In the conceptual part, we introduce the premise that a doctrine qualifies as a pseudoscience if, firstly, its proponents claim scientific standing for it and, secondly, if they produce bullshit to defend it, such that, unlike science, it cannot be viewed as the most reliable knowledge on its topic. In the empirical part, we provide evidence that homoeopathy fulfils both criteria. The first is quickly established since homoeopaths often explicitly claim scientificity.
To establish the second, we dive into the pseudo-academic literature on homoeopathy to provide evidence of bullshit in the arguments of homoeopaths. Specifically, we show that they make bizarre ontological claims incompatible with natural science, illegitimately shift the burden of proof to sceptics, and mischaracterise, cherry-pick, and misreport the evidence. Furthermore, we demonstrate that they reject essential parts of established scientific methodology and use epistemically unfair strategies to immunise their doctrine against recalcitrant evidence.
And here is our conclusion:
At the beginning of the paper, we noted that homoeopathy is commonly named one of the prototypical pseudosciences. However, there has been, to date, no comprehensive discussion as to what makes it a pseudoscience. Moreover, the problem is not trivial since the most well-known and influential demarcation criteria, such as Popper’s falsifiability criterion and Kuhn’s problem-solving criterion, cannot account for it, as we have shown. We have tried to fill this research gap using a novel bullshitology-based approach to the demarcation problem. Following this approach, we have argued that homoeopathy should be regarded as pseudoscience because its proponents claim scientific standing for it and produce argumentative bullshit to defend it, thus violating important epistemic standards central to science.
There is a broad, growing, international consensus that homeopathy is a placebo therapy. Even the Germans who have been notoriously fond of their homeopathic remedies are now slowly beginning to accept this fact. But now, a dispute has started to smolder in Germany’s southwest about further training for doctors in homeopathy. In July, the representative assembly of the Baden-Württemberg Medical Association decided to remove the additional title of homeopathy from the further training regulations of doctors. However, the local health ministry has legal control over the medical association and must therefore review the decision, and the minister (Manne Lucha), a member of the Green Party, has stated that he considers the deletion to be wrong.
In a further deepening of the conflict, it has been reported that the chairwoman of the Green Party, Lena Schwelling, considers the ongoing controversy over homeopathy to be exaggerated and wants to preserve people’s freedom of choice. She said she agrees with Health Minister Manne Lucha that naturopathy and homeopathy are important issues for many people. “There is freedom of choice of doctor and therapy in this country. And if people want to choose it, I think they should be allowed to do so.” She also said continuing education for homeopathy for physicians should remain.
Schwelling spoke out against omitting homeopathy from the benefits catalog of the statutory health insurance funds, as demanded by the German Liberal Party, for example: “We are talking about about 0.003 percent of the total costs of the statutory health insurance funds, which flow into homeopathic medicines and treatments. If you saw that as a homeopathic medicine, that would also be at the detection limit, that’s how little money it is. It’s so diluted and so little in this overall budget that it’s not worth arguing about. That’s why I’m very surprised at the crusade some are waging against the issue of homeopathy.”
Recently, a dispute has been smoldering in the southwest about continuing education for homeopathy. The representative assembly of the Baden-Württemberg Medical Association decided in July to remove the additional title of homeopathy from the continuing education regulations. The local health minister, Lucha, has legal oversight of the medical association and must review the amendment statute. However, the minister has already stated that he believes the deletion is wrong.
In response, Schwelling stated it is a “normal process” for the ministry to review what the medical association has proposed. He added that it was perfectly clear that “further training in homeopathy is additional training and does not replace medical studies. Of course, homeopathic doctors also prescribe antibiotics when indicated. An important point why homeopathy should remain in the canon is that you then have the established control mechanisms, for example, in further education.”
Many older adults commonly take multivitamin-multimineral (MVM) supplements to promote health. Yet, evidence on the use of daily MVMs on invasive cancer is limited.
The objective of this study was therefore to determine if a daily MVM decreases total invasive cancer among older adults. For this purpose, a team of researchers performed a randomized, double-blind, placebo-controlled, 2-by-2 factorial trial of a daily MVM and cocoa extract for prevention of cancer and cardiovascular disease (CVD) among 21,442 US adults (12,666 women aged ≥65 y and 8776 men aged ≥60 y) free of major CVD and recently diagnosed cancer. The intervention phase was from June 2015 through December 2020. This article reports on the MVM intervention.
Participants were randomly assigned to daily MVM or placebo. The primary outcome was total invasive cancer, excluding nonmelanoma skin cancer. Secondary outcomes included major site-specific cancers, total CVD, all-cause mortality, and total cancer risk among those with a baseline history of cancer.
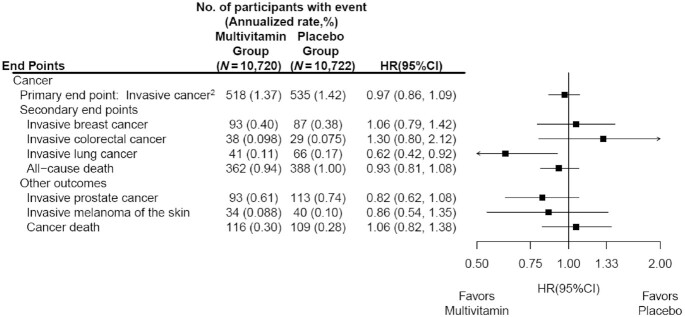
During a median follow-up of 3.6 y, invasive cancer occurred in 518 participants in the MVM group and 535 participants in the placebo group (HR: 0.97; 95% CI: 0.86, 1.09; P = 0.57). No significant effect was observed of a daily MVM on breast cancer (HR: 1.06; 95% CI: 0.79, 1.42) or colorectal cancer (HR: 1.30; 95% CI: 0.80, 2.12). The researchers observed a protective effect of a daily MVM on lung cancer (HR: 0.62; 95% CI: 0.42, 0.92). The composite CVD outcome occurred in 429 participants in the MVM group and 437 participants in the placebo group (HR: 0.98; 95% CI: 0.86, 1.12). MVM use did not significantly affect all-cause mortality (HR: 0.93; 95% CI: 0.81, 1.08). There were no safety concerns.
The authors concluded that a daily MVM supplement, compared with placebo, did not significantly reduce the incidence of total cancer among older men and women. Future studies are needed to determine the effects of MVMs on other aging-related outcomes among older adults.
This is an excellent and important study with clear findings. Nevertheless, the authors insist that several limitations should be considered. First, the COSMOS intervention was relatively short to detect a potential small-to-moderate effect on cancer outcomes given the long duration of time typically required for nutritional interventions to potentially reduce cancer risk. Second, the secondary and exploratory analyses should be interpreted with caution, especially given an overall lack of effect of an MVM on the primary outcome of total invasive cancer. Third, the authors successfully leveraged existing cohorts with mass mailings to expedite recruitment and randomization of 21,442 participants into COSMOS. However, generalizability may be limited, with modest diversity of 10% non-Whites and 2.6% Hispanics plus healthy volunteer bias for participants willing and eligible to enroll in a mail-based clinical trial.
Despite considerable doubts about its effectiveness, osteopathic manipulative treatment (OMT) continues to be used for a range of pediatric conditions. Here is just one example of many osteopaths advertising their services:
I qualified as an Osteopath in 2009 after 4 years of intensive training from the British College of Osteopathic medicine, where I received a distinction for my efforts. After having two children I decided to do a 2-year Postgraduate training in Pediatric Osteopathy from the Osteopathic Centre for Children in London. Whilst at the centre I was lucky enough to meet a wide variety of children from premature babies in a Neonate Hospital ward to children with developmental issues and disabilities, children on the Autistic spectrum, to kids doing exams or experiencing high levels of stress. We also saw lots of children with normal coughs, colds, lumps and bumps.
And the ‘Institute of Osteopathy states this:
Parents visit osteopaths for a range of reasons to support their child’s health. Children, like adults, can be affected by general joint and muscle issues, which is one of the reasons people visit an osteopath. Parents will also take their children to visit an osteopath for a variety of other health reasons that may benefit from osteopathic care.
As osteopathic care is based on the individual needs of the patient, it will vary depending on your child’s age and the diagnosis. Osteopaths generally use a wide range of gentle hands-on techniques that focus on releasing tension, improving mobility and optimising function. This is often used together with exercise and helpful advice. Some osteopaths have been trained in very gentle techniques which are particularly suitable to assess and treat very young children, including new-borns. You do not need to consult your GP before you visit an osteopath, although you may wish to do so.
So, how good or bad is osteopathy for kids? Our systematic review wanted to find out. Specifically, the aim of this paper is to update our previous systematic review (SR) initially published in 2013 by critically evaluating the evidence for or against this treatment.
Eleven databases were searched (January 2012 to November 2021). Only randomized clinical trials (RCTs) of OMT in pediatric patients compared with any type of controls were considered. The Cochrane risk-of-bias tool was used. In addition, the quality of the evidence was rated using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria, as recommended by the Cochrane Collaboration.
Thirteen trials met the eligibility criteria, of which four could be subjected to a meta-analysis. The findings show that, in preterm infants, OMT has little or no effect on reducing the length of hospital stay (standardized mean difference (SMD) -0.03; 95% confidence interval (CI) -0.44 to 0.39; very low certainty of the evidence) when compared with usual care alone. Only one study (8.3%) was judged to have a low risk of bias and showed no effects of OMT on improving exclusive breastfeeding at one month. The methodological quality of RCTs published since 2013 has improved. However, adverse effects remain poorly reported.
We concluded that the quality of the primary trials of OMT has improved during recent years. However, the quality of the totality of the evidence remains low or very low. Therefore, the effectiveness of OMT for selected pediatric populations remains unproven.
These days, it is not often that I am the co-author of a systematic review. So, allow me to discuss one of my own papers for a change by making a few very brief points:
- Considering how many osteopaths treat children, the fact that only 13 trials exist is shameful. To me, it suggests that the osteopathic profession has little interest in research.
- The finding that adverse effects are poorly reported is even more shameful, in my view. It suggests that the few osteopaths who do some research don’t mind violating research ethics.
- The fact that overall our review fails to yield good evidence that osteopathy is effective for any pediatric condition is the most shameful finding of them all. It means that osteopaths are either not informed about the evidence for their own approach, or that they are informed but don’t give a hoot and treat kids regardless. In both cases, they behave unethically.
Cannabis use is a frequently-discussed subject, not just in the realm of so-called alternative medicine (SCAM). In general, SCAM advocates view it as an herbal medicine and recommend it for all sorts of conditions. They also often downplay the risks associated with cannabis use. Yet, these risks might be substantial.
Cannabis potency, defined as the concentration of Δ9-tetrahydrocannabinol (THC), has increased internationally, which could increase the risk of adverse health outcomes for cannabis users. The first systematic review of the association of cannabis potency with mental health and addiction was recently published in ‘The Lancet Psychiatry’.
The authors searched Embase, PsycINFO, and MEDLINE (from database inception to Jan 14, 2021). Included studies were observational studies of human participants comparing the association of high-potency cannabis (products with a higher concentration of THC) and low-potency cannabis (products with a lower concentration of THC), as defined by the studies included, with depression, anxiety, psychosis, or cannabis use disorder (CUD).
Of 4171 articles screened, 20 met the eligibility criteria:
- eight studies focused on psychosis,
- eight on anxiety,
- seven on depression,
- and six on CUD.
Overall, higher potency cannabis, relative to lower potency cannabis, was associated with an increased risk of psychosis and CUD. Evidence varied for depression and anxiety. The association of cannabis potency with CUD and psychosis highlights its relevance in healthcare settings, and for public health guidelines and policies on cannabis sales.
The authors concluded that standardisation of exposure measures and longitudinal designs are needed to strengthen the evidence of this association.
The fact that cannabis use increases the risk of psychosis has long been general knowledge. The notion that the risk increases with increased potency of cannabis seems entirely logical and is further supported by this systematic review. Perhaps it is time to educate the public and make cannabis users more aware of these risks, and perhaps it is time that SCAM proponents negate the harm cannabis can do.
Reports of serious complications of chiropractic manipulation keep on coming. Take this one, for instance:
My daughter went for a routine chiropractor appointment. Now she’s paralysed – 1:20 000 chiropractic neck manipulations result in stroke from vertebral artery dissection.
Or take a recent article by US neurosurgeons:
Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. This study evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement. COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including
- sneezing,
- carrying a heavy load,
- chiropractic manipulation.
Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
The authors concluded that in this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Yes, I know: this study was not meant to investigate the link between chiropractic manipulations and CeAD. The finding that chiropractic manipulation is a predisposing factor for CeAD is entirely incidental. But it is an important finding nevertheless.
Chiropractors will laugh about the notion that manipulation is a risk factor akin to sneezing and thus try to trivialize the danger of their treatments. I would then point out that sneezing is unavoidable and fulfills a purpose. Chiropractic manipulations do neither.
Trevor Zierke is a D.C. who published several videos that have gone viral after saying that “literally 99% of my profession” is a scam. “When I say almost all the usual lines chiropractors tell you are lies, I mean almost all of them,” he stated. Zierke then went on to give examples of issues chiropractors allegedly make up, including someone’s spine being “misaligned,” tension on nerves causing health problems, and someone having back pain because their hips are off-center. “Almost all of these aren’t true,” he concluded.
In a follow-up video, he claimed that the reasons most people are told they need to go to a chiropractor are “overblown or just flat out lies proven wrong by research.” He also noted that, while there are many scams, that “doesn’t mean you can’t get help from a chiropractor.”
In a third TikTok video, Zierke offered some valid reasons to see a chiropractor. He said that one can seek help from a chiropractor if one has musculoskeletal pain that has been ongoing for more than one to two days, and that’s about it. He stated that issues that a chiropractor couldn’t really fix include “GI pain, hormonal issues, nutrition,” among others.
In comments, users were largely supportive of Zierke’s message.
One said: “As a physiotherapist, I’ve been trying to tell this but I don’t want to like offend any chiropractor in doing so,” a commenter shared.
“Working in a chiropractic office, this is fair,” a further user wrote. “I have issues that I know an adjustment will help & other pain that would be better stretched/released.”
In an email, Zierke reiterated the intention of his videos: “I would just like to clarify that chiropractors, in general, are not a scam or are inherently scammers (I myself am a practicing chiropractor), but rather a lot of very popular sales tactics, phrases, and wording used to imply patients need treatment, and methods of treatment, have never been proven to be true,” he explained. “When chiropractors say & use these methods stating things that are not factually true—I believe it’s scammy behavior and practices. There are still a lot of very good, honest, and integral chiropractors out there,” he concluded. “They can provide a lot of help and relief to patients. But that’s unfortunately not the majority, and I’ve heard too many stories of people falling victim to some of these scam-like tactics from bad apple chiropractors.”
None of what DC Zierke said can surprise those who have been following my blog. On the contrary, I could add a few recent posts to his criticism of chiropractic, for example:
- Pediatric chiropractic seems to be on the rise
- Catastrophic injuries after chiropractic treatment
- Chiropractic: “a safe form of treatment”?
- Malpractice Litigation Involving Chiropractic Spinal Manipulation
- Best Practices for the Chiropractic Care of Children
- No effect from adding chiropractic manipulations to exercises for neck pain
- Hurray! The new professional standard by the General Chiropractic Council protects UK chiropractors
- Manual therapy (mainly chiropractic and osteopathy) does not have clinically relevant effects on back pain compared with sham treatment
- Chiropractic Paediatric Courses … it is high time to stop this dangerous nonsense
- Chiropractic ‘subluxation’ is by no means a notion of the past
- Another indirect risk of chiropractic
- And again: chiropractic for infant colic
- Chiropractic misinformation during the COVID-19 pandemic
- The lack of chiropractic ethics: “valid consent was not obtained in a single case”
I rest my case.
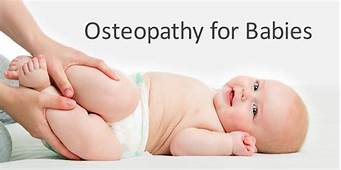
Zinc has been in the limelight recently. The reason is that it has been recommended as a preventative and/or treatment of COVID infections. The basis for such recommendations has been some trial evidence suggesting it is effective for viral respiratory tract infections (RTIs). But the evidence has been full of contradictions which means, we need a systematic review that critically evaluated the totality of the available data.
This systematic review was aimed at evaluating the benefits and risks of zinc formulations compared with controls for the prevention or treatment of acute RTIs in adults.
Seventeen English and Chinese databases were searched in April/May 2020 for randomized clinical trials (RCTs), and from April/May 2020 to August 2020 for SARS-CoV-2 RCTs. Cochrane rapid review methods were applied. Quality appraisals used the Risk of Bias 2.0 and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Twenty-eight RCTs with 5446 participants were identified. None were specific to SARS-CoV-2. Compared with placebo, oral or intranasal zinc prevented 5 RTIs per 100 person-months (95% CI 1 to 8, numbers needed to treat (NNT)=20, moderate-certainty/quality). Sublingual zinc did not prevent clinical colds following human rhinovirus inoculations (relative risk, RR 0.96, 95% CI 0.77 to 1.21, moderate-certainty/quality). On average, symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI 0.61 to 3.50, very low-certainty/quality) and 19 more adults per 100 were likely to remain symptomatic on day 7 without zinc (95% CI 2 to 38, NNT=5, low-certainty/quality). There were clinically significant reductions in day 3 symptom severity scores (mean difference, MD -1.20 points, 95% CI -0.66 to -1.74, low-certainty/quality), but not average daily symptom severity scores (standardised MD -0.15, 95% CI -0.43 to 0.13, low-certainty/quality). Non-serious adverse events (AEs) (eg, nausea, mouth/nasal irritation) were higher (RR 1.41, 95% CI 1.17 to 1.69, NNHarm=7, moderate-certainty/quality). Compared with active controls, there were no differences in illness duration or AEs (low-certainty/quality). No serious AEs were reported in the 25 RCTs that monitored them (low-certainty/quality).
The authors concluded that in adult populations unlikely to be zinc deficient, there was some evidence suggesting zinc might prevent RTIs symptoms and shorten duration. Non-serious AEs may limit tolerability for some. The comparative efficacy/effectiveness of different zinc formulations and doses were unclear. The GRADE-certainty/quality of the evidence was limited by a high risk of bias, small sample sizes and/or heterogeneity. Further research, including SARS-CoV-2 clinical trials is warranted.
The authors provide a short comment on the assumed mode of action of zinc. The rationale for topical intranasal and sublingual zinc is based on the in vitro effects of zinc ions that can inhibit viral replication, stabilize cell membranes and reduce mucosal inflammation. Other conceivable mechanisms include the activation of T lymphocytes, monocytes, and granulocytes.
The authors also remind us to be cautious: clinicians and consumers need to be aware that considerable uncertainty remains regarding the clinical efficacy of different zinc formulations, doses, and administration routes, and the extent to which efficacy might be influenced by the ever changing epidemiology of the viruses that cause RTIs. The largest body of evidence comes from sublingual lozenges and zinc gluconate and acetate salts, suggesting these are suitable choices. Yet, this does not mean that other administration routes and zinc salts are less effective. The new evidence on the prophylactic effects of low-dose nasal sprays adds weight to the otherwise inconclusive findings from the handful of RCTs evaluating zinc nasal sprays or gels for acute treatment. A minimum therapeutic dose for zinc is also yet to be determined. An earlier review suggested the minimum dose for sublingual lozenges is 75 mg. However, the present analysis does not support this conclusion. Furthermore, a daily oral dose of 15 mg has been shown to upregulate lymphocytes within days, so it is plausible that much lower doses might also be effective.
It has been reported that a recent inspection from the Care Quality Commission (CQC) found that the diagnostic imaging service at AECC University College in Parkwood Road, Bournemouth, requires improvement in three out of four areas – including patient safety. This is surprising not least because the AECC prides itself on being “a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence.” 
The unannounced inspection in May this year resulted in several demands for the service to improve upon. For example, the CQC report said staff “did not receive all of the training they needed to keep patients safe” and that patient chaperones “did not receive chaperone training”. Moreover, managers were reported as not always ensuring staff were competent to operate certain equipment. In fact, there was no record of staff competencies which meant inspectors “could not tell if staff had been trained to use equipment”. General cleanliness was also found lacking in relation to certain procedures, namely no sink in any of the site’s nine ultrasound rooms (including those for transvaginal scans) – meaning staff carrying out ultrasound scanning did not have access to a clinical handwashing facility.
The CQC states on its website that it “is the independent regulator of health and adult social care in England. We make sure health and social care services provide people with safe, effective, compassionate, high-quality care and we encourage care services to improve. We monitor, inspect and regulate services. Then we publish what we find, including performance ratings, to help people choose care. Where we find poor care, we will use our powers to take action.”
No doubt, these are laudable aims. What I find, however, disappointing is that the CQC’s inspection of the AECC did not question the nature of some of the courses taught by the AECC. Earlier this year, I reported in a blog post that the AECC has announced a new MSc ‘Musculoskeletal Paediatric Health‘. This motivated me to look into the evidence for such a course. This is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
____________________
Isn’t that a question the CQC should have asked?
Olivia Newton-John, actress, singer, and advocate of so-called alternative medicine (SCAM) has died following a lengthy battle with breast cancer. Her husband announced her death yesterday: “Dame Olivia Newton-John (73) passed away peacefully at her Ranch in Southern California this morning, surrounded by family and friends,” the post read. “We ask that everyone please respect the family’s privacy during this very difficult time. Olivia has been a symbol of triumphs and hope for over 30 years sharing her journey with breast cancer. Her healing inspiration and pioneering experience with plant medicine continues with the Olivia Newton-John Foundation Fund, dedicated to researching plant medicine and cancer.” 
Olivia was born on 26 September 1948 in Cambridge, UK. She came from a remarkable family. Her maternal grandfather was the Nobel Prize-winning physicist Max Born. She was thus the niece of my late friend Gustav Born. Newton-John’s father was an MI5 officer on the Enigma project at Bletchley Park who took Rudolf Hess into custody during World War II. After the war, he became the headmaster of the Cambridgeshire High School for Boys. He then took up a post in Australia, and young Olivia grew up down under. After starting out as a singer, she had her breakthrough with the film ‘Grease’ which brought her world fame.
Olivia was first diagnosed with breast cancer over 30 years ago and became an outspoken advocate of SCAM. Her cancer came back twice, and in 2017, she was diagnosed to have bone metastases. Meanwhile, she had married John Easterling, the boss of a natural remedy company, in an Incan spiritual ceremony in Peru.
In 2017, she said, “I decided on my direction of therapies after consultation with my doctors and natural therapists and the medical team at my Olivia Newton-John Cancer Wellness and Research Centre in Melbourne”. The Olivia Newton-John Cancer Wellness & Research Centre is a treatment centre of Austin Health, an Australian public hospital. They say that “anyone with a referral from their doctor can be treated here, regardless of the stage of their treatment or insurance status. At the ONJ Centre your care is built around your individual needs. This includes your physical, psychological and emotional health. Every patient is surrounded by a multidisciplinary team of cancer specialists, allied health and wellbeing therapists. Your dedicated treatment team work together to guide you through your optimal treatment pathway. Learn more about the cancer treatments we deliver at the ONJ Centre, how we support you through your care, and find answers to commonly asked questions.”
Their therapies include acupuncture and several other alternatives used for palliation, but the site seems refreshingly free of false claims and quackery. On their website, they say that “palliative care assists patients who have a life limiting illness to be as symptom free as possible. We work with you to meet your emotional, spiritual and practical needs in a holistic way. Our support is also extended to your family and carers.”
Olivia Newton-John’s history with SCAM is revealing. It seems that, by initially using SCAM instead of conventional treatments for her breast cancer in 1992, she worsened her prognosis. When the cancer returned, she opted for the best conventional oncology on offer. Yet, her liking for SCAM had not disappeared. Since 2017, she seems to have used cannabis and other SCAMs as add-ons to conventional medicine. Sadly, she had learned her lesson too late: alternative cancer treatments are a dangerous myth.