risk
Today is WORLD ASTHMA DAY, a good opportunity perhaps to revisit a few of our own evaluations of so-called alternative medicine (SCAM) for asthma. Here are the abstracts of some of our systematic reviews on the subject:
Objective: The objective of this systematic review was to assess the effectiveness of yoga as a treatment option for asthma.
Method: Seven databases were searched from their inception to October 2010. Randomized clinical trials (RCTs) and non-randomized clinical trials (NRCTs) were considered, if they investigated any type of yoga in patients with asthma. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Six RCTs and one NRCT met the inclusion criteria. Their methodological quality was mostly poor. Three RCTs and one NRCT suggested that yoga leads to a significantly greater reduction in spirometric measures, airway hyperresponsivity, dose of histamine needed to provoke a 20% reduction in forced expiratory volume in the first second, weekly number of asthma attacks, and need for drug treatment. Three RCTs showed no positive effects compared to various control interventions.
Conclusions: The belief that yoga alleviates asthma is not supported by sound evidence. Further, more rigorous trials are warranted.
Some clinicians believe that spinal manipulation is an effective treatment for asthma. The aim of this systematic review was to critically evaluate the evidence for or against this claim. Four electronic databases were searched without language restrictions from their inceptions to September 2008. Bibliographies and departmental files were hand-searched. The methodological quality of all included studies was assessed with the Jadad score. Only randomised clinical trials of spinal manipulation as a treatment of asthma were included. Three studies met these criteria. All of them were of excellent methodological quality (Jadad score 5) and all used sham-manipulation as the control intervention. None of the studies showed that real manipulation was more effective than sham-manipulation in improving lung function or subjective symptoms. It is concluded that, according to the evidence of the most rigorous studies available to date, spinal manipulation is not an effective treatment for asthma.
Contradictory results from randomised controlled trials of acupuncture in asthma suggest both a beneficial and detrimental effect. The authors conducted a formal systematic review and meta-analysis of all randomised clinical trials in the published literature that have compared acupuncture at real and placebo points in asthma patients. The authors searched for trials published in the period 1970-2000. Trials had to measure at least one of the following objective outcomes: peak expiratory flow rate, forced expiratory volume in one second (FEV1) and forced vital capacity. Estimates of the standarised mean difference, between acupuncture and placebo were computed for each trial and combined to estimate the overall effect. Hetereogeneity was investigated in terms of the characteristics of the individual studies. Twelve trials met the inclusion criteria but data from one could not be obtained. Individual patient data were available in only three. Standardised differences between means ranging from 0.071 to 0.133, in favour of acupuncture, were obtained. The overall effect was not conventionally significant and it corresponds to an approximate difference in FEV1 means of 1.7. After exploring hetereogenenity, it was found that studies where bronchoconstriction was induced during the experiment showed a conventionally significant effect. This meta-analysis did not find evidence of an effect of acupuncture in reducing asthma. However, the meta-analysis was limited by shortcomings of the individual trials, in terms of sample size, missing information, adjustment of baseline characteristics and a possible bias against acupuncture introduced by the use of placebo points that may not be completely inactive. There was a suggestion of preferential publication of trials in favour of acupuncture. There is an obvious need to conduct a full-scale randomised clinical trial addressing these limitations and the prognostic value of the aetiology of the disease.
Background: Emotional stress can either precipitate or exacerbate both acute and chronic asthma. There is a large body of literature available on the use of relaxation techniques for the treatment of asthma symptoms. The aim of this systematic review was to determine if there is any evidence for or against the clinical efficacy of such interventions.
Methods: Four independent literature searches were performed on Medline, Cochrane Library, CISCOM, and Embase. Only randomised clinical trials (RCTs) were included. There were no restrictions on the language of publication. The data from trials that statistically compared the treatment group with that of the control were extracted in a standardised predefined manner and assessed critically by two independent reviewers.
Results: Fifteen trials were identified, of which nine compared the treatment group with the control group appropriately. Five RCTs tested progressive muscle relaxation or mental and muscular relaxation, two of which showed significant effects of therapy. One RCT investigating hypnotherapy, one of autogenic training, and two of biofeedback techniques revealed no therapeutic effects. Overall, the methodological quality of the studies was poor.
Conclusions: There is a lack of evidence for the efficacy of relaxation therapies in the management of asthma. This deficiency is due to the poor methodology of the studies as well as the inherent problems of conducting such trials. There is some evidence that muscular relaxation improves lung function of patients with asthma but no evidence for any other relaxation technique.
Background: Asthma is one of the most common chronic diseases in modern society and there is increasing evidence to suggest that its incidence and severity are increasing. There is a high prevalence of usage of complementary medicine for asthma. Herbal preparations have been cited as the third most popular complementary treatment modality by British asthma sufferers. This study was undertaken to determine if there is any evidence for the clinical efficacy of herbal preparations for the treatment of asthma symptoms.
Methods: Four independent literature searches were performed on Medline, Pubmed, Cochrane Library, and Embase. Only randomised clinical trials were included. There were no restrictions on the language of publication. The data were extracted in a standardised, predefined manner and assessed critically.
Results: Seventeen randomised clinical trials were found, six of which concerned the use of traditional Chinese herbal medicine and eight described traditional Indian medicine, of which five investigated Tylophora indica. Three other randomised trials tested a Japanese Kampo medicine, marihuana, and dried ivy leaf extract. Nine of the 17 trials reported a clinically relevant improvement in lung function and/or symptom scores.
Conclusions: No definitive evidence for any of the herbal preparations emerged. Considering the popularity of herbal medicine with asthma patients, there is urgent need for stringently designed clinically relevant randomised clinical trials for herbal preparations in the treatment of asthma.
Breathing techniques are used by a large proportion of asthma sufferers. This systematic review was aimed at determining whether or not these interventions are effective. Four independent literature searches identified six randomized controlled trials. The results of these studies are not uniform. Collectively the data imply that physiotherapeutic breathing techniques may have some potential in benefiting patients with asthma. The safety issue has so far not been addressed satisfactorily. It is concluded that too few studies have been carried out to warrant firm judgements. Further rigorous trials should be carried out in order to redress this situation.
__________________________________
So, if you suffer from asthma, my advice is to stay away from SCAM. This might be easier said than done because SCAM practitioners are only too willing to lure asthma patients into their cult. In 2003, we have demonstrated this phenomenon by conducting a survey with chiropractors. Here is our short paper in full:
Classic chiropractic theory claims that vertebral subluxation blocks the flow of ‘‘innate intelligence’’ which, in turn, affects the health of asthma patients (1). Chiropractictors often use spinal manipulation (SM) to correct such malalignments and treat asthma (2). Several clinical trials of chiropractic SM exist, but the most rigorous ones are clearly negative (3,4). Chronic medication with corticosteroids can lead to osteoporosis, a condition, which is a contra-indication to chiropractic SM (5). Given this background, we aimed to determine whether chiropractors would advise an asthma patient on long-term corticosteroids (5 years) to try chiropractic as a treatment for this condition.
All 350 e-mail addresses listed at www.interadcom.com/chiro/html were randomised into two groups. A (deceptive) letter from a (fictitious) patient was sent to group A while group B was asked for advice on chiropractic treatment for asthma as part of a research project. Thus, groups A and B were asked the same question in di¡erent contexts: is chiropractic safe and e¡ective for an asthma patient on long-term steroids. After data collection, respondents from group A were informed that the e-mail had been part of a research project.
Of 97 e-mails in group A, we received 31 responses (response rate = 32% (95% CI, 0.23^ 0.41)). Seventy-four per cent (23 respondents) recommended visiting a chiropractor (95% CI, 0.59^ 0.89). Thirty-five per cent (11 respondents) mentioned minimal or no adverse effects of SM (95% CI, 0.18 ^ 0.52). Three chiropractors responded that some adverse e¡ects exist, e.g. risk of bone fracture, or stroke. Two respondents noted that other investigations (X-rays, spinal and neurological examination) were required before chiropractic treatment. Three respondents suggested additional treatments and one warned about a possible connection between asthma and the measles vaccine. Of 77 e-mails sent to group B, we received 16 responses (response rate = 21% (95% CI, 0.17^ 0.25)). Eleven respondents (69%) recommended visiting a chiropractor (95% CI, 0.46 ^ 0.91). Ten respondents mentioned minimal or no adverse effects of SM (95% CI, 0.39^ 0.87). Five chiropractors responded that adverse effects of SM exist (e.g. bone fracture). Five respondents suggested pre-testing the patient to check bone density, allergy, diet, exercise level, hydration and blood. Additional treatments were recommended by three respondents. The pooled results of groups A and B suggested that the majority of chiropractors recommend chiropractic treatment for asthma and the minority mention any adverse effects.
Our results demonstrate that chiropractic advice on asthma therapy is as readily available over the Internet as it is likely to be misleading. The majority of respondents from both groups (72%) recommended chiropractic treatment. This usually entails SM, a treatment modality which has been demonstrated to be ineffective in rigorous clinical trials (3,4,6). The advice may also be dangerous: the minority of the respondents of both groups (17%) caution of the risk of bone fracture. Our findings also suggest that, for the research question asked, a degree of deception is necessary. The response rate in group B was 12% lower than that of group A, and the answers received differed considerably between groups. In group A, 10% acknowledged the possibility of adverse e¡ects, this figure was 33% in group B. In conclusion, chiropractors readily provide advice regarding asthma treatment, which is often not evidence-based and has the potential to put patients at risk.
__________________________
As I stated above: if you suffer from asthma, my advice is to
stay away from SCAM.
This systematic review and meta-analysis of clinical trials were performed to summarize the evidence of the effects of Urtica dioica (UD) consumption on metabolic profiles in patients with type 2 diabetes mellitus (T2DM).
Eligible studies were retrieved from searches of PubMed, Embase, Scopus, Web of Science, Cochrane Library, and Google Scholar databases until December 2019. Cochran (Q) and I-square statistics were used to examine heterogeneity across included clinical trials. Data were pooled using a fixed-effect or random-effects model and expressed as weighted mean difference (WMD) and 95% confidence interval (CI).
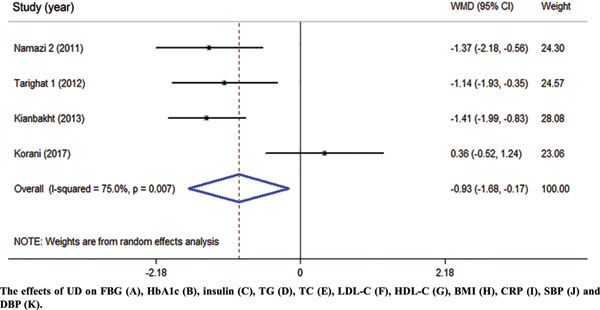
Among 1485 citations, thirteen clinical trials were found to be eligible for the current metaanalysis. UD consumption significantly decreased levels of fasting blood glucose (FBG) (WMD = – 17.17 mg/dl, 95% CI: -26.60, -7.73, I2 = 93.2%), hemoglobin A1c (HbA1c) (WMD = -0.93, 95% CI: – 1.66, -0.17, I2 = 75.0%), C-reactive protein (CRP) (WMD = -1.09 mg/dl, 95% CI: -1.64, -0.53, I2 = 0.0%), triglycerides (WMD = -26.94 mg/dl, 95 % CI = [-52.07, -1.82], P = 0.03, I2 = 90.0%), systolic blood pressure (SBP) (WMD = -5.03 mmHg, 95% CI = -8.15, -1.91, I2 = 0.0%) in comparison to the control groups. UD consumption did not significantly change serum levels of insulin (WMD = 1.07 μU/ml, 95% CI: -1.59, 3.73, I2 = 63.5%), total-cholesterol (WMD = -6.39 mg/dl, 95% CI: -13.84, 1.05, I2 = 0.0%), LDL-cholesterol (LDL-C) (WMD = -1.30 mg/dl, 95% CI: -9.95, 7.35, I2 = 66.1%), HDL-cholesterol (HDL-C) (WMD = 6.95 mg/dl, 95% CI: -0.14, 14.03, I2 = 95.4%), body max index (BMI) (WMD = -0.16 kg/m2, 95% CI: -1.77, 1.44, I2 = 0.0%), and diastolic blood pressure (DBP) (WMD = -1.35 mmHg, 95% CI: -2.86, 0.17, I2= 0.0%) among patients with T2DM.
The authors concluded that UD consumption may result in an improvement in levels of FBS, HbA1c, CRP, triglycerides, and SBP, but did not affect levels of insulin, total-, LDL-, and HDL-cholesterol, BMI, and DBP in patients with T2DM.
Several plants have been reported to affect the parameters of diabetes. Whenever I read such results, I cannot stop wondering whether this is a good or a bad thing. It seems to be positive at first glance, yet I can imagine at least two scenarios where such effects might be detrimental:
- A patient reads about the antidiabetic effects and decides to swap his medication for the herbal remedy which is far less effective. Consequently, the patient’s metabolic control is insufficient.
- A patient adds the herbal remedy to his therapy. Consequently, his blood sugar drops too far and he suffers a hypoglycemic episode.
My advice to diabetics is therefore this: if you want to try herbal antidiabetic treatments, please think twice. And if you persist, do it only under the close supervision of your doctor.
WARNING: SATIRE
This is going to be a very short post. Yet, I am sure you agree that my ‘golden rules’ encapsulate the collective wisdom of so-called alternative medicine (SCAM):
- Conventional treatments are dangerous
- Conventional doctors are ignorant
- Natural remedies are by definition good
- Ancient wisdom knows best
- SCAM tackles the roots of all health problems
- Experience trumps evidence
- People vote with their feet (SCAM’s popularity and patients’ satisfaction prove SCAM’s effectiveness)
- Science is barking up the wrong tree (what we need is a paradigm shift)
- Even Nobel laureates and other VIPs support SCAM
- Only SCAM practitioners care about the whole individual (mind, body, and soul)
- Science is not yet sufficiently advanced to understand how SCAM works (the mode of action has not been discovered)
- SCAM even works for animals (and thus cannot be a placebo)
- There is reliable evidence to support SCAM
- If a study of SCAM happens to yield a negative result, it is false-negative (e.g. because SCAM was not correctly applied)
- SCAM is patient-centered
- Conventional medicine is money-orientated
- The establishment is forced to suppress SCAM because otherwise, they would go out of business
- SCAM is reliable, constant, and unwavering (whereas conventional medicine changes its views all the time)
- SCAM does not need a monitoring system for adverse effects because it is inherently safe
- SCAM treatments are individualized (they treat the patient and not just a diagnostic label like conventional medicine)
- SCAM could save us all a lot of money
- There is no health problem that SCAM cannot cure
- Practitioners of conventional medicine have misunderstood the deeper reasons why people fall ill and should learn from SCAM
QED
I am sure that I have forgotten several important rules. If you can think of any, please post them in the comments section.
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. The characteristics of older adults with debilitating musculoskeletal pain who report SCAM use is also examined. For this purpose, the cross-sectional European Social Survey Round 7 from 21 countries was employed. It examined participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12 months.
Of the 4950 older adult participants, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year.
The most commonly used SCAMs were:
- manual body-based therapies (MBBTs) including massage therapy (17.9%),
- osteopathy (7.0%),
- homeopathy (6.5%)
- herbal treatments (5.3%).
SCAM use was positively associated with:
- younger age,
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe,
- multiple health problems.
(Many years ago, I have summarized the most consistent determinants of SCAM use with the acronym ‘FAME‘ [female, affluent, middle-aged, educated])
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous 12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
I often mutter about the plethora of SCAM surveys that report nothing meaningful. This one is better than most. Yet, much of what it shows has been demonstrated before.
I think what this survey confirms foremost is the fact that the popularity of a particular SCAM and the evidence that it is effective are two factors that are largely unrelated. In my view, this means that more, much more, needs to be done to inform the public responsibly. This would entail making it much clearer:
- which forms of SCAM are effective for which condition or symptom,
- which are not effective,
- which are dangerous,
- and which treatment (SCAM or conventional) has the best risk/benefit balance.
Such information could help prevent unnecessary suffering (the use of ineffective SCAMs must inevitably lead to fewer symptoms being optimally treated) as well as reduce the evidently huge waste of money spent on useless SCAMs.
There is hardly a form of therapy under the SCAM umbrella that is not promoted for back pain. None of them is backed by convincing evidence. This might be because back problems are mostly viewed in SCAM as mechanical by nature, and psychological elements are thus often neglected.
This systematic review with network meta-analysis determined the comparative effectiveness and safety of psychological interventions for chronic low back pain. Randomised controlled trials comparing psychological interventions with any comparison intervention in adults with chronic, non-specific low back pain were included.
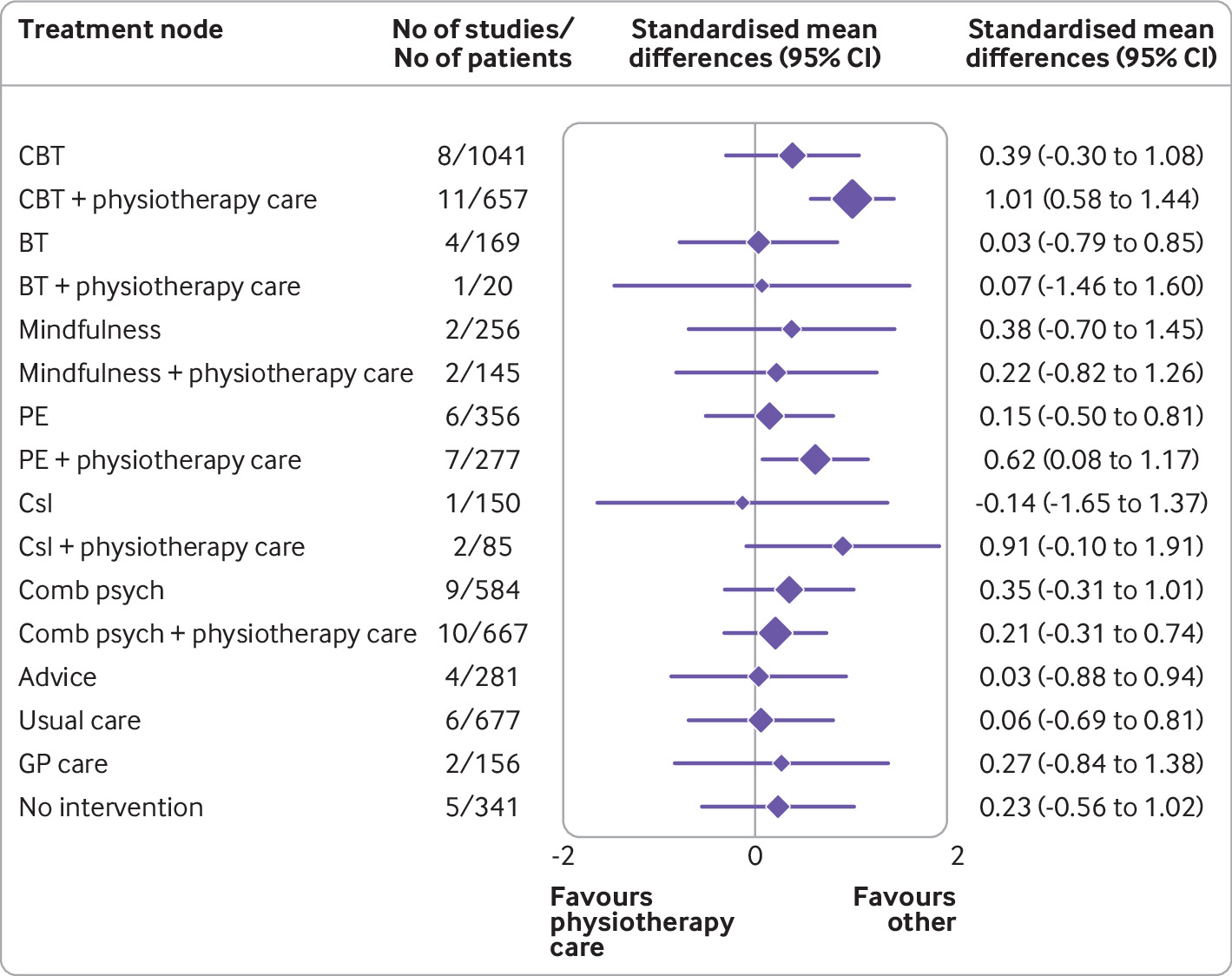
A total of 97 randomised controlled trials involving 13 136 participants and 17 treatment nodes were included. Inconsistency was detected at short term and mid-term follow-up for physical function, and short term follow-up for pain intensity, and were resolved through sensitivity analyses. For physical function, cognitive behavioural therapy (standardised mean difference 1.01, 95% confidence interval 0.58 to 1.44), and pain education (0.62, 0.08 to 1.17), delivered with physiotherapy care, resulted in clinically important improvements at post-intervention (moderate-quality evidence). The most sustainable effects of treatment for improving physical function were reported with pain education delivered with physiotherapy care, at least until mid-term follow-up (0.63, 0.25 to 1.00; low-quality evidence). No studies investigated the long term effectiveness of pain education delivered with physiotherapy care. For pain intensity, behavioural therapy (1.08, 0.22 to 1.94), cognitive behavioural therapy (0.92, 0.43 to 1.42), and pain education (0.91, 0.37 to 1.45), delivered with physiotherapy care, resulted in clinically important effects at post-intervention (low to moderate-quality evidence). Only behavioural therapy delivered with physiotherapy care maintained clinically important effects on reducing pain intensity until mid-term follow-up (1.01, 0.41 to 1.60; high-quality evidence).
Forest plot of network meta-analysis results for physical function at post-intervention. *Denotes significance at p<0.05. BT=behavioural therapy; CBT=cognitive behavioural therapy; Comb psych=combined psychological approaches; Csl=counselling; GP care=general practitioner care; PE=pain education; SMD=standardised mean difference. Physiotherapy care was the reference comparison group
The authors concluded that for people with chronic, non-specific low back pain, psychological interventions are most effective when delivered in conjunction with physiotherapy care (mainly structured exercise). Pain education programmes (low to moderate-quality evidence) and behavioural therapy (low to high-quality evidence) result in the most sustainable effects of treatment; however, uncertainty remains as to their long term effectiveness. Although inconsistency was detected, potential sources were identified and resolved.
The authors’ further comment that their review has identified that pain education, behavioural therapy, and cognitive behavioural therapy are the most effective psychological interventions for people with chronic, non-specific LBP post-intervention when delivered with physiotherapy care. The most sustainable effects of treatment for physical function and fear avoidance are achieved with pain education programmes, and for pain intensity, they are achieved with behavioural therapy. Although their clinical effectiveness diminishes over time, particularly in the long term (≥12 months post-intervention), evidence supports the clinical benefits of combining physiotherapy care with these specific types of psychological interventions at the onset of treatment. The small total sample size at long term follow-up (eg, for physical function, n=6986 at post-intervention v n=2469 for long term follow-up; for pain intensity, n=6963 v n=2272) has resulted in wide confidence intervals at this time point; however, the magnitude and direction of the pooled effects seemed to consistently favour the psychological interventions delivered with physiotherapy care, compared with physiotherapy care alone.
Commenting on their paper, two of the authors, Ferriera and Ho, said they would like to see the guidelines on LBP therapy updated to provide more specific recommendations, the “whole idea” is to inform patients, so they can have conversations with their GP or physiotherapist. Patients should not come to consultations with a passive attitude of just receiving whatever people tell them because unfortunately people still receive the wrong care for chronic back pain,” Ferreira says. “Clinicians prescribe anti-inflammatories or paracetamol. We need to educate patients and clinicians about options and more effective ways of managing pain.”
Is there a lesson here for patients consulting SCAM practitioners for their back pain? Perhaps it is this: it is wise to choose the therapy that has been demonstrated to be effective while having the least potential for harm! And this is not chiropractic or any other form of SCAM. It could, however, well be a combination of physiotherapeutic exercise and psychological therapy.
S-adenosyl methionine – SAMe for short – is a popular dietary supplement available freely via the Internet. It is a naturally occurring methyl radical donor involved in enzymatic transmethylation reactions in humans and animals. It has been used for treating postpartum depression, cholestatic jaundice, osteoarthritis, and numerous other conditions. SAM-e has poor oral bioavailability. SAM-e has so far been thought of as safe. The most frequent adverse effects reported were gastrointestinal, such as nausea, and skin rashes.
I have been involved in two systematic reviews that produced positive evidence for the effectiveness of SAMe:
- One review found “consistent evidence that … S-adenosyl methionine was effective in the management of osteoarthritis.”
- Another review showed that for fibromyalgia “the effects of … S-adenosylmethionine … showed at least one statistically significant improved outcome compared with placebo.”
Now the safety of SAMe has been questioned by new research. A team from Manchester and Kyoto universities reported that the supplement can break down inside the body into substances that cause a wide range of medical problems, including kidney and liver damage. Their study showed that “excess S-adenosylmethionine disrupts rhythms and, rather than promoting methylation, is catabolized to adenine and methylthioadenosine, toxic methylation inhibitors.”
Jean-Michel Fustin, of Manchester University, said experiments that he and his collaborators had carried out had revealed that SAMe breaks down into adenine and methylthioadenosine in the body. These substances are known to be toxic, he added. “This discovery came out of the blue,” Fustin said last week. “When we gave the supplement to mice we expected they would become healthier. But instead we found the opposite. We found that when SAMe breaks down in the body, it produces very toxic molecules, including adenine which causes gout, kidney disease and liver disease.” Fustin added that, although their study was carried out on mice, their results were relevant for humans. “We have not yet tested the supplement on men and women but we have added it to human cells in laboratory cultures and have found it had the same effect as it had on mice.”
Their study, which was funded by the Medical Research Council and the Japanese Society for the Promotion of Science, makes it clear that the health benefits of SAMe are questionable, to say the very least, Fustin added. “It is unclear what dose of it might be safe, so there is a good chance that a safe dose will be exceeded if someone takes this supplement – if a safe dose exists at all.”
I think this press release might interest you:
Science advocates have filed a groundbreaking lawsuit against Boiron, Inc., one of the largest manufacturers of homeopathic products in the world, for deceiving vulnerable consumers with useless products dressed up to look like real medicine. The Center for Inquiry (CFI), which fights on behalf of consumers against pseudoscience, says Boiron routinely made false claims about what its products will treat and heal, misleading the public about the absurd pseudoscientific basis for Boiron products, and even lying about the ingredients their products contain.
“The facts could not be more clear. Boiron profits massively by deceiving consumers in their time of need,” said CFI Vice President and Legal Counsel Nick Little. “Boiron knows its products are worthless junk, so they do everything they can to obscure the truth in order to offload their snake oil upon the unwitting, the ill-informed, and the vulnerable. They can’t be allowed to get away with it any longer.”
Adherents of homeopathy claim, without evidence, that a substance which causes harm to a healthy person will cure anyone else suffering the same type of harm. In homeopathic products, the “active” ingredients are highly diluted mixtures of the so-called cures; the ingredient ends up so diluted, often literally no trace of the original substance remains. Manufacturers like Boiron then sell miniscule amounts of the already incredibly diluted ingredients and promise astounding results.
In its lawsuit, brought under the District of Columbia Consumer Protection Procedures Act, CFI alleges that Boiron sold a plethora of materially identical products, each made up of sugar pills and powders. Despite no scientifically detectable active ingredient, Boiron falsely promised consumers that each item would treat and cure a particular illness, injury, or health condition.
“Boiron sells little pills of sugar with grandiose claims. It’s hard to believe anyone would try to pass off such junk as a surefire way to treat painful skin problems, heal mental health issues, and even to counteract menopause,” said CFI Staff Attorney Aaron D. Green. “But Boiroin has been doing just that by tricking consumers into risking their health and throwing away their money on its fancy faux ‘medicines.’ It’s time for Boiron and all homeopathy hucksters to be held accountable.”
In its complaint, CFI notes that Boiron sells Saccharum officinale as a treatment for “nervous agitation in children after overindulgence.”
“Most parents would rightfully be skeptical of this product if Boiron told them what Saccharum officinale actually is,” said Green. “Table sugar.”
According to recent industry accounts, 85 percent of consumers who purchased homeopathic products did not realize they were homeopathic, and nine out of ten consumers did not even know what the term homeopathic meant.
Apart from selling products they know are useless, Boiron also misrepresented the products’ ingredients. Four Boiron products were analyzed by an independent lab, and, not only were no traces of the supposed active ingredient found, even one of the inactive ingredients could not be scientifically detected.
The Center for Inquiry is currently engaged in other lawsuits regarding homeopathy, including consumer protection cases against megaretailers CVS and Walmart for their sale and marketing of homeopathic products, the matter recently heard by the DC Court of Appeals. CFI is also engaged in an active Freedom of Information Act lawsuit that demands the Department of Health and Human Services grant the public access to the Homeopathic Pharmacopoeia of the United States (HPUS), the “bible of homeopathy” upon which federal regulation of homeopathy is based and to which the industry restricts access but for those willing to pay thousands of dollars for the privilege.
_________________________
All I can add to this is: good luck to the CFI and let’s hope reason will prevail!
An article in PULSE entitled ‘ Revolutionising Chiropractic Care for Today’s Healthcare System’ deserves a comment, I think. Here I give you first the article followed by my comments. The references in square brackets refer to the latter and were inserted by me; otherwise, the article is unchanged.
___________________________
This Chiropractic Awareness Week (4th – 10th April), Catherine Quinn, President of the British Chiropractic Association (BCA), is exploring the opportunity and need for a more integrated healthcare eco-system, putting the spotlight on how chiropractors can help alleviate pressures and support improved patient outcomes.
Chiropractic treatment and its role within today’s health system often prompts questions and some debate – what treatments fit under chiropractic care? Is the profession evidence based? How can it support primary health services, with the blend of public and private practice in mind? This Chiropractic Awareness Week, I want to address these questions and share the British Chiropractic Association’s ambition for the future of the profession.
The role of chiropractic today
The need for effective and efficient musculoskeletal (MSK) treatment is clear – in the UK, an estimated 17.8 million people live with a MSK condition, equivalent to approximately 28.9% of the total population.1 Lower back and neck pain specifically are the greatest causes of years lost to disability in the UK, with chronic joint pain or osteoarthritis affecting more than 8.75 million people.2 In addition to this, musculoskeletal conditions also account for 30% of all GP appointments, placing immense pressure on a system which is already under stress.3 The impact of the COVID-19 pandemic is still being felt by these patients and their healthcare professionals alike. Patients with MSK conditions are still having their care impacted by issues such as having clinic appointments cancelled, difficulty in accessing face-to-face care and some unable to continue regular prescribed exercise.
With these numbers and issues in mind, there is a lot of opportunity to more closely integrate chiropractic within health and community services to help alleviate pressures on primary care [1]. This is something we’re really passionate about at the BCA. However, we recognise that there are varying perceptions of chiropractic care – not just from the public but across our health peers too. We want to address this, so every health discipline has a consistent understanding.
First and foremost, chiropractic is a registered primary healthcare profession [2] and a safe form of treatment [3], qualified individuals in this profession are working as fully regulated healthcare professionals with at least four years of Masters level training. In the UK, chiropractors are regulated by law and required to adhere to strict codes of practice [4], in exactly the same ways as dentists and doctors [5]. At the BCA we want to represent the highest quality chiropractic care, which is encapsulated by a patient centred approach, driven by evidence and science [6].
As a patient-first organisation [7], our primary goal is to equip our members to provide the best treatment possible for those who need our care [8]. We truly believe that working collaboratively with other primary care and NHS services is the way to reach this goal [9].
The benefits of collaborative healthcare
As chiropractors, we see huge potential in working more closely with primary care providers and recognise there’s mutual benefits for both parties [10]. Healthcare professionals can tap into chiropractors’ expertise in MSK conditions, leaning on them for support with patient caseloads. Equally, chiropractors can use the experience of working with other healthcare experts to grow as professionals.
At the BCA, our aim is to grow this collaborative approach, working closely with the wider health community to offer patients the best level of care that we can [11]. Looking at primary healthcare services in the UK, we understand the pressures that individual professionals, workforces, and organisations face [12]. We see the large patient rosters and longer waiting times and truly believe that chiropractors can alleviate some of those stresses by treating those with MSK concerns [13].
One way the industry is beginning to work in a more integrated way is through First Contact Practitioners (FCPs) [14]. These are healthcare professionals like chiropractors who provide the first point of contact to GP patients with MSK conditions [15]. We’ve already seen a lot of evidence showing that primary care services using FCPs have been able to improve quality of care [16]. Through this service MSK patients are also seeing much shorter wait times for treatment (as little as 2-3 days), so the benefits speak for themselves for both the patient and GP [17].
By working as part of an integrated care model, with chiropractors, GPs, physiotherapists and other medical professionals, we’re creating a system that provides patients with direct routes to the treatments that they need, with greater choice. Our role within this system is very much to contribute to the health of our country, support primary care workers and reinforce the incredible work of the NHS [18].
Overcoming integrated healthcare challenges
To continue to see the chiropractic sector develop over the coming years, it’s important for us to face some of the challenges currently impacting progress towards a more integrated healthcare service.
One example is that there is a level of uncertainty about where chiropractic sits in the public/private blend. This is something we’re ready to tackle head on by showing exactly how chiropractic care benefits different individuals, whether that’s through reducing pain, improving physical function or increasing mobility [19]. We also need to encourage more awareness amongst both chiropractors and other healthcare providers about how an integrated workforce could benefit medical professionals and patients alike [20]. For example, there’s only two FCP chiropractors to date, and that’s something we’re looking to change [14].
This is the start of a much bigger conversation and, at the BCA, we’ll continue to work on driving peer acceptance, trust and inclusion to demonstrate the value of our place within the healthcare industry [21]. We’re ready to support the wider health community and primary carers, alleviating some of the pressures already facing the NHS; we’re placed in the perfect position as we have the knowledge and experience to provide essential support [22]. My main takeaway from this year’s Chiropractic Awareness Week would be to simply start a conversation with us about how [23].
About the British Chiropractic Association:
The BCA is the largest and longest-standing association for chiropractors in the UK. As well as promoting international standards of education and exemplary conduct, the BCA supports chiropractors to progress and develop to fulfil their professional ambitions with honour and integrity, at every step [24]. This Chiropractic Awareness Week, the BCA is raising awareness about the rigour, relevance and evidence driving the profession and the association’s ambition for chiropractic to be more closely embedded within mainstream healthcare [25].
- https://bjgp.org/content/70/suppl_1/bjgp20X711497
- https://www.versusarthritis.org/about-arthritis/data-and-statistics/the-state-of-musculoskeletal-health/
- https://www.england.nhs.uk/elective-care-transformation/best-practice-solutions/musculoskeletal/#:~:text=Musculoskeletal%20(MSK)%20conditions%20account%20for,million%20people%20in%20the%20UK
__________________________________
And here are my comments:
- Non sequitur = a conclusion or statement that does not logically follow from the previous argument or statement.
- A primary healthcare profession is a profession providing primary healthcare which, according to standard definitions, is the provision of health services, including diagnosis and treatment of a health condition, and support in managing long-term healthcare, including chronic conditions like diabetes. Thus chiropractors are not in that category.
- This is just wishful thinking. Chiropractic spinal manipulation is not safe!
- “Required to adhere to strict codes of practice”. Required yes, but how often do they not comply?
- This is not true.
- Chiropractic is very far from being “driven by evidence and science”.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Judging from past experience, the primary goal seems to be to protect chiropractors (see, for instance, here).
- Belief is for religion, in healthcare you need evidence. Have you looked at the referral rates of chiropractors to GPs, for instance?
- For chiropractors, the benefit is usually measured in £s.
- To offer the ” best level of care” you need research and evidence, not politically correct statements.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Belief is for religion, in healthcare you need evidence.
- First Contact Practitioners are “regulated, advanced and autonomous health CARE PROFESSIONALS who are trained to provide expert PATIENT assessment, diagnosis and first-line treatment, self-care advice and, if required, appropriate onward referral to other SERVICES.” I doubt that many chiropractors fulfill these criteria.
- Not quite; see above.
- “A lot of evidence”? Really? Where is it?
- “The benefits speak for themselves” only if the treatments used are evidence-based.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Where is the evidence?
- Awareness is not needed as much as evidence?
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Fine, let’s start the conversation: where is your evidence?
- Judging from past experience honor and integrity seem rather thin on the ground (see, for instance here).
The article promised to ‘revolutionize chiropractic care and to answer questions like what treatments fit under chiropractic care? Is the profession evidence-based? Sadly, none of this emerged. Instead, we were offered politically correct platitudes, half-truths, and obscurations.
The revolution in chiropractic, it thus seems, is not in sight.
Today, several UK dailies report about a review of osteopathy just published in BMJ-online. The aim of this paper was to summarise the available clinical evidence on the efficacy and safety of osteopathic manipulative treatment (OMT) for different conditions. The authors conducted an overview of systematic reviews (SRs) and meta-analyses (MAs). SRs and MAs of randomised controlled trials evaluating the efficacy and safety of OMT for any condition were included.
The literature searches revealed nine SRs or MAs conducted between 2013 and 2020 with 55 primary trials involving 3740 participants. The SRs covered a wide range of conditions including
- acute and chronic non-specific low back pain (NSLBP, four SRs),
- chronic non-specific neck pain (CNSNP, one SR),
- chronic non-cancer pain (CNCP, one SR),
- paediatric (one SR),
- neurological (primary headache, one SR),
- irritable bowel syndrome (IBS, one SR).
Although with different effect sizes and quality of evidence, MAs reported that OMT is more effective than comparators in reducing pain and improving the functional status in acute/chronic NSLBP, CNSNP and CNCP. Due
to the small sample size, presence of conflicting results and high heterogeneity, questionable evidence existed on OMT efficacy for paediatric conditions, primary headaches and IBS. No adverse events were reported in most SRs. The methodological quality of the included SRs was rated low or critically low.
The authors concluded that based on the currently available SRs and MAs, promising evidence suggests the possible effectiveness of OMT for musculoskeletal disorders. Limited and inconclusive evidence occurs for paediatric conditions, primary headache and IBS. Further well-conducted SRs and MAs are needed to confirm and extend the efficacy and safety of OMT.
This paper raises several questions. Here a just the two that bothered me most:
- If the authors had truly wanted to evaluate the SAFETY of OMT (as they state in the abstract), they would have needed to look beyond SRs, MAs or RCTs. We know – and the authors of the overview confirm this – that clinical trials of so-called alternative medicine (SCAM) often fail to mention adverse effects. This means that, in order to obtain a more realistic picture, we need to look at case reports, case series and other observational studies. It also means that the positive message about safety generated here is most likely misleading.
- The authors (the lead author is an osteopath) might have noticed that most – if not all – of the positive SRs were published by osteopaths. Their assessments might thus have been less than objective. The authors did not include one of our SRs (because it fell outside their inclusion period). Yet, I do believe that it is one of the few reviews of OMT for musculoskeletal problems that was not done by osteopaths. Therefore, it is worth showing you its abstract here:
The objective of this systematic review was to assess the effectiveness of osteopathy as a treatment option for musculoskeletal pain. Six databases were searched from their inception to August 2010. Only randomized clinical trials (RCTs) were considered if they tested osteopathic manipulation/mobilization against any control intervention or no therapy in human with any musculoskeletal pain in any anatomical location, and if they assessed pain as an outcome measure. The selection of studies, data extraction, and validation were performed independently by two reviewers. Studies of chiropractic manipulations were excluded. Sixteen RCTs met the inclusion criteria. Their methodological quality ranged between 1 and 4 on the Jadad scale (max = 5). Five RCTs suggested that osteopathy compared to various control interventions leads to a significantly stronger reduction of musculoskeletal pain. Eleven RCTs indicated that osteopathy compared to controls generates no change in musculoskeletal pain. Collectively, these data fail to produce compelling evidence for the effectiveness of osteopathy as a treatment of musculoskeletal pain.
It was published 11 years ago. But I have so far not seen compelling evidence that would make me change our conclusion. As I state in the newspapers:
OSTEOPATHY SHOULD BE TAKEN WITH A SIZABLE PINCH OF SALT.
Spinal cord injury after manual manipulation of the cervical spine is rare and has never been described as resulting from a patient performing a self-manual manipulation on his own cervical spine. This seems to be the first well-documented case of this association. 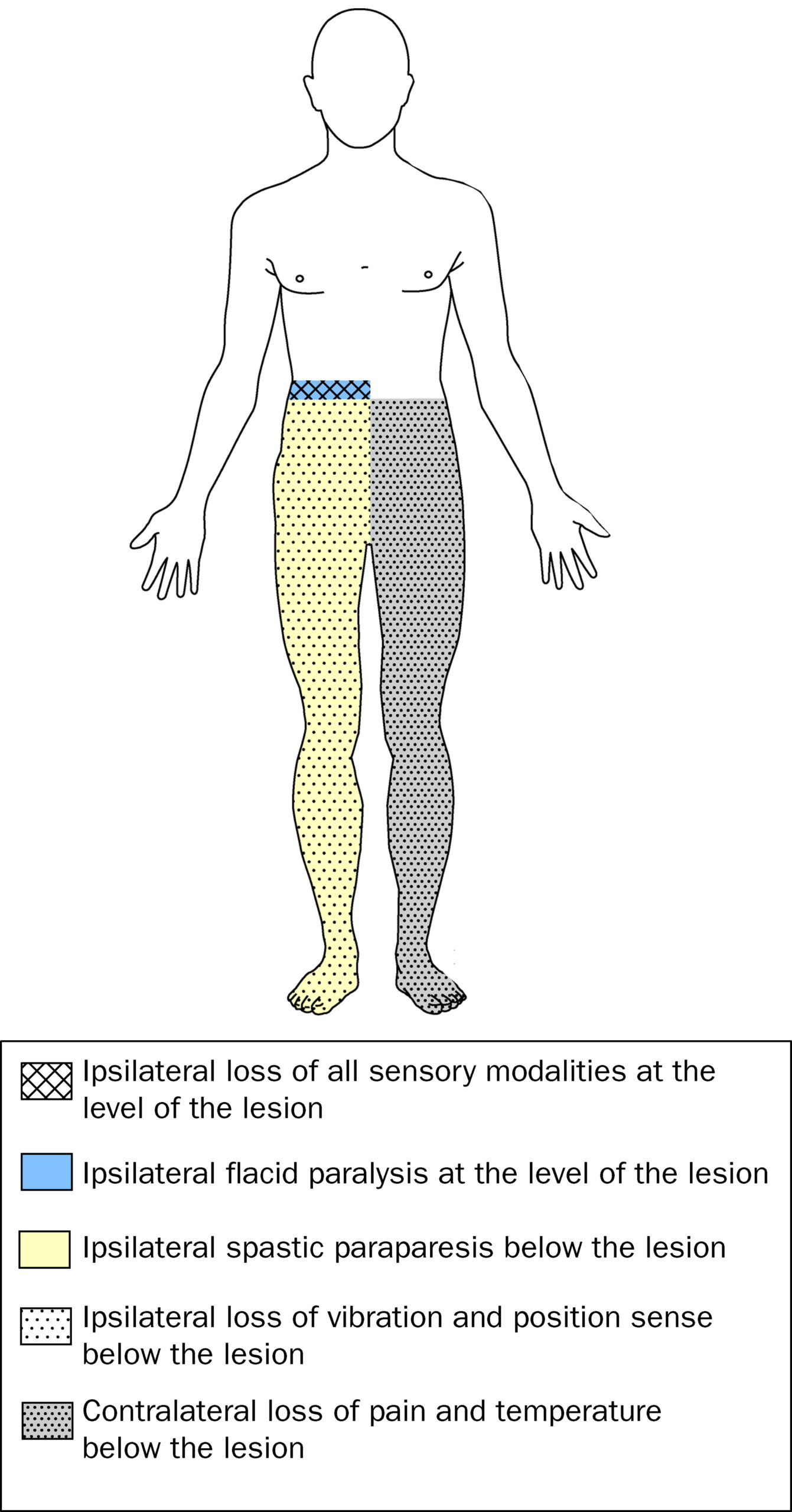
A healthy 29-year-old man developed Brown-Sequard syndrome immediately after performing a manipulation on his own cervical spine. Brown-Sequard syndrome is characterized by a lesion in the spinal cord which results in weakness or paralysis (hemiparaplegia) on one side of the body and a loss of sensation (hemianesthesia) on the opposite side.
Imaging showed large disc herniations at the levels of C4-C5 and C5-C6 with severe cord compression. The patient underwent emergent surgical decompression. He was discharged to an acute rehabilitation hospital, where he made a full functional recovery by postoperative day 8.
The authors concluded that this case highlights the benefit of swift surgical intervention followed by intensive inpatient rehab. It also serves as a warning for those who perform self-cervical manipulation.
I would add that the case also serves as a warning for those who are considering having cervical manipulation from a chiropractor. Such cases have been reported regularly. Here are three of them:
A spinal epidural hematoma is an extremely rare complication of cervical spine manipulation therapy (CSMT). The authors present the case of an adult woman, otherwise in good health, who developed Brown-Séquard syndrome after CSMT. Decompressive surgery performed within 8 hours after the onset of symptoms allowed for complete recovery of the patient’s preoperative neurological deficit. The unique feature of this case was the magnetic resonance image showing increased signal intensity in the paraspinal musculature consistent with a contusion, which probably formed after SMT. The pertinent literature is also reviewed.
Another case was reported of increased signal in the left hemicord at the C4 level on T2-weighted MR images after chiropractic manipulation, consistent with a contusion. The patient displayed clinical features of Brown-Séquard syndrome, which stabilized with immobilization and steroids. Follow-up imaging showed decreased cord swelling with persistent increased signal. After physical therapy, the patient regained strength on the left side, with residual decreased sensation of pain involving the right arm.
A further case was presented in which such a lesion developed after chiropractic manipulation of the neck. The patient presented with a Brown-Séquard syndrome, which has only rarely been reported in association with cervical epidural hematoma. The correct diagnosis was obtained by computed tomographic scanning. Surgical evacuation of the hematoma was followed by full recovery.
Brown-Séquard syndrome after spinal manipulation seems to be a rare event. Yet, nobody can provide reliable incidence figures because there is no post-marketing surveillance in this area.