research
The Buteyko techniques (known in Russia as ‘Voluntary Elimination of Deep Breathing’) are treatments to control respiration developed by the Russian Konstantin Buteyko (1923–2003). Inspired by the methods of respiratory control in yoga, the original Buteyko technique was specifically aimed at easing the symptoms of respiratory conditions, particularly asthma. Konstantin Buteyko postulated that there is a connection between hyperventilation and asthma and that it should be possible to reduce asthma symptoms by deliberate breath control.
The Eucapnic Buteyko method is an adaptation of Buteyko’s original technique which was first introduced in Australia and is now used worldwide. It includes the same focus on ventilation control, but the approach has been re-designed with the aim of achieving better patient-compliance. Both treatments and further variations depend crucially on the cooperation of the patient who has to attend long sessions of learning the technique and must follow the somewhat tedious programme rigorously.
A Cochrane review of Buteyko and similar breathing techniques concluded that “there is no credible evidence regarding the effectiveness of breathing exercises for the clinical symptoms of dysfunctional breathing/hyperventilation syndrome. It is currently unknown whether these interventions offer any added value in this patient group or whether specific types of breathing exercise demonstrate superiority over others.”
Now, a new study adds to this knowledge. This randomized clinical trial included two groups (n = 30 each) of patients with asthma. They received either:
- Buteyko breathing technique (BBT) together with usual therapy (UT)
- or UT alone over a period of 3 months.
The primary outcome comprised the voluntary control pause (CP) after 3 months, secondary outcomes an additional breathhold parameter, forced expiratory volume in 1 s (FEV1), capnovolumetry, exhaled nitric oxide (FeNO), Asthma Control Questionnaire (ACQ) and Nijmegen Questionnaire (NQ), and the use of medication (β2-agonists; inhaled corticosteroids, ICS).
CP showed significant time-by-group interaction [F(1,58.09) = 28.70, p < 0.001] as well as main effects for study group [F(1,58.27) = 5.91, p = 0.018] and time [F(1,58.36) = 17.67, p < 0.001]. ACQ and NQ scores were significantly (p < 0.05 each) improved with BBT. This was associated with reductions in the use of β2-agonists and ICS (p < 0.05 each) by about 20% each. None of these effects occurred in the UT group. While FEV1 and the slopes of the capnovolumetric expiratory phases 2 and 3 did not significantly change, the capnovolumetric threshold volume at tidal breathing increased (p < 0.05) with BBT by about 10 mL or 10%, compared to baseline, suggesting a larger volume of the central airways. No significant changes were seen for FeNO.
The authors concluded that BBT was clinically effective, as indicated by the fact that the improvement in symptom scores and the small increase in bronchial volume occurred despite the significant reduction of respiratory pharmacotherapy. As the self-controlled Buteyko breathing therapy was well-accepted by the participants, it could be considered as supporting tool in asthma therapy being worth of wider attention in clinical practice.
I disagree with this conclusion and think it ought to be changed to:
BBT or a placebo effect was clinically effective.
The reason is that, as many readers have heard me say before, the infamous A+B versus B design does not control for placebo effects and thus is guaranteed to produce a positive result.
The research was conducted by an international team evidently led by the relatively new ARCIM Institute which claims on its website:
The acronym ARCIM stands for Academic Research in Complementary and Integrative Medicine.
The bridging between different treatment and research approaches, disciplines and ways of thinking achieved by the research work of the ARCIM Institute can be symbolized by our logo’s bridge arch. ARCIM integrates this bridge-building metaphor within its name since the Latin term “arcus” means “arch” or “bridge.”
An alarming story of research fraud in the area of so-called alternative medicine (SCAM) is unfolding: Bharat B. Aggarwal, the Indian-American biochemist who worked at MD Anderson Cancer Center, focused his research on curcumin, a compound found in turmeric, and authored more than 125 Medline-listed articles about it. They reported that curcumin had therapeutic potential for a variety of diseases, including various cancers, Alzheimer’s disease and, more recently, COVID-19.
The last of these papers, entitled “Curcumin, inflammation, and neurological disorders: How are they linked?”, was publiched only a few months ago. Here is its abstract:
Background: Despite the extensive research in recent years, the current treatment modalities for neurological disorders are suboptimal. Curcumin, a polyphenol found in Curcuma genus, has been shown to mitigate the pathophysiology and clinical sequalae involved in neuroinflammation and neurodegenerative diseases.
Methods: We searched PubMed database for relevant publications on curcumin and its uses in treating neurological diseases. We also reviewed relevant clinical trials which appeared on searching PubMed database using ‘Curcumin and clinical trials’.
Results: This review details the pleiotropic immunomodulatory functions and neuroprotective properties of curcumin, its derivatives and formulations in various preclinical and clinical investigations. The effects of curcumin on neurodegenerative diseases such as Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS), brain tumors, epilepsy, Huntington’s disorder (HD), ischemia, Parkinson’s disease (PD), multiple sclerosis (MS), and traumatic brain injury (TBI) with a major focus on associated signalling pathways have been thoroughly discussed.
Conclusion: This review demonstrates curcumin can suppress spinal neuroinflammation by modulating diverse astroglia mediated cascades, ensuring the treatment of neurological disorders.
The Anderson Cancer Center initially appeared to approve of Aggarwal’s work. However, in 2012, following concerns about image manipulation raised by pseudonymous sleuth Juuichi Jigen, MD Anderson Cancer Center launched a research fraud probe against Aggarwal which eventually led to 30 of Aggarwal’s articles being retracted. Moreover, PubPeer commenters have noted irregularities in many publications beyond the 30 that have already been retracted. Aggarwal thus retired from M.D. Anderson in 2015.
Curcumin doesn’t work well as a therapeutic agent for any disease – see, for instance, the summary from Nelson et al. 2017:
“[No] form of curcumin, or its closely related analogues, appears to possess the properties required for a good drug candidate (chemical stability, high water solubility, potent and selective target activity, high bioavailability, broad tissue distribution, stable metabolism, and low toxicity). The in vitro interference properties of curcumin do, however, offer many traps that can trick unprepared researchers into misinterpreting the results of their investigations.”
Despite curcumin’s apparent lack of therapeutic promise, the volume of research produced on curcumin grows each year. More than 2,000 studies involving the compound are now published annually. Many of these studies bear signs of fraud and involvement of paper mills. As of 2020, the United States National Institutes of Health (NIH) has spent more than 150 million USD funding projects related to curcumin.
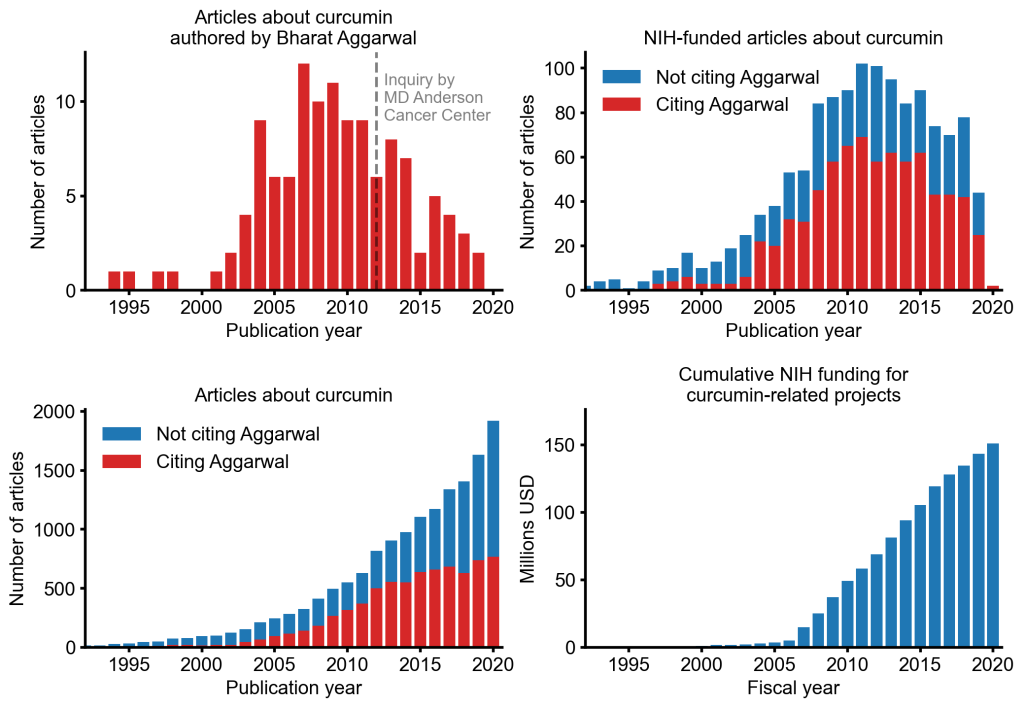
This proliferation of research has fueled curcumin’s popularity as a dietary supplement. It is estimated that the global market for curcumin as a supplement is around 30 million USD in 2020.
The damage done by this epic fraud is huge and far-reaching. Hundreds of millions of taxpayer dollars, countless hours spent toiling by junior scientists, thousands of laboratory animals sacrificed, thousands of cancer patients enrolled in clinical trials for ineffective treatments, and countless people who have eschewed effective cancer treatment in favor of curcumin, were encouraged by research steeped in lies.
Getting old is not nice – but think of the alternative!
I think it was Woody Allen who said something to that extent. But there is a third way, at least this is waht Tai Chi advocates want us to believe.
Utilizing a hybrid design, this study aimed to test whether both long-term and short-term Tai Chi (TC) training are associated with age-related decline in physical function in healthy older adults.
The authors first conducted cross-sectional comparisons among TC-naïve older adults (n = 60, 64.2 ± 7.7 years), TC-expert older adults (n = 27, 62.8 ± 7.6 years, 24.5 ± 12 years experience), and TC-naïve younger adults (n = 15, 28.7 ± 3.2 years) to inform long-term effects of TC training on physical function, including single leg stance time with eyes closed, grip strength, Timed Up and Go, maximum walking speed, functional reach, and vertical jump for lower-extremity power. There were significant differences among the three groups on all the six tests. For most functional tests, TC-experts performed better than age-matched TC-naïve controls and were statistically indistinguishable from young healthy adult controls. Long-term TC training was associated with higher levels of physical function in older adults, suggesting a potential preventative healthy aging effect.
In the randomized longitudinal trial, TC-naïve subjects were randomized (n = 31 to Tai Chi group, n = 29 to usual care control group) to evaluate the short-term effects of TC over 6 months on all outcomes. TC’s short-term impacts on physical function were small and not statistically significant. The impact of short-term training in healthy adults is less clear.
The authors concluded that both potential longer-term preventive effects and shorter-term restorative effects warrant further research with rigorous, adequately powered controlled clinical trials.
Even though the authors imply that their cross-sectional comparison points to a causal effect, this is clearly not true. For instance, it could easily be that people who are somehow destined to keep fit and agile are the ones who keep up Tai Chi. So, rather than being the result of Tai Chi, the proneness to fitness and agility could be the cause for doing Tai Chi.
The authors laudably were aware of these problems and therefore also did an RCT. Sadly this RCT did not yield significant findings. Essentially this means that eitherTai Chi did not work, or the study was naively inadequate, e.g. too small and too short-term.
Thus the authors finish with the usual statement that MORE RESEARCH IS NEEDED. This might be true, but is a definitive RCT likely?
I don’t think so.
A long time ago I had designed such a definitive study. It needed to be very large considering that many participants might drop out. Crucially, it also had to be long- term, i.e. years, not months.
And what happened to my study?
I never managed to get it funded, mainly because the costs would have been astronomical.
Supportive care is often assumed to be beneficial in managing the anxiety symptoms common in patients in sterile hematology unit. The authors of this study hypothesize that personal massage can help the patient, particularly in this isolated setting where physical contact is extremely limited.
The main objective of this study therefore was to show that anxiety could be reduced after a touch-massage performed by a nurse trained in this therapy.
A single-center, randomized, unblinded controlled study in the sterile hematology unit of a French university hospital, validated by an ethics committee. The patients, aged between 18 and 65 years old, and suffering from a serious and progressive hematological pathology, were hospitalized in sterile hematology unit for a minimum of three weeks. They were randomized into either a group receiving 15-minute touch-massage sessions or a control group receiving an equivalent amount of quiet time once a week for three weeks.
In the treated group, anxiety was assessed before and after each touch-massage session, using the State-Trait Anxiety Inventory questionnaire with subscale state (STAI-State). In the control group, anxiety was assessed before and after a 15-minute quiet period. For each patient, the difference in the STAI-State score before and after each session (or period) was calculated, the primary endpoint was based on the average of these three differences. Each patient completed the Rosenberg Self-Esteem Questionnaire before the first session and after the last session.
Sixty-two patients were randomized. Touch-massage significantly decreased patient anxiety: a mean decrease in STAI-State scale score of 10.6 [7.65-13.54] was obtained for the massage group (p ≤ 0.001) compared with the control group. The improvement in self-esteem score was not significant.
The authors concluded that this study provides convincing evidence for integrating touch-massage in the treatment of patients in sterile hematology unit.
I find this conclusion almost touching (pun intended). The wishful thinking of the amateur researchers is almost palpable.
Yes, I mean AMATEUR, despite the fact that, embarrassingly, the authors are affiliated with prestigeous institutions:
- 1Nantes Université, CHU Nantes, Service Interdisciplinaire Douleur, Soins Palliatifs et de Support, Médecine intégrative, UIC 22, Nantes, F-44000, France.
- 2Université Paris Est, EA4391 Therapeutic and Nervous Excitability, Creteil, F-93000, France.
- 3Nantes Université, CHU Nantes, Hematology Department, Nantes, F-44000, France.
- 4Nantes Université, CHU Nantes, CRCI2NA – INSERM UMR1307, CNRS UMR 6075, Equipe 12, Nantes, F-44000, France.
- 5Institut Curie, Paris, France.
- 6Université Paris Versailles Saint-Quentin, Versailles, France.
- 7Nantes Université, CHU Nantes, Direction de la Recherche et l’Innovation, Coordination Générale des Soins, Nantes, F-44000, France.
- 8Methodology and Biostatistics Unit, DRCI CHU Nantes CHD Vendée, La Roche Sur Yon, F-85000, France.
- 9Nantes Université, CHU Nantes, Service Interdisciplinaire Douleur, Soins Palliatifs et de Support, Médecine intégrative, UIC 22, Nantes, F-44000, France. [email protected].
So, why do I feel that they must be amateurs?
- Because, if they were not amateurs, they would know that a clinical trial should not aim to show something, but to test something.
- Also, if they were not amateurs, they would know that perhaps the touch-massage itself had nothing to do with the outcome, but that the attention, sympathy and empathy of a therapist or a placebo effect can generate the observed effect.
- Lastly, if they were not amateurs, they would not speak of convincing evidence based on a single, small, and flawed study.
Guest post by Udo Endruscheit
Switzerland is probably the European country with the strangest complementary and alternative medicine (CAM) regulations in the health insurance system. A total of five different CAM methods have been included in the benefits catalogue of basic insurance for several years. However, this is subject to a strange proviso. How did this come about?
As almost everywhere in Europe, there was a desire in Switzerland in the 1990s to include CAM in the public healthcare system, with homeopathy naturally once again taking pole position. Initially, the urge to include five CAM modalities in basic care was granted, but only provisionally. A major project called the “Complementary Medicine Evaluation Programme” (PEK) was launched in 1999 to evaluate the procedures. Even back then, the criteria of efficacy, appropriateness and cost-effectiveness were prerequisites for reimbursement in health insurance. PEK was intended to create clarity here.
One part of PEK has been the well-known Shang/Egger (2005) study on homeopathy “Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy”, which was to become a bone of contention without precedent. However, this did not change the negative result for homeopathy.
In any case, clear conclusions were drawn in Switzerland not only from this study, but also from the results of the other evaluations: the provisional inclusion of the methods in statutory basic insurance was terminated.
This in turn enraged the supporters of CAM methods, who thought they had already reached their goal with the provisional decision in their favour. Apparently, they had not even considered the possibility that scientific evaluations could actually lead to a sudden end to their wishes, which they believed had already been fulfilled.
In fact, in 2009, the friends of ineffective methods succeeded in bringing about one of the referendums for which Switzerland is known under the catchphrase “direct democracy”. And they prevailed – around two thirds of the votes cast were in favour of CAM and its inclusion in the Swiss Federal Constitution. However, it should be borne in mind that the two-thirds figure is put into perspective if the approval, including the low voter turnout, is converted to the proportion of the total electorate. This leaves just 17 per cent who voted for the CAM. And a closer look at the issue of the constitution also reveals that no unconditional protection space has been created for CAM. This is more or less a kind of good behaviour clause for CAM methods, but not rules that could render laws null and void.
The Swiss government was faced with the question of how to avoid simply ignoring the result of the referendum, while at the same time complying with the still valid requirements for reimbursement in basic insurance. So the representatives of the five CAM directions were actually asked to come to the Federal Office of Public Health with their proof of efficacy and economic efficiency. This was done in 2011.
Of course, this was a little bizarre at this stage – and of course nothing came of it. Or actually it did: once again, no proof could be provided. Meanwhile, a lot of time had passed again and a new Federal Council was forced to take up the matter.
The latter, Alain Berset, came up with the plan that the necessary proof of efficacy could actually be postponed until after the methods had been included in the catalogue of basic insurance benefits. In other words, he gave the methods a governmental leap of faith (which, in view of the long-year history of the case, meant closing several eyes) and postulated that this should be the matter until someone applied for an evaluation of one of the methods.
This is what happened in the year of our Lord 2017. Apparently everyone was able to make their peace with it, which is hardly surprising after ten years of moving around and around. Only the umbrella organisation of health insurers, Santesuisse, grumbled about it and predicted that the announced cost neutrality of such a measure could hardly be expected. Which Santesuisse did indeed prove in a dossier two years later.
The exhausted Swiss have so far left it at that. Homeopathy remained untouched. This was also unfortunate for the reason that the fairy tale of the clever and innovative Switzerland, which knew how important the wishes and preferences of its patients were, was propagated in Germany. The rather strange result of more than ten years of struggle was even passed around by German homeopaths under the name “Swiss model”. Even the leading Swiss press was embarrassed by this and published a clarifying article. And unfortunately, the Swiss began to get used to the existence of hocus-pocus in their basic insurance and to take it for granted.
Until now. Even in Switzerland, the fact that homeopathy is coming under increasing criticism everywhere has probably not gone unnoticed. And the Swiss are actually a rather critical and resistant people. And so it happened that a single brave inhabitant of the country recently decided to exercise his right to demand a new evaluation of homeopathy. The Federal Office of Public Health must have been surprised – or perhaps they were desperately waiting for it? Perhaps. In any case, the application was accepted without hesitation. Meanwhile, a notification has been issued that the hearing procedure for the evaluation has been initiated. The representatives of homeopathy (the service providers), the representatives of the Swiss medical profession and the representatives of the health insurance companies – the aforementioned Santesuisse – will be heard. The final decision will then be made by the Swiss government’s Department of Home Affairs.
How many attempts at an evaluation has this actually been – the third? The fourth? We can’t keep up … We have seen the consequences of scientific questions being decided by majorities. It is to be hoped that Switzerland will not add another chapter to the drama that has been going on since 2005. Mr Berset’s successor, who has been in office since the beginning of the year, should only be given a brief reminder: in Switzerland, too, homeopathy has no effect beyond contextual effects. And that is not enough to prove efficacy, appropriateness and cost-effectiveness.
But cheers to the courageous descendant of William Tell, who is about to single-handedly bring down homeopathy in the Swiss healthcare system!
If you live in the UK, it was impossible during the last week or so to escape the news that our King is going into hospital for a ‘corrective procedure’ on his benign prostate problem. Apparently, he is keen to share his diagnosis with the public to encourage other men who may be experiencing symptoms to get checked. “In common with thousands of men each year, the King has sought treatment for an enlarged prostate,” the official statement said.
According to the NHS website, the King should make lifestyle changes, such as:
- drinking less alcohol, caffeine and fizzy drinks
- limiting your intake of artificial sweeteners
- exercising regularly
- drinking less in the evening
Medicine to reduce the size of the prostate and relax your bladder may be recommended to treat moderate to severe symptoms of an enlarged prostate. Surgery is usually only recommended for moderate to severe symptoms that have not responded to medicine.
It is said that Charles had symptoms since Christmas. So, being the most outspoken fan of so-called alternative medicine (SCAM), why has he not tried SCAM? Has he, for example, tried any of these treatments that have reported at least in one or more studies some promise?:
- Camelia sinensis (green or black tea),
- Solanum lycopersicum (common tomato),
- Punica granatum (pomegranate),
- Glycine max (common soy),
- Linum usitatissimum (linen),
- Ellagic acid,
- Saw palmetto,
- Pumpkin seed,
- Willow herb,
- Maritime pine bark,
- Pygeum africanum bark,
- Rye pollen,
- Nettle root,
- Dozens of Chinese herbs,
- Acupuncture,
- Homeopathy.
It seems not!
But why not?
Why does the world’s greatest SCAM enthusiast not go for his beloved natural cures and ancient wisdom?
Has Charles been advised that the studies are flimsy and the evidence is unconvincing (in that case, well-done Michael!)? I might have given the same advice. Yet, this begs the question, why are he and his head of the royal medical household, Dr Michael Dixon, fiercely in favor of SCAM? Is the evidence for other conditions any better?
Michael, in case you read this: it is not – trust me, I have studied the subject for >30 years.
Anyway, I would probably have consulted a surgeon too, if I had Charles’ problem. Yet, there is an important difference: I (in common with thousands of men) have to join the UK waiting list which currently stands at around 8 000 000.
Yes, I do try to understand that the King is the King and that I am far less of a priority.
The King is special!
The King deserves special, non-NHS treatment!
But scientific evidence is the scientific evidence, no matter whether it relates to SCAM or surgery. So, why does the King (and Dixon) promote SCAM when he himself does evidently not trust it?
A we have heard from our homeopathic friend, Dana Ullaman, homeopathy works well for plants. Unfortunatley, he was unable to provide any good evidence for his claim. To show what a nice guy I am, I herewith help him out and present a recent study on the subject:
Given the seasonal climatic characteristics, forest fires in “cerrado” areas in Central Brazil are not infrequently, with permanent damage. Due to its physicochemical qualities acting in biological regulation processes, water has been considered the primary vehicle for propagating signals from homeopathic ingredients, as suggested by previous studies carried out with solvatochromic dyes. Therefore, such inputs could, in theory, be inserted into watercourses to stimulate the regeneration of the biome destroyed by fire. This hypothesis motivated this case study.
A slow dispersion device was developed aiming at promoting continuous environmental regeneration, containing hydrocolloid and calcium carbonate as a solid base soaked in a homeopathic complex specifically designed for this purpose, composed of Arsenicum album, Arnica montana, Staphysagria, Ignatia amara, and Phosphorus, all at 30cH. The case occurred in Nascentes do Rio Taquari Park, between Mato Grosso and Mato Grosso do Sul state, Brazil. It is a “cerrado” area, with multiple springs that feed the Paraguay River, occupying an area of 26,849 hectares over the Guarani and Bauru aquifers.
After the fire in early September 2020, the devices were fixed at 9 strategic points in the park (P1 to P9) over 10 days, between September 29, and October 11, 2020, in water courses close to the main springs. To assess the restoration signs of the post-fire environment, the technicians responsible for monitoring the park made observations of flora and fauna recomposition in different locations close to four device-insertion points (P3, P5, P7, P8).
Signs of recovery were observed 40 days after the fire was over. A rapid pioneer plant restructuring was noted, with a significant regrowth of grass, herbaceous and shrub species, such as Mutamba (Guazuma ulmifolia), Murici (Byrsonima spp.), Inga (Inga sp.), Brachiaria (Brachiaria sp.), Jaraguá grass (Hyparrhenia rufa), Colonião grass (Panicum maximum), Gabiroba (Campomanesia sp.), and Pixirica (Miconia sp.). Some species, such as Mimosa (Mimosa sp.), Colonião grass (Panicum maximum), and Jaraguá grass (Hyparrhenia rufa), were not detected in the area before the fire, probably by the seed bank stimulation caused by the heat. There was rapid forest regeneration (4 months after the fire) and restoration of most of the burned trees, both for resisting the fire and for being free of invasive species highly aggressive to native plants, which were controlled by the action of fire. Concerning the fauna, a vast animal population was detected, especially birds, highlighting the “Tuiuiú” (Jabiru mycteria) and “Socó” (Tigrisoma lineatum) close to a water body with a waterfall area (P3). Both species belong to the “Pantanal” biome close to the park. Such species began to frequent the park’s lakes, being observed until February 2023 (the last survey date). The park’s inventory of lichens and fungi showed an unusual tolerance to fire in species that adhered to burned trees and remained active.
In this way, it is suggested that installing slow dispersion devices in watercourses can contribute to the regeneration of other “cerrado” biome areas subjected to fire, protecting the local biodiversity. More studies of this nature are needed to know the real impact of this method on the recovery of different biomes.
Convinced?
I suspect Dana might be (he seems to be particularly prone to confirmation bias) – but rational thinkers do probably have questions; let me just mention two:
- Was there a control area with which the findings were compared?
- Was the outcome measure objective?
As the answers are NO and NO, I fear that we need to disappoint Dana yet again:
homeopathy is a placebo treatment no matter whether we apply it to humans, animals or plants.
Dragons’ Den is a British reality television business programme, presented by Evan Davis and based upon the original Japanese series. The show allows several entrepreneurs an opportunity to present their varying business ideas to a panel of five wealthy investors, the “Dragons” of the show’s title, and pitch for financial investment while offering a stake of the company in return.
It has been reported that Giselle Boxer began selling needle-free acupuncture kits for ears after being diagnosed with myalgic encephalomyelitis (ME). She said the technique had helped improve her own health. Ms Boxer worked for advertising agency before starting her business. A researcher on the show had contacted her to ask if she would like to take part.
Entrepreneur and former footballer Gary Neville was so impressed with her pitch he made her an offer in full before the Dragons had a chance to begin asking questions. She said the impact on the business since the show aired had been “bonkers”. “It’s just been a complete whirlwind,” she said.

The tiny beads are a needle-free form of auriculotherapy, designed to stimulate specific points of the ear to address physical and emotional health concerns. “It completely transformed my life alongside lots and lots of other things like diet, lifestyle changes, meditation, breathwork and movement,” said Ms Boxer. She has since had a child and claimed she was fully healed within a year. “It was like a full overhaul of my life,” Ms Boxer said. Her business, Acu Seeds, sells kits for people to use at home and made a £64,000 profit in its first year, she added.
On the Acu Seed website, we learn the following:
Ear seeds are a form of auriculotherapy, which is the stimulation of specific points of the ear to support physical and emotional health concerns. They are a needle-free form of acupuncture that have been used in Traditional Chinese Medicine (TCM) for thousands of years. TCM teaches that the ear is a microsystem of the whole body, where certain points on the ear correspond to different organs or body parts. Energy pathways (or ‘qi’ or vital life energy) pass through the ear and ear seeds stimulate specific points which send an abundant flow of energy to the related organ or area that needs attention. Think of it like reflexology, but for the ears instead of feet.
Ear seeds also create continual, gentle pressure on nerve impulses in the ear which send messages to the brain that certain organs or systems need support. The brain will then send signals and chemicals to the rest of the body to support whatever ailments you’re experiencing, releasing endorphins into the bloodstream, relaxing the nervous system, and naturally soothing pain and discomfort. Some people use ear seeds alongside acupuncture treatments as they may help the effects of acupuncture last longer between sessions.
I am impressed by the lingo used here:
- support physical and emotional health concerns – the seeds support the concerns but not the health?
- a needle-free form of acupuncture – sorry, the seeds don’t puncture anything; they exert pressure; therefore it’s called acuPRESSURE.
- have been used in Traditional Chinese Medicine (TCM) for thousands of years – no, it was invented just a few decades ago by Paul Nogier.
- TCM teaches that the ear is a microsystem of the whole body – TCM teaches plenty of nonsense but not this one.
- Energy pathways (or ‘qi’ or vital life energy) pass through the ear –Qi is nothing more than a figment of the imagination of TCM advocates.
- send an abundant flow of energy to the related organ or area – only if you believe in your own fictional form of physiology.
- Think of it like reflexology – which btw is also nonsense.
- nerve impulses in the ear send messages to the brain that certain organs or systems need support – only if you believe in your own fictional form of physiology.
- The brain will then send signals and chemicals to the rest of the body – only if you believe in your own fictional form of physiology.
- help the effects of acupuncture last longer – help the non-existing effects of acupuncture last longer?
One the website, we also learn what for which conditions the treatment is effective:
Ear seeds may support a broad spectrum of health concerns including anxiety, stress, headaches, digestion, immunity, focus, sleep and fatigue. Our ear seed kits include the protocol ear maps for these eight health concerns and each protocol uses between 3 to 5 ear seeds. Ear seeds have also been found to support with women’s health issues like menstrual issues, libido, fertility, postpartum issues, inflammation, menopause and weight loss. The ear maps for these issues are given in our women’s health ear seed kit bundles. The specific combination of seed placements will support your chosen health concern. Further issues that they may support with are addiction, pain, tinnitus, vertigo, thyroid health and more.
Here, I am afraid, we might have a major problem:
THERE IS NO GOOD EVIDENCE TO SUPPORT ANY OF THESE CLAIMS!
I thus do wonder whether the venture of Giselle Boxer might be a case for the Advertising Standards Authority.
I had the rare pleasure to give an interview for the ‘Frankfurter Allgemeine’. As it was, of course, in German, I took the liberty to translate it for my non-German speaking readers:
You have researched so-called alternative medicine over several decades, including homeopathy. What is your conclusion?
We are talking about far more than 400 methods – to draw one conclusion about all of them
is completely impossible. Except perhaps for this one: if something sounds too good to be true, it probably is.
Does this apply to homeopathy?
Highly diluted homeopathic remedies are popular because they have no side-effects. But there is also no effect. They are touted as a panacea. This is certainly not the case, on the contrary, they are
ineffective. And any therapy that is ineffective and promoted as a panacea is also dangerous.
How do you explain the fact that so many people swear by homeopathy?
There are several reasons for this. In Germany, homeopathy has an unbroken tradition, it was, for instance, promoted by the Nazis and later in the Federal Republic of Germany. It has a reputation for being gentle and effective. It might be gentle, but it is certainly not effective. It is also supported by lobby groups such as the manufacturers. And most people who use it don’t even understand what it actually is.
In any case, the placebo effect helps. What’s so bad about that??
Nothing at all, on the contrary: it is to be advocated. When we talk about placebo effects, we subsume many things under this umbrella that do not actually belong to it, such as the extensive, empathetic conversation that homeopaths often have with their patients. Besides, a common cold goes away whether you treat it or not. If you then use homeopathy, you can easily get the impression that it worked. Every good, empathetic doctor tries to maximize the placebo effect. To put it bluntly: you don’t need a placebo to generate a placebo effect. Patients also benefit from it when I give an effective remedy with empathy. In addition they benefit from the specific effect of my therapy, which should make up the lion’s share of the therapeutic response. If I withhold the most important thing I mistreat my patient.
But there are diseases for which there are no good remedies.
I often hear that argument. But there is practically always something we can do that at least
improves symptoms. Otherwise you should also say that instead of lying and recommending homeopathy – and thinking that, although there is nothing in it and it doesn’t work, but the patient, being an idiot, should take it nevertheless. It is unethical to use placebos as much as it is to use homeopathy.
Neurophysiologically, the placebo effect is becoming better and better understood.
The Italian neuroscientist Fabrizio Benedetti in particular has done very good work. But he also warns that this does not justify the use of homeopathy, for example.
Are there any studies on whether the placebo effect of homeopathy with its esoteric superstructure is greater than that giving just a piece of sugar?
There are analyses of what makes a particularly effective placebo. From this, we can learn that effective therapies in evidence-based medicine must be applied with empathy and sufficient time in order to maximize the ever-present placebo effect. So-called alternative medicine often does this quite well, and we can learn something from it. But the reason is that it often has nothing else. Homeopaths are a serious danger because they see homeopathy as a panacea. If someone has homeopathically treated their cold “successfully” for years and then gets cancer, they might think of turning to homeopathy for their cancer. It sounds crazy, but many homeopaths do offer cancer treatments on the internet, for instance. That sends shivers down my spine.
How should doctors and pharmacists react to the demand for homeopathic remedies?
Pharmacists are not primarily salespeople, they are a medical profession – they have to adhere to ethical guidelines. In this respect, evidence-based information of their clients/patients is very important.
Thomas Benkert, President of the German Federal Chamber of Pharmacists, has stated that he would not be able to stop giving advice if he always had to explain the lack of proof of efficacy.
He should perhaps read up on what his ethical duty to patients is.
What if doctors or pharmacists themselves believe in the effect?
Belief should not play a role, but evidence should.
Are you pleased with Lauterbach’s plan to no longer reimburse homeopathy?
I think it’s a shame that he justifies it by saying it’s ineffective. That is true. But the justification should be that it’s esoteric nonsense and therefore ineffective – and dangerous.
In the end, the Bundestag will decide.
I think Lauterbach has a good chance because things have started to move. Medical associations in Germany have spoken out against the additional designation of homeopathy, for example, and overall the wind has changed considerably.
What is it like in the UK, where you live?
The UK healthcare system, NHS, said goodbye to reimbursement of homeopathy about five years ago, even before France. The pharmacists’ association has distanced itself very clearly from homeopathy. However, most pharmacists still sell the remedies and many continue to support them.
You have also had disputes with the current head of state, King Charles. How did that come about?
A few years ago, he commissioned a paper claiming that so-called alternative medicine could save the British health service a lot of money. I protested against this – Charles accused me of leaking it to The Times before it was published. My university launched an investigation, which eventually found me innocent, but it led to the demise of my department. That caused me to retire two years early.
So Charles managed to close down the only research unit in the world that conducted critical and systematic research into so-called alternative medicine. Most researchers in this field only want to confirm their own prejudices and not disprove hypotheses. This is a serious misunderstanding of how science works. If someone reports only positive results for their favorite therapy in all conditions, something is wrong.
Some people say that homeopathy should not be researched because nothing positive can come out of it anyway.
There are certainly some SCAMs that are so nonsensical that they should not be researched, as is currently the case with homeopathy. I put it this way because I have researched homeopathy myself and, from my point of view, the situation was not so crystal clear 30 years ago.
Would you say that you have approached the matter with a sufficiently open mind?
No one can be completely unbiased. That’s why it’s important to do science properly, then you minimize bias as much as possible. When I took up my position at Exeter in 1993, I was perhaps somewhat biased towards homeopathy in a positive sense, because I had learned and used it myself, as well as other alternative medicine methods. The fact that the results then turned out to be negative in the vast majority of cases initially depressed me. But I have to live with that.
Every researcher prefers positive results, also because they are easier to publish. It was clear to me that, if I had succeeded in proving homeopathy right, I wouldn’t get one Nobel Prize, but two. Who wouldn’t want that?
(The interview was conducted by Hinnerk Feldwisch-Drentrup.)
This systematic review aimed to investigate the effectiveness of cupping therapy on low back pain (LBP). Medline, Embase, Scopus and WANFANG databases were searched for relevant cupping RCTs on low back pain articles up to 2023. A complementary search was manually made on 27 September for update screening. Full-text English and Chinese articles on all ethnic adults with LBP of cupping management were included. Studies looking at acute low back pain only were excluded. Two independent reviewers screened and extracted data, with any disagreement resolved through consensus by a third reviewer. The methodological quality of the included studies was evaluated independently by two reviewers using an adapted tool. Change-from-baseline outcomes were treated as continuous variables and calculated according to the Cochrane Handbook. Data were extracted and pooled into the meta-analysis by Review Manager software (version 5.4, Nordic Cochrane Centre).
Eleven trials involving 921 participants were included. Five studies were assessed as being at low risk of bias, and six studies were of acceptable quality. The findings reveal:
- High-quality evidence demonstrated cupping significantly improves pain at 2-8 weeks endpoint intervention (d=1.09, 95% CI: [0.35-1.83], p=0.004).
- There was no continuous pain improvement observed at one month (d=0.11, 95% CI: [-1.02-1.23], p=0.85) and 3-6 months (d=0.39, 95% CI: [-0.09-0.87], p=0.11).
- Dry cupping did not improve pain (d=1.06, 95% CI: [-0.34, 2.45], p=0.14) compared with wet cupping (d=1.5, 95% CI: [0.39-2.6], p=0.008) at the endpoint intervention.
- There was no evidence indicating the association between pain reduction and different types of cupping (p=0.2).
- Moderate- to low-quality evidence showed that cupping did not reduce chronic low back pain (d=0.74, 95% CI: [-0.67-2.15], p=0.30) and non-specific chronic low back pain (d=0.27, 95% CI: [-1.69-2.24], p=0.78) at the endpoint intervention.
- Cupping on acupoints showed a significant improvement in pain (d=1.29, 95% CI: [0.63-1.94], p<0.01) compared with the lower back area (d=0.35, 95% CI: [-0.29-0.99], p=0.29).
- A potential association between pain reduction and different cupping locations (p=0.05) was found.
- Meta-analysis showed a significant effect on pain improvement compared to medication therapy (n=8; d=1.8 [95% CI: 1.22 – 2.39], p<0.001) and usual care (n=5; d=1.07 [95% CI: 0.21- 1.93], p=0.01).
- Two studies demonstrated that cupping significantly mediated sensory and emotional pain immediately, after 24 hours, and 2 weeks post-intervention (d= 5.49, 95% CI [4.13-6.84], p<0.001).
- Moderate evidence suggested that cupping improved disability at the 1-6 months follow-up (d=0.67, 95% CI: [0.06-1.28], p=0.03).
- There was no immediate effect observed at the 2-8 weeks endpoint (d=0.40, 95% CI: [-0.51-1.30], p=0.39).
- A high degree of heterogeneity was noted in the subgroup analysis (I2 >50%).
The authors concluded that high- to moderate-quality evidence indicates that cupping significantly improves pain and disability. The effectiveness of cupping for LBP varies based on treatment durations, cupping types, treatment locations, and LBP classifications. Cupping demonstrated a superior and sustained effect on pain reduction compared with medication and usual care. The notable heterogeneity among studies raises concerns about the certainty of these findings. Further research should be designed with a standardized cupping manipulation that specifies treatment sessions, frequency, cupping types, and treatment locations. The real therapeutic effects of cupping could be confirmed using a sham device or objective outcome measurements. Studies with at least six- to twelve-month follow-ups are needed to investigate the long-term efficacy of cupping in managing LBP.
Confused?
No need, it’s really quite simple: cupping can, according to this review, be shown to have some short-lasting effect, provided the study is flawed and does not control for placebo effects.
Surprised?
No need! There is hardly a form of so-called alternative medicine (SCAM) that does not have a similarly small effect of back pain, if tested in equally dodgy studies. This is particularly true for those treatments that can act as a theatrical placebo, e.g. acupuncture or chiropractic.
So, should a back pain sufferer try cupping?
If he/she insists, why not? But please don’t use wet cupping (which can do quite a bit of harm). Dry cupping (without injuring the skin) is arguably better (less risk, less expense, possibility of home treatment by your partner) than chiropractic, osteopathy, acupuncture, or many other SCAMs.
My conclusions – as mentioned many times previously – are as follows:
- Most SCAMs help a little with back pain (and similar conditions) because they can have a powerful placebo effect.
- Conventional medicine is also not convincingly effective for back pain.
- If you insist on SCAM, it is best to use one that is relatively harmless and inexpensive.
