research
This systematic review and meta-analysis investigated the effectiveness and safety of manual therapy (MT) interventions compared to oral or topical pain medications in the management of neck pain.
The investigators searched from inception to March 2023, in Cochrane Central Register of Controller Trials (CENTRAL), MEDLINE, EMBASE, Allied and Complementary Medicine (AMED) and Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO) for randomized controlled trials that examined the effect of manual therapy interventions for neck pain when compared to oral or topical medication in adults with self-reported neck pain, irrespective of radicular findings, specific cause, and associated cervicogenic headaches. Trials with usual care arms were also included if they prescribed medication as part of the usual care and they did not include a manual therapy component. The authors used the Cochrane Risk of Bias 2 tool to assess the potential risk of bias in the included studies, and the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach to grade the quality of the evidence.
Nine trials with a total of 779 participants were included in the meta-analysis.
- low certainty of evidence was found that MT interventions may be more effective than oral pain medication in pain reduction in the short-term (Standardized Mean Difference: -0.39; 95% CI -0.66 to -0.11; 8 trials, 676 participants),
- moderate certainty of evidence was found that MT interventions may be more effective than oral pain medication in pain reduction in the long-term (Standardized Mean Difference: −0.36; 95% CI −0.55 to −0.17; 6 trials, 567 participants),
- low certainty evidence that the risk of adverse events may be lower for patients who received MT compared to the ones that received oral pain medication (Risk Ratio: 0.59; 95% CI 0.43 to 0.79; 5 trials, 426 participants).
The authors conluded that MT may be more effective for people with neck pain in both short and long-term with a better safety profile regarding adverse events when compared to patients receiving oral pain medications. However, we advise caution when interpreting our safety results due to the different level of reporting strategies in place for MT and medication-induced adverse events. Future MT trials should create and adhere to strict reporting strategies with regards to adverse events to help gain a better understanding on the nature of potential MT-induced adverse events and to ensure patient safety.
Let’s have a look at the primary studies. Here they are with their conclusions (and, where appropriate, my comments in capital letters):
- For participants with acute and subacute neck pain, spinal manipulative therapy (SMT) was more effective than medication in both the short and long term. However, a few instructional sessions of home exercise with (HEA) resulted in similar outcomes at most time points. EXERCISE WAS AS EFFECTIVE AS SMT
- Oral ibuprofen (OI) pharmacologic treatment may reduce pain intensity and disability with respect to neural mobilization (MNNM and CLG) in patients with CP during six weeks. Nevertheless, the non-existence of between-groups ROM differences and possible OI adverse effects should be considered. MEDICATION WAS BETTER THAN MT
- It appears that both treatment strategies (usual care + MT vs usual care) can have equivalent positive influences on headache complaints. Additional studies with larger study populations are needed to draw firm conclusions. Recommendations to increase patient inflow in primary care trials, such as the use of an extended network of participating physicians and of clinical alert software applications, are discussed. MT DOES NOT IMPROVE OUTCOMES
- The consistency of the results provides, in spite of several discussed shortcomings of this pilot study, evidence that in patients with chronic spinal pain syndromes spinal manipulation, if not contraindicated, results in greater improvement than acupuncture and medicine. THIS IS A PILOT STUDY, A TRIAL TESTING FEASIBILITY, NOT EFFECTIVENESS
- The consistency of the results provides, despite some discussed shortcomings of this study, evidence that in patients with chronic spinal pain, manipulation, if not contraindicated, results in greater short-term improvement than acupuncture or medication. However, the data do not strongly support the use of only manipulation, only acupuncture, or only nonsteroidal antiinflammatory drugs for the treatment of chronic spinal pain. The results from this exploratory study need confirmation from future larger studies.
- In daily practice, manual therapy is a favorable treatment option for patients with neck pain compared with physical therapy or continued care by a general practitioner.
- Short-term results (at 7 weeks) have shown that MT speeded recovery compared with GP care and, to a lesser extent, also compared with PT. In the long-term, GP treatment and PT caught up with MT, and differences between the three treatment groups decreased and lost statistical significance at the 13-week and 52-week follow-up. MT IS NOT SUPERIOR [SAME TRIAL AS No 6]
- In this randomized clinical trial, for patients with chronic neck pain, Chuna manual therapy was more effective than usual care in terms of pain and functional recovery at 5 weeks and 1 year after randomization. These results support the need to consider recommending manual therapies as primary care treatments for chronic neck pain.
- In patients with chronic spinal pain syndromes, spinal manipulation, if not contraindicated, may be the only treatment modality of the assessed regimens that provides broad and significant long-term benefit. SAME TRIAL AS No 5
- An impairment-based manual physical therapy and exercise (MTE) program resulted in clinically and statistically significant short- and long-term improvements in pain, disability, and patient-perceived recovery in patients with mechanical neck pain when compared to a program comprising advice, a mobility exercise, and subtherapeutic ultrasound. THIS STUDY DID NOT TEST MT ALONE AND SHOULD NOT HAVE BEEN INCLUDED
I cannot bring myself to characterising this as an overall positive result for MT; anyone who can is guilty of wishful thinking, in my view. The small differences in favor of MT that (some of) the trials report have little to do with the effectiveness of MT itself. They are almost certainly due to the fact that none of these studies were placebo-controlled and double blind (even though this would clearly be possible). In contrast to popping a pill, MT involves extra attention, physical touch, empathy, etc. These factors easily suffice to bring about the small differences that some studies report.
It follows that the main conclusion of the authors of the review should be modified:
There is no compelling evidence to show that MT is more effective for people with neck pain in both short and long-term when compared to patients receiving oral pain medications.
The Academy of Homeopathy Education is a US-based accredited teaching institution offering homeopathy education services to professional and medically licensed homeopathy students. This study reports on clinical outcomes from the teaching clinic from 2020 to 2021.
Data were collected using the patient-generated outcome measure, the Measure Yourself Concerns and Wellbeing (MYCaW). Mean MYCaW values for initial and subsequent consultations were analyzed for the degree of change across the intervention period in 38 clients. Each client listed up to two complaints. MYCaW scores between initial and subsequent consultations were analyzed for the degree of change (delta) across the intervention period.
A total of 95 body system-related symptoms were analyzed for change in intensity following the homeopathic intervention. Statistically significant improvements in the intensity of main symptoms were observed between initial and subsequent follow-ups. The main symptom scores showed a mean change in intensity (delta MYCaW) of −0.79 points (95% confidence interval (CI), −1.29 to −0.29; p = 0.003) at first follow-up, a mean change of −1.67 points (95% CI, −2.34 to −0.99; p = 0.001) at second follow-up compared with the initial visit, and a mean change of −1.93 points (95% CI, −3.0 to −0.86; p = 0.008) at third follow-up compared with the initial visit. For clients with four or more follow-ups, the mean delta MYCaW was −1.57 points (95% CI, −2.86 to −0.28; p = 0.039).
The authors concluded that statistically significant improvements as well as some clinically meaningful changes in symptom intensity were found across a diverse group of individuals with a variety of long-term chronic conditions. The improvement was evident across different body systems and different levels of chronicity. There are limitations to the generalizability of the study due to the research design. Further research and investigation are warranted given the promising results of this work.
There are, of course, not just limits to the generalizability of this study! I’d say there are limits to the interpretation of any of its findings.
What was the cause of the improvements?
Here are just a few questions that I asked myself while reading this paper:
- Are the guys from the Academy of Homeopathy Education not aware of the fact that even chronic conditions often get better by themselves?
- Have they heard of the placebo effect?
- Are they trying to tell us that the patients did not also use conventional treatments for their chronic conditions?
- What about regression towards the mean?
- What about social desirability?
- Why do they think that further research is needed?
- Are these really results that look ‘promising for homeopathy?
To answer just the last question: No, these findings are in perfect agreement with the fact that highly diluted homeopathic remedies are pure placebos (to be honest, they would even be in agreement with such remedies being mildly harmful).
Introduction
There has been accumulating interest in the application of biofield therapy as complementary and alternative medicine (CAM) to treat various diseases. The practices include reiki, qigong, blessing, prayer, distant healing, known as biofield therapies. This paper aims to state scientific knowledge on preclinical and clinical studies to validate its potential use as an alternative medicine in the clinic. It also provides a more in-depth context for understanding the potential role of quantum entanglement in the effect of biofield energy therapy.
Content
A comprehensive literature search was performed using the different databases (PubMed, Scopus, Medline, etc.). The published English articles relevant to the scope of this review were considered. The review gathered 45 papers that were considered suitable for the purpose. Based on the results of these papers, it was concluded that biofield energy therapy was effective in treating different disease symptoms in preclinical and clinical studies.
Summary
Biofield therapies offer therapeutic benefits for different human health disorders, and can be used as alternative medicine in clinics for the medically pluralistic world due to the growing interest in CAM worldwide.
Outlook
The effects of the biofield energy therapies are observed due to the healer’s quantum thinking, and transmission of the quantum energy to the subject leads to the healing that occurs spiritually through instantaneous communication at the quantum level via quantum entanglement.
The authors of this article are affiliated with Trivedi Global, an organisation that states this about ‘biofield energy’:
Human Biofield EBnergy has subtle energy that has the capacity to work in an effective manner. This energy can be harnessed and transmitted by the gifted into living and non-living things via the process of a Biofield Energy Healing Treatment or Therapy.
If they aleady know that “Biofield EBnergy has subtle energy that has the capacity to work in an effective manner”, I wonder why they felt the need to conduct this review. Even more wonderous is the fact that their review showed such a positive result.
How did they manage this?
The answer might lie in their methodology: they “gathered 45 papers that were considered suitable”. While scientists gather the totality of the available evidence (and assess it critically), they merely selected what was suitable for the purpose of generating a positive result. This must be the reason our two studies on the subject were discretely omitted:
Purpose: Distant healing, a treatment that is transmitted by a healer to a patient at another location, is widely used, although good scientific evidence of its efficacy is sparse. This trial was aimed at assessing the efficacy of one form of distant healing on common skin warts.
Subjects and methods: A total of 84 patients with warts were randomly assigned either to a group that received 6 weeks of distant healing by one of 10 experienced healers or to a control group that received a similar preliminary assessment but no distant healing. The primary outcomes were the number of warts and their mean size at the end of the treatment period. Secondary outcomes were the change in Hospital Anxiety and Depression Scale and patients’ subjective experiences. Both the patients and the evaluator were blinded to group assignment.
Results: The baseline characteristics of the patients were similar in the distant healing (n = 41) and control groups (n = 43). The mean number and size of warts per person did not change significantly during the study. The number of warts increased by 0.2 in the healing group and decreased by 1.1 in the control group (difference [healing to control] = -1.3; 95% confidence interval = -1.0 to 3.6, P = 0.25). Six patients in the distant healing group and 8 in the control group reported a subjective improvement (P = 0.63). There were no significant between-group differences in the depression and anxiety scores.
Conclusion: Distant healing from experienced healers had no effect on the number or size of patients’ warts.
Spiritual healing is a popular complementary and alternative therapy; in the UK almost 13000 members are registered in nine separate healing organisations. The present randomized clinical trial was designed to investigate the efficacy of healing in the treatment of chronic pain. One hundred and twenty patients suffering from chronic pain, predominantly of neuropathic and nociceptive origin resistant to conventional treatments, were recruited from a Pain Management Clinic. The trial had two parts: face-to-face healing or simulated face-to-face healing for 30 min per week for 8 weeks (part I); and distant healing or no healing for 30 min per week for 8 weeks (part II). The McGill Pain Questionnaire was pre-defined as the primary outcome measure, and sample size was calculated to detect a difference of 8 units on the total pain rating index of this instrument after 8 weeks of healing. VASs for pain, SF36, HAD scale, MYMOP and patient subjective experiences at week 8 were employed as secondary outcome measures. Data from all patients who reached the pre-defined mid-point of 4 weeks (50 subjects in part I and 55 subjects in part II) were included in the analysis. Two baseline measurements of outcome measures were made, 3 weeks apart, and no significant differences were observed between them. After eight sessions there were significant decreases from baseline in McGill Pain Questionnaire total pain rating index score for both groups in part I and for the control group in part II. However, there were no statistically significant differences between healing and control groups in either part. In part I the primary outcome measure decreased from 32.8 (95% CI 28.5-37.0) to 23.3 (16.8-29.7) in the healing group and from 33.1 (27.2-38.9) to 26.1 (19.3-32.9) in the simulated healing group. In part II it changed from 29.6 (24.8-34.4) to 24.0 (18.7-29.4) in the distant healing group and from 31.0 (25.8-36.2) to 21.0 (15.7-26.2) in the no healing group. Subjects in healing groups in both parts I and II reported significantly more ‘unusual experiences’ during the sessions, but the clinical relevance of this is unclear. It was concluded that a specific effect of face-to-face or distant healing on chronic pain could not be demonstrated over eight treatment sessions in these patients.
In addition, they, of course, also omitted many further studies by other investigators that failed to be positive. Considering this amount of cherry-picking, it is easy to understand how they arrived at their conclusion. It is all a question of chosing the right methodology!
A few decades ago, the cigarette industry employed this technique to show that smoking did not cause cancer! Luckily, we have since moved away from such pseudo-scientific ‘research’ – except, of course, in the realm of SCAM where it is still hughely popular.
Cervical spondylosis is a chronic degenerative process of the cervical spine characterized by pain in neck, degenerative changes in intervertebral disc and osteophyte formation. The present study was aimed at evaluating the effect of wet cupping (Ḥijāma Bish Sharṭ) in the pain management of cervical spondylosis.
This Open, randomized, clinical study was conducted on 44 patients.
- Subjects in the test group (n = 22) received a series of three-staged wet cupping treatment, performed on 0, 7th and 14th day.
- Subjects in the control group (n = 22) received 12 sittings of Transcutaneous Electrical Nerve Stimulation (TENS): 6 sittings per week for two weeks.
The outcomes were assessed with the help of VAS, Neck Disability Index (NDI) and Cervical range of motion.
Intra group comparison in test group from baseline to 21st day were found highly significant (p < 0.001) in terms of VAS, NDI, Flexion, Extension and Left rotation score. While in Right rotation, Left rotation and Left lateral flexion score were found moderately significant (p < 0.01). Statistically significant difference was observed between two groups at 21st day in VAS scale, NDI, and Cervical range of motion score (p < 0.001).
The authors concluded that Ḥijāma Bish Sharṭ was found better in the management of pain due to cervical spondylosis than TENS. It can be concluded that Ḥijāma Bish Sharṭ may a better option for the pain management of cervical spondylosis.
Wet cupping is the use of a vacuum cup applied to the skin which has previously been lacerated. It draws blood and can thus be seen as a form of blood letting. It has been used in various cultures for the treatment of joint pain and many other conditions since antiquity.
The authors point out that, in Unani medicine, it is believed to reduce pain and other symptoms by diverting and evacuating the causative pathological humours (akhlāṭ-e-fasida). Galen (Jalinoos) mentioned wet cupping as a very useful modality in evacuating the thick humours (akhlāṭ-e-Ghaleez) (Nafeesi, 1954; Qamri, 2008). Wet cupping works on the principle of diversion and evacuation of morbid matter (imala wa tanqiya-i-mawād-i-fasida). It opens the pores of the skin, enhances the blood circulation, nourishes the affected area with fresh blood, improves the eliminative function and facilitates the evacuation of morbid matter from the body.
There are several studies of wet cupping, most of which are as flawed as the one above. This new trial has several limitations, e.g.:
- It makes no attempt to control for placebo effects which could well be more prominent for wet cupping than for TENS.
- It did not inhibit the influence of verbal or non-verbal communications between therapists and patients which are likely to influence the results.
- The sample size is far too small, particularly as the study was designed as an equivalence study.
But some might say that my arguments a petty and argue that, regardless of a flimsy study, wet cupping is still worth a try. I would disagree – not because of the flaws of this study, nor the implausibility of the long-obsolete assumptions that underpin the therapy, but because wet cupping is associaated with infections of the skin lacerations which occasionally can be serious.
This study aims to assess the feasibility of a pragmatic prospective study aiming to report the immediate and delayed (48-hours post-treatment) AEs associated with manual therapies in children aged 5 or younger and to report preliminary data on AEs frequency.
Between July 2021 and March 2022, chiropractors were recruited through purposive sampling and via a dedicated Facebook group for Quebec chiropractors interested in pediatrics. Legal guardians of patients aged 5 or younger were invited to fill out an online information and consent form. AEs were collected using the SafetyNET reporting system, which had been previously translated by the research team. Immediate AEs were collected through a questionnaire filled out by the legal guardian immediately after the treatment, while delayed AEs were collected through a questionnaire sent by email to the legal guardian 48 h after the treatment. Feasibility was assessed qualitatively through feedback from chiropractors and quantitatively through recruitment data.
Overall, a total of 28 chiropractors expressed interest following the Facebook publication, and 5 participated. An additional two chiropractors were enrolled through purposive sampling. In total, 80 legal guardians consented to their child’s participation, and data from 73 children were included for the analysis of AEs. At least one AE was reported in 30% of children (22/73), and AEs were mainly observed immediately following the treatment (16/22). The most common AEs were irritability/crying (11 children) or fatigue/tiredness (11 children). Feasibility analysis demonstrated that regular communication between the research team and clinicians, as well as targeting clinicians who showed great interest in pediatrics, were key factors for successful research.
The authors concluded that their results suggest that it is feasible to conduct a prospective pragmatic study evaluating AEs associated with manual therapies in private practices. Direct communication with the clinicians, a strategic clinicians’ recruitment plan, and the resulting administrative burden should be considered in future studies. A larger study is required to confirm the frequency of AEs reported in the current study.
It is hardly surprising that such a study is ‘feasible’. I could have told the authors that and saved them the trouble of doing the study. What is surprising, in my view, that chiropractors, after ~120 years of existence of the profession, ask whether it is feasible.
I suggest to do the definitive study on a much larger sample, extend the observation period, and recruit a representative rather than self-selected sample of chiros … or – much better – forget about the study and establich a functioning post-marketing surveillance system.
In recent weeks and months, I have been thinking quite a lot about the various types of scientists. This is partly due to me finishing a book entitled:
1. SCIENTIST
Scientists gather information through observation and experimentation, formulate hypothesis, and then test them. They work in vastly different areas but have certain attitudes or qualities in common, e.g. critial thinking and an open mind. As scientists tend to publish their findings, a very simple (but not fool-proof) way to identify a scinetist is to look him/her up, for example by finding his/her H-Index. (The H-Index is defined as the maximum value of h such that the given author/journal has published at least h papers that have each been cited at least h times. For instance, if someone has 10 papers that were cited 10 times, his H-Index would be 10. If another scientist has 50 papers that were cited 50 times, his H-Index would be 50.)
2. PSEUDO-SCIENTIST
Pseudo-scientists are people who pretend to produce science but, in fact, they generate pseudoscience. The demarkation of pseudo-science from science is sometimes difficult, as we have seen several times on this blog, e.g.:
- Characteristics of pseudoscience
- Science or Pseudoscience?
- Is acupuncture pseudoscience?
- The techniques of pseudoscience
- Pseudoscience revisited
- Tolerance towards pseudo-science?
- How to become a charlatan
The pseudo-scientist does have no or just a few publications in the peer-reviewed literature and no H-Index to speak of.
3. WOULD-BE SCIENTIST
The term ‘would-be scientist’ is not one that is commonly used, nor is it one that has an accepted definition. The way I see it, would-be scientists are aspiring to become scientist. They are on the way to become a scientist but have not quite arrived yet. To the would-be scientist I say: good luck to you; I hope you make it and I look forward to reading about your scientific achievements. The would-be scientist is, however, not the topic of my post.
4. THE PREDEND-SCIENTIST
The predent-scientist (PS) is the one who I want to focus on here. He – yes, the PS is usually male – talks a lot about science; so much so that outsiders would get the impression that he actually is a scientist. Crucially, the PS himself has managed to delude himself to the point where believes to be a scientist.
While scientists tend to be media-shy, the PS enjoys the limelight to generate the impression of being a scientist. He talks eloquently and at length about science. Much of what he says or writes might even be correct. The PS is often quite well-versed and knows (most of) his stuff.
The crucial difference between the PS and the scientist is that the PS produces no or very little science; neither does he intend to. To identify the PS, an easy (but not fool-proof) method is to him look up. Typically, he has published several articles in the popoular press or books for the lay public, but – as he does not conduct scientific research – he does not generate papers in the peer-reviewed scientific literature. This void, however, has never stopped the PS from appearing in the media speaking about science, nor from occupying prominent positions in the world of science, nor from avidly rubbing shoulders with scientists. Few people see anything wrong with that, mainly because the PS has convinced them (most importantly himself) that he actually is a scientist. While the scientist is trained in doing science, the PS is trained in talking about science.
Don’t get me wrong, the PS can have his merits. He often presents science to the public more or less accurately and frequently is rhetorically superior to the scientist. I nevertheless have reservations about the PS (and the recent pandemic has shown us how dangerous PSs can beome). The questions to ask ourselves are the following:
- Does PS have a truly open mind?
- Can he set aside ideologies?
- Will he change his opinion vis a vis new evidence?
- Is he prepared to consider criticism?
- Does he avoid ‘black and white’ thinking?
- Is he sufficiently humble?
- Is he honest with himself and others?
These questions refer to important attitudes that scientists learn – often the hard way – while doing science. If someone lacks this experience, such attitudes are likely to be under-developed. Perhaps, it all boils down to honesty: if a man who has never done any amount of science to speak of has convinced himself to be a scientist, he arguably is dishonest with himself and the public.
In order to make my points as clearly as possible, I admittedly caricaturized the extremes of a wider spectrum; my appologies for that. In reality, the different types of scientists rarely exist as entirely pure forms. Frequently, people are mixtures of two types, either because they did different things during different periods of their lives, or because they simply are hybrids.
To provide a few examples, let me show you 14 H-Indices (according to ‘Google Scholar’) of people (in alphabetical order) who you might have heard of, for instance, because they have featured on my blog. I leave it up to you to decide how well they fit in any of my three categories and who might qualify to be a PS.
- Fabrizio Benedetti – H-Index = 83
- David Colquhoun – H-Index = 78
- Ian Chalmers – H-Index = 84
- Michael Dixon – H-Index = 0
- David Gorski – H-Index = 30
- Holm Hümmler – H-Index = 0
- Ted Kaptchuk – H-Index = 103
- Jos Kleinjen – H-Index = 104
- Andreas Michalsen – H-Index = 0
- Michael Mosely – H-Index = 0
- Dana Ullman – H-Index = 0
- Dale Thompson (alias DC) – H-Index = 0
- Chris van Tulleken – H-Index = 0
- Harald Walach – H-Index = 9
My conclusion: the PS, a person who presents himself as a scientist without having done any meaningful amount of science himself, is a man who is not entirely honest. The H-Index can be helpful for identifying PSs. An index of zero, for instance, seems to send out a fairly clear message. In the case low indices, it is advisable to go one step further and study the actual articles That mede up the index. However, the H-Index tells us nothing about whether someone presents himself as a scientist; this information must be gleaned from the person him(her)self.
These days, it has become a rare event – I am speaking of me publishing a paper in the peer-reviewed medical literature. But it has just happened: Spanish researchers and I published a meta-analysis on the effectiveness of craniosacral therapy. Here is its abstract:
The aim of this study was to evaluate the clinical effectiveness of craniosacral therapy (CST) in the management of any conditions. Two independent reviewers searched the PubMed, Physiotherapy Evidence Database, Cochrane Library, Web of Science, and Osteopathic Medicine Digital Library databases in August 2023, and extracted data from randomized controlled trials (RCT) evaluating the clinical effectiveness of CST. The PEDro scale and Cochrane Risk of Bias 2 tool were used to assess the potential risk of bias in the included studies. The certainty of the evidence of each outcome variable was determined using GRADEpro. Quantitative synthesis was carried out with RevMan 5.4 software using random effect models.
Fifteen RCTs were included in the qualitative and seven in the quantitative synthesis. For musculoskeletal disorders, the qualitative and quantitative synthesis suggested that CST produces no statistically significant or clinically relevant changes in pain and/or disability/impact in patients with headache disorders, neck pain, low back pain, pelvic girdle pain, or fibromyalgia. For non-musculoskeletal disorders, the qualitative and quantitative synthesis showed that CST was not effective for managing infant colic, preterm infants, cerebral palsy, or visual function deficits.
We concluded that the qualitative and quantitative synthesis of the evidence suggest that CST produces no benefits in any of the musculoskeletal or non-musculoskeletal conditions assessed. Two RCTs suggested statistically significant benefits of CST in children. However, both studies are seriously flawed, and their findings are thus likely to be false positive.
So, CST is not really an effective option for any condition.
Not a big surprise! After all, the assumptions on which CST is based fly in the face of science.
Since CST is nonetheless being used by many healthcare professionals, it is, I feel, important to state and re-state that CST is an implausible intervention that is not supported by clinical evidence. Hopefully then, one day, these practitioners will remember that their ethical obligation is to treat their patients not according to their beliefs but according to the best available evidence. And, hopefully, our modest paper will have helped rendering healthcare a little less irrational and somewhat more effective.
Looking at some ancient papers of mine, I came across a short BMJ paper from 1994. Here is a passage from it:
… A standard letter (on departmental letterhead) was written (in German) to all 189 firms that we identified as marketing herbal drugs in Germany. It asked (among other questions) for reprints of articles reporting controlled clinical trials on the company’s product(s).
Only 19 replies had reached us six weeks later. Four of these included at least one reprint. Twelve respondents regretted not knowing of clinical trials on their drug(s). In three cases we had written to a wrong address (one
instance) or to a firm which did not market phytomedicines (two instances).
These data, though far from conclusive, do not give the impression that research is in proportion to either prevalence or financial tumover of herbal remedies…
I wonder what the results would be, if we repeated this little excercise today, 30 years afteer the original investigation. I fear that the findings would be much the same or perhaps even worse. I also suspect that they would be similar regardless of the country we chose. Those who sell herbal remedies have very little incentive to do expensive clinical trials to test whether the products they earn their money with actually work. They may be doing well without it and ask themselves, why spend money on research that might not show what we hope and could easily turn out to jeopardize our financial success?
But the problem is by no means confined to herbal manufacturers (who would arguably have an important share to initiate and sponsor research). Even though fundamental questions remain unanswered, research into herbal medicine is scarce across the board.
To see whether this statement is true, I did a very quick Medline search. It showed that, in 2023, just over 13 000 papers on herbal medicine emerged. Of those, just 460 were listed as clinical trials. The latter figure is almost certainly considerably smaller than the true amount because Medline is over-generous in classifying papers as clinical trials. I thus estimate that only around 200 clinical trials of herbal medicine are conducted each year. Considering that we are dealing with thousands of herbs and ten thousands of herbal products, this figure is an embarrassment for the sector – which, as we have seen just days ago, is doing extremely well in finacial terms.
Dry needling is a therapy that is akin to acupuncture and trigger point therapy. It is claimed to be safe – but is this true?
Researchers from Ghent presented a series of 4 women aged 28 to 35 who were seen at the emergency department (ED) with post-dry needling pneumothorax between September 2022 and December 2023. None of the patients had any relevant medical history. All had been treated for a painful left shoulder, trapezius muscle or neck region in outpatient physiotherapist practices. At least three different physiotherapists were involved.
One patient presented to the ER on the same day as the dry needling procedure, the others presented the day after. All mentioned thoracic pain and dyspnoea. Clinical examination in all of these patients was unremarkable, as were their vital signs. Diagnosis was confirmed with ultrasound (US) and chest X-ray (CXR) in all patients. The latter exam showed left-sided apical pleural detachment with a median of 3.65 cm in expiration.
Two patients were managed conservatively. One patient (initial pneumothorax 2.5 cm) was discharged. The US two days later displayed a normally expanded lung. One patient with an initial apical size of 2.8 cm was admitted with 2 litres of oxygen through a nasal canula and discharged from the hospital the next day after US had shown no increase in size. Her control CXR 4 days later showed only minimal pleural detachment measuring 6 mm. The two other patients were treated with US guided needle aspiration. One patient with detachment initially being 4.5 cm showed decreased size of the pneumothorax immediately after aspiration. She was admitted to the respiratory medicine ward and discharged the next day. Control US and CXR after 1 week showed no more signs of pneumothorax. In the other patient, with detachment initially being 5.5 cm, needle aspiration resulted in complete deployment on US immediately after the procedure, but control CXR showed a totally collapsed lung 3 hours later. A small bore chest drain was placed but persistent air leakage was seen. Several trials of clamping the drain resulted in recurrent collapsing of the lung. After CT-scan had shown no structural deformities of the lung, suction was gradually reduced and the drain was successfully removed on the sixth day after placement. The patient was then discharged home. Control CXR 3 weeks later was normal.
The authors concluded that post-dry needling pneumothorax is, contrary to numbers cited in literature, not extremely rare. With rising popularity of the technique we expect complications to occur more often. Patients and referring doctors should be aware of this. In their informed consent practitioners should mention pneumothorax as a considerable risk of dry needling procedures in the neck, shoulder or chest region.
The crucial question, in my view, is this: do the risks of dry-needling out weigh the risks of this form of therapy? Let’s have a look at some of the recent evidence that we discussed on this blog:
- Spinal Manipulation and Electrical Dry Needling for Subacromial Pain Syndrome: A Nonsensical Trial
- Dry needling is useless for rehabilitation after shoulder surgery
- High velocity, low amplitude techniques are not superior to no treatment in the management of tension-type headache
- Which treatments are best for acute and subacute mechanical non-specific low back pain? A systematic review with network meta-analysis
- Acupuncture for chronic pain: the new NICE guideline
- Acupuncture for the Relief of Chronic Pain? A new, thorough synthesis fails to produce strong evidence that acupuncture works
The evidence is clearly mixed and unconvincing. I am not sure whether it is strong enough to afford a positive risk/benefit balance. In other words: dry needling is a therapy that might best be avoided.
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
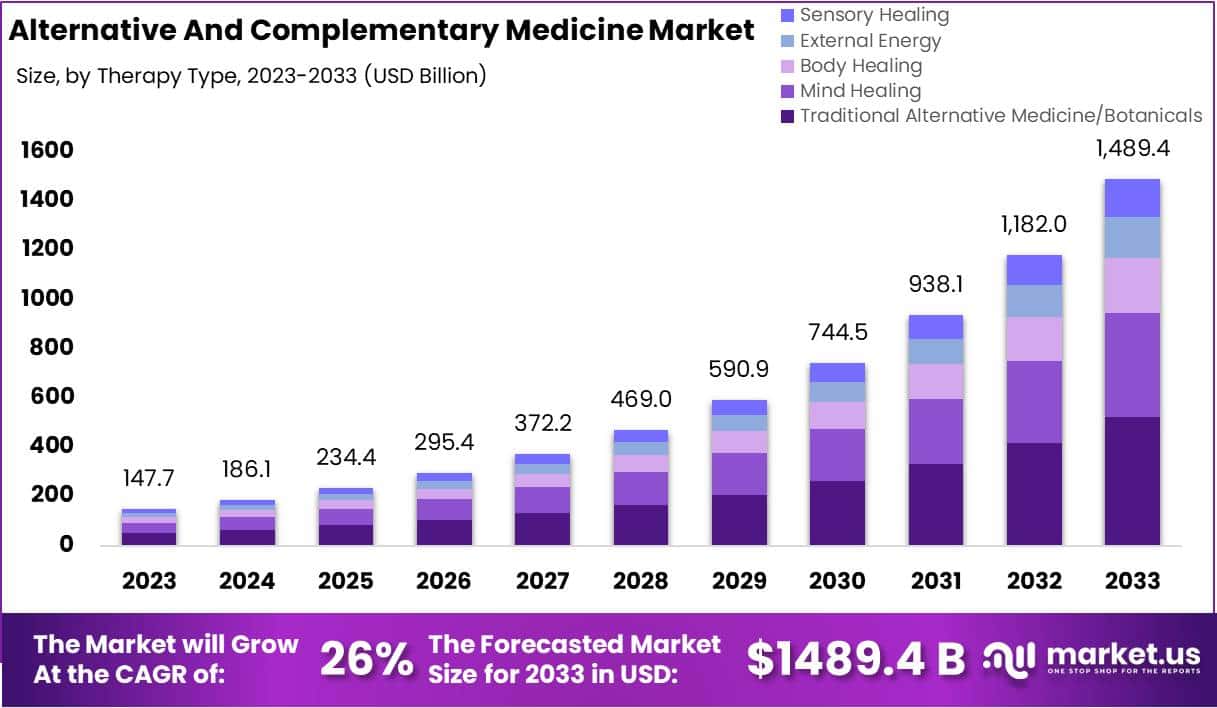
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.
