regulation
The following announcement was made by the NHS on 7 August 2018:
The Governing Body of Bristol, North Somerset and South Gloucestershire (BNSSG) Clinical Commissioning Group (CCG) today approved changes that mean NHS funded homeopathy will only be available in exceptional circumstances in the area. The changes will mean the CCG’s Individual Funding Request (IFR) Panel would need a clinician to set out why the patient is clinically exceptional before treatment could be provided.
The decision comes after the publication of a report, which took evidence from local people, clinicians, patient groups, providers of homeopathic treatments and national guidelines.
CCG Clinical Chair Dr Jonathan Hayes said, “We are working hard to become an evidence-informed organisation because we need to make the best use of all resources to offer treatment and care to the widest range of people. The decision on homeopathy funding today is a step towards this and brings us in line with national guidelines.”
It is estimated that 41 patients receiving NHS funded homeopathic consultations in the area cost the local NHS £109,476 in the 2017/2018 financial year.
END OF QUOTE

The move is the result of 4 years of excellent work by the GOOD THINKING SOCIETY, a charity dedicate to the promotion of rational thinking.
Michael Marshall, its Project Director, said: “We are very pleased to see the Bristol CCGs take this decision to cease funding for homeopathy – every other CCG across the country has made it clear that homeopathic remedies are no better than placebo and such there is simply no place for homeopathy on the NHS.
“With the end to homeopathy funding in Bristol, the region joins NHS bodies across the rest the country in recognising that homeopathy is not a valid use of limited NHS resources. There is now no CCG in England where homeopathic pills or consultations can be routinely funded with NHS money – instead, funding can be directed towards treatments that have been shown to actually work.”
Does that not call for a knighthood for Mr Marshall?
One would have thought so!
Who will tell Prince Charles to get the ball rolling?
And while we are all waiting for the big event, you might as well donate a few £s to this truly splendid charity.
Please be generous!!!
This recent announcement by the Society of Homeopaths (SoH), the organisation of non-doctor homeopaths in the UK, seems worthy of a short comment. Here is the unabbreviated text in question:
Two new members have been appointed to the Society’s Public Affairs (PAC) and Professional Standards (PSC) committees for three-year terms of office.
Selina Hatherley RSHom is joining the PAC. She has been a member since 2004 and works in three multi-disciplinary practices in Oxfordshire and previously ran a voluntary clinic working with people with drug, alcohol and mental health issues for 12 years. She has also been involved in the acute trauma clinics following the Grenfell Tower fire in 2017.
New to the PSC is Lynne Howard. She became a RSHom in 1996 and runs a practice in three locations in east London and a major London hospital. She specialises in pregnancy, birth and mother-and-baby issues.
“Following an open and comprehensive appointment process, we are delighted to welcome Selina and Lynne ‘on-board’ as brand-new committee members who will bring new ideas, experiences and knowledge to the society,” said Chief Executive Mark Taylor.
END OF QUOTE
It seems to me that the SoH might be breaching its very own Code of Ethics with these appointments.
1) Lynne Howard BA, LCH, MCH, RSHom tells us on her website that she has been practising homeopathy for 25 years, she has run many children’s clinics and is a registered CEASE practitioner with a special interest in fertility and children’s health.
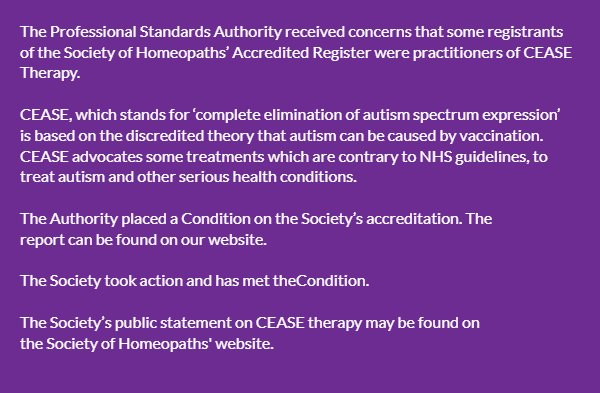
CEASE therapy has been discussed before on this blog. It is highly unethical and the SoH have been warned about it before. They even pretended to take the warning seriously.
 2) Selina Hatherley has a website where she tells us this: In 2011 I trained as a Vega practitioner – enabling me to use the Vega machine to test for food sensitivity and allergens. I use homeopathic remedies to support the findings and to help restore good health… I am a registered member of the Society of Homeopaths – the largest organisation registering professional homeopaths in Europe, I abide by their Code of Ethics and Practice and am fully insured.
2) Selina Hatherley has a website where she tells us this: In 2011 I trained as a Vega practitioner – enabling me to use the Vega machine to test for food sensitivity and allergens. I use homeopathic remedies to support the findings and to help restore good health… I am a registered member of the Society of Homeopaths – the largest organisation registering professional homeopaths in Europe, I abide by their Code of Ethics and Practice and am fully insured.
Vega, or electrodermal testing for allergies has been evaluated by the late George Lewith (by Jove not a man who was biased against such things) and found to be bogus. Here are the conclusions of his study published in the BMJ: “Electrodermal testing cannot be used to diagnose environmental allergies.” That’s pretty clear, I think. As the BMJ is not exactly an obscure journal, the result should be known to everyone with an interest in Vega-testing. And, of course, disregarding such evidence is unethical.
But perhaps, in homeopathy, ethics can be diluted like homeopathic remedies?
Perhaps the SoH’s Code of Ethics even allows such behaviour?
Have a look yourself; here are the 16 core principles of the SoH’s CODE OF ETHICS:
1.1 Put the individual needs of the patient first.
1.2 Respect the privacy and dignity of patients.
1.3 Treat everyone fairly, respectfully, sensitively and appropriately without discrimination.
1.4 Respect the views of others and, when stating their own views, avoid the disparagement of others either professionally or personally.
1.5 Work to foster and maintain the trust of individual patients and the public.
1.6 Listen actively and respect the individual patient’s views and their right to personal choice.
1.7 Encourage patients to take responsibility for their own health, through discussion and provision of information.
1.8 Comprehensively record any history the patient may give and the advice and treatment the registered or student clinical member has provided.
1.9 Provide comprehensive clear and balanced information to allow patients to make informed choices.
1.10 Respect and protect the patients’ rights to privacy and confidentiality.
1.11 Maintain and develop professional knowledge and skills.
1.12 Practise only within the boundaries of their own competence.
1.13 Respond promptly and constructively to concerns, criticisms and complaints.
1.14 Respect the skills of other healthcare professionals and where possible work in cooperation with them.
1.15 Comply with the current statutory legislation in relation to their practice as a homeopath of the country, state or territory where they are practising.
1.16 Practise in accordance with the Core Criteria for Homeopathic Practice and the Complementary and Natural Healthcare National Occupational Standards for Homeopathy.
______________________________________________________
I let you decide whether or not the code was broken by the new appointments and, if so, on how many accounts.
I have written about the ethics of pharmacists selling homeopathic preparations pretending they are effective medicines often – not just on this blog, but also in medical journals (see for instance here and here) and in our recent book. So, maybe I should give it a rest?
No!
I believe that the issue is far too important not to remain silent about it.
A recent article in the ‘Australian Journal of pharmacy’ caught my eye. As it makes a new and relevant point, I will quote some short excerpts for you:
One of the greatest criticisms pharmacists face is the ranging of homeopathic products in pharmacies. It is difficult to deny that ranging homeopathic products provides a level of legitimacy to these products that they do not deserve.
Conclusive evidence now exists [1] that homeopathy does not work. This is different from a lack of evidence for an effect; this is specific evidence that shows that this modality cannot and does not provide any of the purported benefits or mechanisms of action.
This evidence for lack of effect is important, due to the ethical responsibilities of pharmacists to provide evidence-based medicine. Specifically, from the Pharmaceutical Society of Australia’s Code of Ethics [2]:
Care Principle 1 g)
Before recommending a therapeutic product, considers available evidence and supports the patient to make an informed choice and only supplies a product when satisfied that it is appropriate and the person understands how to use it correctly.
It is not possible to adhere to this principle while also selling homeopathic and other non-EBM products – it is incumbent on pharmacists to always notify a patient that homeopathic medicines cannot work. Ranging homeopathic products therefore opens a pharmacist up to conflict of interest, where their professional judgement tells them that there is no benefit to a product, yet a patient wishes to purchase it anyway, even when advised not to. Not ranging a product is the only method of preventing this conflict.
Pharmacists may also find themselves in position where the pharmacy they work in ranges homeopathic or other non-EBM products, yet they do not want to be involved in the sale or recommendation of these products. In this situation, it is important to remember that the code of ethics requires that a pharmacist does not undertake any action or role if their judgement determines that this is not the correct course of action.
Integrity Principle 2
A pharmacist only practises under conditions which uphold the professional independence, judgement and integrity of themselves and others.
Professional misconduct
This leads to the professional risk a pharmacist puts themselves in when recommending or selling a product that lacks evidence … any breach of the code of ethics can be the basis of a report to the Pharmacy Board for professional misconduct. If a pharmacist were to be referred to the Pharmacy Board for recommending a non-EBM product, pharmacists will be put in the position of having to justify their decision to supply a product that has no evidence, especially if this supply harms a patient or delays them from accessing effective treatment. In addition, it will not be possible to make a case defending the decision to supply non-EBM products based on pressures from employers wishes, due to Integrity Principle 2.
Clearly, the use of Non-EBM products, including homeopathy, puts consumers at risk due to delayed treatment and the risk of unexpected outcomes. It also puts pharmacists at risk of professional and ethical reprimand. Relying on evidence, and having a working knowledge of how to access and assess this evidence, remains a critical part of the role of pharmacists in all areas of practice.
[1] https://www.nhmrc.gov.au/guidelines-publications/cam02
[2] https://www.psa.org.au/downloads/codes/PSA-Code-of-Ethics-2017.pdf
END OF QUOTE
I find this comment important: we all knew (and I have dwelled on it repeatedly) that pharmacists can put consumers at risk when they sell homeopathic remedies masquerading as medicines (while in truth they are placebos that cure absolutely nothing). What few people so far appreciated, I think, is the fact that pharmacists also put themselves at risk.
Of course, you might say, this is a view from Australia, and it might not apply elsewhere. But I think, because the codes of ethics differ only marginally from country to country, it might well apply everywhere. If that is so, pharmacists across the globe – most of them do sell homeopathics regularly – are in danger of breaking their own codes of ethics, if they recommend or sell homeopathic products. And violating professional ethics must mean that pharmacists are vulnerable to reprimands.
Perhaps we should all go to our next pharmacy, ask for some advice about homeopathy, and test this hypothesis!
With depressing regularity, we hear that this or that VIP has decided to travel to Germany to get her/his cancer cured. As long as I can remember, cancer quackery has been wide-spread in Germany. More recently, dozens of private clinics have sprung up that seem to specialise in treating rich, foreign cancer patients. The message they like to send out is that, in Germany, one gets more advanced and effective treatments.
Having looked at some of the clinics’ websites, I do, however, not get the impression that this is true. For instance, one clinic that is often mentioned offers amongst other treatments the following (the descriptions are quotes from the clinic’s website):
- Orthomolecular medicine aims to restore the ideal and beneficial environment of the body by correcting molecular imbalances, and this approach is used in cancer, infections, depression and atherosclerosis, among others.
- Here at the Hallwang Private Oncology Clinic every patient receives a well-balanced supportive infusion program consisting of anti-inflammatory, potent anti-oxidant and detoxifying substances, which help you recover from previous treatments, minimize side effects from current treatments and strengthen your immune system to enhance treatment effects. Substances used are for example vitamin C, selenium, zinc, L-ornithine aspartate, glutathione, alpha lipoic acid, among many others.
- Vitamin C, also known as ascorbic acid, is an essential vitamin. It is a potent antioxidant which helps to protect against free radical damage to our proteins, fats, carbohydrates, DNA and RNA. Vitamin C is used to boost the immune system.
- Ozone is a powerful oxidizing agent. While high concentrations can be toxic, small ozone doses may increase naturally occurring antioxidants in the body. Antioxidants help to eliminate malignant calles and are needed to keep the body healthy. Ozone used for treatment is known for its bactericidal, fungicidal and virostatic properties. It also stimulates circulation and immune functions, and revitalizes the body.
- Hyperbaric oxygen therapy is used to treat several medical conditions. It is a well-established treatment for decompression sickness, a hazard of scuba diving. Other conditions treated with hyperbaric oxygen therapy include serious infections, skin lesions or radiation injury. Wounds for example need oxygen to heal properly, and exposing a wound to 100 percent oxygen can improve and speed the healing process. This has been shown in a number of studies. The goal of this treatment is to increase the amount of oxygen your blood can carry in order to restore normal levels of blood gases and tissue function to promote healing and cure infection.
- Whole body hyperthermia can be applied in a number of different diseases, including malignant, immunological, viral and other diseases. The aim of WBH is the destruction of malignant cells by induction of apoptosis via hyperthermia along with elimination of malignant cells that have become resistant to chemotherapy. With the help pf WBH, effects of other treatments, including chemotherapy and immunotherapy, can be enhanced.
END OF QUOTES
This does not look like cutting edge cancer therapy at all; in fact, none of these treatments are new and none have been shown to cure cancer or any other condition. Thus they are all examples of cancer quackery.
But, to be fair, the clinic in question (and most similar institutions in Germany) also employs a range of conventional cancer therapies. I am not an oncologist and therefore not competent to comment on these treatments; I leave this to someone who is competent; this is what David Gorski writes about them: Hallwang uses very experimental treatments in a “blunderbuss” fashion, basically throwing everything but the kitchen sink together with no sophistication. We can’t even know if these doctors know what the hell they are doing. Patients are treated, and, as far as we can tell, no systematic record of how well these patients do and how long they survive is kept, or, if such records are kept, they are kept secret.
One might, of course, argue that many patients are suffering from terminal cancers. They are desperate and have a right to try anything. As good physicians, we must not take their hope away. I would not dispute that; on the contrary, these patients deserve the best care we can muster. But I would still warn them to be cautious, and again I concur with David Gorski: People will often say of a terminal illness: How could things get any worse? The lesson of Hallwang tells us. Things can get worse if you’re induced into chasing false hope. Things can get worse if you are enticed into eschewing effective palliative treatment and suffer more than is necessary—or even die prematurely from the treatment. Things can get worse if you drain your life’s savings, leave nothing behind for your family, and spend the rest of your life chasing ever more money. Things can get worse if your family joins you in draining their life’s savings to pay for your treatments. Things can always get worse, and quack cancer clinics virtually guarantee that they will.
In view of all this, I feel strongly that it is high time the German regulators have a close look at the plethora of cancer quackery and find a way of stopping this unethical, despicable exploitation.
This study examined websites of naturopathic clinics and practitioners in the provinces of British Columbia and Alberta, looking for the presence of discourse that may contribute to vaccine hesitancy, and for recommendations for ‘alternatives’ to vaccines or flu shots.
Of the 330 naturopath websites analysed, 40 included vaccine hesitancy discourse and 26 offered vaccine or flu shot alternatives. Using these data, the authors explored the potential impact such statements could have on the phenomenon of vaccine hesitancy.
Next the researchers considered these misrepresentations in the context of Canadian law and policy, and outlined various legal methods of addressing them. They concluded that tightening advertising law, reducing CAM practitioners’ ability to self-regulate, and improving enforcement of existing common and criminal law standards would help limit naturopaths’ ability to spread inaccurate and science-free anti-vaccination and vaccine-hesitant perspectives.
The paper listed some poignant examples of vaccine hesitancy discourse:
1) ‘…children are now being given increasing numbers of vaccinations containing potentially harmful derivatives and substances such as mercury, thimerisol [sic], aluminum and formaldehydes. These harmful derivatives can become trapped in our tissues, clogging our filters and diminishing one’s ability of further toxins out.’ — www.evolvenaturopathic.com
2) ‘Vaccines given to children and adults contain mercury and aluminum. Babies are especially susceptible to small amounts of mercury injected directly into their tiny bodies. It is now suspected that the increase in autism and Asperger Syndrome is related to the mercury in childhood vaccinations.’ — www.vancouvernaturopathicclinic.com
3) ‘The conventional Flu Shot is a mixture of 3 strains of flu viruses mixed with a number of chemical preservatives and these strains are based on a prediction of what flu viruses some medical experts think will be the most problematic this season. This is really an impossible prediction to make when we have thousands of different strains of viruses that are continuously mutating.’ — www.advancednaturopathic.com
4) ‘A [sic] epidemiologist researcher from British Columbia, Dr. Danuta Skowronski, published a study earlier this year showing that people who were vaccinated consecutively in 2012, 2013 and 2014 appeared to have a higher risk of being infected with new strains of the flu.’ — www.drtas.ca
5) ‘Increasing evidence suggests that injecting a child with nearly three dozen doses of 10 different viral and bacterial vaccines before the age of five, while the immune system is still developing, can cause chronic immune dysfunction. The most that vaccines can do is lead to an increase in antibodies to a specific disease.’ — www.evolvevitality.com
6) ‘The bugs in question (on the Canadian Vaccine List) can enter our systems and depending on our bodies, our histories, and mostly the bugs’ propensity, they can cause serious harm. There are certainly questionable ingredients in vaccines that have the potential to do the same.’ — www.tharavayali.ca
The authors also considered that, in Canada, a naturopath who recommends homeopathic vaccines or who counsels against conventional vaccination could potentially be criminally negligent. Section 219 of the Criminal Code of Canada [Code] states that ‘[e]very one is criminally negligent who, in doing anything, or in omitting to do anything that it is his duty to do, shows wanton or reckless disregard for the lives or safety of other persons’. Subsection (2) goes on to state that, for the purposes of criminal negligence, ‘duty’ means a duty imposed by law; a legal duty in this context is one arising from statute or from the common law. The Code creates a legal duty for anyone ‘who undertakes to administer surgical or medical treatment to another person or to do any other lawful act that may endanger the life of another person’ to ‘have and to use reasonable knowledge, skill and care in so doing’. This duty is a uniform standard, meaning the requirement of reasonable knowledge, care, and skill is based on the treatment or lawful act in question, not on the level of experience of the person administering it. As such, naturopaths offering services similar to medical doctors will be held to the same standards under the Code.
Criminal negligence occurs due to the ‘failure to direct the mind to a risk of harm which [a] reasonable person would have appreciated’. Fault is premised on the wrongful act involved, rather than the guilty mind of the perpetrator. Naturopaths counseling patients against vaccination are arguably undertaking a lawful act that endangers the life of another person (especially in the case of a young child, elderly individual, or immunocompromised person), breaching s.216 of the Code. In addition, since relevant legal duties include those arising through the common law, naturopaths could alternatively be criminally negligent for failing to satisfy the aforementioned duty of reasonable disclosure inherent to standard of care in tort. In the context of a community with diminished vaccination rates, either failure could be considered wanton or reckless, as it may greatly and needlessly endanger the patient. However, under the standard for criminal negligence, the trier of fact must ‘assess whether the accused’s conduct, in view of his or her perception of the facts, constituted a marked and substantial departure from what would be reasonable in the circumstances’. This is similar to the standard of gross negligence, so ultimately a finding of criminal negligence would require meeting a rather onerous threshold.
______________________________________________________________________________
This, of course, is according to Canadian law; but I imagine that the law in other countries must be similar.
Therefore, this is a legal opinion which might be worth considering also outside Canada.
If there is a legal expert amongst my readers, please do post a comment.
An article has just been published announcing the reform of the German Heilpraktiker, the profession of alternative practitioners that has been discussed repeatedly on this blog and criticised recently by the ‘Muensteraner Kreis’. As the new article is in German, I will try to summarise the essence of it here:
The health ministers of all German counties have decided yesterday that they will start reforming the profession of the Heilpraktiker that has attracted much criticism in recent months. The current laws are no longer fit for purpose. There is neither a mandatory agreement for the education of the Heilpraktiker, nor a uniform regulation of the profession.
The senator for health from Hamburg stated: “We feel that the Heilpraktiker should not be allowed to do certain thing, but be permitted to do plenty of activities that remain legal.” At present, the Heilpraktiker is allowed to treat fractures, malignancies, give injections, and even manufacture certain medicines. “We believe there is a need for regulation to protect patients.”
Now a working group will be formed to investigate and produce a report within a year. Remarkably, the German health secretary avoided commenting. In a statement, it was said that patients must be empowered to make decisions on the basis of quality-assured information.
The full German text is below.
__________________________________________________________________________________
Nach mehreren deutschlandweit Aufsehen erregenden Todesfällen beispielsweise von Krebspatienten, die kurz nach der Therapie durch einen Heilpraktiker in Brüggen-Bracht starben, will die Politik sich nun diesen Berufszweig vornehmen. Die Gesundheitsminister aller Bundesländer haben am Donnerstag beschlossen, eine Reform anzugehen. „Das unzureichend regulierte Heilpraktikerwesen mit seiner umfassenden Heilkundebefugnis steht unverändert in der Kritik“, heißt es in einer Erklärung. Das Heilpraktikergesetz könne dem heutigen Anspruch an den Gesundheitsschutz der Patienten nicht mehr gerecht werden. Für Heilpraktiker gebe es weder verbindliche Regeln zur Ausbildung noch eine einheitliche Berufsordnung. Andere Gesundheitsberufe müssten hingegen strenge Qualifikationskriterien erfüllen.
„Wir sehen es als kritisch an, dass einige Tätigkeiten zwar den Heilpraktikern untersagt sind, aber es noch eine Fülle von Tätigkeiten gibt, die zugelassen sind“, sagte die Hamburger Senatorin für Gesundheit, Cornelia Prüfer-Storcks, auf einer Pressekonferenz – sie hatte die Initiative maßgeblich vorangetrieben. So dürfen Heilpraktiker Knochenbrüche therapieren, schwere und bösartige Erkrankungen behandeln und Injektionen geben. Selbst die Herstellung von Arzneimitteln für bestimmte Patienten sei Heilpraktikern erlaubt. „Ohne die Prüfmechanismen, die wir normalerweise haben, wenn wir Arzneimittel zulassen und produzieren“, kritisierte Prüfer-Storcks. „Wir glauben, dass es hier Regelungsbedarf gibt aus Sicht des Patientenschutzes.“
„Die Ministerinnen und Minister, Senatorinnen und Senatoren für Gesundheit sehen eine zwingende Reformbedürftigkeit des Heilpraktikerwesens“, heißt es in dem kurzen, MedWatch vorliegenden Beschluss. „Der Bund wird gebeten, eine Bund-Länder-Arbeitsgruppe einzurichten, die eine grundlegende Reform des Heilpraktikerwesens prüft.“ Das Ergebnis der Prüfung solle bis zur Gesundheitsministerkonferenz in einem Jahr vorgelegt werden.
Bundesgesundheitsminister Jens Spahn erklärte auf der Pressekonferenz das Patientenwohl zwar zum entscheidenden Maßstab für die Gesundheitspolitik. „Deshalb finde ich es richtig, dass die Gesundheitsministerkonferenz bei der Patientenorientierung ihren Schwerpunkt setzt“, sagte er. Auf mögliche Reformen des Heilpraktikerberufes ging der Minister bei der Pressekonferenz jedoch nicht ein. Inwiefern sein Haus die von den Landesministern geforderte Reform des Heilpraktikerwesens mit unterstützen wird, bleibt offen. Auf Nachfrage, ob das Ministerium eine Bund-Länder-Arbeitsgruppe unterstützen würde, versteckte sich eine Sprecherin bereits im Mai hinter der Mini-Reform von Gröhe. Mit Blick auf die kurze Zeit seit Inkrafttreten dieser Änderungen sei es angemessen, zunächst zu prüfen, ob und inwieweit diese zum Schutz des Patientenwohles beiträgt, erklärte sie – „ehe weitere gesetzliche Maßnahmen in Betracht gezogen werden sollten“.
In einem Grundsatzbeschluss sprach sich die Gesundheitsministerkonferenz außerdem für „Patientenorientierung als Element einer zukunftsweisenden Gesundheitspolitik“ aus. „Das heißt, dass der Patient natürlich das Heft in der Hand haben muss, dass er versteht, was mit ihm gemacht wird, warum es mit ihm gemacht wird, mit welchen Chancen die Behandlung verbunden ist“, sagte NRW-Gesundheitsminister Karl Laumann. Auch in der Ausbildung des Gesundheitspersonals sollten diese Aspekte einen großen Stellenwert bekommen, betonte Laumann – und erwähnte zwar Ärzte als Berufsgruppe explizit, nicht aber Heilpraktiker. Der frühere Bundespatientenbeauftragte forderte außerdem mehr Transparenz ein. In Teilen des Gesundheitssystems gebe es wegen mangelnder Transparenz „eine gewisse Misstrauenskultur“, sagte er.
Die Minister wollen laut dem Beschluss die Patientensouveränität und der Orientierung im Gesundheitswesen verbessern, die Gesundheitskompetenz und gesundheitliche Eigenverantwortung beispielsweise durch die Einrichtung eines nationalen Gesundheitsportals deutlich stärken und Kommunikation und Wissenstransfer zwischen Patienten und allen Beteiligten im Gesundheitswesen fördern. „Patienten sollen so in die Lage versetzt werden, ihre Interessen besser zu vertreten und ihre Entscheidungen auf der Basis qualitätsgesicherter Informationen zu treffen“, heißt es.
Kommunikationskompetenz und wertschätzende Beziehungsgestaltung sei im Gesundheitswesen von wesentlicher Bedeutung für die Partizipation, Qualität, Sicherheit und den Erfolg der gesundheitlichen Prävention und der medizinischen Behandlung, betonen die Minister. Allgemeinverständliche „Patientenbriefe“ sollen als erster Schritt die Informiertheit von Patienten nach Krankenhausbehandlungen erhöhen. Außerdem soll das Bundesgesundheitsminister eine Pflicht schaffen, dass niedergelassene Ärzte ihren Patienten neutrale und evidenzbasierte schriftliche Informationen zu Zusatzangeboten – sogenannten „Individuellen Gesundheitsleistungen“ – zur Verfügung stellen müssen.
Bei Behandlungsfehlern sollen nach Ansicht der Landesminister auf Bundesebene weitere Erleichterungen umgesetzt werden: Die Beweislast und das Beweismaß soll zu Gunsten von Patienten überarbeitet werden. Außerdem sollten Krankenkassen gesetzlich verpflichtet werden, Patienten beim Nachweis eines Behandlungsfehlers besser zu unterstützen.
______________________________________________________________________________
I have been banging on about the German Heilpraktiker, its infamous history and its utter inadequacy since many years. This is what I published in 1996, for instance:
Complementary medicine is increasing in popularity. In most countries its practice is in the hands of non-medically trained practitioners, professions which are often not properly regulated. When discussing solutions to this problem the German “Heilpraktiker” is often mentioned. The history and present situation of this profession are briefly outlined. The reasons why the “Heilpraktiker concept” is not an optimal solution are discussed. It is concluded that the best way forward consists of regulation and filling the considerable gaps in knowledge relating to complementary medicine.
It goes without saying that, after so many tears of warning about the risks involved in allowing poorly trained practitioners, who are all too often unable to see the limits of their competency (and after many unnecessary fatalities), I am delighted that progress seems finally to be on the horizon.
The ‘Pharmaceutical Journal’ just published a ‘pro/contra’ piece discussing whether UK community pharmacists should be selling homeopathic remedies to the public. Here are the essential parts of both arguments:
PRO
… I do not believe there is good scientific evidence to validate homeopathic remedies as medicines, but it is important to provide patients with choice in an informed environment — pharmacists and pharmacy teams are able to provide this expertise.
It is better for the public to buy these products from a reputable source where the community pharmacist — the expert on medicines — can provide professional advice, which is not available from unregulated online suppliers or other non-healthcare outlets…
So, I’m not here to argue the science: I argue that some people can benefit from homeopathy.
We ought to explore homeopathy’s placebo effect. Placebos are often dismissed as fakes, but they seem to act on the same brain pathways that are targeted by ‘real’ treatments. I wonder whether, through the placebo effect, homeopathy has a role to play in mental health treatment and pain relief. Whether for anxiety, mild-to-moderate depression, sleeplessness or stress, taking a little white tablet may benefit the patient, have fewer side effects than conventional medication, cause no harm, and is better than an excess of alcohol or illegal drugs.
Of course, homeopathy should not replace conventional medicines, and people should continue to be vaccinated, should use their inhalers and take their insulin. Homeopathy should not be funded on the NHS, but we do not live in a nanny state.
The clinical efficacy of many other products sold in the pharmacy is also questionable, but we still provide them. One example is guaifenesin for chesty coughs, which, at over-the-counter strength, provides a suboptimal dose. Many people are sceptical of the benefits of vitamin and mineral supplements. Bach flower remedies claim to tackle stress. We drink herbal tea for its ‘health’ benefits or buy fortified cereals because they are ‘better for you’, but these benefits are not clinically proven.
If the public finds comfort in a complementary therapy — whether it is acupuncture, reflexology, vitamins or homeopathy — I am happy to offer that choice, as long as the chosen therapies do no harm, and people continue to take their prescribed medicines.
If the patient wants my professional advice, I will explain that homeopathic medicines are not clinically proven but they may help certain conditions. I will probably recommend a different product, but at least I am there to do so.
You will not find a pharmacist in a health shop or on the internet, but in the community pharmacy you will find a highly qualified medicines expert, who will advise and inform, and who truly cares about the public’s health.
CONTRA
… given pharmacy’s heavy promotion of homeopathy, I feared that the profession was in danger of losing science as its bedrock.
… in 2009, a London-based pharmacy was supplying homeopathic ‘swine flu formula’. This was a dangerous practice but government agencies failed to regulate it effectively or to close it down.
In 2010, the then professional standards director at Boots, Paul Bennett (now chief executive, Royal Pharmaceutical Society), appeared before the Science and Technology Committee in its discussion of homeopathy’s availability on the NHS. Bennett stood by the sale of homeopathic remedies in Boots’ stores: “It is about consumer choice for us,” he said. I disagree with this argument.
Like the sale of cigarettes in US pharmacies, homeopathy threatens to fatally damage the reputation of community pharmacy. Pharmacies that sell homeopathic remedies give them unjustified credibility. Informed patient choice should be king; if pharmacists, pharmacy staff and shelf-barkers fail to clearly inform customers that homeopathic remedies are no more effective than placebo, we have acted unethically.
Yet Boots, perhaps alarmed by the number of subsequent protests against homeopathy outside its stores, got the message. Its website now reflects a more scientific approach: the homeopathic remedies it supplies state that they are “without approved therapeutic indications”. Boots also seems to have modified its range and offering of homeopathic remedies. So there is hope for community pharmacy.
Homeopathic remedies are still sold in pharmacies only because they make a profit. Sales in pharmacy are nonsense because, as most homeopathic practitioners claim, it is not possible to sell homeopathic remedies in isolation of a homeopathic consultation. The consultation determines the remedy. Off-the-shelf homeopathy is a relatively recent phenomenon.
The remedies are no more effective compared with placebo, anyway. Systematic reviews from the Cochrane Library — the gold standard of medical science — have considered homeopathy in the treatment of dementia, asthma and attention deficit hyperactivity disorder, all of which have confirmed the placebo effect. Irritatingly, supporters of homeopathy will always, in any debate, quote a bunkum study that shows some possible efficacy. Some might argue that placebo, or suggestion, is effective therapy, so why not use it? We must question the ethics of this approach.
Pharmacists act immorally when they sell the products without making clients aware that homeopathy does not work.
… I find that most pharmacists, when asked, appreciate that homeopathy has no scientific basis and provides merely a placebo effect. I sincerely hope that with this insight, pharmacy will finally clear its shelves of this expensive hocus pocus for good.
____________________________________________________________________________
I find both pieces quite weak and poorly argued. In fact, the ‘pro’ – arguments are quite laughable and could easily be used for teaching students the meaning and use of logical fallacies. In my view, all that needs to be pointed out here is this:
- Homeopathy is based on implausible assumptions.
- Despite 200 years of research and around 500 clinical trials, there is still no proof that highly diluted homeopathic remedies have effects beyond placebo.
- Therefore, selling them to the naïve public, while pretending they are real medicines, is dishonest, arguably fraudulent and certainly not the behaviour one would expect of a healthcare professional.
- Pharmacists who nevertheless sell these remedies as medicines are in breach of their very own regulations.
_____________________________________________________________________________
Strangely enough, when trying to find the relevant passage from the code of ethics for UK pharmacists, I struggled. The General Pharmaceutical Council’s ‘Standards fro Pharmacy Professionals‘ merely states this:
People receive safe and effective care when pharmacy professionals reflect on the application of their knowledge and skills and keep them up-to-date, including using evidence in their decision making. A pharmacy professional’s knowledge and skills must develop over the course of their career to reflect the changing nature of healthcare, the population they provide care to and the roles they carry out. There are a number of ways to meet this standard and below are examples of the attitudes and behaviours expected.
People receive safe and effective care when pharmacy professionals:
- recognise and work within the limits of their knowledge and skills, and refer to others when needed
- use their skills and knowledge, including up-to-date evidence, to deliver care and improve the quality of care they provide
- carry out a range of continuing professional development (CPD) activities relevant to their practice
- record their development activities to demonstrate that their knowledge and skills are up to date
- use a variety of methods to regularly monitor and reflect on their practice, skills and knowledge
This, I admit, is not as clear as I had hoped (if my memory serves me right, this used to be much more explicit; in case anyone knows of a more suitable section in the code of ethics, please let me know); but it does preclude selling placebos, while pretending they are effective medicines.
When NHS England announced several months ago that they plan to stop the reimbursement of homeopathy, UK homeopaths were understandably upset and decided to launch a legal challenge to this decision. Yesterday, the result of this challenge has been published in a NHS press-release:
START OF QUOTE
NHS chief Simon Stevens has today welcomed the High Court’s decisive rejection of a legal challenge by the British Homeopathic Association to overturn plans to no longer routinely fund homeopathy on the NHS.
As part of action to clamp down on waste, over the last two years NHS England has taken action to curb prescriptions for medicines that can be bought over the counter or are of low value.
At the end of last year NHS England published guidance to curb prescriptions for 18 ineffective, unsafe or low clinical priority treatments, such as coproxamol, some dietary supplements, herbal treatments and homeopathy, saving up to £141 million a year. Earlier this year NHS England published a further list of 35 minor, short-term conditions for which over the counter medicines should not routinely be prescribed, saving around a further £100 million a year.
Savings form a key building block of the NHS’s 10 point efficiency plan contained in the Next Steps on the NHS Five Year Forward View, published in March 2017.
NHS chief, Simon Stevens said: “There is no robust evidence to support homeopathy which is at best a placebo and a misuse of scarce NHS funds.
“So we strongly welcome the High Court’s clear cut decision to kick out this costly and spurious legal challenge.”
Guidance on items which should not be routinely prescribed in primary care is available on the NHS England website.
END OF QUOTE
The reaction of UK homeopaths was as swift and deluded as it was predictable. The British Homeopathy Association, for instance, commented thus:
… The charity’s main claims against NHS England were that the consultation misrepresented homeopathy and therefore was unfair; and a report used in the consultation to inform the public was so complicated it would deter rather than encourage people to respond. Although the judge found there were sufficient grounds for a judicial review, after four days of lengthy legal arguments he dismissed the claims. Margaret Wyllie, BHA Chair, said the case highlighted how health bosses were unfairly manipulating the consultation process and making decisions about healthcare services without genuine patient engagement. “That NHS England attracted fewer than 3,000 responses from patients to a national consultation that ran for three months highlights its failure to genuinely engage with the public on important decisions about healthcare provision. Although 18 medicines were under review the only negative statement in NHS England’s press release promoting its public consultation was about homeopathy. The statement was so prejudicial it was widely reported in the media that the decision to deny patients homeopathic medicines had already been taken. How the judge failed to recognise that this was a deliberate attempt by NHS England to unfairly influence the public is astonishing,” said Mrs Wyllie.
In The Telegraph, Wyllie is quoted saying: “It appears NHS England can fail to engage with patients properly on removing services and get away with it. That is not good enough, for it is important to remember that the real losers in this case are the patients who are now being refused a treatment on which they have come to depend.”
One can only marvel at the lack of insight and self-criticism. I should to add that the BHA is a charity; with this court case, they have wasted significant amounts of public money for their own, hopelessly misguided interests. To me, this indicates that they no longer deserve a charitable status.
Personally, I had very little doubt that the court would decide as it did. The evidence was simply overwhelming and indisputable. In the written judgement, the judge stated that “I am satisfied that NHSE was rigorous in the discharge of the duty to have “due regard” to relevant matters, and that it was entitled, on the evidence before it, to conclude that the Guidance would not have an adverse impact on the statutory equality objectives, but rather, as the Analysis found, “would [enable] patients to have access to the most effective medications to achieve the best outcomes”.
In all this, the open questions, in my view, were whether
- Prince Charles, the prime defender of quackery in the UK, would intervene,
- and whether his intervention might change anything.
So, did he try to intervene?
I do not know. It could be that, after all the hoo-ha about his spider memos, he now is a little more cautions about meddling in health politics. It could also be that, as he is getting ready to become king, he wants to keep a low profile about his more bizarre ideas. Lastly, it could be that his opinion does not weigh as heavily as I had feared.
In any case, The High Court ruling is most welcome and unquestionably just, progressive, and long-overdue. I applaud all who have worked hard to bring it about, and am sure that (most of) my readers agree.
On this blog, we have seen more than enough evidence of how some proponents of alternative medicine can react when they feel cornered by critics. They often direct vitriol in their direction. Ad hominem attacks are far from being rarities. A more forceful option is to sue them for libel. In my own case, Prince Charles went one decisive step further and made sure that my entire department was closed down. In China, they have recently and dramatically gone even further.
This article in Nature tells the full story:
A Chinese doctor who was arrested after he criticized a best-selling traditional Chinese remedy has been released, after more than three months in detention. Tan Qindong had been held at the Liangcheng county detention centre since January, when police said a post Tan had made on social media damaged the reputation of the traditional medicine and the company that makes it.
On 17 April, a provincial court found the police evidence for the case insufficient. Tan, a former anaesthesiologist who has founded several biomedical companies, was released on bail on that day. Tan, who lives in Guangzhou in southern China, is now awaiting trial. Lawyers familiar with Chinese criminal law told Nature that police have a year to collect more evidence or the case will be dismissed. They say the trial is unlikely to go ahead…
The episode highlights the sensitivities over traditional Chinese medicines (TCMs) in China. Although most of these therapies have not been tested for efficacy in randomized clinical trials — and serious side effects have been reported in some1 — TCM has support from the highest levels of government. Criticism of remedies is often blocked on the Internet in China. Some lawyers and physicians worry that Tan’s arrest will make people even more hesitant to criticize traditional therapies…
Tan’s post about a medicine called Hongmao liquor was published on the Chinese social-media app Meipian on 19 December…Three days later, the liquor’s maker, Hongmao Pharmaceuticals in Liangcheng county of Inner Mongolia autonomous region, told local police that Tan had defamed the company. Liangcheng police hired an accountant who estimated that the damage to the company’s reputation was 1.4 million Chinese yuan (US$220,000), according to official state media, the Beijing Youth Daily. In January, Liangcheng police travelled to Guangzhou to arrest Tan and escort him back to Liangcheng, according to a police statement.
Sales of Hongmao liquor reached 1.63 billion yuan in 2016, making it the second best-selling TCM in China that year. It was approved to be sold by licensed TCM shops and physicians in 1992 and approved for sale over the counter in 2003. Hongmao Pharmaceuticals says that the liquor can treat dozens of different disorders, including problems with the spleen, stomach and kidney, as well as backaches…
Hongmao Pharmaceuticals did not respond to Nature’s request for an interview. However, Wang Shengwang, general manager of the production center of Hongmao Liquor, and Han Jun, assistant to the general manager, gave an interview to The Paper on 16 April. The pair said the company did not need not publicize clinical trial data because Hongmao liquor is a “protected TCM composition”. Wang denied allegations in Chinese media that the company pressured the police to pursue Tan or that it dispatched staff to accompany the police…
Xia is worried that the case could further silence public criticism of TCMs, environmental degredation, and other fields where comment from experts is crucial. The Tan arrest “could cause fear among scientists” and dissuade them from posting scientific comments, he says.
END OF QUOTE
On this blog, we have repeatedly discussed concerns over the validity of TCM data/material that comes out of China (see for instance here, here and here). This chilling case, I am afraid, is not prone to increase our confidence.
I have written about the use of homeopathy in France before (as I now live half of my time in France, this is a subject of considerable interest to me). After decades of deafening silence and uncritical acceptance by the French public, it seems that finally some change to the better might be on its way. Recently, a sizable number of prominent doctors protested publicly against the fact that, despite its implausibility and the lack of proof of efficacy, homeopathy continues to be reimbursed in France and scarce funds are being wasted on it. This action seems to have put pressure on officials to respond.
Yesterday (just in time for the ‘HOMEOPATHIC AWARENESS WEEK’) the French minister of health was quoted making a statement on homeopathy. Here is my translation of what Agnès Buzyn was quoted saying:
“There is a continuous evaluation of the medicines we call complementary. A working group* at the head office of my department checks that all these practices are not dangerous. If a therapy continues to be beneficial without being harmful, it continues to be reimbursed… The French are very attached [to homeopathy]; it’s probably a placebo effect. If it can prevent the use of toxic medicine, I think that we all win. I does not hurt.”

- I would like to know who they are, how they can be contacted, and whether they would consider recruiting my assistance in evaluating alternative therapies.
So, if I understand her correctly, Agnès Buzyn believes that:
- the French people are fond of homeopathy;
- homeopathy is a placebo-therapy;
- homeopathy does no harm;
- homeopathy can even prevent harm from conventional medicine;
- on balance, therefore, homeopathy should continue to be reimbursed in France.
My views of this type of reasoning have been expressed repeatedly. Nevertheless, I will briefly state them again:
- true but not relevant; healthcare is not a popularity contest; and the current popularity is essentially the result of decades of systematic misinformation of consumers;
- correct;
- wrong: we have, on this blog, discussed ad nauseam how homeopathy can cause serious harm; for instance, whenever it replaces effective treatments, it can cause serious harm and might even kill patients;
- if doctors harm patients by needlessly prescribing harmful treatments, we need to re-train them and stop this abuse; using homeopathy is not the solution to bad medicine;
- wrong: the reimbursement of homeopathy is a waste of money and undermines evidence-based medicine.
So, what’s the conclusion?
Politicians are usually not good at understanding science or scientific evidence. They (have to?) think in time spans from one election to the next. And they are, of course, keenly aware that, in order to stay in power, they rely on the vote of the people. Therefore, the popularity of homeopathy (even though it is scientifically irrelevant) is a very real factor for them. This means that, on a political level, homeopathy is sadly much more secure than it should be. In turn, this means we need to:
- use different arguments when arguing with politicians (for instance, the economic impact of wasting money on placebo-therapies, or the fact that systematically misinforming the public is highly unethical and counter-productive),
- and make politicians understand science better than they do at present, perhaps even insist that ministers are experts in their respective areas (i. e. a minister of health fully understands the fundamental issues of healthcare).
Does that mean the new developments in the realm of French homeopathy are all doomed to failure?
No, I don’t think so – at least (and at last) we have a vocal group of doctors protesting against wasteful nonsense, and a fairly sound and accurate statement from a French minister of health:
HOMEOPATHY, IT’S PROBABLY A PLACEBO EFFECT!
