pseudo-science
I was alerted to the following conference announcement:
The MEP Interest Group on Integrative Medicine and Health is delighted to invite you to the event ‘Integrative Medicine and Health in prevention and management of COVID-19 and long COVID’ on Thursday 2 June 16.00–18.00 CEST.
This event will give you in-depth information about:
Expert speakers will share their knowledge and insights about how:
• Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
• Promoting resilience and health restoration can reduce the risk of severe COVID-19 or development of Long COVID.
• These interventions can improve the recovery from Long COVID.
Key speakers and topics:
Therapeutic strategies of complementary medicines in the COVID 19 pandemic and Long COVID in addition to conventional medicine
Dr Joanna Dietzel, MD Neurologist, Acupuncturist. Department for integrative & complementary medicine, Institute of social medicine, epidemiology and health economics, Charité – Universitätsmedizin Berlin, Germany.
Chinese herbal medicine treatment in cases of infections with SARS-CoV-2 – therapeutic strategies for COVID-19 and Long COVID
Dr Christian Thede, MD, General practitioner, specialised in Acupuncture and Chinese Medicine. Former lecturer in Chinese medicine, University of Witten-Herdecke, Germany
Instructor for Acupuncture and Chinese Medicine at International Society of Chinese Medicine (SMS).
Traditional and Complementary Medicine contributions to health system resilience during COVID-19 – the WHO perspective
Dr Geetha Kopalakrishna, MD, Bachelor of Ayurvedic Medicine & Surgery
Technical Officer at Traditional, Complementary & Integrative Medicine, Department of Service Delivery and Safety, World Health Organization, Geneva, Switzerland
Key member of the AYUSH-based COVID-19 response Task Force for the Government of India.
Research programme into integrative medicine’s contribution to improving resilience to COVID-19 infection and reducing the risk of severe COVID-19 or development of Long COVID
Dr Helene M. Langevin, Director at National Center for Complementary and Integrative Health, National Institutes of Health, Bethesda, Maryland (MD), USA. Previously, Director of the Harvard Osher Center for Integrative Medicine and professor of medicine at Harvard Medical School, Boston (MA) and professor of neurological sciences at the Larner College of Medicine at the University of Vermont (VT).
Q&A sessions after the presentations.
Resilience to infections: a solution for COVID-19 and other infectious illnesses
Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19. Nearly two-thirds of COVID-19 hospitalizations could be attributed to obesity, diabetes, hypertension, and heart failure. There is increasing awareness that a health system that focuses on improving health could prevent all these conditions to a large extent.
Long COVID
More than 40% of people who have or had COVID-19 get long COVID, and among people who needed hospitalization, the statistics go up to 57%. The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
MEP Interest Group on Integrative Medicine and Health
The event is hosted by the members of the MEP Interest Group on Integrative Medicine & Health:
Michèle Rivasi, Greens/EFA, France
Sirpa Pietikäinen, EPP, Finland
Tilly Metz, Greens/EFA, Luxembourg
Margrete Auken, Greens/EFA, Denmark
Romana Jerković, S&D, Croatia
Manuela Ripa, Greens/EFA, Germany
I had not been aware of the ‘MEP Interest Group on Integrative Medicine & Health‘. Therefore, I looked it up and found this:
The newly established Interest Group on Integrative Medicine & Health continues the work of the former MEP Interest Group on CAM. This group brings together MEPs who work collectively to promote the inclusion of CAM as part of Integrative Medicine & Health in all possible European Parliament public health policy.
Why an Interest Group in the European Parliament?
One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care. This high demand is not yet reflected in EU or national health policy or provision. In addition, there is diversity in complementary medicine regulation across the EU. There are differences in who can practice complementary medicine, what qualifications are required and how services are offered and financed. These discrepancies mean that citizens experience practical and attitudinal barriers that limit their access to and use of TCIM.
The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges. These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine. Integrative Medicine and Health focuses on the whole person and considers the individual in its physical, psychological, spiritual, social and environmental context. It is inclusive of all professions and practices that use this approach and meets the demand of EU citizens for a more holistic, patient-centered approach in medicine. At the same time, TCIM is at the center of political and scientific debate. In this context, a forum for discussion on Integrative and Complementary Medicine’s contribution to EU health systems will bring clarity and rationality to this debate.
Aims and objectives of the Interest Group on Integrative Medicine & Health
- Establish and maintain a forum for discussion and action with all stakeholders regarding Integrative Medicine and Health.
- Raise awareness of Integrative Medicine and its contribution to more sustainable healthcare systems in the EU and a more holistic approach to health.
- Focus on the integration of complementary modalities into the health systems of the EU Member States.
- Protect and promote citizens’ right to choose their own healthcare while providing access to Integrative Medicine and Health information.
- Advocate for EU involvement in setting unified standards to regulation of Integrative Medicine and Health.
__________________________________
Unified standards? But what about high or perhaps just scientific standards? What about first doing the research and then making claims about CAM or TCIM or however you decide to call it? Has common sense gone out of fashion?
Yes, you guessed it: I am seriously underwhelmed by all this. To show you why, let me list just a few claims from the above two statements that are based purely on wishful thinking:
- Complementary and Integrative Medicine and Health interventions can improve resilience to COVID-19 infection.
- These interventions can improve the recovery from Long COVID.
- Studies show that certain common medical conditions put people at higher risk for severe illness and death from COVID-19.
- The recovery from such post viral syndromes will be greatly helped by offering patients access to complementary and integrative medicine interventions that aim at restoring their health balance.
- One in two EU citizens uses complementary medicine either alongside or as an alternative to conventional biomedical care.
- The health sector in the EU Member States is facing considerable challenges, such as antimicrobial resistance (AMR), increasing prevalence of Non-Communicable Diseases (NCDs) and soaring costs. Complementary medicine can offer a significant contribution to meet these challenges.
- These modalities are “integrative”, offering patient-centered healthcare, based on evidence-informed integration of conventional biomedicine and complementary medicine.
- Integrative medicine … meets the demand of EU citizens for a more holistic, patient-centered approach in medicine.
I find all this confusing and concerning in equal measure. I also seriously doubt that the forum for discussion on Integrative and Complementary Medicine will bring clarity and rationality to this debate. If they really wanted a debate, they would need to include a few critical thinkers; can anyone recognize one on the list of speakers? I cannot!
I fear the aim of the group and their meeting is to mislead us all into thinking that CAM, TCIM, etc. generate more good than harm without ever delivering the evidence for that assumption. Therefore, I suggest they rename both the conference as well as their group:
‘Wishful thinking in prevention and management of COVID-19 and long COVID’
and
MEP Interest Group on Wishful Thinking and Promotion of Quackery
PS
As an antidote to wishful thinking, I recommend reading some proper science papers on the subject. Here are the conclusions of an up-to-date and wishful-thinking-free review on the subject of post-acute infection syndrome:
Unexplained post-acute infection syndromes (PAISs) appear to be an under-recognized feature of a spectrum of infectious diseases in a minority of patients. At present, our understanding of the underlying pathophysiologic mechanisms and etiologic factors is poor and there are no known objective markers or effective therapeutic options. More basic biomedical research is needed. The overlap of symptoms, signs, and general features of the individual PAISs suggests the involvement of shared pathological pathways and the possibility that common diagnostic markers, or even a unified etiological model, might be established.
However, some symptoms or clinical characteristics seem to be trigger-specific or more prevalent in one PAIS than in others, emphasizing the need for cohorts with a well-documented infectious trigger. The overall clinical picture of many PAISs often overlaps with the presentation of post-infectious ME/CFS or fibromyalgia, or resembles other fatiguing, neurological, or rheumatic disorders. Exploiting existing knowledge of these conditions might help guide future scientific discovery and progress in clinical care.
The SARS-CoV-2 pandemic uncovered a significant gap in knowledge about post-acute sequelae of infectious diseases and identified the need for better diagnostic care and clinical infrastructure for patients experiencing these long-term effects. In addition to basic biomedical research, more needs to be done to refine diagnostic criteria and obtain more reliable estimates of the prevalence and societal burden of these disorders to help shape health-policy decisions. Moreover, we call for unified nomenclature and better conceptualization of post-acute infection symptoms.
There is much to be done, but the unprecedented amount of attention and resources that have recently been allocated to the study of COVID-19-related pathology brings a promise of much-needed progress in the wider field of unexplained infection-associated chronic disability.
Ayush-64 is an Ayurvedic formulation, developed by the Central Council for Research in Ayurvedic Sciences (CCRAS), the apex body for research in Ayurveda under the Ministry of Ayush. Originally developed in 1980 for the management of Malaria, this drug has now been repurposed for COVID-19 as its ingredients showed notable antiviral, immune-modulator, and antipyretic properties. Its ingredients are:
| Alstonia scholaris R. Br. Aqueous extract of (Saptaparna) | Bark-1 part |
| Picrorhiza Kurroa Royle Aqueous extract of (Kutki) | Rhizome-1 part |
| Swertia chirata Buch-Ham. Aqueous extract of (Chirata) | Whole plant-1 part |
| Caesalphinia crista, Linn. Fine powder of seed (Kuberaksha) | Pulp-2 parts |
The crucial question, of course, is does AYUSH-64 work?
An open-label randomized controlled parallel-group trial was conducted at a designated COVID care centre in India with 80 patients diagnosed with mild to moderate COVID-19 and randomized into two groups. Participants in the AYUSH-64 add-on group (AG) received AYUSH-64 two tablets (500 mg each) three times a day for 30 days along with standard conventional care. The control group (CG) received standard care alone.
The outcome measures were:
- the proportion of participants who attained clinical recovery on days 7, 15, 23, and 30,
- the proportion of participants with negative RT-PCR assay for COVID-19 at each weekly time point,
- change in pro-inflammatory markers,
- metabolic functions,
- HRCT chest (CO-RADS category),
- the incidence of Adverse Drug Reaction (ADR)/Adverse Event (AE).
Out of 80 participants, 74 (37 in each group) contributed to the final analysis. A significant difference was observed in clinical recovery in the AG (p < 0.001 ) compared to CG. The mean duration for clinical recovery in AG (5.8 ± 2.67 days) was significantly less compared to CG (10.0 ± 4.06 days). Significant improvement in HRCT chest was observed in AG (p = 0.031) unlike in CG (p = 0.210). No ADR/SAE was observed or reported in AG.
The authors concluded that AYUSH-64 as adjunct to standard care is safe and effective in hastening clinical recovery in mild to moderate COVID-19. The efficacy may be further validated by larger multi-center double-blind trials.
I do object to these conclusions for several reasons:
- The study cannot possibly determine the safety of AYUSH-64.
- Even for assessing its efficacy, it was too small.
- The trial design followed the often-discussed A+B vs B concept and is thus prone to generate false-positive results.
I believe that it is highly irresponsible, during a medical crisis like ours, to conduct studies that can only produce unreliable findings. If there is a real possibility that a therapy might work, we do need to test it, but we should take great care that the test is rigorous enough to generate reliable results. This, I think, is all the more true, if – like in the present case – the study was done with governmental support.
This meta-analysis was conducted by researchers affiliated to the Evangelical Clinics Essen-Mitte, Department of Internal and Integrative Medicine, Faculty of Medicine, University of Duisburg-Essen, Germany. (one of its authors is an early member of my ALTERNATIVE MEDICINE HALL OF FAME). The paper assessed the safety of acupuncture in oncological patients.
The PubMed, Cochrane Central Register of Controlled Trials, and Scopus databases were searched from their inception to August 7, 2020. Randomized controlled trials in oncological patients comparing invasive acupuncture with sham acupuncture, treatment as usual (TAU), or any other active control were eligible. Two reviewers independently extracted data on study characteristics and adverse events (AEs). Risk of bias was assessed using the Cochrane Risk of Bias Tool.
Of 4590 screened articles, 65 were included in the analyses. The authors observed that acupuncture was not associated with an increased risk of intervention-related AEs, nonserious AEs, serious AEs, or dropout because of AEs compared with sham acupuncture and active control. Compared with TAU, acupuncture was not associated with an increased risk of intervention-related AEs, serious AEs, or dropout because of AEs but was associated with an increased risk for nonserious AEs (odds ratio, 3.94; 95% confidence interval, 1.16-13.35; P = .03). However, the increased risk of nonserious AEs compared with TAU was not robust against selection bias. The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.
The authors concluded that the current review indicates that acupuncture is as safe as sham acupuncture and active controls in oncological patients. The authors recommend researchers heed the CONSORT (Consolidated Standards of Reporting Trials) safety and harm extension for reporting to capture the side effects and better investigate the risk profile of acupuncture in oncology.
You might think this article is not too bad. So, why do I feel that this paper is so bad?
One reason is that the authors included evidence up to August 2020. Since then, there must have been hundreds of further papers on acupuncture. The article was therefore out of date before it was published.
But that is by no means my main reason. We know from numerous investigations that acupuncture studies often fail to report AEs (and thus violate publication ethics). This means that this new analysis is merely an amplification of the under-reporting. It is, in other words, a means of perpetuating a wrong message.
Yes, you might say, but the authors acknowledge this; they even state in the abstract that “The meta-analyses may have been biased because of the insufficient reporting of AEs in the original randomized controlled trials.” True, but this fact does not erase the mistake, it merely concedes it. At the very minimum, the authors should have phrased their conclusion differently, e.g.: the current review confirms that AEs of acupuncture are under-reported in RCTs. Therefore, a meta-analysis of RCTs is unable to verify whether acupuncture is safe. From other types of research, we know that it can cause serious AEs.
An even better solution would have been to abandon or modify the research project when they first came across the mountain of evidence showing that RCTs often fail to mention AEs.
As it stands, the conclusion that acupuncture is as safe as sham acupuncture is simply not true. Since the article probably looks sound to naive readers, I feel that is a particularly good candidate for the WORST PAPER OF 2022 COMPETITION.
PS
For those who are interested, here are 4 of my own peer-reviewed articles on the safety of acupuncture (much more can, of course, be found on this blog):
- Patient safety incidents from acupuncture treatments: a review of reports to the National Patient Safety Agency – PubMed (nih.gov)
- Acupuncture–a critical analysis – PubMed (nih.gov)
- Prospective studies of the safety of acupuncture: a systematic review – PubMed (nih.gov)
- The risks of acupuncture – PubMed (nih.gov)
Anyone who has followed this blog for a while will know that advocates of so-called alternative medicine (SCAM) are either in complete denial about the risks of SCAM or they do anything to trivialize them. Here is a dialogue between a SCAM proponent (P) and a scientist (S) that is aimed at depicting this situation. The conversation is fictitious, of course, but it is nevertheless based on years of experience in discussing these issues with practitioners of various types of SCAM. As we shall see, the arguments turn out to be perfectly circular.
P: My therapy is virtually free of risks.
S: How can you be so sure?
P: I am practicing it for decades and have never seen a single problem.
S: That could have several reasons; perhaps the patients who experience problems did simply not come back.
P: I find this unlikely.
S: I don’t, and I know of reports where patients had serious complications after the type of SCAM you practice.
P: These are isolated case reports. They do not amount to evidence.
S: How do you know they are isolated?
P: They must be isolated because, in the many clinical trials of my therapy available to date, you will not find any evidence of serious adverse effects.
S: That is true, but it has been repeatedly shown that these trials regularly fail to mention side effects altogether.
P: That’s because there aren’t any.
S: Not quite, clinical trials should always mention adverse effects, and if there were none, they should mention this too.
P: So, you admit that you have no evidence that my therapy causes adverse effects.
S: The thing is, I don’t need such evidence. It is you, the practitioners of this therapy, who should provide evidence that your treatments are safe.
P: We did! The complete absence of reports of side effects constitutes that evidence.
S: Except, there is some evidence. I already told you that there are several case reports of serious problems.
P: But case reports are anecdotes; they are no evidence.
S: Look, here is a systematic review of all the case reports. You cannot possibly deny that this is a concern.
P: It’s still merely a bunch of anecdotes, nothing more.
S: Only because your profession does nothing about it.
P: What do you think we need to do about it?
S: Like other professions, you need to systematically record adverse effects.
P: How would that help?
S: It would give us a rough indication of the size and severity of the problem.
P: This sounds expensive and complicated to organize.
S: Perhaps, but it is necessary if you want to be sure that your therapy is safe.
P: But we are sure already!
S: No, you believe it, but you don’t know it.
P: You are getting on my nerves with your obsession. Don’t you know that the true danger in healthcare is the adverse effects of pharmaceutical drugs?
S: But these drugs are also effective.
P: Are you saying my therapy isn’t?
S: What I am saying is that the drugs you claim to be dangerous do more good than harm, while this is not at all clear with your SCAM.
P: To me, that is very clear. My therapy helps many and harms nobody!
S: How do you know that it harms nobody?
… At this point, we have gone full circle and we can re-start this conversation from its beginning.
I was alerted to the following short article from ‘The Blackpool Gazette‘:
Criminals have been using the brand name Pfizer to sell fake homeopathic vaccines to residents, according to police. The white tablets are sold under the pretence that they are an alternative to traditional vaccines, but actually contain no active ingredient. Analysis conducted by Lancashire Police revealed the tablets were nothing more than sugar pills. “Please note Pfizer do not produce any tablets as a cure or prophylactic for COVID-19,” a spokesman for the force added.
Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can help the body heal itself, according to the NHS. A 2010 House of Commons Science and Technology Committee report on homeopathy said that homeopathic remedies perform no better than placebos. In 2017, NHS England said it would no longer fund homeopathy on the NHS as the lack of any evidence for its effectiveness did not justify the cost. This was backed by a High Court judgement in 2018.
I think there might be a slight misunderstanding here. The homeopathic remedy might not be fake, as it was produced according to the concepts of homeopathy. It is homeopathy itself that is fake. To me, it looks as though we are dealing with the German product I mentioned a while ago. Let me remind you:
Many people believe that homeopathy is essentially plant-based – but they are mistaken! Homeopathic remedies can be made from anything: Berlin wall, X-ray, pus, excrement, dental plaque, mobile phone rays, poisons … anything you can possibly think of. So, why not from vaccines?
This is exactly what a pharmacist specialized in homeopathy thought.
It has been reported that the ‘Schloss-Apotheke’ in Koblenz, Germany offered for sale a homeopathic remedy made from the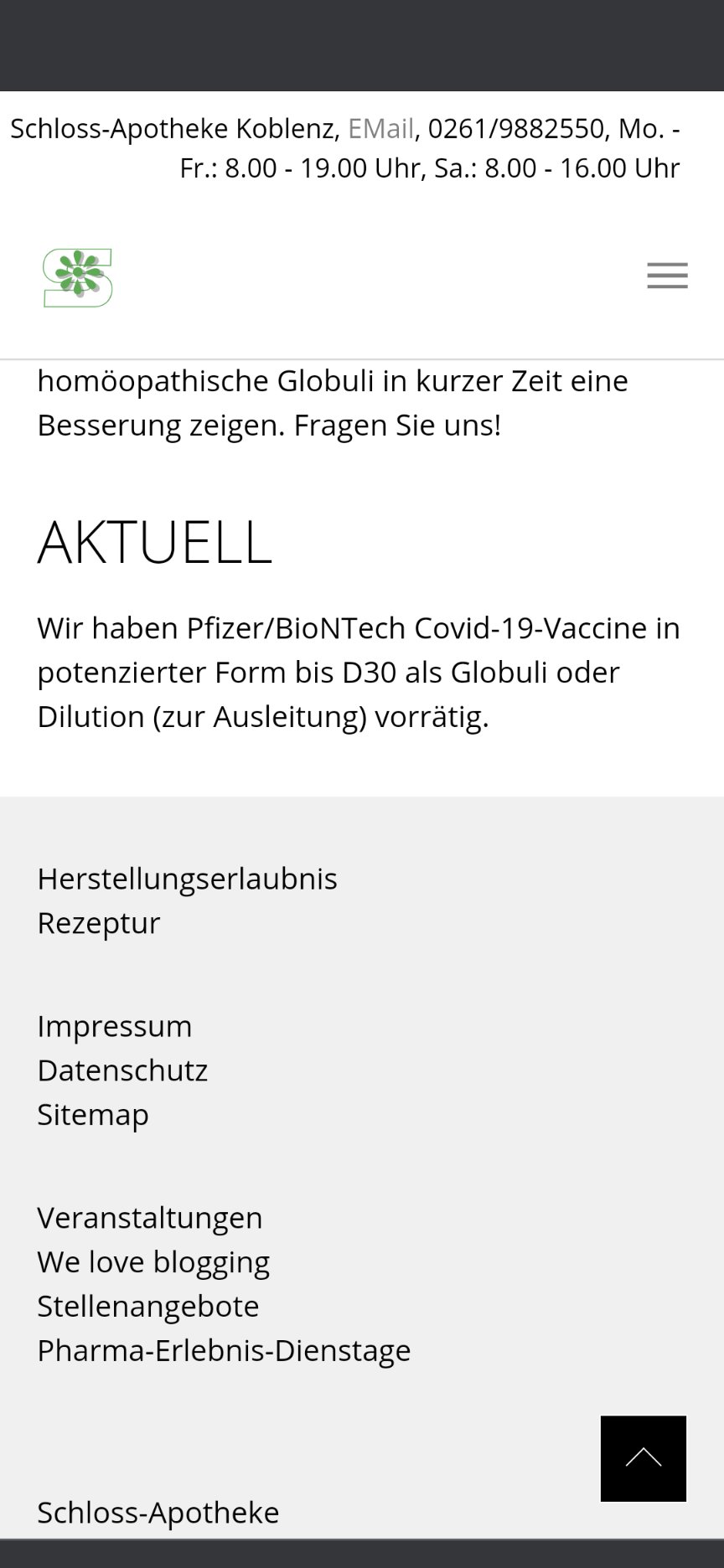 Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
Pfizer vaccine. This has since prompted not only the Chamber of Pharmacists but also the Paul Ehrlich Institute and Pfizer to issue statements. On Friday (30/4/2021) morning, the pharmacy had advertised homeopathic remedies based on the Pfizer/Biontech vaccine. The Westphalia-Lippe Chamber of Pharmacists then issued an explicit warning against it. “We are stunned by this,” said a spokesman. The offer has since disappeared from the pharmacy’s website.
On Friday afternoon, the manufacturer of the original vaccine also intervened. The Paul Ehrlich Institute released a statement making it clear that a vaccine is only safe “if it is administered in accordance with the marketing authorization.”
The Schloss-Apotheke had advertised the product in question with the following words:
“We have Pfizer/BioNTech Covid-19-Vaccine in potentized form up to D30 as globules or dilution (for discharge) in stock.”
The chamber of pharmacists countered with a warming under the heading “Facts instead of Fake News” on Facebook and Instagram:
“Whatever they might contain: These remedies are no effective protection against Covid-19.”
Pharmacy manager, Annette Eichele, of the Schloss-Apotheke claimed she had not sold homeopathic Corona vaccines and stressed that effective vaccines of this kind do not exist. According to Eichele, only an additional “mini drop” of the original Biontech vaccine had been used and “highly potentized” and prepared homeopathically. According to Eichele, Corona vaccinations that had already been administered were thus to have a “better and more correct effect with this supplementary product, possibly without causing side effects … but this is not scientifically proven”. The homeopathic product had been produced only on customer request and had been sold less than a dozen times in the past weeks. Ten grams of the remedy were sold for about 15 Euros. On Twitter, Eichele stated: „Wir haben nichts Böses getan, wir wollten nur Menschen helfen!“ (We have done nothing evil, we only wanted to help people). I am reminded yet again of Bert Brecht who observed:
“The opposite of good is not evil but good intentions”.
_______________________
If I am right, the remedy is not truly fake but a genuine product of a fake concept, namely homeopathy. In that case, the term ‘criminal’ might need to be applied to homeopathy itself – an interesting thought!
The cardiothoracic surgeon and famous US woo merchant, Dr. Mehmet Oz, is probably known to most readers. I have previously mentioned him several times, for instance, here and here. His institution, Columbia University in New York City, has had many (I’d say too many) years of patience with his relentless promotion of outright and often dangerous quackery. Now it has been reported that the university has finally cut ties with Dr. Oz:
“It took Columbia far too long to remove Oz from its otherwise distinguished medical faculty,” Henry Miller, MD, of the Pacific Research Institute in California, told MedPage Today via email. Miller stressed that “the ‘Oz controversy’ was never about free speech. It was about an unethical grifter whose claims and pronouncements were not supported by science and were injurious to consumers — in the interest of financial benefit to Oz himself. That constitutes professional misconduct.”
The university’s Irving Medical Center quietly ended its relationship with Oz at the end of April, according to The Daily Beast. He had been removed from several pages of the medical center’s website in mid-January. In 2018, Oz’s title had been changed to professor emeritus and special lecturer, according to reports. A spokesperson for Columbia University confirmed the 2018 change in an email to MedPage Today.
In 2015, Miller and colleagues sent a letter to Lee Goldman, MD, MPH, dean of the Faculties of Health Sciences and Medicine at the university, calling for Oz’s expulsion. Oz had “repeatedly shown disdain for science and for evidence-based medicine” and “manifested an egregious lack of integrity by promoting quack treatments and cures in the interest of personal financial gain,” according to Miller’s group…
In 2014, Oz was called to testify before the Senate Subcommittee on Consumer Protection, Product Safety, and Insurance during a hearing on false advertising in the diet and weight-loss industry. Senators grilled Oz regarding statements he made on “The Dr. Oz Show” that promoted green coffee bean extract as a “miracle pill” for weight loss.
But long before that hearing, tensions had built between Oz and the medical community because of his penchant for spouting dubious medical claims on his TV show and in the media. For example, in a 2011 segment, ABC News‘ chief health and medical editor Richard Besser, MD, called out a purported “study” of arsenic in apple juice that Oz conducted for an episode of his show.
Besser charged that Oz’s science was shoddy because he reported total arsenic rather than the breakdown between organic and inorganic arsenic — only the latter of which is known to be toxic. Even the FDA sent the show a letter before the segment aired saying it would be “irresponsible and misleading” to report the results.
Oz again broke with medical science during the pandemic when he touted hydroxychloroquine as a cure for COVID-19, even as evidence mounted that it had no effect on disease course.
Oz is currently running for a U.S. Senate seat in Pennsylvania as a Republican candidate. Former President Trump endorsed Oz, touting Oz’s medical and academic credentials in a statement, according to NPR: “He even said that I was in extraordinary health, which made me like him even more (although he also said I should lose a couple of pounds!).”
__________________________
I have to admit that I find these reports somewhat puzzling. Don’t get me wrong: it’s not that I don’t think Oz deserves to be dismissed. In fact, he had already richly deserved it many years ago. What I find, however, odd is that giving someone the title ’emeritus professor’ can hardly be called ‘cutting ties’ with him. In some ways, it is even the opposite (I should know because I currently have this status).
When I looked up Oz, Columbia listed him as:
Oz, Mehmet C. (MD)
Special Lecturer in the Department of Surgery
Phone: 212.305.4434 · Fax: 212.342.3520
Location: MHB, Rm. 435-62
Similarly, the website of the Irving Medical Center is full of entries about Oz. Confusion is therefore more than justified, I think.
What is needed, I feel, is a clear statement from Columbia University about its relationship with Dr. Oz. Are they still proud of his considerable fame/notoriety, or did they in fact have the integrity to cut ties with one of the most self-aggrandizing woo merchants of all times?
Harad Matthes, the boss of the anthroposophical Krankenhaus Havelhoehe and professor for Integrative and Anthroposophical Medicine at the Charite in Berlin, has featured on my blog before (see here and here). Now he is making headlines again.
‘Die Zeit‘ reported that Matthes went on German TV to claim that the rate of severe adverse effects of COVID-19 vaccinations is about 40 times higher than the official figures indicate. In the MDR broadcast ‘Umschau’ Matthes said that his unpublished data show a rate of 0,8% of severe adverse effects. In an interview, he later confirmed this notion. Yet, the official figures in Germany indicate that the rate is 0,02%.
How can this be?
Die ZEIT ONLINE did some research and found that Matthes’ data are based on extremely shoddy science and mistakes. The Carite also distanced themselves from Matthes’ evaluation: “The investigation is an open survey and not really a scientific study. The data are not suitable for drawing definitive conclusions regarding incidence figures in the population that can be generalized” The problems with Matthes’ ‘study’ seem to be sevenfold:
- The data are not published and can thus not be scrutinized.
- Matthes’ definition of a severe adverse effect is not in keeping with the generally accepted definition.
- Matthes did not verify the adverse effects but relied on the information volunteered by people over the Internet.
- Matthes’ survey is based on an online questionnaire accessible to anyone. Thus it is wide open to selection bias.
- The sample size of the survey is around 10 000 which is far too small for generalizable conclusions.
- There is no control group which makes it impossible to differentiate a meaningful signal from mere background noise.
- The data contradict those from numerous other studies that were considerably more rigorous.
Despite these obvious flaws Matthes insisted in a conversation with ZEIT ONLINE that the German official incidence figures are incorrect. As Germany already has its fair share of anti-vaxxers, Matthes’ unfounded and irresponsible claims contribute significantly to the public sentiments against COVID vaccinations. They thus endangering public health.
In my view, such behavior amounts to serious professional misconduct. I, therefore, feel that his professional body, the Aerztekammer, should look into it and prevent further harm.
Acupuncture for animals has a long history in China. In the West, it was introduced in the 1970s when acupuncture became popular for humans. A recent article sums up our current knowledge on the subject. Here is an excerpt:
Acupuncture is used mainly for functional problems such as those involving noninfectious inflammation, paralysis, or pain. For small animals, acupuncture has been used for treating arthritis, hip dysplasia, lick granuloma, feline asthma, diarrhea, and certain reproductive problems. For larger animals, acupuncture has been used for treating downer cow syndrome, facial nerve paralysis, allergic dermatitis, respiratory problems, nonsurgical colic, and certain reproductive disorders.Acupuncture has also been used on competitive animals. There are veterinarians who use acupuncture along with herbs to treat muscle injuries in dogs and cats. Veterinarians charge around $85 for each acupuncture session.[8]Veterinary acupuncture has also recently been used on more exotic animals, such as chimpanzees (Pan troglodytes)[9] and an alligator with scoliosis,[10] though this is still quite rare.
To put it in a nutshell: acupuncture for animals is not evidence-based.
How can I be so sure?
Because ref 1 in the text above refers to our paper. Here is its abstract:
Acupuncture is a popular complementary treatment option in human medicine. Increasingly, owners also seek acupuncture for their animals. The aim of the systematic review reported here was to summarize and assess the clinical evidence for or against the effectiveness of acupuncture in veterinary medicine. Systematic searches were conducted on Medline, Embase, Amed, Cinahl, Japana Centra Revuo Medicina and Chikusan Bunken Kensaku. Hand-searches included conference proceedings, bibliographies, and contact with experts and veterinary acupuncture associations. There were no restrictions regarding the language of publication. All controlled clinical trials testing acupuncture in any condition of domestic animals were included. Studies using laboratory animals were excluded. Titles and abstracts of identified articles were read, and hard copies were obtained. Inclusion and exclusion of studies, data extraction, and validation were performed independently by two reviewers. Methodologic quality was evaluated by means of the Jadad score. Fourteen randomized controlled trials and 17 nonrandomized controlled trials met our criteria and were, therefore, included. The methodologic quality of these trials was variable but, on average, was low. For cutaneous pain and diarrhea, encouraging evidence exists that warrants further investigation in rigorous trials. Single studies reported some positive intergroup differences for spinal cord injury, Cushing’s syndrome, lung function, hepatitis, and rumen acidosis. These trials require independent replication. On the basis of the findings of this systematic review, there is no compelling evidence to recommend or reject acupuncture for any condition in domestic animals. Some encouraging data do exist that warrant further investigation in independent rigorous trials.
This evidence is in sharp contrast to the misinformation published by the ‘IVAS’ (International Veterinary Acupuncture Society). Under the heading “For Which Conditions is Acupuncture Indicated?“, they propagate the following myth:
Acupuncture is indicated for functional problems such as those that involve paralysis, noninfectious inflammation (such as allergies), and pain. For small animals, the following are some of the general conditions which may be treated with acupuncture:
- Musculoskeletal problems, such as arthritis, intervertebral disk disease, or traumatic nerve injury
- Respiratory problems, such as feline asthma
- Skin problems such as lick granulomas and allergic dermatitis
- Gastrointestinal problems such as diarrhea
- Selected reproductive problems
For large animals, acupuncture is again commonly used for functional problems. Some of the general conditions where it might be applied are the following:
- Musculoskeletal problems such as sore backs or downer cow syndrome
- Neurological problems such as facial paralysis
- Skin problems such as allergic dermatitis
- Respiratory problems such as heaves and “bleeders”
- Gastrointestinal problems such as nonsurgical colic
- Selected reproductive problems
In addition, regular acupuncture treatment can treat minor sports injuries as they occur and help to keep muscles and tendons resistant to injury. World-class professional and amateur athletes often use acupuncture as a routine part of their training. If your animals are involved in any athletic endeavor, such as racing, jumping, or showing, acupuncture can help them keep in top physical condition.
And what is the conclusion?
Perhaps this?
Never trust the promotional rubbish produced by SCAM organizations.
For quite some time now, I have had the impression that the top journals of general medicine show less and less interest in so-called alternative medicine. So, I decided to do some Medline searches to check. Specifically, I searched for 4 different SCAMs:
- homeopathy
- acupuncture
- chiropractic
- herbal medicine
I wanted to see how often 7 leading medical journals from the US, UK, Australia, Germany, and Austria carried articles indexed under these headings:
- JAMA – US
- NEJM – US
- BMJ – UK
- Lancet – UK
- Aust J Med – Australia
- Dtsch Med Wochenschrift – Germany
- Wien Med Wochenschrift – Austria
This is what I found (the 1st number is the total number of articles ever listed; the 2nd number is the maximum number in any year; the 3rd number in brackets is the year when that maximum occurred)
JAMA
Homeopathy: 17, 3 (1998)
Acupuncture: 176, 21 (2017)
Chiropractic: 49, 4 (1998)
Herbal medicine: 43, 5 (2001)
NEJM
Homeopathy: 6, 3 (1986)
Acupuncture: 49, 8 (1974)
Chiropractic: 43, 13 (1980)
Herbal medicine: 29, 12 (1999)
BMJ
Homeopathy: 122, (10, 1995)
Acupuncture: 405, 31 (2021)
Chiropractic: 99, 11 (2021)
Herbal medicine: 158, 13 (2018)
Lancet
Homeopathy: 75, 11 (2005)
Acupuncture: 93, 12 (1973)
Chiropractic: 20, 5 (1993)
Herbal medicine: 46, 6 (1993)
Aust J Med
Homeopathy: 9, 2 (2010)
Acupuncture: 78, 13 (1974)
Chiropractic: 34, 4 (1985)
Herbal medicine: 20, 2 (2017)
Deutsche Medizinische Wochenschrift
Homeopathy: 27, 4 (1999)
Acupuncture: 34, 6 (1978)
Chiropractic: 14, 3 (1972)
Herbal medicine: 6, 1 (2020)
Wiener Medizinische Wochenschrift
Homeopathy: 11, 4 (2005)
Acupuncture: 32, 8 (1998)
Chiropractic: 8, 2 (1956)
Herbal medicine: 16, 3 (2002)
These figures need, of course, to be taken with a rather large pinch of salt. There are many pitfalls in interpreting them, e.g. misclassifications by Medline. Yet they are, I think, revealing in that they suggest several interesting trends.
- All in all, my suspicion that the top journals of various countries are less and less keen on SCAM seems to be confirmed. The years where the maximum of papers on specific SCAMs was published are often long in the past.
- The UK journals seem to be by far more open to SCAM that the publications from other countries. This is mostly due to the BMJ – in fact, it turns out to be the online journal ‘BMJ-open’. And this again is to a great part caused by the BMJ-open carrying a sizable amount of acupuncture papers in recent months.
- The two US journals seem particularly cautious about SCAM papers. When looking at the type of articles in the US journals (and especially the NEJM), one realizes that most of them are ‘letters to the editor’ which seems to confirm the dislike of these journals for publishing original research into SCAM. Another interpretation of this phenomenon, of course, would be that only very few SCAM studies are of a high enough quality to make it into these two top journals.
- I was amazed to see how little SCAM was published in the two German-language journals. Vis a vis the high popularity of SCAM in these countries, I find this not easy to understand. Perhaps, one also needs to consider that these two journals publish considerably less original research than the other publications
- If we look at the differences between the 4 types of SCAM included in my assessment, we find that acupuncture is by far the most frequently published modality. The other 3 are on roughly the same level, with chiropractic being the least frequent – which I thought was surprising.
- Overall, the findings do not generate the impression that – despite the many billions spent on SCAM research during the last decades – SCAM has made important inroads into science or medicine.
I have often commented on the dismal state of the many SCAM journals; these days, they seem to publish almost exclusively poor-quality papers with misleading conclusions. It can therefore be expected that these journals will be more and more discarded by everyone (except the few SCAM advocates who publish their rubbish in them) as some sort of cult publications. In turn, this means that only SCAM studies published in mainstream journals will have the potential of generating any impact at all.
For this reason, my little survey might be relevant. It is far from conclusive, of course, yet it might provide a rough picture of what is happening in the area of SCAM research.
There is a lack of data describing the state of naturopathic or complementary veterinary medicine in Germany. This survey maps the currently used treatment modalities, indications, existing qualifications, and information pathways. It records the advantages and disadvantages of these medicines as experienced by veterinarians. Demographic influences are investigated to describe the distributional impacts of using veterinary naturopathy and complementary medicine.
A standardized questionnaire was used for the cross-sectional survey. It was distributed throughout Germany in a written and digital format from September 2016 to January 2018. Because of the open nature of data collection, the return rate of questionnaires could not be calculated. To establish a feasible timeframe, active data collection stopped when the previously calculated limit of 1061 questionnaires was reached.
With the included incoming questionnaires of that day, a total of 1087 questionnaires were collected. Completely blank questionnaires and those where participants did not meet the inclusion criteria were not included, leaving 870 out of 1087 questionnaires to be evaluated. A literature review and the first test run of the questionnaire identified the following treatment modalities:
- homeopathy,
- phytotherapy,
- traditional Chinese medicine (TCM),
- biophysical treatments,
- manual treatments,
- Bach Flower Remedies,
- neural therapy,
- homotoxicology,
- organotherapy,
- hirudotherapy.
These were included in the questionnaire. Categorical items were processed using descriptive statistics in absolute and relative numbers based on the population of completed answers provided for each item. Multiple choices were possible.
Overall 85.4% of all the questionnaire participants used naturopathy and complementary medicine. The treatments most commonly used were:
- complex homoeopathy (70.4%, n = 478),
- phytotherapy (60.2%, n = 409),
- classic homoeopathy (44.3%, n = 301),
- biophysical treatments (40.1%, n = 272).
The most common indications were:
- orthopedic (n = 1798),
- geriatric (n = 1428),
- metabolic diseases (n = 1124).
Over the last five years, owner demand for naturopathy and complementary treatments was rated as growing by 57.9% of respondents (n = 457 of total 789). Veterinarians most commonly used scientific journals and publications as sources for information about naturopathic and complementary contents (60.8%, n = 479 of total 788). These were followed by advanced training acknowledged by the ATF (Academy for Veterinary Continuing Education, an organisation that certifies independent veterinary continuing education in Germany) (48.6%, n = 383). The current information about naturopathy and complementary medicine was rated as adequate or nearly adequate by many (39.5%, n = 308) of the respondents.
The most commonly named advantages in using veterinary naturopathy and complementary medicine were:
- expansion of treatment modalities (73.5%, n = 566 of total 770),
- customer satisfaction (70.8%, n = 545),
- lower side effects (63.2%, n = 487).
The ambiguity and unclear evidence of the mode of action and effectiveness (62.1%, n = 483) and high expectations of owners (50.5%, n = 393) were the disadvantages mentioned most frequently. Classic homoeopathy, in particular, has been named in this context (78.4%, n = 333 of total 425). Age, gender, and type of employment showed a statistically significant impact on the use of naturopathy and complementary medicine by veterinarians (p < 0.001). The university of final graduation showed a weaker but still statistically significant impact (p = 0.027). Users of veterinary naturopathy and complementary medicine tended to be older, female, self-employed and a higher percentage of them completed their studies at the University of Berlin. The working environment (rural or urban space) showed no statistical impact on the veterinary naturopathy or complementary medicine profession.
The authors concluded that this is the first study to provide German data on the actual use of naturopathy and complementary medicine in small animal science. Despite a potential bias due to voluntary participation, it shows a large number of applications for various indications. Homoeopathy was mentioned most frequently as the treatment option with the most potential disadvantages. However, it is also the most frequently used treatment option in this study. The presented study, despite its restrictions, supports the need for a discussion about evidence, official regulations, and the need for acknowledged qualifications because of the widespread application of veterinary naturopathy and complementary medicine. More data regarding the effectiveness and the mode of action is needed to enable veterinarians to provide evidence-based advice to pet owners.
I can only hope that the findings are seriously biased and not a true reflection of the real situation. The methodology used for recruiting participants (it is fair to assume that those vets who had no interest in SCAM did not bother to respond) strongly indicates that this might be the case. If, however, the findings were true, one would have to conclude that, for German vets, evidence-based healthcare is still an alien concept. The evidence that the preferred SCAMs are effective for the listed conditions is very weak or even negative. If the findings were true, one would need to wonder how much of veterinary SCAM use amounts to animal abuse.
