progress
Yes, I have just published a new book! Its title is ‘Alternativmedizin – was hilft, was schadet: Die 20 besten, die 20 bedenklichsten Methoden’ (Alternative medicine – treatments that help and treatments that harm: The 20 best and the 20 most worrying methods). Yes, it is in German, and somehow I doubt that there will be an English version of it. Therefore I take the liberty of translating a short section for those who do not read German. 
But first, let me tell you about the book’s concept.
Some people who read this blog seem to have the impression that I am dead against so-called alternative medicine (SCAM) – my friend Dana Ullman, for instance, is convinced of it. This, however, is not quite correct (Dana rarely is). The truth is that I am
- FOR evidence-based medicine,
- FOR a level playing field in all areas of healthcare,
- FOR critically evaluating all options.
This also means, of course, that I am against misleading consumers about the value of SCAM. And therefore I am FOR any SCAM that demonstrably does more good than harm.
This attitude should have been clear from all my books. However, it seems to be difficult to understand for those who are on the more fanatical end of the SCAM spectrum. And because it is not that obvious, I decided to write a book that analyses (understandably yet analytically [including ~300 references of the original science]) the evidence for 20 SCAMs that are supported by reasonably sound evidence together with 20 for which this is not the case. My hope is that, with this approach, I might reach more consumers who are in favour of SCAM.
There is a risk, of course. Chances are that, instead of reaching more people from the pro-camp, I will merely offend both the sceptics as well as the enthusiasts.
We shall see.
Anyway, here is the promised bit that I translated for you. It is the postscript of the book, and I hope it gives you a flavour of what it is all about. Here we go:
In the first chapter of the book, I promised that I would neither uncritically hype alternative medicine nor unfairly condemn it. I have taken great pains to keep this promise.
Have I succeeded?
I fear there will be many who answer this question in the negative. And I can’t even blame my critics! Who likes to be criticized for something in which he deeply believes? Who likes to hear that his prejudices against everything called alternative medicine are wrong and counter-productive? Who doesn’t mind an ugly fact that destroys his beautiful theory? Both the dogmatic naysayers and the naive believers will be dissatisfied with my book (or at least parts of).
That’s a shame, but ultimately it is irrelevant. My point was not to take the word of one camp or another in the endless trench warfare that is alternative medicine. My main concern was to present the evidence as up-to-date, understandable, and objective as possible, and to serve those who are seriously interested in facts.
The book is thus not for dogged trench warriors; rather, it is aimed at ordinary consumers with an interest in their health. After all, the vast majority of the population is not among the unteachables of one camp or the other. Most people don’t want ideology, they want effective medicine. And most of them are baffled by the unmanageable variety of alternative medicine on offer, the grandiose promises of healing, and the vehement emotions that it all triggers.
In the area of alternative medicine, there is undoubtedly a lot of nonsense, charlatanry, and danger. But there are also some things that demonstrably do more good than harm. In order to separate the wheat from the chaff, consumers don’t need creeds. What they need above all is reliable evidence!
You can read about this evidence in my book. How you then deal with it is solely your decision. I do not want to tell anyone what to do with my presentation of the facts. But I know that the abundance of misinformation in the field of alternative medicine causes great damage and that the consumer and reader of my book, deserve better than to be led up the garden path.
If this book helps readers to make wise treatment decisions, my efforts will have been worthwhile. And if they get half as much pleasure from reading it as I did from writing it, my goal has been achieved.
THE END
(If by any chance you do read German and are in the position to publish a book review, please let me know and I will see that you get a free review copy of my book)
Unintended consequences are outcomes of a purposeful action that are not intended or foreseen. They exist almost everywhere and often have effects that are the opposite of what was intended.
Just look at our current misery, the pandemic, for instance. Practically all epidemiologists advocated stricter and earlier preventative measures than the ‘anti-lockdown’ brigade in politics and elsewhere wanted and implemented. Had we listened to the epidemiologists, we would almost certainly have had fewer lockdowns and less economic downturn. The unintended consequences of the political decisions to be slow and less than strict with lockdowns are what we can currently observe in many countries:
- repeated, longer, and less and less effective lockdowns,
- huge economic damage,
- more deaths,
- more long-term illness;
- financial hardship for many,
- more psychological problems and frustration.
But I am not here to moan about politicians not listening enough to scientists. I want to vent my anger and concern about much of the research that is currently being published in the realm of so-called alternative medicine (SCAM).
What is happening here – slightly simplified and exaggerated to make my point – is (as often discussed previously) roughly this:
- more and more enthusiasts of SCAM feel that they should conduct and publish some research;
- they are largely ignorant of or willfully ignore the accepted standards of science;
- they have little interest in cause and effect or critical thinking;
- they aim to promote and not to test SCAM;
- several SCAM journals have realized that there is good money to be earned from publishing utter rubbish;
- more and more papers are being published that are flawed to the point of being meaningless;
- the few relevant SCAM papers with sound science get drowned out and become all but invisible;
- outsiders glancing at the literature get the impression that SCAM is swamped with rubbish and thus an area that is best avoided;
- consequently, SCAM research is fast losing all credibility and is becoming the laughing stock of proper scientists;
- eventually, the notion that ‘ALL SCAM IS RUBBISH’ must filter through into public life;
- in the end, the pseudo-researchers of SCAM will have provided the nail in SCAM’s coffin.
The INTENDED consequence was to promote SCAM.
The UNINTENDED consequence will be to destroy SCAM.
This self-destructive course of SCAM might be applauded by some skeptics. However, if you believe (as I do) that there are a few good things to be found in SCAM, this development can only be regrettable.
What can be done to avert such a negative outcome?
I wish I knew!
But four productive steps might be the following:
- make sure researchers are adequately trained and supervised to do sound science;
- motivate funding agencies to stop supporting pseudo-science;
- ensure that journal editors and reviewers realize they have the responsibility to avoid publishing nonsense
- motivate Medline to de-list a few of the worst SCAM journals.
“Today, scientists note that the glycyrrhizic acid contained in this plant prevents the development of a new coronavirus, which the whole world is fighting against. Moreover, even a small concentration of an aqueous extract of licorice root has a neutralizing effect.”

These are the words of President Gurbanguly Berdymukhamedov of Turkmenistan. The plant he referred to is licorice. With is the promotion of a herbal solution for the pandemic, he is in good company:
- Thailand’s health ministry approved the use of Andrographis Paniculata, commonly known as green chiretta, to treat patients who are in the early stages of a Covid-19 infection.
- The health authorities of Tamil Nadu distributed herbal medicine to the general public as a preventive measure against Coronavirus disease.
- Madagascar claims to have a cure for Covid-19, the herbal tea named Covid-Organics has the plant artemisia as an ingredient.
- China has been using TCM alongside conventional treatment methods to treat Covid-19 patients. Some of the herbal formulations used in the treatment are:
- Jinhua Qinggan Granule
- Sheganmahuang decoction
- Lianhuaqingwen capsule
- Maxingshigan decoction
- Xuebijing Injection
- Indonesia is testing two herbal medicines: Cordyceps militaris, a fungus common in the Himalayas, and a herbal formulation comprising Ginger, gripeweed, Ngai camphor, and Andrographis paniculata.
And what about some evidence? In 2020, Medline listed 302 articles on herbal medicine for COVID-19. Here I selected just 10 of them to give you a flavor:
COVID-19 is the most recently discovered coronavirus infectious disease and leads to pandemic all over the world. The clinical continuum of COVID-19 varies from mild illness with non-specific signs and symptoms of acute respiratory disease to extreme respiratory pneumonia and septic shock. It can transmit from animal to human in the form of touch, through the air, water, utensils, fomite and feco-oral route blood. The pathogenesis and clinical features of COVID-19 be the same as the clinical manifestation associated epidemic Fever. In Unani medicine, various herbal drugs are described under the caption of epidemic disease. Great Unani scholar also Avicenna (980-1037 AD) recommended that during epidemic condition movement should be restricted, self-isolation, fumigation around the habitant with perfumed herbs (Ood, Kafoor, Sumbuluttib, Saad Kofi, Loban, etc.), and use of appropriate antidotes (Tiryaqe Wabai) and vinegar (Sirka) as prophylaxis. Herbal approach is based on single (Unnab-Ziziphus jujuba, Sapistan-Cordia myxa, Bahidana-Cydonia oblonga, Khatmi-Althea officinalis, Khubazi-Malva sylvestris, Zafran-Crocus sativus, Sibr-Aloe barbedensis, Murmuki-Commiphora myrrha, Darchini-Cinnamomum zeylanicum, Qaranfal-Syzygium aromaticum, Rihan-Oscimum sanctum, Habtus Sauda-Nigella sativa, Aslus Sus-Glycyrrhiza glabra, Maghze Amaltas-Cassia fistula and Adusa-Adhatoda vasica) and compound drugs (Habbe Bukhar, Sharbat Khaksi, Sharbat Zanjabeel, Naqu Nazla, Majoon Chobchini, Jawrish Jalinus and Khamira Marvareed) most of them are claimed for anti-viral, anti-pyretic, blood purifier, cardioprotective and expectorant activities. Traditionally most of the herbal practitioners are using it.
According to the World Health Organization (WHO), viral diseases continue to rise, and pose a significant public health problem. Novel coronavirus disease (COVID-19) is an infectious disease caused by SARS-CoV-2. The pathogenesis and clinical manifestations of COVID-19 is close to Amraz-e-Wabai (epidemic diseases) which was described by Hippocrates, Galen, Aristotle, Razes, Haly Abbas, Avicenna, Jurjani etc. Presently, there is no specific or challenging treatment available for COVID-19. Renowned Unani Scholars recommended during epidemic situation to stay at home, and fumigate the shelters with aromatics herbs like Ood kham (Aquilaria agallocha Roxb.), Kundur (Boswellia serrata Roxb), Kafoor (Cinnamomum camphora L.), Sandal (Santalum album L), Hing (Ferula foetida L.) etc. Use of specific Unani formulations are claimed effective for the management of such epidemic or pandemic situation like antidotes (Tiryaqe Wabai, Tiryaqe Arba, Tiryaqe Azam, Gile Armani), Herbal Decoction (Joshandah), along with Sharbate Khaksi, Habbe Bukhar, Sharbate Zanjabeel, Khamira Marwareed, Jawarish Jalinus, and Sirka (vinegar). Such drugs are claimed for use as antioxidant, immunomodulatory, cardiotonic, and general tonic actions. The study enumerates the literature regarding management of epidemics in Unani medicine and attempts to look the same in the perspective of COVID-19 prevention and management.
Unani system of medicine is based on the humoral theory postulated by Hippocrates, according to him the state of body health and disease are regulated by qualitative and quantitative equilibrium of four humours. Amraz-e-Waba is an umbrella term which is used in Unani medicine for all types of epidemics (smallpox, measles, plague, Hameer Saifi, influenza, Nipaha, Ebola, Zika, and 2019 novel coronavirus, etc.) mostly fatal in nature. The coronavirus disease 2019 (COVID-19) is a severe acute respiratory infection, and the pathogenesis and clinical features resemble with those of Nazla-e-Wabaiya (influenza) and Zatul Riya (pneumonia) which were well described many years ago in Unani text such as high-grade fever, headache, nausea and vomiting, running nose, dry cough, respiratory distress, alternate and small pulse, asthenia, foul smell from breath, insomnia, frothy stool, syncope, coldness in both upper and lower extremities, etc. The World Health Organization declared COVID-19 as a global emergency pandemic. Unani scholars like Hippocrates (370-460 BC), Galen (130-200 AD), Rhazes (865-925 AD), and Avicenna (980-1037 AD) had described four etiological factors for Amraz-e-Waba viz., change in quality of air, water, Earth, and celestial bodies, accordingly mentioned various preventive measures to be adopted during epidemics such as restriction of movement, isolation or “quarantena”, and fumigation with loban (Styrax benzoin W. G. Craib ex Hartwich.), sandalwood (Santalum album L.), Zafran (Crocus sativus L.), myrtle (Myrtus communis L.), and roses (Rosa damascena Mill.) and use of vinegar (sirka) and antidotes (Tiryaq) as prophylaxis, and avoiding consumption of milk, oil, sweet, meat, and alcohol. This review focuses and elaborates on the concept, prevention, and probable management of COVID-19 in the light of Amraz-e-Waba.
Background: Current recommendations for the self-management of SARS-Cov-2 disease (COVID-19) include self-isolation, rest, hydration, and the use of NSAID in case of high fever only. It is expected that many patients will add other symptomatic/adjuvant treatments, such as herbal medicines.
Aims: To provide a benefits/risks assessment of selected herbal medicines traditionally indicated for “respiratory diseases” within the current frame of the COVID-19 pandemic as an adjuvant treatment.
Method: The plant selection was primarily based on species listed by the WHO and EMA, but some other herbal remedies were considered due to their widespread use in respiratory conditions. Preclinical and clinical data on their efficacy and safety were collected from authoritative sources. The target population were adults with early and mild flu symptoms without underlying conditions. These were evaluated according to a modified PrOACT-URL method with paracetamol, ibuprofen, and codeine as reference drugs. The benefits/risks balance of the treatments was classified as positive, promising, negative, and unknown.
Results: A total of 39 herbal medicines were identified as very likely to appeal to the COVID-19 patient. According to our method, the benefits/risks assessment of the herbal medicines was found to be positive in 5 cases (Althaea officinalis, Commiphora molmol, Glycyrrhiza glabra, Hedera helix, and Sambucus nigra), promising in 12 cases (Allium sativum, Andrographis paniculata, Echinacea angustifolia, Echinacea purpurea, Eucalyptus globulus essential oil, Justicia pectoralis, Magnolia officinalis, Mikania glomerata, Pelargonium sidoides, Pimpinella anisum, Salix sp, Zingiber officinale), and unknown for the rest. On the same grounds, only ibuprofen resulted promising, but we could not find compelling evidence to endorse the use of paracetamol and/or codeine.
Conclusions: Our work suggests that several herbal medicines have safety margins superior to those of reference drugs and enough levels of evidence to start a clinical discussion about their potential use as adjuvants in the treatment of early/mild common flu in otherwise healthy adults within the context of COVID-19. While these herbal medicines will not cure or prevent the flu, they may both improve general patient well-being and offer them an opportunity to personalize the therapeutic approaches.
Recently, the novel life-threatening coronavirus infection (COVID-19) was reported at the end of 2019 in Wuhan, China, and spread throughout the world in little time. The effective antiviral activities of natural products have been proved in different studies. In this review, regarding the effective herbal treatments on other coronavirus infections, promising natural products for COVID-19 treatment are suggested. An extensive search in Google Scholar, Science Direct, PubMed, ISI, and Scopus was done with search words include coronavirus, COVID-19, SARS, MERS, natural product, herb, plant, and extract. The consumption of herbal medicine such as Allium sativum, Camellia sinensis, Zingiber officinale, Nigella sativa, Echinacea spp. Hypericum perforatum, and Glycyrrhiza glabra, Scutellaria baicalensis can improve the immune response. It seems that different types of terpenoids have promising effects in viral replication inhibition and could be introduced for future studies. Additionally, some alkaloid structures such as homoharringtonine, lycorine, and emetine have strong anti-coronavirus effects. Natural products can inhibit different coronavirus targets such as S protein (emodin, baicalin) and viral enzymes replication such as 3CLpro (Iguesterin), PLpro (Cryptotanshinone), helicase (Silvestrol), and RdRp (Sotetsuflavone). Based on previous studies, natural products can be introduced as preventive and therapeutic agents in the fight against coronavirus.
Background: The aim of the present review is to provide basic knowledge about the treatment of Coronavirus via medicinal plants. Coronavirus (COVID-19, SARS-CoV, and MERS-CoV) as a viral pneumonia causative agent, infects thousands of people in China and worldwide. There is currently no specific medicine or vaccine available and it is considered a threat to develop effective novel drug or anti-coronavirus vaccine treatment. However, natural compounds to treat coronaviruses are the most alternative and complementary therapies due to their diverse range of biological and therapeutic properties.
Methods: We performed an open-ended, English restricted search of Scopus database, Web of Science, and Pubmed for all available literature from Jan-March, 2020, using terms related to phytochemical compounds, medicinal plants and coronavirus.
Results: The view on anti-coronavirus (anti-CoV) activity in the plant derived phytochemicals and medicinal plants give the strong base to develop a novel treatment of corona virus activity. Various phytochemicals and medicinal plant extracts have been revised and considered to be the potential anti-CoV agents for effective control and future drug development. We discuss some important plants (Scutellaria baicalensis, Psorothamnus arborescens, Glycyrrhiza radix, Glycyrrhiza uralensis , Lycoris radiate, Phyllanthus emblica, Camellia sinensis, Hyptis atrorubens Poit, Fraxinus sieboldiana, Erigeron breviscapus, Citri Reticulatae Pericarpium, Amaranthus tricolor, Phaseolus vulgaris, Rheum palmatum, Curcuma longa and Myrica cerifera) emerged to have broad spectrum antiviral activity.
Conclusion: Nigella sativa has potent anti-SARS-CoV activity and it might be useful souce for developing novel antiviral therapies for coronaviruses.
COVID-19 has been declared a pandemic by WHO on March 11, 2020. No specific treatment and vaccine with documented safety and efficacy for the disease have been established. Hence it is of utmost importance to identify more therapeutics such as Chinese medicine formulae to meet the urgent need. Qing Fei Pai Du Tang (QFPDT), a Chinese medicine formula consisting of 21 herbs from five classical formulae has been reported to be efficacious on COVID-19 in 10 provinces in mainland China. QFPDT could prevent the progression from mild cases and shorten the average duration of symptoms and hospital stay. It has been recommended in the 6th and 7th versions of Clinical Practice Guideline on COVID-19 in China. The basic scientific studies, supported by network pharmacology, on the possible therapeutic targets of QFPDT and its constituent herbs including Ephedra sinica, Bupleurum chinense, Pogostemon cablin, Cinnamomum cassia, Scutellaria baicalensis were reviewed. The anti-oxidation, immuno-modulation and antiviral mechanisms through different pathways were collated. Two clusters of actions identified were cytokine storm prevention and angiotensin converting enzyme 2 (ACE2) receptor binding regulation. The multi-target mechanisms of QFPDT for treating viral infection in general and COVID-19 in particular were validated. While large scale clinical studies on QFPDT are being conducted in China, one should use real world data for exploration of integrative treatment with inclusion of pharmacokinetic, pharmacodynamic and herb-drug interaction studies.
In December 2019, a novel coronavirus SARS-CoV-2, causing the disease COVID-19, spread from Wuhan throughout China and has infected people over 200 countries. Thus far, more than 3,400,000 cases and 240,000 deaths have occurred worldwide, and the coronavirus pandemic continues to grip the globe. While numbers of cases in China have been steadying, the number of infections outside China is increasing at a worrying pace. We face an urgent need to control the spread of the COVID-19 epidemic, which is currently expanding to a global pandemic. Efforts have focused on testing antiviral drugs and vaccines, but there is currently no treatment specifically approved. Traditional Chinese medicine (TCM) is grounded in empirical observations and the Chinese people use TCM to overcome these sorts of plagues many times in thousands of years of history. Currently, the Chinese National Health Commission recommended a TCM prescription of Qing-Fei-Pai-Du-Tang (QFPDT) in the latest version of the “Diagnosis and Treatment guidelines of COVID-19” which has been reported to provide reliable effects for COVID-19. While doubts about TCM still exist today, this review paper will describe the rationalities that QFPDT is likely to bring a safe and effective treatment of COVID-19.
The fight against the novel coronavirus pneumonia (namely COVID-19) that seriously harms human health is a common task for all mankind. Currently, development of drugs against the novel coronavirus (namely SARS-CoV-2) is quite urgent. Chinese medical workers and scientific researchers have found some drugs to play potential therapeutic effects on COVID-19 at the cellular level or in preliminary clinical trials. However, more fundamental studies and large sample clinical trials need to be done to ensure the efficacy and safety of these drugs. The adoption of these drugs without further testing must be careful. The relevant articles, news, and government reports published on the official and Preprint websites, PubMed and China National Knowledge Infrastructure (CNKI) databases from December 2019 to April 2020 were searched and manually filtered. The general pharmacological characteristics, indications, adverse reactions, general usage, and especially current status of the treatment of COVID-19 of those potentially effective drugs, including chemical drugs, traditional Chinese medicines (TCMs), and biological products in China were summarized in this review to guide reasonable medication and the development of specific drugs for the treatment of COVID-19.
Objective: To analysis the medication characteristics of the prescriptions issued via open channel by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine in treating coronavirus disease 2019 (COVID-19).
Methods: We collected the data of traditional Chinese medicine related to treatment plans published by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine from the start of COVID-19 outbreak to February 19, 2020. The frequency analysis, cluster analysis and association analysis were performed.
Results: The study collected 4 national and 34 regional prevention and treatment plans, 578 items, 84 traditional Chinese formulations, 60 Chinese patent medicines, and 230 Chinese herbs. The high frequently used herbs were Liquorice, Scutellariabaicalensis, Semen armeniacaeamarae, and Gypsum. The commonly used traditional formulations included Maxing Shigan decoction, Yin Qiao powder, and Xuanbai Chengqi decoction. The Chinese patent drugs included Angong Niuhuang pill, Xuebijing injection, and Lianhua Qingwen capsule. The most common paired medications were Ephedra and Semen armeniacaeamarae, Fructusforsythiae and Liquorice. Two core combinations and one novel formula were discovered in the study.
Conclusions: Yin Qiao powder and Huopo Xialing decoction are the basic formulations for Weifen syndrome of COVID-19. In addition, Maxing Shigan decoction, Liang Ge powder, Qingwen Baidu decoction and Da Yuan decoction are the basic formulations for Qifen syndrome of COVID-19. The main medication characteristics are clearing heat, entilating lung, removing toxicity and removing turbidity. It shows that removing toxicity and eliminating evil are the prescription thought in treating epidemic disease of traditional Chinese medicine.
Confused?
Me too!
What seems to emerge is this:
- ‘Herbalists and Co’ did not wait long to jump on the corona bandwagon.
- They managed to confuse not just you and me, but even politicians, presidents, and their advisers.
- They produced a plethora of articles implying that an endless array of herbs might be effective.
- In doing so, no clear consensus emerged as to which herbs are the most promising.
- Sound evidence seems to be not available.
- Clinical trials are slow to start or not even planned.
- Everything is based on more or less wild extrapolation.
- Much of what is being published is borderline irresponsible.
- YET, IT MUST BE GOOD FOR BUSINESS!
THE TELEGRAPH is not my favourite paper, but occasionally it does publish something worth reading – like, for instance, yesterday when it carried this article:
The head of NHS England warned homeopaths had “crossed the line” after a Sunday Telegraph investigation revealed some were peddling myths that taking duck extract was as effective as the coronavirus vaccines.
Sir Simon Stephens warned people taking their advice from homeopaths were putting themselves at greater risk, and warned they would slow down the nation’s vaccine efforts. His calls were echoed by Professor Stephen Powis, the NHS medical director, who said the findings were the “latest in a long line of disturbing and potentially dangerous online myths”…
Sir Simon told the Sunday Telegraph: “It’s one thing for homeopaths to peddle useless but harmless potions, but they cross a dangerous line when making ridiculous assertions about protecting people from Covid infection. “Anyone who took those seriously would be putting themselves at higher risk of coming to harm from Covid infection.” Prof Powis added: “Spouting claims on social media about Covid cures that are not backed by scientific evidence and accurate public health advice is the latest in a long line of disturbing and potentially dangerous online myths. We urge everyone to ignore misleading claims and get vital protection against Covid when they are invited for their vaccine.” …
Helen Earner, operations director at the Charity Commission, said the findings were being examined as “a matter of urgency”. She added: “Any claims that a charity may be providing misinformation during this time of national emergency is a matter of serious concern to the Commission.” She added that a regulatory compliance case had been opened into the matter and that the commission will be liaising with other agencies as part of the investigation…
These days, I read such articles with mixed feelings. On the one hand, I applaud the fact that UK officials do take note of dangerous quackery and promise to take action. On the other hand, I cannot help feeling a bit frustrated and ask myself: WHY HAS IT TAKEN THEM SO LONG?
I know, for instance, that the Charity Commission has long been dragging its feet to do something about charities that promote overtly dangerous quackery. I have discussed such charities three years ago, and others have done so even before me. As to the UK homeopaths’ (and other practitioners of so-called alternative medicine, SCAM) dangerously bizarre attitude towards vaccinations, I started providing evidence and warning the public as early as 1995.
Perhaps they did not know about it?
Yes, perhaps – I only published these warnings in the
BRITISH JOURNAL OF GENERAL PRACTICE
and in the
This gets even more frustrating when I consider that the anti-vaccination attitude in SCAM is merely one facet of a much bigger and much more important subject. Starting also in 1995, I published dozens of papers, gave hundreds of lectures on it, and often called it the ‘indirect risks‘ of SCAM. They can be summarised in one single sentence:
EVEN IF A SCAM IS TOTALLY HARMLESS, THE SCAM PRACTITIONER OFTEN ISN’T.
It is therefore tempting to shout:
I TOLD YOU SO!
But that would hardly be helpful. Instead, I let me beg Sir Simon Stephens, Prof Powis, Helen Earner, and anyone else in a position of power to take a minute and consider the wider implications of tolerating SCAM practitioners impose their overtly dangerous health-related views on the unsuspecting public.
On 10/1/2021 THE GUARDIAN reported about some bizarre anthroposophic treatments in Germany. About a month before, we had discussed the issue here on this blog. The GUARDIAN article prompted the following press release, dated 12/1/2021, by the ‘International Federation of Anthroposophic Medical Associations’ (oddly abbreviated IVAA):
IVAA welcomes the reporting by The Observer, a sister paper of The Guardian, on the care of Covid-19 patients in German anthroposophic hospitals, including critically ill patients in the intensive care ward. The article rightly highlights how these treatments are provided in addition to state-of-the-art conventional treatments, how anthroposophic medicine is fully integrated into the German health care system and how anthroposophy “enjoys a high level of social acceptance and institutional support in German-speaking countries”. The World Health Organization’s Traditional Medicine Strategy has indeed set integration of traditional and complementary medicine into health care systems as one of its strategic goals.
While the article is generally biased against anthroposophic medicine and only quotes two known opponents of anthroposophy, it nevertheless provides welcome reporting on integrative medicine that is highly popular with patients in Europe.
There are many peer-reviewed studies on anthroposophic medicine and anthroposophic medications have been in use for decades, showing an excellent safety profile. The Observer’s critique that patients should provide consent for such treatments does not hold because the treatments are not experimental, are provided in addition to standard care, based on long clinical experience and in hospitals openly publicizing their integrative medicine approach. As the article reports, German insurance companies pay flat-rate payments for hospital treatment of coronavirus patients; the additional anthroposophic treatments are thus financed out of hospital budgets and are cost-neutral for insurance companies.
Unfortunately, and as correctly reported by The Observer, individual supporters of anthroposophic medicine have sided with demonstrations against corona measures; this does in no way reflect the official position of anthroposophic medicine and IVAA member organizations have clearly distanced themselves.
END OF PRESS RELEASE
One does not need to be a champion in critical thinking to realize that this press release deserves a few comments.
- The claim that anthroposophic medicine (AM) is ‘fully integrated into the German healthcare system‘ is misleading. In Germany, AM belongs to the special therapeutic measures (‘besondere Therapierichtungen’) which indicates almost the opposite of ‘fully integrated’.
- Similarly, AM is not ‘highly accepted’ but belongs to the fringe of so-called alternative medicine (SCAM). There are only very few anthroposophic hospitals in Germany, and most Germans would not even know what AM is.
- The press release claims that ‘there are many peer-reviewed studies on anthroposophic medicine‘. The link it provides leads to an AM organization’s list of references. For infections, this list references the following 9 papers: (1) Martin DD. Fever: Views in Anthroposophic Medicine and their Scientific Validity. Evid Based Complement Alternat Med. 2016;2016(1):13 pages.(2) Soldner G, Stellman HM. Individual Paediatrics: Physical, Emotional and Spiritual Aspects of Diagnosis and Counseling – Anthroposophic-homeopathic Therapy, Fourth edition. 4 edition. CRC Press; 2014. 984 S. (3) Glöckler M, Goebel W. A Guide to Child Health: A Holistic Approach to Raising Healthy Children. Floris Books; 2013. (4) Goebel MW, Michael MK, Glöckler MM. Kindersprechstunde: ein medizinisch-pädagogischer Ratgeber. Verlag Urachhaus; 2016. (5) Szoeke H, Marodi M, Sallay Z, Székely B, Sterner M-G, Hegyi G. Integrative versus Conventional Therapy of Chronic Otitis Media with Effusion and Adenoid Hypertrophy in Children: A Prospective Observational Study. Forsch KomplementärmedizinResearch Complement Med. 2016;23(4):231–239. (6) Hamre HJ, Glockmann A, Schwarz R, Riley DS, Baars EW, Kiene H, u. a. Antibiotic use in children with acute respiratory or ear infections: prospective observational comparison of anthroposophic and conventional treatment under routine primary care conditions. Evid Based Complement Alternat Med. 2014;2014(Article ID 243801). (7) Hamre HJ, Fischer M, Heger M, Riley D, Haidvogl M, Baars E, u. a. Anthroposophic vs. conventional therapy of acute respiratory and ear infections. Wien Klin Wochenschr. 2005;117(7–8):256–268. (8) Hamre HJ, Glockmann A, Fischer M, Riley DS, Baars E, Kiene H. Use and Safety of Anthroposophic Medications for Acute Respiratory and Ear Infections: A Prospective Cohort Study. Drug Target Insights. 14. September 2007;2:209–19. (9) Jeschke E, Lüke C, Ostermann T, Tabali M, Huebner J, Matthes H. Verordnungsverhalten anthroposophisch orientierter Ärzte bei akuten Infektionen der oberen Atemwege. Forsch KomplementärmedizinResearch Complement Med. 2007;14(4):207–215. These are mostly NOT peer-reviewed papers, and none yields anything close to conclusive findings about the alleged efficacy of AM treatments. The truth is that there is no good evidence to support AM.
- The mention that AM remedies have been used for decades is a fallacy (appeal to tradition).
- Yes, AM remedies are safe – mainly because they, like homeopathic remedies, usually contain no active ingredients.
- Patients should provide consent for such treatments to ALL treatments, experimental or not.
- Clinicians practicing AM have long been known to hold an anti-vax attitude which has also caused problems in the past.
My conclusion: this press release was written in true anthroposophic style and spirit: ill-informed, in disregard of medical ethics, based on wishful thinking and aimed at misleading the public.
Trump and his lamentable influence on so-called alternative medicine (SCAM) have been the subject of several of my posts (see for instance here, here, and here). Now they are a thing of the past, and one may well ask how Biden and his new administration might influence the SCAM boom in the US and the rest of the world.
Joe Biden has chosen former Food and Drug Administration (FDA) commissioner, Dr. David Kessler, to lead Operation Warp Speed — the U.S. government’s program for accelerating the Covid-19 vaccine and treatments rollout. The Alliance for Natural Health seemed to think that was bad news:
Dr. David Kessler, an anti-supplement crusader, drug industry adviser, and former FDA Commissioner, has been named to Biden’s COVID-19 task force. We must push back. Action Alert!
… During that time, Kessler demonstrated his hostility towards the dietary supplement industry. The last thing we need is someone who is diametrically opposed to natural medicine in a position of power, particularly concerning how our country deals with a virus against which natural medicines like zinc, potassium, and vitamin D have demonstrated efficacy.
The record on Dr. Kessler is clear. In 1993, he took aim at the supplement industry by trying to limit the health claims supplements could make under the Nutrition Labeling and Education Act of 1990. This law gave the FDA the authority to approve disease-prevention claims for food, including supplements (for example, “adequate calcium throughout life may reduce the risk of osteoporosis”)—but Dr. Kessler said the FDA would not approve any of the proposed claims for supplements. He stood before Congress that same year and compared the supplement industry to “snake oil salesmen.”…
Dr. Kessler also serves as board chair for the Center for Science in the Public Interest’s (CSPI) Board of Directors. It is a fitting post for Dr. Kessler, as CSPI shares his negative views on dietary supplements. In particular, CSPI worked to eliminate legal structure/function claims for dietary supplements. (A structure/function claim describes the role of a nutrient on the structure or function of the body, such as “calcium builds strong bones,” or “antioxidants maintain cell integrity.”)
There is also speculation that Dr. Kessler is being considered for a more prominent role in government, such as heading up the Health and Human Services Department.
Dr. Kessler’s appointment to the COVID-19 task force is therefore particularly concerning. We are already dealing with federal agencies trying to gag doctors to prevent them from disseminating basic information about the benefits of supplements for COVID-19—supplements that were part of President Trump’s own treatment regimen. There is clear evidence to suggest many natural medicines to help prevent and treat COVID…
To me, this shows foremost that the ‘Alliance for Natural Health’ is an irresponsible lobby group for SCAM that does not hesitate to put public health at risk in order to boost the already enormous profits of the SCAM industry. If these lobbyists are unhappy, it should be good news.
Right now, Joe Biden has certainly other things on his mind than SCAM. But the appointment of Kessler is one of several indications that he intends to take much more of a pro-science, pro-public health course than his predecessor. The fact that the ‘Alliance for Natural Health’ is up in arms might be a sign that he is not likely to take SCAM fools lightly.
Personally, I am relieved that Trump is gone and I wish the new administration and the American people only the very best.
The state of acupuncture research has long puzzled me. The first thing that would strike who looks at it is its phenomenal increase:
- Until around the year 2000, Medline listed about 200 papers per year on the subject.
- From 2005, there was a steep, near-linear increase.
- It peaked in 2020 when we had a record-breaking 20515 acupuncture papers currently listed in Medline.
Which this amount of research, one would expect to get somewhere. In particular, one would hope to slowly know whether acupuncture works and, if so, for which conditions. But this is not the case.
On the contrary, the acupuncture literature is a complete mess in which it gets more and more difficult to differentiate the reliable from the unreliable, the useful from the redundant, and the truth from the lies. Because of this profound confusion, acupuncture fans are able to claim that their pet-therapy is demonstrably effective for a wide range of conditions, while skeptics insist it is a theatrical placebo. The consumer might listen in bewilderment.
Yesterday (18/1/2021), I had a quick (actually, it was not that quick after all) look into what Medline currently lists in terms of new acupuncture research published in 2021 and found a few other things that are remarkable:
- There were already 100 papers dated 2021 (today, there were even 118); that corresponds to about 5 new articles per day and makes acupuncture one of the most research-active areas of so-called alternative medicine (SCAM).
- Of these 100 papers, only 7 were clinical trials (CTs). In my view, clinical trials would be more important than any other type of research on acupuncture. To see that they amount to just 7% of the total is therefore disappointing.
- Twelve papers were systematic reviews (SRs). It is odd, I find, to see almost twice the amount of SRs than CTs.
- Eighteen papers referred to protocols of studies of SRs. In particular protocols of SRs are useless in my view. It seems to me that the explanation for this plethora of published protocols might be the fact that Chinese researchers are extremely keen to get papers into Western journals; it is an essential boost to their careers.
- Seven papers were surveys. This multitude of survey research is typical for all types of SCAM.
- Twenty-four articles were on basic research. I find basic research into an ancient therapy of questionable clinical use more than a bit strange.
- The rest of the articles were other types of publications and a few were misclassified.
- The vast majority (n = 81) of the 100 papers were authored exclusively by Chinese researchers (and a few Korean). In view of the fact that it has been shown repeatedly that practically all acupuncture studies from China report positive results and that data fabrication seems rife in China, this dominance of China could be concerning indeed.
Yes, I find all this quite concerning. I feel that we are swamped with plenty of pseudo-research on acupuncture that is of doubtful (in many cases very doubtful) reliability. Eventually, this will create an overall picture for the public that is misleading to the extreme (to check the validity of the original research is a monster task and way beyond what even an interested layperson can do).
And what might be the solution? I am not sure I have one. But for starters, I think, that journal editors should get a lot more discerning when it comes to article submissions from (Chinese) acupuncture researchers. My advice to them and everyone else:
if it sounds too good to be true, it probably is!
So-called alternative medicine (SCAM) is, as we all know, an umbrella term. Under this umbrella, we find hundreds of different modalities that have little in common with each other. Here I often focus on:
- homeopathy,
- chiropractic,
- acupuncture,
- herbal medicine.
There are uncounted others, and in my recent book, I published critical evaluations 150 of them. But for the moment, let’s keep to the 4 SCAMs listed above.
What strikes me regularly is that many SCAM enthusiasts do seem to appreciate my critical assessments of SCAM; for instance:
- When I point out that the assumptions of homeopathy fly in the face of science, most SCAM enthusiasts agree.
- When I point out that chiropractic spinal manipulations might not be safe, most SCAM enthusiasts agree.
- When I point out that acupuncture is not a panacea, most SCAM enthusiasts agree.
- When I point out that herbal remedies can interact with prescribed drugs, most SCAM enthusiasts agree.
Most but not all!
- Those who find my criticism of homeopathy unfair are the homeopaths and their proponents.
- Those who find my criticism of chiropractic unfair are the chiropractors and their proponents.
- Those who find my criticism of acupuncture unfair are the acupuncturists and their proponents.
- Those who find my criticism of herbal medicine unfair are the herbalists and their proponents.
Hardly ever does a herbalist defend homeopathy’s weird assumptions; rarely does an acupuncturist tell me that I am too harsh with the chiropractors; never have I heard a chiropractor complain that my criticism of acupuncture is unjustified.
Entirely obvious?
Perhaps!
But I find it nevertheless curious, because my critical stance is always the same. I do not change it for this or that form of SCAM (I would also not change it for conventional medicine, but I leave it to those who have more specific expertise to do the criticising). I have no axe to grind against any particular SCAM. All I do is point out flaws in their logic, limitations in their studies, gaps in the evidence. All I do is provide my honest interpretation of the evidence.
It really seems to me that everyone appreciates my honesty, until I start being honest with them.
And this is why I find it curious. Homeopaths, chiropractors, acupuncturists, herbalists and all the other types of SCAM practitioners like to be seen on the side of science, evidence, critical thinking and progress. This, I suppose, is good for the (self) image; it might even help the delusion that they are all evidence-based. But as soon as someone applies science, evidence, critical thinking and progress to their very own little niche within SCAM, they stop liking it and start aggressing the critic.
I suppose this is entirely obvious as well?
Perhaps!
But it also exposes the double standard that is so deeply ingrained in SCAM.
This is an analysis that I have long hesitated to conduct. The reason for my hesitation is simple: some people might think it is vindictive, revengeful or ad hominem. After reflecting about it for years, I have now decided to go ahead with it (sorry, it’s a bit lengthy). This case study is not meant to be vindictive, but offers an important insight into the power of conflicts of interest in SCAM that are not financial but ideological. I think it is crucial that people are aware of and consider such conflicts carefully, and I can’t see how else I might demonstrate my point so plainly.
Dr Adrian White was a co-worker of mine for about 10 years. He became a trusted colleague, my ‘right hand’ man and even my deputy at my Exeter department. When I discovered that my trust had been misplaced, I did not prolong his contract (I will not dwell on this episode, those who are interested find it in my memoir). Adrian then got a senior research fellowship with Prof John Campbell (not my favourite colleague at Exeter) at the department of general practice where he continued his research on acupuncture for about 10 more years largely unsupervised.
Adrian had been an acupuncturist body and soul (in fact, I had never before met anyone so utterly convinced of the value of this therapy). When he joined my team, he was scientifically naive, and we spent many month trying to teach him how to think like a scientist. Initially, he found it very difficult to think critically about acupuncture. Later, I thought the problem was under control. Yet, most of his research in my department was guided by me and tightly supervised (i.e. I made sure that out studies were testing rather than promoting SCAM, and that our reviews were critical assessments of the existing evidence).
Thus there exist two separate and well-documented periods of a pro-acupuncture researcher:
- 10 years guided by me and members of my team;
- 10 years largely unsupervised.
What could be more tempting than to compare Adrian’s output during these two periods?
To do this, I looked up all of Adrian’s 120 publications on acupuncture and selected those 52 articles that generated factual new data (mostly clinical trials or systematic reviews). As it happens, they are numerically distributed almost equally within the two periods. The endpoints for my analysis were the directions of the conclusions of his papers. I therefore extracted, dated, and rated the 52 articles as follows:
- P = positive from the point of view of an acupuncture advocate,
- N = negative from the point of view of an acupuncture advocate.
- P/N = not clearly pointing in either direction.
To render this exercise transparent (occasionally, I was not entirely sure about my ratings), I copied all the 52 conclusions and provided links to the original papers so that anyone inferested is able to check easily.
Here are my findings. Articles 1 – 27 were published AFTER Adrian had left my department; articles 28 – 52 are his papers from the time while he worked with me.
- A definitive three-arm trial is feasible. Further follow-up reminders, minimum data collection and incentives should be considered to improve participant retention in the follow-up processes in the standardised advice and exercise booklet arm. (2016) P/N
- The available evidence suggests that adding acupuncture to symptomatic treatment of attacks reduces the frequency of headaches. Contrary to the previous findings, the updated evidence also suggests that there is an effect over sham, but this effect is small. The available trials also suggest that acupuncture may be at least similarly effective as treatment with prophylactic drugs. Acupuncture can be considered a treatment option for patients willing to undergo this treatment. As for other migraine treatments, long-term studies, more than one year in duration, are lacking. (2016) P
- The available results suggest that acupuncture is effective for treating frequent episodic or chronic tension-type headaches, but further trials – particularly comparing acupuncture with other treatment options – are needed. (2016) P
- Acupuncture during pregnancy appears to be associated with few AEs when correctly applied. (2014) P
- Although pooled estimates suggest possible short-term effects there is no consistent, bias-free evidence that acupuncture, acupressure, or laser therapy have a sustained benefit on smoking cessation for six months or more. However, lack of evidence and methodological problems mean that no firm conclusions can be drawn. Electrostimulation is not effective for smoking cessation. Well-designed research into acupuncture, acupressure and laser stimulation is justified since these are popular interventions and safe when correctly applied, though these interventions alone are likely to be less effective than evidence-based interventions. (2014) P
- The current evidence suggests that acupuncture may have some effects on drug dependence that have been missed because of choice of outcome in many previous studies, and future studies should use outcomes suggested by clinical experience. Body points and electroacupuncture, used in the original clinical observation, justify further research. (2013) P
- Acceptability is very high and may be maximised by taking a number of factors into account: full information should be provided before treatment begins; flexibility should be maintained in the appointment system and different levels of contact between fellow patients should be fostered; sufficient space and staffing should be provided and single-sex groups used wherever possible. (2012) P
- This is the first evaluation of nurse-led group (multibed) acupuncture clinics for patients with knee osteoarthritis to include a 2 year follow-up. It shows the practicability of offering a low-cost acupuncture service as an alternative to knee surgery and the service’s success in providing long-term symptom relief in about a third of patients. Using realistic assumptions, the cost consequences for the local commissioning group are an estimated saving of £100 000 a year. Sensitivity analyses are presented using different assumptions. (2012) P
- There is no consistent, bias-free evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation, but lack of evidence and methodological problems mean that no firm conclusions can be drawn. Further, well designed research into acupuncture, acupressure and laser stimulation is justified since these are popular interventions and safe when correctly applied, though these interventions alone are likely to be less effective than evidence-based interventions. (2011) P/N
- Eight (8) of 10 international acupuncture experts were able to reach consensus on the syndromes, symptoms, and treatment of postmenopausal women with hot flashes. The syndromes were similar to those used by practitioners in the ACUFLASH clinical trial, but there were considerable differences between the acupuncture points. This difference is likely to be the result of differences in approach of training schools, and whether it is relevant for clinical outcomes is not well understood. (2011) P
- 70% of those patients eligible to participate volunteered to do so; all participants had clinically identified MTrPs; a 100% completion rate was achieved for recorded self-assessment data; no serious adverse events were reported as a result of either intervention; and the end of treatment attrition rate was 17%. A phase III study is both feasible and clinically relevant. This study is currently being planned. (2010) P
- In conclusion, the results from all studies are in agreement with the hypothesis that acupuncture needling relieves hot flushes. There are few data however supporting the hypothesis that the effect of acupuncture is point specific. Future research should investigate whether there is a biological effect of needling on hot flushes or not, whether tailored treatment is superior to standardised treatment, and ways of delivering treatment that causes least discomfort and least cost. (2010) P
- Acupuncture can contribute to a more rapid reduction in vasomotor symptoms and increase in health-related quality of life in postmenopausal women but probably has no long-term effects. (2010) P
- within the context of this pilot study, the sham acupuncture intervention was found to be a credible control for acupuncture. This supports its use in a planned, definitive, randomised controlled trial on a similar whiplash injured population. (2009) N/P
- factors other than the TCM syndrome diagnoses and the point selection may be of importance regarding the outcome of the treatment. (2009) N/P
- Acupuncture plus self-care can contribute to a clinically relevant reduction in hot flashes and increased health-related quality of life in postmenopausal women. (2009) P
- the authors conclude that acupuncture could be a valuable non-pharmacological tool in patients with frequent episodic or chronic tension-type headaches. (2009) P
- there is consistent evidence that acupuncture provides additional benefit to treatment of acute migraine attacks only or to routine care. There is no evidence for an effect of ‘true’ acupuncture over sham interventions, though this is difficult to interpret, as exact point location could be of limited importance. Available studies suggest that acupuncture is at least as effective as, or possibly more effective than, prophylactic drug treatment, and has fewer adverse effects. Acupuncture should be considered a treatment option for patients willing to undergo this treatment. (2009) P
- We have conducted the first survey of the effects of provision of acupuncture in UK general practice, using data provided by the NHS, and uncovered a wide variation in the availability of the service in different areas. We have been unable to demonstrate any consistent differences in the prescribing or referral rates that could be due to the use of acupuncture in these practices. The wide variation in the data means that if such a trend exists, a very large survey would be needed to identify it. However, we discovered inaccuracies and variations in presentation of data by the PCTs which have made the numerical input, and hence our results, unreliable. Thus the practicalities of access to data and the problems with data accuracy would preclude a nationwide survey. (2008) P
- In conclusion, there is limited evidence deriving from one study that deep needling directly into myofascial trigger points has an overall treatment effect when compared with standardised care. Whilst the result of the meta-analysis of needling compared with placebo controls does not attain statistically significant, the overall direction could be compatible with a treatment effect of dry needling on myofascial trigger point pain. However, the limited sample size and poor quality of these studies highlights and supports the need for large scale, good quality placebo controlled trials in this area. (2009) P
- We conclude that limited evidence supports acupuncture use in treating pregnancy-related pelvic and back pain. Additional high-quality trials are needed to test the existing promising evidence for this relatively safe and popular complementary therapy. (2008) P
- Acupuncture appears to offer symptomatic improvement to some patients with fibromyalgia in a tertiary clinic who have failed to respond to other treatments. In view of its safety, further acupuncture research is justified in this population. (2007) P
- It is speculated that optimal results from acupuncture treatment for osteoarthritis of the knee may involve: climatic factors, particularly high temperature; high expectations of patients; minimum of four needles; electroacupuncture rather than manual acupuncture, and particularly, strong electrical stimulation to needles placed in muscle; and a course of at least 10 treatments. These factors offer some support to criteria for adequate acupuncture used in the recent review. In addition, ethnic and cultural factors may influence patients’ reporting of their symptoms, and different versions of an outcome measure are likely to differ in their sensitivity – both factors which may lead to apparent rather than real differences between studies. The many variables in a study are likely to be more tightly controlled in a single centre study than in multicentre studies. (2007) P
- Any effects of acupressure on smoking withdrawal, as an adjunct to the use of NRT and behavioural intervention, are unlikely to be detectable by the methods used here and further preliminary studies are required before the hypothesis can be tested. (2007) P
- Auricular acupuncture appears to be effective for smoking cessation, but the effect may not depend on point location. This calls into question the somatotopic model underlying auricular acupuncture and suggests a need to re-evaluate sham controlled studies which have used ‘incorrect’ points. Further experiments are necessary to confirm or refute these observational conclusions. (2006) P
- Acupuncture that meets criteria for adequate treatment is significantly superior to sham acupuncture and to no additional intervention in improving pain and function in patients with chronic knee pain. Due to the heterogeneity in the results, however, further research is required to confirm these findings and provide more information on long-term effects. (2007) P
- There is no consistent evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation, but methodological problems mean that no firm conclusions can be drawn. Further research using frequent or continuous stimulation is justified. (2006) N/P
- Acupuncture is not superior to sham treatment for recovery in activities of daily living and health-related quality of life after stroke, although there may be a limited effect on leg function in more severely affected patients. (2005) N
- The evidence from controlled trials is insufficient to conclude whether acupuncture is an effective treatment for depression, but justifies further trials of electroacupuncture. (2005) N
- Acupuncture effectively relieves chronic low back pain. No evidence suggests that acupuncture is more effective than other active therapies. (2005) N/P
- In view of the small number of studies and their variable quality, doubt remains about the effectiveness of acupuncture for gynaecological conditions. Acupuncture and acupressure appear promising for dysmenorrhoea, and acupuncture for infertility, and further studies are justified. (2003) N
- In conclusion, the results suggest that the procedure using the new device is indistinguishable from the same procedure using real needles in acupuncture naïve subjects, and is inactive, where the specific needle sensation (de qi) is taken as a surrogate measure of activity. It is therefore a valid control for acupuncture trials. The findings also lend support to the existence of de qi, a major concept underlying traditional Chinese acupuncture. (2002) N/P
- There is no clear evidence that acupuncture, acupressure, laser therapy or electrostimulation are effective for smoking cessation. (2002) N
- Collectively, these data imply that acupuncture is superior to various control interventions, although there is insufficient evidence to state whether it is superior to placebo. (2002) N/P
- In conclusion, the incidence of adverse events following acupuncture performed by doctors and physiotherapists can be classified as minimal; some avoidable events do occur. Acupuncture seems, in skilled hands, one of the safer forms of medical intervention. (2001) N/P
- Based on the evidence of rigorous randomised controlled trials, there is no compelling evidence to show that acupuncture is effective in stroke rehabilitation. Further, better-designed studies are warranted. (2001) N
- Although it has already been demonstrated that severe adverse events seem to be uncommon in standard practice, many serious cases of negligence have been found in the present review, suggesting that training system for acupuncturists (including medical doctors) should be improved and that unsupervised self-treatment should be discouraged. (2001) N
- Direct needling of myofascial trigger points appears to be an effective treatment, but the hypothesis that needling therapies have efficacy beyond placebo is neither supported nor refuted by the evidence from clinical trials. Any effect of these therapies is likely because of the needle or placebo rather than the injection of either saline or active drug. Controlled trials are needed to investigate whether needling has an effect beyond placebo on myofascial trigger point pain. (2001) N/P
- Although the incidence of minor adverse events associated with acupuncture may be considerable, serious adverse events are rare. Those responsible for establishing competence in acupuncture should consider how to reduce these risks. (2001) N
- In conclusion, this study does not provide evidence that this form of acupuncture is effective in the prevention of episodic tension-type headache. (2000) N
- The present study provides no strong evidence to support the hypothesis that the acupuncture point SP6 is more tender in women and in men. Recommendations for further investigations are discussed. (2000) N
- Acupuncture has not been demonstrated to be efficacious as a treatment for tinnitus on the evidence of rigorous randomized controlled trials. (2000) N
- We conclude that acupuncture continues to be associated with occasional, serious adverse events and fatalities. These events have no geographical limits. Most of these events are due to negligence. Everyone concerned with setting standards, delivering training, and maintaining competence in acupuncture should familiarise themselves with the lessons to be learnt from these untoward events. (2000) N
- Overall, the existing evidence suggests that acupuncture has a role in the treatment of recurrent headaches. However, the quality and amount of evidence is not fully convincing. There is urgent need for well-planned, large-scale studies to assess effectiveness and efficiency of acupuncture under real life conditions. (1999) N/P
- While the frequency of adverse effects of acupuncture is unknown and they may be rare, knowledge of normal anatomy and anatomical variations is essential for safe practice and should be reviewed by regulatory bodies and those responsible for training courses. (1999) N
- In conclusion, the hypothesis that acupuncture is efficacious in the treatment of neck pain is not based on the available evidence from sound clinical trials. Further studies are justified. (1999) N
- Even though all studies are in accordance with the notion that acupuncture is effective for temporomandibular joint dysfunction, this hypothesis requires confirmation through more rigorous investigations. (1999) N
- Acupuncture is not free of risks. All adverse events reported in 1997 would have been avoidable. The absolute number of cases is small, but the degree of underreporting remains unknown. (1999) N
- This form of electroacupuncture is no more effective than placebo in reducing nicotine withdrawal symptoms. (1998) N
- Acupuncture was shown to be superior to various control interventions, although there is insufficient evidence to state whether it is superior to placebo. (1998) N/P
- Considerable variation was observed in the scores awarded by the acupuncture experts. (1998) N
- It is therefore concluded that, according to the data published to date, the evidence that acupuncture is a useful adjunct for stroke rehabilitation is encouraging but not compelling. More and better trials are required to clarify this highly relevant issue. (1996) N
The results are remarkable (particularly considering that one would not expect unbiased studies or reviews of acupuncture to generate plenty of positive conclusions):
0 times N, 5 times N/P, 22 times P – after Adrian had left my department,
17 times N, 7 times N/P, 0 times P – while Adrian worked in my department.
From these figures, it is tempting to calculate the ratios for both periods of negative : positive conclusions:
zero versus infinite
If that is not impressive, I don’t know what is!
Looking just at the positive and the negative papers over the years:
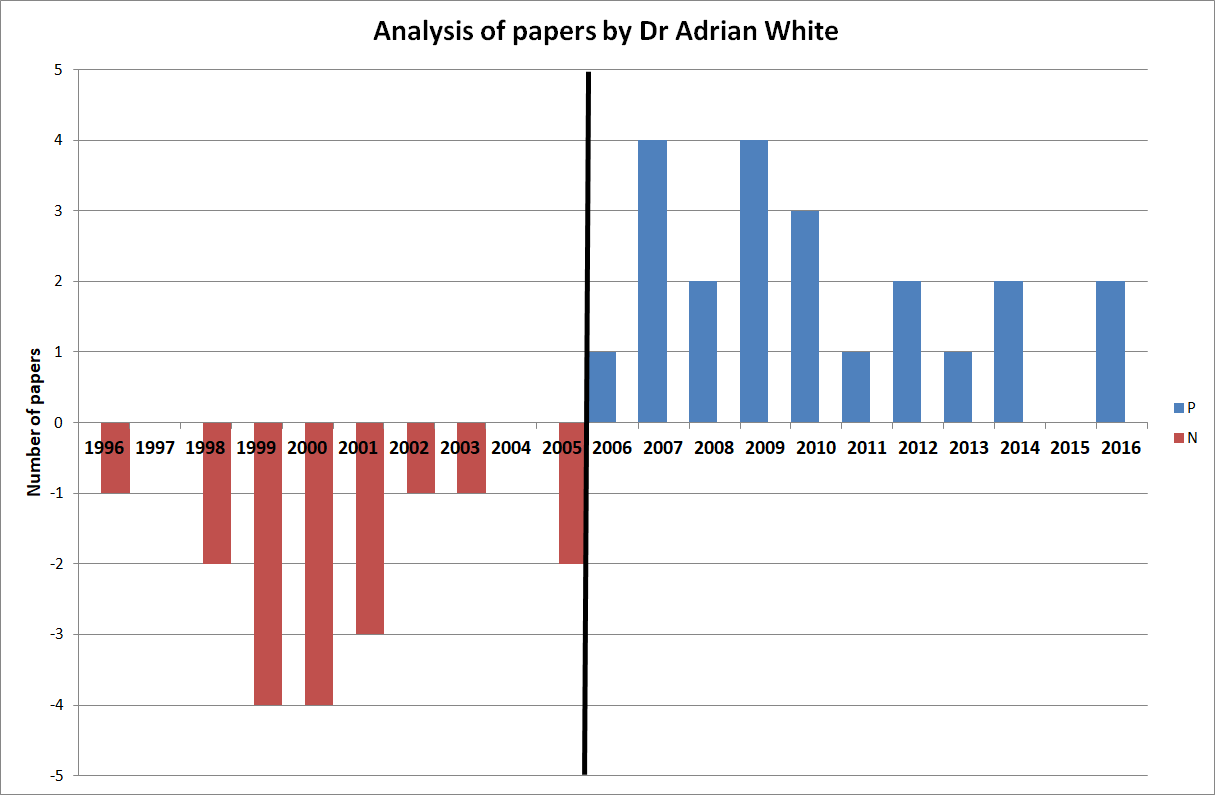 One could discuss these papers in more detail, but I think this is hardly necessary. Just a few highlights perhaps: look at articles No 5, 20 and 27 for examples of turning an essentially negative finding into a positive conclusion. Notice that Adrian conducted a clinical trial of acupuncture for smoking cessation (No 49) while working with me and later published uncritical positive reviews on the subject. Does this not indicate that he distrusted his own study because it had not generated the result he had hoped for?
One could discuss these papers in more detail, but I think this is hardly necessary. Just a few highlights perhaps: look at articles No 5, 20 and 27 for examples of turning an essentially negative finding into a positive conclusion. Notice that Adrian conducted a clinical trial of acupuncture for smoking cessation (No 49) while working with me and later published uncritical positive reviews on the subject. Does this not indicate that he distrusted his own study because it had not generated the result he had hoped for?
Of course, my analysis is merely a case study and therefore my findings are not generalisable. However, in my personal experience, the described phenomenon is by no means an exception in SCAM research. I have observed similar phenomena over and over again. Just look at the ALTERNATIVE MEDICINE HALL OF FAME that I created for this blog:
- John Weeks (editor of JCAM)
- Deepak Chopra (US entrepreneur)
- Cheryl Hawk (US chiropractor)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various, Germany)
- Claudia Witt (homeopathy, Germany and Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
But Adrian’s case might be unique because it allows us to make a longitudinal observation over two decades. And it suggests to me that an ideological bias can (and often is) so strong and indistructable that is re-emerges as soon as it is no longer kept under strict control.
I have long suspected that ideological conflicts of interest have a much more powerful influence in SCAM research than financial ones. Such an overpowering influence might even be characteristic to much of SCAM research. And because it can be so dominant, it seems important to know about. People reading research need to be aware that it originates from a biased source, and funders who finance research would be wise to think twice about supporting researchers who are likely to generate findings that are biased and therefore false-positive. In the final analysis, such research is worse than no research at all.
Today is the day to admit it: we all owe a big THANKS to the worldwide homeopathy community. We should be most grateful to them all for selflessly demonstrating so indisputably something of fundamental importance:
homeopaths do not believe in their own outlandish, science-defying assumptions.
Yes, I really do appreciate the courage and altruism that was required for this epoch-making step!
Perhaps I better explain.
On 10 November, I issued ‘a challenge for all homeopaths of the world‘.
The deal was structured around a homeopathic proving (or, if you wish, around the assumption that highly diluted homeopathic remedies can have any noticable effects) and went as follows:
- you, the convinced homeopath, name the 6 homeopathic remedies that you cannot possibly miss when doing a proving on yourself;
- I order them in the potency you wish (only condition: it must be higher than C12) from a reputable source;
- I have the bottles delivered unopened to a notary where I live;
- the notary fills them into containers marked 1-6 (if you wish, you can send the notary empty containers for that ppurpose);
- the notary keeps the code under lock and key that links the name of the remedies to the numbers 1-6;
- he then mails the coded 6 remedies to you;
- you can use the proving method which you consider best and do as many provings as you like (the only limiting factors are the number of globuli in the containers and the time you have to crack the code);
- I give you 100 days for conducting the provings;
- once you are ready, you send your verdicts to the notary (e.g. 1 = rhus, tox, 2 = sulfur, 3 = arsenic, etc., etc.);
- the notary looks up the code and lets us both know the result.
I am happy to pay all the costs involved in the experiment (notary, remedies, postage, etc.). We can also discuss some of the details of this challenge, in case they run counter to your views on provings, rigorous science, etc.
To make sure we both ‘mean business’, once we both accept these conditions (you can flesh out the missing details as you wish), we both transfer a sum Euro 2 000 to an account with the notary. If you want to increase the sum, please let me know; as I said, we can discuss most of the details of my challenge to suit your needs. If you manage to ‘crack the code’ 1-6, the notary will transfer the sum of Euro 4 000 (your deposit and mine) to your account. If you fail, he will transfer the same amount to my account.
__________________________________________
In my original post, I made it abundantly clear that the entry to the challenge would close at the end of 2020. While it was still open, I did everything I could to let homeopaths know about the challenge. Because homeopathy originated in Germany and is still fairly popular there, I even re-published my challenge in German. In addition, I and others tweeted many times about it (in English, German, French, Spanish and possibly other languages as well), even directly to homeopaths across the globe.
As no homeopath has come forward to take up the challenge in time, and as no sound argument has emerged to convince me that my challenge was unreasonable, unscientific or unfair, it now is an indisputable fact that:
homeopaths do not believe in their own outlandish, science-defying assumptions.
I am most grateful to the worldwide community of homeopaths for heroically documenting the truth so clearly. It can’t have been easy to be so honest at the cost of homeopathy’s reputation. But I believe that this is an important and honourable step into the right direction. It provides essential information for non-homeopaths who want to understand the practice and profession of homeopathy.
MANY THANKS AGAIN
PS
In the interest of progress, please publicise the news as widely as you can.
