progress
For quite some time now, I have had the impression that the top journals of general medicine show less and less interest in so-called alternative medicine. So, I decided to do some Medline searches to check. Specifically, I searched for 4 different SCAMs:
- homeopathy
- acupuncture
- chiropractic
- herbal medicine
I wanted to see how often 7 leading medical journals from the US, UK, Australia, Germany, and Austria carried articles indexed under these headings:
- JAMA – US
- NEJM – US
- BMJ – UK
- Lancet – UK
- Aust J Med – Australia
- Dtsch Med Wochenschrift – Germany
- Wien Med Wochenschrift – Austria
This is what I found (the 1st number is the total number of articles ever listed; the 2nd number is the maximum number in any year; the 3rd number in brackets is the year when that maximum occurred)
JAMA
Homeopathy: 17, 3 (1998)
Acupuncture: 176, 21 (2017)
Chiropractic: 49, 4 (1998)
Herbal medicine: 43, 5 (2001)
NEJM
Homeopathy: 6, 3 (1986)
Acupuncture: 49, 8 (1974)
Chiropractic: 43, 13 (1980)
Herbal medicine: 29, 12 (1999)
BMJ
Homeopathy: 122, (10, 1995)
Acupuncture: 405, 31 (2021)
Chiropractic: 99, 11 (2021)
Herbal medicine: 158, 13 (2018)
Lancet
Homeopathy: 75, 11 (2005)
Acupuncture: 93, 12 (1973)
Chiropractic: 20, 5 (1993)
Herbal medicine: 46, 6 (1993)
Aust J Med
Homeopathy: 9, 2 (2010)
Acupuncture: 78, 13 (1974)
Chiropractic: 34, 4 (1985)
Herbal medicine: 20, 2 (2017)
Deutsche Medizinische Wochenschrift
Homeopathy: 27, 4 (1999)
Acupuncture: 34, 6 (1978)
Chiropractic: 14, 3 (1972)
Herbal medicine: 6, 1 (2020)
Wiener Medizinische Wochenschrift
Homeopathy: 11, 4 (2005)
Acupuncture: 32, 8 (1998)
Chiropractic: 8, 2 (1956)
Herbal medicine: 16, 3 (2002)
These figures need, of course, to be taken with a rather large pinch of salt. There are many pitfalls in interpreting them, e.g. misclassifications by Medline. Yet they are, I think, revealing in that they suggest several interesting trends.
- All in all, my suspicion that the top journals of various countries are less and less keen on SCAM seems to be confirmed. The years where the maximum of papers on specific SCAMs was published are often long in the past.
- The UK journals seem to be by far more open to SCAM that the publications from other countries. This is mostly due to the BMJ – in fact, it turns out to be the online journal ‘BMJ-open’. And this again is to a great part caused by the BMJ-open carrying a sizable amount of acupuncture papers in recent months.
- The two US journals seem particularly cautious about SCAM papers. When looking at the type of articles in the US journals (and especially the NEJM), one realizes that most of them are ‘letters to the editor’ which seems to confirm the dislike of these journals for publishing original research into SCAM. Another interpretation of this phenomenon, of course, would be that only very few SCAM studies are of a high enough quality to make it into these two top journals.
- I was amazed to see how little SCAM was published in the two German-language journals. Vis a vis the high popularity of SCAM in these countries, I find this not easy to understand. Perhaps, one also needs to consider that these two journals publish considerably less original research than the other publications
- If we look at the differences between the 4 types of SCAM included in my assessment, we find that acupuncture is by far the most frequently published modality. The other 3 are on roughly the same level, with chiropractic being the least frequent – which I thought was surprising.
- Overall, the findings do not generate the impression that – despite the many billions spent on SCAM research during the last decades – SCAM has made important inroads into science or medicine.
I have often commented on the dismal state of the many SCAM journals; these days, they seem to publish almost exclusively poor-quality papers with misleading conclusions. It can therefore be expected that these journals will be more and more discarded by everyone (except the few SCAM advocates who publish their rubbish in them) as some sort of cult publications. In turn, this means that only SCAM studies published in mainstream journals will have the potential of generating any impact at all.
For this reason, my little survey might be relevant. It is far from conclusive, of course, yet it might provide a rough picture of what is happening in the area of SCAM research.
I think this press release might interest you:
Science advocates have filed a groundbreaking lawsuit against Boiron, Inc., one of the largest manufacturers of homeopathic products in the world, for deceiving vulnerable consumers with useless products dressed up to look like real medicine. The Center for Inquiry (CFI), which fights on behalf of consumers against pseudoscience, says Boiron routinely made false claims about what its products will treat and heal, misleading the public about the absurd pseudoscientific basis for Boiron products, and even lying about the ingredients their products contain.
“The facts could not be more clear. Boiron profits massively by deceiving consumers in their time of need,” said CFI Vice President and Legal Counsel Nick Little. “Boiron knows its products are worthless junk, so they do everything they can to obscure the truth in order to offload their snake oil upon the unwitting, the ill-informed, and the vulnerable. They can’t be allowed to get away with it any longer.”
Adherents of homeopathy claim, without evidence, that a substance which causes harm to a healthy person will cure anyone else suffering the same type of harm. In homeopathic products, the “active” ingredients are highly diluted mixtures of the so-called cures; the ingredient ends up so diluted, often literally no trace of the original substance remains. Manufacturers like Boiron then sell miniscule amounts of the already incredibly diluted ingredients and promise astounding results.
In its lawsuit, brought under the District of Columbia Consumer Protection Procedures Act, CFI alleges that Boiron sold a plethora of materially identical products, each made up of sugar pills and powders. Despite no scientifically detectable active ingredient, Boiron falsely promised consumers that each item would treat and cure a particular illness, injury, or health condition.
“Boiron sells little pills of sugar with grandiose claims. It’s hard to believe anyone would try to pass off such junk as a surefire way to treat painful skin problems, heal mental health issues, and even to counteract menopause,” said CFI Staff Attorney Aaron D. Green. “But Boiroin has been doing just that by tricking consumers into risking their health and throwing away their money on its fancy faux ‘medicines.’ It’s time for Boiron and all homeopathy hucksters to be held accountable.”
In its complaint, CFI notes that Boiron sells Saccharum officinale as a treatment for “nervous agitation in children after overindulgence.”
“Most parents would rightfully be skeptical of this product if Boiron told them what Saccharum officinale actually is,” said Green. “Table sugar.”
According to recent industry accounts, 85 percent of consumers who purchased homeopathic products did not realize they were homeopathic, and nine out of ten consumers did not even know what the term homeopathic meant.
Apart from selling products they know are useless, Boiron also misrepresented the products’ ingredients. Four Boiron products were analyzed by an independent lab, and, not only were no traces of the supposed active ingredient found, even one of the inactive ingredients could not be scientifically detected.
The Center for Inquiry is currently engaged in other lawsuits regarding homeopathy, including consumer protection cases against megaretailers CVS and Walmart for their sale and marketing of homeopathic products, the matter recently heard by the DC Court of Appeals. CFI is also engaged in an active Freedom of Information Act lawsuit that demands the Department of Health and Human Services grant the public access to the Homeopathic Pharmacopoeia of the United States (HPUS), the “bible of homeopathy” upon which federal regulation of homeopathy is based and to which the industry restricts access but for those willing to pay thousands of dollars for the privilege.
_________________________
All I can add to this is: good luck to the CFI and let’s hope reason will prevail!
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?
The pandemic has shown how difficult it can be to pass laws stopping healthcare professionals from giving unsound medical advice has proved challenging. The right to freedom of speech regularly conflicts with the duty to protect the public. How can a government best sail between Scylla and Charybdis? JAMA has just published an interesting paper addressing these issues. Here is an excerpt from the article that might stimulate some discussion:
The government can take several actions, including:
- Imposing sanctions on COVID-19–related practices by licensed professionals that flout substantive laws in connection with providing medical services, even if those medical services include speech. This includes physicians failing to comply with COVID-19–related public health laws applicable to medical offices and health facilities, such as mask wearing, social distancing, and restrictions on elective procedures.
- Sanctioning recommendations by professionals that patients take illegal medications or controlled substances without following legally required procedures. The government can also sanction the marketing by others of prescription medications for unapproved indications. However, “off-label” prescribing by physicians (eg, for hydroxychloroquine or ivermectin) remains lawful as long as a medication is approved by the US Food and Drug Administration for any indication and no specific legal conditions on use are in effect.
- Enforcing tort law actions (eg, malpractice, lack of informed consent) in cases of alleged patient injury that result from recommending a potentially dangerous treatment or failing to recommend a necessary treatment.
- Imposing sanctions on individualized medical advice by unlicensed individuals or organizations if giving that advice constitutes the unlawful practice of medicine.
In addition, the government probably can:
- Impose sanctions for false or misleading information offered to obtain a financial or personal benefit, particularly if giving the information constitutes fraud under applicable law. This would encompass physicians who knowingly spread false information to create celebrity or attract patients.
- Threaten disciplinary action by licensing boards against health professionals whose speech to patients conveys incorrect science or substandard medicine.
- Specify the information that may and may not be imparted by private organizations and professionals as part of specific clinical services paid for by government, such as special programs for COVID-19 testing or treatment.
- Reject legal challenges to, and enforce through generally applicable contract or employment laws, any restrictions private health care organizations place on speech by affiliated health professionals, particularly in the absence of special laws conferring “conscience” protections. This would include medical staff membership and privileges, hospital or other employment agreements, and insurance network participation.
- Enforce restrictions on speech adopted by private professional or self-regulatory organizations if the consequences for violations are limited to revoking organizational membership or accreditation.
However, the government probably cannot:
- Compel or limit health professional speech not made in connection with patient care, even if the speech is false or misleading, regardless of its alleged effect on public trust in health professions.
- Sanction speech to the general public rather than to patients, whether or not by health professionals, especially if conveyed with a disclaimer that the speech is “not intended as medical advice.”
- Sanction speech by health professionals to patients conveying political views or skepticism of government policy.
- Enforce restrictions involving information by public universities and public hospitals that legislatures, regulatory agencies, and professional licensing boards would not be constitutionally permitted to impose directly.
- Adopt restrictions on information related to overall clinical services funded by large government health programs, such as Medicare and Medicaid.
_____________________________
The article was obviously written with MDs in mind and applies only to US law. As we have seen in previous posts and comments, the debate is, however, wider. We should, I think, also have it in relation to practitioners of so-called alternative medicine (SCAM) and medical ethics. Moreover, it should go beyond advice about COVID and be extended to any medical advice given by any type of healthcare practitioner.
Homeopathy was born in Germany about 200 years ago. Now we are witnessing its slow demise due to a lack of convincing evidence.
It is only a small announcement by, but it sends out a big signal: Bremen’s doctors’ parliament has decided to cancel all homeopathy contracts.
Opponents and supporters of homeopathy agree on one thing: the latest decision of the Association of Statutory Health Insurance (KV) Bremen is an important nail in the coffin for alternative medicine. The KV representative assembly has just decided to terminate all selective contracts concerning the reimbursement of homeopathic services.
Some are rejoicing: “In Bremen it’s over” tweeted Dr. Hans-Werner Bertelsen, for example. The “sugar-sugar affine clientele” will have a harder time in the future, he stated. And: “The financing of woo must be stopped politically.”
Oliver Borrmann, a general practitioner and homeopath from Bremen, on the other hand, is outraged. He speaks of discrimination, of a conflagration, and of being the “whipping boy for everything”. “They are watching alternative medicine die right now,” he professes. It is considered chic to rise above homeopathy, he claims, and anyone who defends it is put down.
In Bremen, three contracts existed with several companies and health insurance funds which extended the range of paid services to include homeopathy for their patients. Both the KV Bremen and the homeopath Borrmann speak of a group of insured persons that is not particularly large – in Borrmann’s practice there are about 30 patients – but of a political signal that emanates from the decision.
It is the reason for the termination that makes him concerned and take notice, says Borrmann. It states: “As long as not all treatments whose benefits have already been scientifically proven can be fully financed in the statutory health insurance system, there will be no funds left for procedures for whose concrete benefits there is no evidence.”
This phraseology which quotes the KV board members Bernhard Rochell and Peter Kurt Josenhans sounds unwieldy – but it contains a clear message: homeopathy is considered useless by the KV.
——————————————-
One does not need to be a clairvoyant to predict that other parts of Germany will follow Bremen’s example. Effective lobbying and financial interests have protected German homeopathy for decades, but the eventual victory of reason, science, and evidence was inevitable.
The new German secretary of health, Prof Lauterbach, tweeted in connection with the news from Bremen:
“Mit der Wissenschaft werden Pandemien bekämpft und Krankheiten geheilt. Wir brauchen mehr Wissenschaft in der Behandlung, nicht weniger. Die Homöopathie hat keinen Platz in der modernen Medizin.”
(Science is used to fight pandemics and cure diseases. We need more science in treatment, not less. Homeopathy has no place in modern medicine.)
It must have been 17 or 18 years ago that I first met Fiona Fox. We were both giving a lecture at the same meeting. My talk was about a small study we did surveying UK homeopaths’ attitudes toward MMR vaccinations. It had landed me in deep waters: some homeopaths had complained and the Exeter ethics committee retrospectively withdrew their approval and forbade me to publish the findings (which were less than flattering for the homeopaths). I told my committee to go yonder and multiply and published our results swiftly. I was then told that I had violated our research ethics and threatened with disciplinary action by my own university.
Fiona seemed to like my stance and realized why I had to do what I did. A little later, she invited me to give a presentation at the ‘Science Media Centre’ (SMC) for journalists about our research. It was then that I realized what the SMC did and how important its work truly was.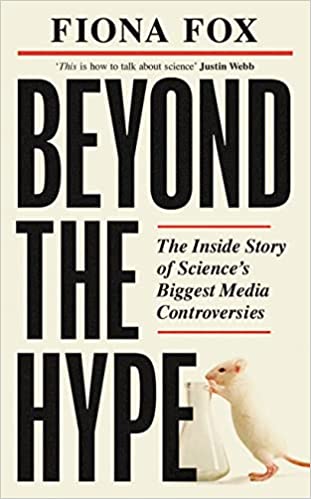
At the time, the SMC consisted of a small team of highly motivated people linking scientists with journalists – potentially a win/win situation:
- The scientists would see with their own eyes how important journalists could be for getting their message across.
- And the journalists might comprehend that things were frequently more complex than expected.
Yet, by no means an easy job; scientists are often (sometimes rightly) nervous about speaking to journalists, and journalists sometimes (rightly) feel that scientists are not from the same planet as they are. But if it works out well – and in the SMC it usually does – the beneficiary is the consumer who can read excellent science journalism.
The concept of the SMC was as simple as it was convincing!
No wonder then that it was a monumental success. The SMC grew and so did his influence nationally and internationally. Today, there is hardly a media outlet in the UK that does not regularly refer to the SMC when reporting on matters of science. Much of the outstanding reputation of the SMC is due to the tireless work of Fiona. Her enthusiasm for science is infectious, her energy is impressive, her skills in dealing with experts are immaculate, and her nose for a good story is infallible.
In ‘BEYOND THE HYPE‘, Fiona has now summarized the first 20 eventful years of the SMC. She recounts her favorite moments and some of the biggest science stories that emerged with the help of the SMC. The book is a true page-turner and a ‘must read’ for everyone with an interest in science – entertaining and educational in equal measure. It takes us behind the scenes of some of the most remarkable recent developments in science. Fiona’s book will be out on 7 April; it is a historical document that teaches us important lessons and deserves to be read widely.
I hope that the next 20 years of the SMC will be as good as the first.
Vaccine hesitancy is currently recognized by the WHO as a major threat to global health. During the COVID-19 pandemic, there has been a growing interest in the role of social media in the propagation of false information and fringe narratives regarding vaccination. Using a sample of approximately 60 billion tweets, Danish investigators conducted a large-scale analysis of the vaccine discourse on Twitter. They used methods from deep learning and transfer learning to estimate the vaccine sentiments expressed in tweets, then categorize individual-level user attitudes towards vaccines. Drawing on an interaction graph representing mutual interactions between users, They analyzed the interplay between vaccine stances, interaction network, and the information sources shared by users in vaccine-related contexts.
The results show that strongly anti-vaccine users frequently share content from sources of a commercial nature; typically sources that sell alternative health products for profit. An interesting aspect of this finding is that concerns regarding commercial conflicts of interests are often cited as one of the major factors in vaccine hesitancy.
The authors furthermore demonstrate that the debate is highly polarized, in the sense that users with similar stances on vaccination interact preferentially with one another. Extending this insight, the authors provide evidence of an epistemic echo chamber effect, where users are exposed to highly dissimilar sources of vaccine information, enforcing the vaccination stance of their contacts.
The authors concluded that their findings highlight the importance of understanding and addressing vaccine mis- and disinformation in the context in which they are disseminated in social networks.
In the article, the authors comment that their findings paint a picture of the vaccine discourse on Twitter as highly polarized, where users who express similar sentiments regarding vaccinations are more likely to interact with one another, and tend to share contents from similar sources. Focusing on users whose vaccination stances are the positive and negative extremes of the spectrum, we observe relatively disjoint ‘epistemic echo chambers’ which imply that members of the two groups of users rarely interact, and in which users experience highly dissimilar ‘information landscapes’ depending on their stance. Finally, we find that strongly anti-vaccine users much more frequently share information from actors with a vested commercial interest in promoting medical misinformation.
One implication of these findings is that online (medical) misinformation may present an even greater problem than previously thought, because beliefs and behaviors in tightly knit, internally homogeneous communities are more resilient, and provide fertile ground for fringe narratives, while mainstream information is attenuated. Furthermore, such polarization of communities may become self-perpetuating, because individuals avoid those not sharing their views, or because exposure to mainstream information might further entrench fringe viewpoints.
Chronic low back pain (CLBP) is among the most common types of pain in adults. It is also the domain for many types of so-called alternative medicine (SCAM). However, their effectiveness remains questionable, and the optimal approach to CLBP remains elusive. Meditation-based therapies constitute a form of SCAM with high potential for widespread availability.
This systematic review and meta-analysis of randomized clinical trials evaluated the efficacy of meditation-based therapies for CLBP management. The primary outcomes were pain intensity, quality of life, and pain-related disability; the secondary outcomes were the experienced distress or anxiety and pain bothersomeness in the patients. The PubMed, Embase, and Cochrane databases were searched for studies published from their inception until July 2021, without language restrictions.
A total of 12 randomized clinical trials with 1153 patients were included. In 10 trials, meditation-based therapies significantly reduced the CLBP pain intensity compared with nonmeditation therapies (standardized mean difference [SMD] -0.27, 95% CI = -0.43 to – 0.12, P = 0.0006). In 7 trials, meditation-based therapies also significantly reduced CLBP bothersomeness compared with nonmeditation therapies (SMD -0.21, 95% CI = -0.34 to – 0.08, P = 0.002). In 3 trials, meditation-based therapies significantly improved patient quality of life compared with nonmeditation therapies (SMD 0.27, 95% CI = 0.17 to 0.37, P < 0.00001).
The authors concluded that meditation-based therapies constitute a safe and effective alternative approach for CLBP management.
The problem with this conclusion is that the primary studies are mostly of poor quality. For instance, they do not control for placebo effects (which is obviously not easy in this case). Thus, we need to take the conclusion with a pinch of salt.
However, since the same limitations apply to chiropractic and osteopathy, and since meditation has far fewer risks than these approaches, I would gladly recommend meditation over manipulative therapies. Or, to put it plainly: in terms of risk/benefit balance, meditation seems preferable to spinal manipulation.
The new issue of the BMJ carries an article on acupuncture that cries out for a response. Here, I show you the original article followed by my short comments. For clarity, I have omitted the references from the article and added references that refer to my comments.
_________________________________________
Conventional allopathic medicine [1]—medications and surgery [2] used in conventional systems of medicine to treat or prevent disease [3]—is often expensive, can cause side effects and harm, and is not always the optimal treatment for long term conditions such as chronic pain [4]. Where conventional treatments have not been successful, acupuncture and other traditional and complementary medicines have potential to play a role in optimal patient care [5].
According to the World Health Organisation (WHO) 2019 global report, acupuncture is widely used across the world. [6] In some countries acupuncture is covered by health insurance and established regulations. [7] In the US, practitioners administer over 10 million acupuncture treatments annually. [6] In the UK, clinicians administer over 4 million acupuncture treatments annually, and it is provided on the NHS. [6]
Given the widespread use of acupuncture as a complementary therapy alongside conventional medicine, there has been an increase in global research interest and funding support over recent decades. In 2009, the European Commission launched a Good Practice in Traditional Chinese Medicine Research (GP-TCM) funding initiative in 19 countries. [7] The GP-TCM grant aimed to investigate the safety and efficacy of acupuncture as well as other traditional Chinese medicine interventions.
In China, acupuncture is an important focus of the national research agenda and receives substantial research funding. [8] In 2016, the state council published a national strategy supporting universal access to acupuncture by 2020. China has established more than 79 evidence-based traditional Chinese medicine or integrative medicine research centers. [9]
Given the broad clinical application and rapid increase in funding support for acupuncture research, researchers now have additional opportunities to produce high-quality studies. However, for this to be successful, acupuncture research must address both methodological limitations and unique research challenges.
This new collection of articles, published in The BMJ, analyses the progress of developing high quality research studies on acupuncture, summarises the current status, and provides critical methodological guidance regarding the production of clinical evidence on randomised controlled trials, clinical practice guidelines and health economic evidence. It also assesses the number and quality of systematic reviews of acupuncture. [10] We hope that the collection will help inform the development of clinical practice guidelines, health policy, and reimbursement decisions. [11]
The articles document the progress of acupuncture research. In our view, the emerging evidence base on the use of acupuncture warrants further integration and application of acupuncture into conventional medicine. [12] National, regional, and international organisations and health systems should facilitate this process and support further rigorous acupuncture research.
Footnotes
This article is part of a collection funded by the special purpose funds for the belt and road, China Academy of Chinese Medical Sciences, National Natural Science Foundation of China, the National Center for Complementary and Integrative Health, the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine, the Special Project of “Lingnan Modernization of Traditional Chinese Medicine” of the 2019 Guangdong Key Research and Development Program, and the Project of First Class Universities and High-level Dual Discipline for Guangzhou University of Chinese Medicine. The BMJ commissioned, peer reviewed, edited, and made the decision to publish. Kamran Abbasi was the lead editor for The BMJ. Yu-Qing Zhang advised on commissioning for the collection, designed the topic of the series, and coordinated the author teams. Gordon Guyatt provided valuable advice and guidance. [13]
1. Allopathic medicine is the term Samuel Hahnemann coined for defaming conventional medicine. Using it in the first sentence of the article sets the scene very well.
2. Medicine is much more than ‘medications and surgery’. To imply otherwise is a strawman fallacy.
3. What about rehabilitation medicine?
4. ‘Conventional medicine is not always the optimal treatment’? This statement is very confusing and wrong. It is true that conventional medicine is not always effective. However, it is by definition the best we currently have and therefore it IS optimal.
5. Another fallacy: non sequitur
6. Another fallacy: appeal to popularity.
7. Yet another fallacy: appeal to authority.
8. TCM is heavily promoted by China not least because it is a most lucrative source of income.
9. Several research groups have shown that 100% of acupuncture research coming out of China report positive results. This casts serious doubt on the reliability of these studies (see, for instance, here, here, and here).
10. It has been noted that more than 80 percent of clinical data from China is fabricated.
11. Based on the points raised above, it seems to me that the collection’s aim is not to provide objective information but uncritical promotion.
12. I find it telling that the authors do not even consider the possibility that rigorous research might demonstrate that acupuncture cannot generate more good than harm.
13. This statement essentially admits that the series of articles constitutes paid advertising for TCM. The BMJ’s peer-review process must have been less than rigorous in this case.
Neurosurgeons from the Philippines recently presented the case of a 36-year-old woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and double vision. A cranial computed tomography scan showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief.
The headaches occurred 2 weeks after the patient had received a cervical chiropractic manipulation (CM). Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma. The patient improved with conservative management.
The authors found 12 articles of SIH and CM after a systematic review of the literature. Eleven patients (90.9%) initially presented with orthostatic headaches. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had a complete recovery. Recovery was achieved within 14 days from the start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch, and one required neurosurgical intervention.
The authors concluded that this report highlights that a thorough history is warranted in patients with new-onset headaches. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first-line treatment.
As the authors rightly state, their case report does not stand alone. There are many more. In 2014, an Australian chiropractor published this review:
Background: Intracranial hypotension (IH) is caused by a leakage of cerebrospinal fluid (often from a tear in the dura) which commonly produces an orthostatic headache. It has been reported to occur after trivial cervical spine trauma including spinal manipulation. Some authors have recommended specifically questioning patients regarding any chiropractic spinal manipulation therapy (CSMT). Therefore, it is important to review the literature regarding chiropractic and IH.
Objective: To identify key factors that may increase the possibility of IH after CSMT.
Method: A systematic search of the Medline, Embase, Mantis and PubMed databases (from 1991 to 2011) was conducted for studies using the keywords chiropractic and IH. Each paper was reviewed to examine any description of the key factors for IH, the relationship or characteristics of treatment, and the significance of CSMT to IH. In addition, other items that were assessed included the presence of any risk factors, neck pain and headache.
Results: The search of the databases identified 39 papers that fulfilled initial search criteria, from which only eight case reports were relevant for review (after removal of duplicate papers or papers excluded after the abstract was reviewed). The key factors for IH (identified from the existing literature) were recent trauma, connective tissue disorders, or otherwise cases were reported as spontaneous. A detailed critique of these cases demonstrated that five of eight cases (63%) had non-chiropractic SMT (i.e. SMT technique typically used by medical practitioners). In addition, most cases (88%) had minimal or no discussion of the onset of the presenting symptoms prior to SMT and whether the onset may have indicated any contraindications to SMT. No case reports included information on recent trauma, changes in headache patterns or connective tissue disorders.
Discussion: Even though type of SMT often indicates that a chiropractor was not the practitioner that delivered the treatment, chiropractic is specifically cited as either the cause of IH or an important factor. There are so much missing data in the case reports that one cannot determine whether the practitioner was negligent (in clinical history taking) or whether the SMT procedure itself was poorly administered.
The new case report can, of course, be criticized for being not conclusive and for not allowing to firmly establish the cause of the adverse event. This is to a large extent due to the nature of case reports. Essentially, they provide a ‘signal’, and once the signal is loud enough, we need to act. In this case, action would mean to prohibit the intervention that is under suspicion and initiate conclusive research to prove or disprove a causal relationship.
This is how it’s done in most areas of healthcare … except, of course in so-called alternative medicine(SCAM). Here we do not even have the most basic tool to get to the bottom of the problem, namely a transparent post-marketing surveillance system that monitors the frequency of adverse events.
And whose responsibility is it to put such a system in place?
I let you guess.
