placebo
Homeopathic remedies are highly diluted formulations without proven clinical benefits, traditionally believed not to cause adverse events. Nonetheless, published literature reveals severe local and non–liver-related systemic side effects. Here is the first series on homeopathy-related severe drug-induced liver injury (DILI) from a single center.
A retrospective review of records from January 2019 to February 2022 identified 9 patients with liver injury attributed to homeopathic formulations. Competing causes were comprehensively excluded. Chemical analysis was performed on retrieved formulations using triple quadrupole gas chromatography-mass spectrometry and inductively coupled plasma atomic emission spectroscopy.
Males predominated with a median age of 54 years. The most typical clinical presentation was acute hepatitis, followed by acute or chronic liver failure. All patients developed jaundice, and ascites were notable in one-third of the patients. Five patients had underlying chronic liver disease. COVID-19 prevention was the most common indication for homeopathic use. Probable DILI was seen in 77.8%, and hepatocellular injury predominated (66.7%). Four (44.4%) patients died (3 with chronic liver disease) at a median follow-up of 194 days. Liver histopathology showed necrosis, portal and lobular neutrophilic inflammation, and eosinophilic infiltration with cholestasis. A total of 29 remedies were consumed between 9 patients, and 15 formulations were analyzed. Toxicology revealed industrial solvents, corticosteroids, antibiotics, sedatives, synthetic opioids, heavy metals, and toxic phyto-compounds, even in ‘supposed’ ultra-dilute formulations.
The authors concluded that homeopathic remedies potentially result in severe liver injury, leading to death in those with underlying liver disease. The use of mother tinctures, insufficient dilution, poor manufacturing practices, adulteration and contamination, and the presence of direct hepatotoxic herbals were the reasons for toxicity. Physicians, the public, and patients must realize that Homeopathic drugs are not ‘gentle placebos.’
The authors also cite our own work on this subject:
A detailed systematic review of homeopathic remedies-induced adverse events from published case reports and case series by Posadzski and colleagues showed that severe side effects, some leading to fatality, are possible with classic and unspecified homeopathic formulations. The total number of patients included was 1159, of which 1142 suffered adverse events directly related to homeopathy. The direct adverse events had acute pancreatitis, severe allergic reactions, arsenical keratosis, bullous pemphigoid, neurocognitive disorders, sudden cardiac arrest and coma, severe dyselectrolytemia, interstitial nephritis, kidney injury, thallium poisoning, syncopal attacks, and focal neurological deficits as well as movement disorders. Fatal events involved advanced renal failure requiring dialysis, toxic polyneuropathy, and quadriparesis. The duration of adverse events ranged from a few hours to 7 months, and 4 patients died. The authors state that in most cases, the mechanism of action for side effects of homeopathy involved allergic reactions or the presence of toxic substances—the use of strong mother tinctures, drug contaminants, adulterants, or poor manufacturing (incorrect dilutions).
When we published our paper back in 2012, it led to a seies of angry responses from defenders of homeopathy who claimed that one cannot ‘have the cake and eat it’; either homeopathic remedies are placebos and thus harmless, or they have effects and thus also side-effects, they claimed. As the new publication by Indian researchers yet again shows, they were mistaken. In fact, homeopathy is dangerous in more than one way:
- the homeopathic remedies can do harm if not diluted or wrongly manufactured;
- the homeopaths can do harm through their often wrong advice in health matters;
- homeopathy erodes rational thinking (as, for instance, the resopnses to our 2012 paper demonstrated).
This study aimed to compare the effects of cognitive functional therapy (CFT) and movement system impairment (MSI)-based treatment on pain intensity, disability, Kinesiophobia, and gait kinetics in patients with chronic non-specific low back pain (CNSLBP).
In a single-blind randomized clinical trial, the researchers randomly assigned 91 patients with CNSLBP into CFT (n = 45) and MSI-based treatment (n = 46) groups. An 8-week training intervention was given to both groups. The researchers measured the primary outcome, which was pain intensity (Numeric rating scale), and the secondary outcomes, including disability (Oswestry disability index), Kinesiophobia (Tampa Kinesiophobia Scale), and vertical ground reaction force (VGRF) parameters at self-selected and faster speed (Force distributor treadmill). They evaluated patients at baseline, at the end of the 8-week intervention (post-treatment), and six months after the first treatment. Mixed-model ANOVA was used to evaluate the effects of the interaction between time (baseline vs. post-treatment vs. six-month follow-up) and group (CFT vs. MSI-based treatment) on each measure.
CFT showed superiority over MSI-based treatment in reducing pain intensity (P < 0.001, Effect size (ES) = 2.41), ODI (P < 0.001, ES = 2.15), and Kinesiophobia (P < 0.001, ES = 2.47) at eight weeks. The CFT also produced greater improvement in VGRF parameters, at both self-selected (FPF[P < 0.001, ES = 3], SPF[P < 0.001, ES = 0.5], MSF[P < 0.001, ES = 0.67], WAR[P < 0.001, ES = 1.53], POR[P < 0.001, ES = 0.8]), and faster speed, FPF(P < 0.001, ES = 1.33, MSF(P < 0.001, ES = 0.57), WAR(P < 0.001, ES = 0.67), POR(P < 0.001, ES = 2.91)] than the MSI, except SPF(P < 0.001, ES = 0.0) at eight weeks.
The authors concluded that this study suggests that the CFT is associated with better results in clinical and cognitive characteristics than the MSI-based treatment for CNSLBP, and the researchers maintained the treatment effects at six-month follow-up. Also, This study achieved better improvements in gait kinetics in CFT. CTF seems to be an appropriate and applicable treatment in clinical setting.
To understand this study, we need to know what CFT and MSI exactly entailed. Here is the information that the authors provide:
Movement system impairment-based treatment
The movement system impairment-based treatment group received 11 sessions of MSI-based treatment over the 8 weeks for 60 min per session with a supervision of a native speaker experienced (above 5 years) physical therapist with the knowledge of MSI-based treatment. The researchers designed the MSI-based treatment uniquely for each patient based on the interview, clinical examination, and questionnaires, just like they did with the CFT intervention. First, they administered standardized tests to characterize changes in the patient’s low back pain symptoms, and then they modified the treatment to make it more specific based on the participant’s individual symptoms. Depending on the participant’s direction-specific low back pain classification, they performed the intervention following one of the five MSI subgroups namely [1] rotation, [2] extension, [3] flexion, [4] rotation with extension, and [5] rotation with flexion. Finally, Patients treated using the standardized MSI protocol as follows: [1] education regarding normal postures and movements such as sitting, walking, bending, standing, and lying down; [2] education regarding exercises to perform trunk movements as painlessly as possible; and [3] prescription of functional exercises to improve trunk movement [32].
Cognitive functional therapy
Cognitive functional therapy was prescribed for each patient in CFT group based the CFT protocol conducted by O’Sullivan et al. (2015). Patients received supervised 12 sessions of training over the 8-week period with 60 min per session provided with another physical therapist who had been trained in CFT treatment. In this protocol, a physical therapist with more than 5 years of experience conducted an interview and physical examination of the patients to determine their own unique training programs, considering modifiable cognitive, biopsychosocial, functional, and lifestyle behavior factors. The intervention consists of the following 3 main stages: [1] making sense of pain that is completely reflective, where physical therapist could use the context of the patient’s own story to provide a new understanding of their condition and question their old beliefs [2] exposure with control which is designed to normalize maladaptive or provocative movement and posture related to activities of daily living that is integrated into each patient’s functional impairments, including teaching how to relax trunk muscles, how to have normal body posture while sitting, lying, bending, lifting, moving, and standing, and how to avoid pain behaviors, which aims to break poor postural habits; and [3] lifestyle change which is investigating the influence of unhealthy lifestyles in the patient’s pain context. Assessing the individual’s body mass, nutrition, quality of sleep, levels of physical activity or sedentary lifestyle, smoking, and other factors via video calls. Identifying such lifestyle factors helped us to individually advise and design exercise programs, rebuild self-confidence and self-efficacy, promote changes in lifestyle, and design coping strategies.
I must admit that I am not fully convinced.
Firstly, the study was not large and we need – as the authors state – more evidence. Secondly, I am not sure that the results show CFT to be more effective that MSI. They might merely indicate 1) that the bulk of the improvement is due to non-specific effects (e.g. reression towards the mean, natural history of the condition, placebo) and 2) that CFT is less harmful than MSI.
My conclusion:
we need not just more but better evidence.
A ‘pragmatic, superiority, open-label, randomised controlled trial’ of sleep restriction therapy versus sleep hygiene has just been published in THE LANCET. Adults with insomnia disorder were recruited from 35 general practices across England and randomly assigned (1:1) using a web-based randomisation programme to either four sessions of nurse-delivered sleep restriction therapy plus a sleep hygiene booklet or a sleep hygiene booklet only. There was no restriction on usual care for either group. Outcomes were assessed at 3 months, 6 months, and 12 months. The primary endpoint was self-reported insomnia severity at 6 months measured with the insomnia severity index (ISI). The primary analysis included participants according to their allocated group and who contributed at least one outcome measurement. Cost-effectiveness was evaluated from the UK National Health Service and personal social services perspective and expressed in terms of incremental cost per quality-adjusted life year (QALY) gained. The trial was prospectively registered (ISRCTN42499563).
Between Aug 29, 2018, and March 23, 2020 the researchers randomly assigned 642 participants to sleep restriction therapy (n=321) or sleep hygiene (n=321). Mean age was 55·4 years (range 19–88), with 489 (76·2%) participants being female and 153 (23·8%) being male. 580 (90·3%) participants provided data for at least one outcome measurement. At 6 months, mean ISI score was 10·9 (SD 5·5) for sleep restriction therapy and 13·9 (5·2) for sleep hygiene (adjusted mean difference –3·05, 95% CI –3·83 to –2·28; p<0·0001; Cohen’s d –0·74), indicating that participants in the sleep restriction therapy group reported lower insomnia severity than the sleep hygiene group. The incremental cost per QALY gained was £2076, giving a 95·3% probability that treatment was cost-effective at a cost-effectiveness threshold of £20 000. Eight participants in each group had serious adverse events, none of which were judged to be related to intervention.
The authors concluded that brief nurse-delivered sleep restriction therapy in primary care reduces insomnia symptoms, is likely to be cost-effective, and has the potential to be widely implemented as a first-line treatment for insomnia disorder.
I am frankly amazed that this paper was published in a top journal, like THE LANCET. Let me explain why:
The verum treatment was delivered over four consecutive weeks, involving one brief session per week (two in-person sessions and two sessions over the phone). Session 1 introduced the rationale for sleep restriction therapy alongside a review of sleep diaries, helped participants to select bed and rise times, advised on management of daytime sleepiness (including implications for driving), and discussed barriers to and facilitators of implementation. Session 2, session 3, and session 4 involved reviewing progress, discussion of difficulties with implementation, and titration of the sleep schedule according to a sleep efficiency algorithm.
This means that the verum group received fairly extensive attention, while the control group did not. In other words, a host of non-specific effects are likely to have significantly influenced or even entirely determined the outcome. Despite this rather obvious limitation, the authors fail to discuss any of it. On the contrary, that claim that “we did a definitive test of whether brief sleep restriction therapy delivered in primary care is clinically effective and cost-effective.” This is, in my view, highly misleading and unworthy of THE LANCET. I suggest the conclusions of this trial should be re-formulated as follows:
The brief nurse-delivered sleep restriction, or the additional attention provided exclusively to the patients in the verum group, or a placebo-effect or some other non-specific effect reduced insomnia symptoms.
Alternatively, one could just conclude from this study that poor science can make it even into the best medical journals – a problem only too well known in the realm of so-called alternative medicine (SCAM).
I have to admit that I do not regularly read the DMZ, a German paper. In fact, until a minute ago, I did not know it existed. Nor do I know Anton Aeberhard. I saw his DMZ homeopathy article on the Internet and find it excellent; so much so that I translated parts of it for you:
… Because this pseudoscience is considered by some people to be an effective alternative to conventional medicine, it is important to understand the potential dangers and risks of homeopathy…
Homeopathy is based on the principle of the rule of similars and extreme dilution of substances. However, there is no scientific evidence that homeopathic remedies have any therapeutic effect beyond the placebo effect. Most studies that purport to show efficacy are methodologically flawed. Homeopathy contradicts fundamental principles of biology, chemistry, and physics. It is therefore irresponsible to consider this practice a legitimate medical treatment.
One of the greatest and real dangers of homeopathy is that it can cause people to refuse or delay effective medical treatments. By believing in homeopathic remedies, life-threatening conditions such as cancer, heart disease, or infections may not be treated appropriately. This can lead to worsening health conditions and increase the risk of complications or even death…
Conclusion I
Homeopathy is a pseudoscientific practice based on outdated principles and a lack of scientific evidence. The dangers of this practice should not be underestimated. It can cause people to reject or delay effective medical treatments, which can endanger their health and lives. It is important to make informed decisions about health care and to rely on evidence-based medicine to provide the best possible treatment and care.
Conclusion II.
Homeopathy is a joke.
________________________
Thank you Anton Aeberhard!
It is not often that we find a journalist who has the courage to defy the demand for ‘balance’. In the case of clear nonsensical issues, this demand becomes a demand for misleading people, a demand for FALSE balance!
When a journalist writes about the planet, he does not require a representative of the FLAT EARTH SOCIETY to add his views. Similarly, when someone writes about homeopathy, there is no need to interview the chair of a homeopaths’ association saying: “But we have 200 years of experience and we therefore know it works…”
It has been reported, at the German Medical Congress (DÄT) a year ago, that it was decided to delete the additional title of homeopathy from the model further training regulations of the German Medical Association. And Federal Health Minister Karl Lauterbach (SPD) tweeted applause: “Homeopathy has no place in modern medicine.”
Now the ‘ Bundesverband der Pharmaziestudierenden in Deutschland’ (BPhD), the German Pharmacists Organization, even goes a few steps further. The position paper distinguishes between evidence-based medicine (EBM) and unproven therapeutic methods. According to the BPhD, these include homeopathy, but also anthroposophy, traditional Chinese medicine, and traditional medicines.
Among other things, the BPhD is disturbed by the way homeopathy presents itself as an alternative, because an alternative means “a choice between two equally suitable possibilities” to achieve a goal, and this is not the case. Compared to evidence-based medicine (EBM), homeopathy is a “constructed, illusory concept” and “the principles of homeopathic teachings and principles” are to be rejected as “unscientific”. According to the BPhD, a designation as “alternative” for advertising purposes should no longer be allowed.
They would also like to see a demarcation from naturopathy; the clear distinction between homeopathy and phytopharmacy has been lacking up to now. The advertising attribute “natural” should therefore also be banned in order to prevent equalization in advertising, the position paper states.
Like doctors, pharmacy students point to the lack of proof of efficacy beyond the placebo effect. According to the BPhD, the dogma WER HEILT HAT RECHT, “he who heals is right” would “disregard all processes that work towards healing and glorify the result”. The “gold standard” of EBM – randomized, double-blind studies with placebo control – should in future also have to be fulfilled by homeopathic medicines, experience reports are not sufficient, it continues.
Homeopathic medicines are only registered as medicinal products without indication, which requires neither proof of efficacy nor clinical studies. The BPhD, therefore, demands that a warning be placed on the preparations that they have “no proven efficacy beyond the placebo effect”. Up to now, without this warning, patients have been “deceived about the efficacy”, and there is an “urgent need for detailed public information and counseling on homeopathy since its unjustified reputation poses a danger of not seeking treatment”. The BPhD also demands that the status of homeopathic medicines is withdrawn and that the pharmacy obligation for the preparations is abolished…
“In the health professions, no trivialization of unproven therapeutic procedures should be tolerated, as inadequate counseling or ignorance poses a danger to patients,” the BPhD said.
_________________________
When I first read this article – I translated and shortened it for those who cannot read German- I was truly dazzled. These are the suggestions that I have been making for around 20 years now, not specifically for Germany but for pharmacists in general. For many years, the Germans seemed the least likely to agree with me. But now they seem to be ahead of everyone else in Europe!
How come?
I suspect and hope that our recent initiative might have something to do with it.
Let’s hope that the pharmacists of other countries follow the German example.
A “null field” is a scientific field where there is nothing to discover and where observed associations are thus expected to simply reflect the magnitude of bias.
This analysis aimed to characterize a null field using a known example, homeopathy (a pseudoscientific medical approach based on using highly diluted substances), as a prototype. The researchers identified 50 randomized placebo-controlled trials of homeopathy interventions from highly cited meta-analyses. The primary outcome variable was the observed effect size in the studies. Variables related to study quality or impact were also extracted.
The mean effect size for homeopathy was 0.36 standard deviations (Hedges’ g; 95% confidence interval: 0.21, 0.51) better than placebo, which corresponds to an odds ratio of 1.94 (95% CI: 1.69, 2.23) in favor of homeopathy. 80% of studies had positive effect sizes (favoring homeopathy). The effect size was significantly correlated with citation counts from journals in the directory of open-access journals and CiteWatch. We identified common statistical errors in 25 studies.
The authors concluded that a null field like homeopathy can exhibit large effect sizes, high rates of favorable results, and high citation impact in the published scientific literature. Null fields may represent a useful negative control for the scientific process.
The paper is perhaps not the easiest to comprehend but once you got the idea, you will agree with me that it is BRILLIANT. I warmly recommend it to all fans of homeopathy – in fact, if I could I’d offer it to King Charles as a present for the coronation.
Its authors are among the most prominent medical epidemiologist of our time with affiliations that speak for themselves:
- Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA; Meta-Research Innovation Center at Stanford (METRICS), Stanford University, Stanford, CA, USA.
- 2Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA.
- 3Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA; Meta-Research Innovation Center at Stanford (METRICS), Stanford University, Stanford, CA, USA; Department of Medicine, Stanford University, Stanford, CA, USA; Department of Biomedical Data Science, Stanford University, Stanford, CA, USA; Department of Statistics, Stanford University, Stanford, CA, USA.
It is, of course, a pity that the article is behind a paywall – but fortunately, the senior author, John Ioannidis, published his email address together with the abstract: [email protected]. So, if you have trouble understanding the point of the analysis, I suggest you ask for a reprint to get your head around it. I promise it’s worth it.
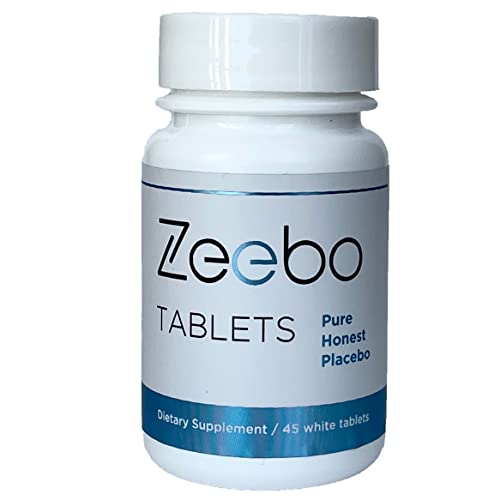
At first, I thought this was an ‘April fools’ joke. Then I looked at it a bit closer and realized that it seemed for real: Amazon is selling a placebo tablet. Here is how it is advertised:
- Honest Placebo Tablets by Zeebo Effect, inert ingredients, halal & kosher
- Focus on symptom relief, concentration, clarity, energy, calm, sleep
- Ze logo on each tablet, the original honest placebo brand trusted since 2014
- Randomized Controlled Trials with Zeebo Published in Journal for Pain, Nature, American Family Physician
- Each bottle is sealed with a transparent, tamper-proof neckband
Zeebo Tablets – Honest placebo tablets (white, round, 250mg each) are designed to help you create a safe placebo experience. Zeebo comes with the Ze logo on each tablet. Zeebo is made from an inert, natural fiber. Vegan, free of sugar or dyes. When it comes to Zeebo, You are the active ingredient. Users of Zeebo Tablets know they are taking a placebo containing only inert ingredients. Zeebo Tablets are taken intentionally obtain stress and pain relief, to release tension, irritability and nervousness, to help with calm and sleep serving as a sleep aid. Some of our customers take Zeebo Tablets to solicit placebo effects for increased mental focus, clarity, concentration, test performance and to sustain higher energy levels during physical exercise. Zeebo tablets are pure placebo, they are non-drowsy, non-homeopathic. There are no known interactions between Zeebo Placebo Tablets and other medications or supplements. Do not use Zeebo to delay or replace medical treatment. Visit zeeboeffect.com to learn about Zeebo. Look for the ebook The Placebo Cure to find out more about how to create your own Honest Placebo experience.
Take as needed. You may or may not respond to placebo. Do not use Zeebo to replace or delay medical treatment. Use Zeebo without deceit.*
* These statements have not been evaluated by the FDA. This product is not intended to diagnose, cure, treat, or prevent any disease.
Statements regarding dietary supplements have not been evaluated by the FDA and are not intended to diagnose, treat, cure, or prevent any disease or health condition.
Zeebo Tablets are an ethical placebo. People take it knowing it is a placebo. Take it without self-deceit. Zeebo is not made to look like any other ingestible. In fact, we think that the Zeebo branding can help enhance the experience. Have a look into ethical placebo or honest placebo studies. You will find a lot of research there, published in the journals Nature, Pain, for example. No need to trick yourself.
_________________________
After reading all this, I am again not entirely sure whether this is a hoax. If it is, I failed to get the fun of it. If it isn’t, there might be reasons for concern. When a placebo was marketed, a few years ago, THE GUARDIAN published opinions about the idea:
Jennifer Buettner, whose company Efficacy is marketing the placebo, says it can stimulate “the body’s ability to repair itself and the miracle power of the brain”. She said the company planned to distribute the pills, which cost £3 for 50, in the UK. “When drugs are not needed and the patient still thinks that medicine would help, we believe that the placebo effect can work,” she said.
But Dr Clare Gerada, vice-chair of the Royal College of GPs, described the pill as “medicalising love”, adding: “This placebo disempowers parents. It is telling them that unless you give your children this pill there’s nothing else.” Douglas Kamerow, associate editor of the British Medical Journal, said giving placebos to children was a “deeply bad idea”. Writing in the latest edition of the journal, he said: “The problems are numerous. Firstly, whom are we treating here, children or their parents?” He added that if parents used placebos to comfort their children they were teaching them that tablets are the answer for all life’s aches and pains.
As we have seen previously, the evidence on ‘open placebos’ is less impressive than many think. It makes me wonder whether the sale of placebo tablets is a good idea.
WHAT DO YOU THINK?
‘Agoro’ is a German (all texts are my translations from German) website that claims this:
“We specialize in alternative methods of treatment from the field of natural medicine. Our mission is to ensure that the ancient wisdom of our grandparents and ancestors is not forgotten.”
Unsurprisingly, this subject interests me. In particular, I was fascinated by an article entitled
Nux vomica Globuli in der Homöopathie
Nux Vomica in homeopathy
Nux vomica is (after arnica) amongst the most popular remedies in homeopathy. Therefore, we should all be keen to learn all about it.
Here is the translation of this article:
Nux vomica is one of the homeopathic remedies that you can get in all pharmacies. It can help you with various diseases, such as stomach pain. You can also use this homeopathic remedy for nausea and heartburn. You can buy it in the city pharmacies, but you can also make it easy for yourself and use the online pharmacy for globules. Here you will be well advised on the dosage of homeopathic remedies. Similarly, you can also contact the homeopath or naturopath for good advice.
Nux vomica is a remedy derived from the medicinal plant nux vomica. You can use the homeopathic remedy in the potencies D6 and D12. In some cases, it can be recommended to you also in C6, C12, or C30.
You can use the homeopathic remedy in many ways, including for constipation or exhaustion. You will find out which dosage you can take if you consult a professional. In this way, you will be recommended the appropriate potency to experience help from it.
It is crucial that you always seek advice before taking the remedy. As already mentioned, you can use several contact points for this. Whether it is the pharmacy, the naturopath, or the homeopath. In addition, there are many family doctors who now also use homeopathy and could recommend you the appropriate dosage. The consultation is important in any case because the homeopathy must be adapted to your complaints. Otherwise, the remedy will not work or will not work properly.
If you want to use the remedy for yourself, you always need patience. Homeopathic remedies need a little time to work, that is their only disadvantage. How long this always depends on the person and the remedy. Sometimes it takes only a few hours, sometimes a few days or weeks. You can also get advice on this.
Indications for nux vomica
Stomach and intestinal problems
You can use the remedy for you in case of abdominal pain, mild biliousness, and various stomach and intestinal problems. The remedy can also be of great help for nausea, flatulence, nausea, and constipation.
Headaches and migraines
The remedy Nux vomica can help you if you suffer from headaches that are located just above the eye. It can also help you with migraines. Even with a hangover, the remedy could help.
Moods
If you suffer from autumn depression or are often easily frustrated, you can use the remedy.
_______________________
Yes, I do get easily frustrated with texts like this!
But I doubt that nux vomica can help me with this or any other problem.
Some might say that doubting is not good enough, evidence is needed!
I agree but was unable to find sound evidence to show that homeopathic nux vomica was better than a placebo for any condition (in case any of our regular defenders of homeopathy know more, please let me know). On the contrary, I only found studies that suggested its ineffectiveness. Here is an example:
In a monocenter prospective randomized double-blind clinical trial the efficacy of homeopathic treatment was investigated on children with adenoid vegetations justifying an operation. Patients were treated with either homeopathic remedies such as Nux vomica D200, Okoubaka D3, Tuberculinum D200, Barium jodatum D4 and Barium jodatum D6 or with placebo. The duration of the study for each patient was 3 months. Examination of the ears using a microscope, rhinoscopy, stomatoscopy and pharyngoscopy, as well as tympanometry and audiometry were performed after 4, 8 and 12 weeks. Out of a total of 97 children studied between the ages of 4 to 10 years 82 could be analyzed. At the end of the study no operation was required in 70.7% of the placebo-treated children and in 78.1% of the children treated with homeopathic preparations. These results show no statistical significance.
So, where does that leave us in relation to the “ancient wisdom of our grandparents and ancestors“? I fear, that this story shows yet again that, when it comes to homeopathy, the scrutiny of ancient wisdom quickly turns it into old bullshit.
Acupuncture is a panacea, we are often told.
But is it true?
Of course not!
This study was aimed at evaluating the effect of acupuncture on myelosuppression and quality of life in women with breast cancer during treatment with anthracyclines (ANT).
Women with an indication for ANT chemotherapy were randomized into two groups:
- the acupuncture group (AG) was submitted to an acupuncture intervention, starting before the first chemotherapy infusion, and continuing throughout the treatment;
- the control group (CG) received no acupuncture.
A quality of life questionnaire (FACT-G) and peripheral blood levels of the participants were evaluated before and at the end of treatment.
A total of 26 women were randomized into 2 groups: AG (10) and CG (16). Of these, 26.9% had a dense dose indication according to the service’s protocol for the administration of granulocyte-stimulating factor (G-CSF) from the first cycle, not participating in the analysis. The need for secondary prophylaxis with G-CSF occurred in 72.7% in the control group versus 12% in the acupuncture group. Regarding quality of life (QoL), it was observed that the groups did not initially differ from each other. At the end of the treatment, there was a significant difference in the AG for the physical (GP) (p-value=0.011), social/family (GS) (p-value=0.018), and functional (GF) (p-value=0.010) domains, regarding the initial and final FACT-G showed a difference between the groups, where the GA average at the end rose from 80.68 to 90.12 (p-value = 0.004) and in the CG the average dropped from 81.95 to 70.59 (p-value=0.003).
The authors concluded that acupuncture was efficient in the secondary prophylaxis of myelosuppression during chemotherapy and the quality of life of women during treatment has increased.
My interpretation of these results is quite different from that of the authors.
Please let me explain.
The improvement of the quality of life can easily be explained via a placebo effect; acupuncture itself has not necessarily any part in it. But what about the effect on the bone marrow? Might it too be due to a placebo response, or the additional attention? Probably not.
Does that mean that this study proves a definite positive effect of acupuncture?
No!
Why not?
Because firstly the study was far too small for allowing such a far-reaching conclusion, and secondly one would need independent confirmation before accepting such a far-reaching conclusion.
This systematic review and meta-analysis aimed to evaluate the effectiveness and safety of Chinese herbal medicine (CHM) combined with Western medicine (WM) in comparison with WM in reducing systolic and diastolic blood pressure for patients with primary hypertension (PHTN).
Various literature searches located a total of 29 studies that included 2623 patients. The results showed that the clinical effectiveness in the treatment of hypertension with CHM+WM was considerably higher than that with WM alone, clinical effective (RR 1.23, 95% CI [1.17, 1.30], P < 0.00001), and markedly effective (ME) in the patients (RR 1.66, 95% CI [1.52, 1.80], and P < 0.00001). Random effect in SBP (MD 7.91 mmHg,[6.00, 983], P < 0.00001) and DBP (MD 5.46 mmHg, [3.88, 6.43], P < 0.00001), a subgroup analysis was carried out based on the type of intervention, duration of treatment, and CHM formulas that showed significance. Furthermore, no severe side effects were reported, and no patients stopped treatment or withdrawal due to any severe adverse events.
The authors concluded that compared to WM alone, the therapeutic effectiveness of CHM combined with WM is significantly improved in the treatment of hypertension. Additionally, CHM with WM may safely and efficiently lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) in individuals with PHTN. However, rigorous randomized controlled trials with a large sample, high quality, long duration of treatment, and follow-up are recommended to strengthen this clinical evidence.
The authors can boast of an impressive list of affiliations:
- 1Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China; School of Pharmacy, Lebanese International University, 18644, Sana’a, Yemen.
- 2Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 3Key Laboratory of Chinese Materia Medica, Ministry of Education of Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 4Department of Urology, Affiliated Hospital of Qingdao Binhai University, Qingdao, Shandong, China.
- 5Department of Respiratory Diseases, Shandong Second Provincial General Hospital, Shandong University, Shandong, China.
- 6Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China. Electronic address: [email protected].
Impressive in the sense of being impressively prone to bias, particularly knowing that ~80% of Chinese research findings have been shown to be fabricated and considering that Chinese authors as good as never publish anything negative about TCM.
But perhaps you still believe that the results reported here are 100% true? In this case, I might even agree with you. The reason is that the authors demonstrate in exemplary fashion what I have been saying so often before:
Blood pressure is one of the many endpoints that are highly prone to placebo effects. Therefore, even the addition of an ineffective CHM to WM would lower blood pressure more effectively than WM alone.
But there is a third way of explaining the findings of this review: some herbal remedies might actually have a hypotensive effect. The trouble is that this review does come not even close to telling us which.