patient choice
A German paper reported the following horrific story about a Heilpraktiker, an alternative practitioner without a medical degree:
Starting July 7, Torben K. (46) from Solingen will have to answer to the Wuppertal Regional Court. The Heilpraktiker is said to have injected silicone oil into the penis and testicles of a man († 32) at his request. Shortly thereafter, the patient developed health problems and later died.
The prosecution accuses the Heilpraktiker from Solingen of bodily injury resulting in death and violation of the Heilpraktikergesetz.
According to the report, the victim had traveled to Solingen in June 2019, where the defendant had given him the injection in his apartment.
Back home, the 32-year-old patient suddenly developed shortness of breath, had to be hospitalized, then transferred to the university hospital in Giessen. Seven months after the injection, he is dead. According to the indictment, the patient suffered multiple organ failure as a result of blood poisoning.
Three days of trial are scheduled. The defendant faces up to 15 years in prison.
_________________________
I had never heard of intra-testicular injections. So, I did a Medline search and found just two papers of the procedure in human patients:
Blunt trauma is the most common mechanism of injury to the scrotum and testicle. Surgical exploration with primary repair, hematoma evacuation, and de-torsion are common surgical interventions. A 20-year-old male with no previous medical history presented after a high-speed motor vehicle collision. Ultrasonography demonstrated heterogeneous changes of the tunica albuginea and decreased arterial flow to bilateral testicles. He was subsequently taken to the operating room for surgical exploration, which revealed bilateral mottled testes with questionable viability. Papaverine was injected into each testicle, which resulted in visibly increased perfusion and subsequent preservation of the testicles. Conclusion: Current evidence on the use of papaverine is isolated to testicular torsion. Additional research should be conducted on the use of papaverine in blunt testicular trauma. Papaverine injection may be a valuable treatment option when inadequate perfusion is observed intra-operatively.
No 2:
Purpose: We describe a simple technique to deliver local anaesthetic for percutaneous testis biopsies.
Materials and methods: With the testis held firmly, a 25 gage needle is used to inject lidocaine, without epinephrine, into the skin and dartos superficial to the testis, then the needle is advanced through the tunica albuginea and 0.5 mL to 1.0 mL of lidocaine is injected directly into the testis. The testis becomes slightly more turgid with the injection. A percutaneous biopsy is then immediately performed.
Results: Intra-testicular lidocaine, (without the need of a cord block or any sedation) was used on a total of 45 consecutive patients having percutaneous testicular biopsies. Procedure time was short (averages less than 5 minutes) and anaesthesia was profound. There was no change in the number of seminiferous tubules for evaluation compared to biopsies on men using a cord block. Only 1/45 men had a post-procedure testicular hematoma (this resolved in 4 weeks).
Conclusions: Intra-testicular lidocaine appears to be a simple, rapid and safe method to provide anaesthesia for a percutaneous testis biopsy.
All the other papers on intra-testicular injections were about animal experiments, mostly for exploring means of castration. This renders the above case even more unusual. The Heilpraktiker’s defense might stress that the patient wanted the treatment. That may be so but is it a valid excuse? No, of course not. In my view – and I am just a medic, not a lawyer – the Heilpraktiker is responsible for the treatment regardless of how much the patient insisted on it.
I missed this paper when it first came out in 2022. Yet, it seems potentially quite important and I, therefore, feel like discussing it here:
President of the UNESCO Committee on Bioethics Stefan Semplici called on the governments of all countries to ensure free and wider access of their citizens to alternative medicine and pay for this therapy through health insurance. Alternative medicine based on tradition – traditional medicine, in many poor countries is the only treatment option for the population. In developed countries, and especially in China and India, it enjoys well-deserved prestige (for example, acupuncture and herbal medicine) and is often integrated into the public health system.
The International Committee on Bioethics of UNESCO announced the recognition of these alternative therapies as an option for medical practice and, at the same time, as part of the identity of the cultural traditions of various nations. The UNESCO Universal Declaration on Bioethics and Human Rights includes the right to the highest attainable standard of health (Article 14), the right to respect for pluralism and cultural diversity (Article 12) and traditional knowledge (Article 17). The purpose of this document is to establish criteria for the respect and acceptability of different types of medicine without compromising the assurance of quality and patient safety that is essential in all treatments.
In order to adapt the traditions of traditional therapies to advances in medicine, this international organization calls on governments and the scientific community to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety and develop therapeutic standards and protocols for integrating traditional medicine into healthcare system. The UNESCO International Bioethics Committee believes that these methods should be seen as complementary to modern medicine, and not just an alternative to it.
_________________________
The United Nations Educational, Scientific and Cultural Organization (UNESCO) is an agency of the United Nations aimed at promoting world peace and security through international cooperation in education, arts, sciences, and culture. UNESCO’s International Bioethics Committee (IBC) is a body of 36 independent experts that follows progress in the life sciences and its applications in order to ensure respect for human dignity and freedom.
I have to say that I rarely have seen an announcement in so-called alternative medicine (SCAM) that is more confusing and less well thought through. The UNESCO Committee on Bioethics wants:
- alternative therapies as an option for medical practice,
- the highest attainable standard of health,
- to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety.
When I first read these lines, I asked myself: who on earth wrote such nonsense? It was certainly not written by someone who understands healthcare, SCAM, and evidence-based medicine.
As discussed almost permanently on this blog, most forms of SCAM have not been shown to generate more good than harm. This means that employing them ‘as an option in medical practice’ cannot possibly produce ‘the highest attainable standards of health’. In fact, the UNESCO plan would lead to lower not higher standards. How can a committee on bioethics not realize that this is profoundly unethical?
Collaboration with practitioners of alternative therapies to evaluate SCAM’s effectiveness and safety sounds a bit more reasonable. It ignores, however, that tons of evidence already exist but fail to be positive. Why do these experts in bioethics not advocate to first make a sober assessment of the published literature?
I must say that the initiative of the UNESCO Committee on Bioethics puzzles me a lot and disturbs me even more.
I’d be keen to learn what you think of it.
The current secondary analysis based on the WHO database (VigiBase) of individual case safety reports (ICSRs) focuses on the suspected cutaneous adverse drug reactions (ADRs) linked to traditional medicines (TMs).
All the ICSRs reported between 1st January 2016 and 30th June 2021 from the UN Asia region in VigiBase where at least one TM was suspected to cause cutaneous ADRs were included in the study. Data regarding demographic details, suspected drug, adverse reaction as per MedDRA term, the seriousness of the reaction, de-challenge, re-challenge, and clinical outcome for suspected cutaneous ADRs associated with TM were obtained from VigiBase and analyzed for frequency of reported events and suspected medicines.
A total of 3,523 ICSRs with 5,761 ADRs related to “skin and subcutaneous tissue disorders” were included in the analysis. Amongst these, 6.8% of ICSRs were reported as serious.
The most common ADRs were:
- pruritus (29.6%),
- rash (20.3%),
- urticaria (18.9%),
- hyperhidrosis (3.3%).
Artemisia argyi H.Lév. and Vaniot. (14.9%), Ginkgo biloba L. (5.1%), Vitis vinifera L. (4%), Vitex agnus-castus L. (3.8%), Silybum marianum (L.), Gaertn (3.5%), and Viscus album L. (2.7%) were some commonly suspected TMs for cutaneous ADRs. There were 46 cases of Stevens-Johnson syndrome and toxic epidermal necrolysis reported with TMs during the study period. Death was reported in 5 ICSRs.
The authors concluded that TMs are linked with various cutaneous ADRS ranging from pruritus to toxic epidermal necrolysis which may have serious consequences. TMs listed as suspected offending agents in this analysis, should be kept in mind while dealing with suspected cutaneous ADRs. Clinicians should be more vigilant in detecting and reporting events associated with TMs.
Herbal remedies have a reputation for being time-tested, gentle, harmless, and benign. Reports such as this one might make us doubt this cliche. More importantly, they should force us to ask whether the remedy we are tempted to try truly does generate more good than harm. In most instances, I fear, the answer is not positive.
The ‘American Heart Association News’ recently reported the case of a 33-year-old woman who suffered a stroke after consulting a chiropractor. I take the liberty of reproducing sections of this article:
Kate Adamson liked exercising so much, her goal was to become a fitness trainer. She grew up in New Zealand playing golf and later, living in California, she worked out often while raising her two young daughters. Although she was healthy and ate well, she had occasional migraines. At age 33, they were getting worse and more frequent. One week, she had the worst headache of her life. It went on for days. She wasn’t sleeping well and got up early to take a shower. She felt a wave of dizziness. Her left side seemed to collapse. Adamson made her way down to the edge of the tub to rest. She was able to return to bed, where she woke up her husband, Steven Klugman. “I need help now,” she said.
Her next memory was seeing paramedics rushing into the house while her 3-year-old daughter, Stephanie, was in the arms of a neighbor. Rachel, her other daughter, then 18 months old, was still asleep. When she woke up in the hospital, Adamson found herself surrounded by doctors. Klugman was by her side. She could see them, hear them and understand them. But she could not move or react.
Doctors told Klugman that his wife had experienced a massive brain stem stroke. It was later thought to be related to neck manipulations she had received from a chiropractor for the migraines. The stroke resulted in what’s known as locked-in syndrome, a disorder of the nervous system. She was paralyzed except for the muscles that control eye movement. Adamson realized she could answer yes-or-no questions by blinking her eyes.
Klugman was told that Adamson had a very minimal chance of recovery. She was put on a ventilator to breathe, given nutrition through a feeding tube, and had to use a catheter. She learned to coordinate eye movements to an alphabet chart. This enabled her to make short sentences. “Am I going to die?” she asked one of her doctors. “No, we’re going to get you into rehab,” he said.
Adamson stayed in the ICU on life support for 70 days before being transferred to an acute rehabilitation facility. She could barely move a finger, but that small bit of progress gave her hope. In rehab, she slowly started to regain use of her right side; her left side remained paralyzed. Therapists taught her to swallow and to speak. She had to relearn to blow her nose, use the toilet and tie her shoes.
She was particularly fond of a social worker named Amy who would incorporate therapy exercises into visits with her children, such as bubble blowing to help her breathing. Amy, who Adamson became friends with, also helped the children adjust to seeing their mother in a wheelchair.
Adamson changed her dream job from fitness trainer to hospital social worker. She left rehab three and a half months later, still in a wheelchair but able to breathe, eat and use the toilet on her own. She continued outpatient rehab for another year. She assumed her left side would improve as her right side did. But it remained paralyzed. She would need to use a brace on her left leg to walk and couldn’t use her left arm and hand. Still, two years after the stroke, which happened in 1995, Adamson was able to drive with a few equipment modifications…
In 2018, Adamson reached another milestone. She graduated with a master’s degree in social work; she’d started college in 2011 at age 49. “It wasn’t easy going to school. I just had to take it a day at a time, a semester at a time,” she said. “The stroke has taught me I can walk through anything.” …
Now 60, she works with renal transplant and pulmonary patients, helping coordinate their services and care with the rest of the medical team at Vanderbilt University Medical Center. “Knowing that you’re making a difference in somebody’s life is very satisfying. It takes me back to when I was a patient – I’m always looking at how I would want to be treated,” she said. “I’ve really come full circle.”
Adamson has adapted to doing things one-handed in a two-handed world, such as cooking and tying her shoes. She also walks with a cane. To stay in shape, she works with a trainer doing functional exercises and strength training. She has a special glove that pulls her left hand into a fist, allowing her to use a rowing machine and stationary bike….
Adamson is especially determined when it comes to helping her patients. “I work really hard to be an example to them, to show that we are all capable of going through difficult life challenges while still maintaining a positive attitude and making a difference in the world.”
________________________
What can we learn from this story?
Mainly two things, in my view:
- We probably should avoid chiropractors and certainly not allow them to manipulate our necks. I know, chiros will say that the case proves nothing. I agree, it does not prove anything, but the mere suspicion that the lock-in syndrome was caused by a stroke that, in turn, was due to upper spinal manipulation plus the plethora of cases where causality is much clearer are, I think, enough to issue that caution.
- Having been in rehab medicine for much of my early career, I feel it is good to occasionally point out how important this sector often neglected part of healthcare can be. Rehab medicine has been a sensible form of multidisciplinary, integrative healthcare long before the enthusiasts of so-called alternative medicine jumped on the integrative bandwagon.
A regional court in the Bavarian city of Ingolstadt has sentenced a natural healing practitioner, i.e. Heilpraktiker, and her supplier to jail for fraud. The pair were found to have deceived patients suffering from terminal cancer to put their faith in a remedy that they touted as a miracle cure. The practitioner was jailed for three years for her part in the scam, while the supplier was sentenced to six years and nine months.
The defendants in the case were a 57-year-old Heilpraktiker from the town of Schrobenhausen and a 68-year-old businessman from Ingolstadt who supplied the preparation. Both defendants were said to have promoted the remedy BG-Mun, saying that it could quickly cure cancer without any evidence of this being the case.
The court heard that patients paid up to €6,000 for the remedy. According to the court, the practitioner had boasted of “great successes” with one patient, Sabine H., who had acquired the remedy and stopped her course of chemotherapy at the defendant’s advice. The court was told that the pair would have known at this point that the substance would have no effect. A drug researcher from the University of Bremen had described the defendants’ actions as “profiteering” from the suffering of desperate patients. “Ultimately, it is a hustle against those who really are clutching at straws when it comes to their illness,” he said.
Even after the death of former patients, the defendants continued to promote their bogus remedy, the prosecutor emphasized. The Heilpraktiker advised several patients to rely exclusively on BG-Mun for their treatment and to discontinue the chemotherapy advised by orthodox medicine.
The defense lawyers demanded a comprehensive acquittal for both clients. The central argument: Both the Heilpraktiker and the entrepreneur had tried BG-Mun on themselves, found it helpful and therefore believed in its effect. The two had therefore acted without any intention to deceive. Without an intention to deceive, however, there is no fraud. In addition, BG-Mun had only ever been advertised as a “component in an overall therapy” and never as a sole medicine. According to the defense lawyers, BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. In the opinion of the lawyers, empirical effectiveness, therefore, does not have to be proven. The public prosecutor, on the other hand, quoted experts who say that BG-Mun is a protein solution that has no effect whatsoever against cancer and is also not approved as a medicine.
Elsewhere it had been reported that the court also dealt with the charge of misuse of title, specifically with the fact that the Heilpraktiker used the title of professor orally and also on advertising flyers. The title of professor comes from an educational institution in the USA, which itself is not recognized as a university in the USA. The German Conference of Ministers of Education and Cultural Affairs does not recognize this title in this country and calls it a “decorative certificate”.
____________________
What I find particularly fascinating about this case is that the defense lawyers claimed, that BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. This type of argument crops up regularly when quacks go to trial. I am not a legal expert and can thus only judge it from a medical point of view. Medically speaking, I find it hard to think of an argument that is more ridiculous than this one. To me, it seems like saying: “I am a charlatan and therefore you cannot judge by by the standards of regular healthcare.”
The second argument of the defense is hardy any better: “I was convinced that it worked, therefore, my prescribing it was honest and correct.” Imagine a doctor saying such nonsense! The argument makes a mockery of evidence by replacing it with belief. I am glad that the German court did not fall for such pseudo-arguments.
This survey evaluated the attitude of healthcare professionals toward the use of so-called alternative medicine (SCAM) to improve current care. A questionnaire on the current practice and opinions about SCAM use was sent to healthcare professionals in Amsterdam UMC, who work for the department of hematology or oncology. Oncologists, hematologists, residents, (specialized) nurses, dieticians, (hospital)pharmacists, and pharmacy technicians were asked to participate.
Among eligible healthcare professionals, 77 responded to the questionnaire (34%). Overall, 87% of healthcare
professionals indicated it is important to be aware of their patient’s SCAM use, and all find the potential of drug–herb interactions important. However, more than half of the healthcare professionals inquire about the patient’s SCAM use infrequently. In addition, only 15% of the healthcare professionals stated they had sufficient knowledge of SCAM to advise patients on their use of SCAM.
The authors concluded that healthcare professionals are aware of the potential risks of SCAM use in combination with anti-cancer treatment. However, SCAM use is not yet discussed with every patient. This may be due to healthcare professionals’ lack of knowledge about SCAM.
This survey would in itself be fairly irrelevant; it employed only a tiny convenience sample and its findings cannot be generalized. Yet, it produced results that have been shown dozens of times before, and it might therefore be a good idea to remind ourselves of their relevance and implications.
- Patients use SCAM whether we want it or not.
- Contrary to what is often said, SCAM is not harmless.
- Therefore conventional healthcare professionals need to know about their patients’ SCAM use.
- To find out, healthcare professionals need to ask specific questions about SCAM.
- Next, they must advise their patients responsibly (this is an ethical obligation, not a choice).
- In order to do that they need to learn the essentials about SCAM.
- Failing to do this means failing their patients.
Numerous qualitative studies and a few quantitative studies have linked vaccine hesitancy or refusal with the belief in the efficacy of so-called alternative medicine (SCAM). Yet, large-scale data on this topic are scarce. In this study, the French researchers investigated the factors associated with the coverage rates of seven childhood vaccines or vaccine groups in the ninety-six metropolitan French departments. One of the factors investigated was the local interest in SCAM. In order to assess this interest, they built an Alternative Medicine Index based on departmental internet searches regarding SCAM—internet searches being a reliable indicator of the public’s actual interest in a given topic. They then conducted multiple regression analyses, which showed that this Index is a significant explanatory factor for the departmental variance in vaccination coverage rates, exceeding in importance the effect of other relevant local sociodemographic factors.
A further recent study from France adds to the picture. It presents the results of a survey conducted in July 2021 among a representative sample of the French mainland adult population (n = 3087). Using cluster analysis, the researchers identified five profiles of SCAM attitudes and found that even among the most pro-SCAM group, very few respondents disagreed with the idea that SCAM should only be used as a complement to conventional medicine. They then compared these SCAM attitudes to vaccine attitudes. Attitudes to SCAM had a distinct impact as well as a combined effect on attitudes to different vaccines and vaccines in general. They found that:
- attitudes to SCAM provide a very limited explanation of vaccine hesitancy;
- among the hesitant, pro-SCAM attitudes are often combined with other traits associated with vaccine hesitancy such as distrust of health agencies, radical political preferences, and low income.
Both SCAM endorsement and vaccine hesitancy are more prevalent among the socially disadvantaged. Drawing on these results, the researchers argue that, to better understand the relationship between SCAM and vaccine hesitancy, it is necessary to look at how both can reflect a lack of access and recourse to mainstream medicine and distrust of public institutions.
 The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- Sorry, I was wrong about homeopathy and vaccination
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
What seems fairly clear to me is that a cross-correlation exists: an attitude against modern medicine and the ‘scientific establishment’ determines both the enthusiasm for SCAM and the aversion to vaccination. What is, however, far from clear to me is what we could do about it.
Yes, better education seems important – and that’s precisely what I aim at achieving with this blog. Sadly, judging from some of the comments we receive, it does not seem crowned with much success.
Any other ideas?
Semen retention is a so-called alternative medicine (SCAM) that involves intentionally avoiding ejaculating. A person can do this by abstaining from any sexual activity, stopping before the point of ejaculation, or teaching themselves to orgasm without ejaculating.
Although this practice may seem new, this is likely only due to recent internet popularity. In fact, semen retention is an ancient practice, believed to boost male physical and spiritual energy.
Some other names for semen retention include:
- coitus reservatus
- seminal conservation
- sexual continence
It is also known as or included in practices called:
- karezza (Italian)
- maithuna (Hindu Tantra)
- sahaja (Hindu Yoga)
- tantra (Hinduism and Buddhism)
- cai Yin pu Yang and cai Yang pu Yin (Taoist)
Semen retention is said to be good for a range of things:
Mental health
- increased motivation
- improved energy and focus
- more self-confidence
- reduced anxiety
- better memory
- improved concentration
Physical health
- clearer skin
- increased testosterone
- more weight loss
- increased muscle mass
- physical rejuvenation
- a deeper voice
Spiritual health
- a greater sense of purpose
- stronger or deeper emotional bonds in relationships
- a stronger sense of overall harmony
________________________
Yes, I agree, this sounds weird!
But is there any evidence?
Yes, e.g.:
Males of some species use mate retention behavior and investment in ejaculate quality as anti-cuckoldry tactics concurrently while others do so in a compensatory fashion. Leivers, Rhodes, and Simmons (2014) reported that men who performed mate retention less frequently produced higher-quality ejaculates, suggesting that humans use these tactics compensatorily. We conducted a conceptual replication of this research in a sample of 41 men (18-33 years; M = 23.33; SD = 3.60). By self-report, participants had not had a vasectomy and had never sought infertility treatment. We controlled for several covariates known to affect ejaculate quality (e.g., abstinence duration before providing an ejaculate) and found no statistically significant relationships between mate retention behavior and four components of ejaculate quality: sperm velocity, sperm concentration, slow motility, and ejaculate volume. The present results provide little support for the hypothesis that human males deploy mate retention behavior and ejaculate quality investment compensatorily. We discuss the limitations of this study and highlight the need for research to address questions about the nature of anti-cuckoldry tactic deployment in humans, especially concerning investment in ejaculate quality.
In species where females mate with multiple males, the sperm from these males must compete to fertilise available ova. Sexual selection from sperm competition is expected to favor opposing adaptations in males that function either in the avoidance of sperm competition (by guarding females from rival males) or in the engagement in sperm competition (by increased expenditure on the ejaculate). The extent to which males may adjust the relative use of these opposing tactics has been relatively neglected. Where males can successfully avoid sperm competition from rivals, one might expect a decrease in their expenditure on tactics for the engagement in sperm competition and vice versa. In this study, we examine the relationship between mate guarding and ejaculate quality using humans as an empirical model. We found that men who performed fewer mate guarding behaviors produced higher quality ejaculates, having a greater concentration of sperm, a higher percentage of motile sperm and sperm that swam faster and less erratically. These effects were found independent of lifestyle factors or factors related to male quality. Our findings suggest that male expenditure on mate guarding and on the ejaculate may represent alternative routes to paternity assurance in humans.
The uncritical application of western psychiatric concepts in non-western societies resulting in culturally invalid psychiatric syndromes, have been extensively documented. Such instances are considered ‘category errors’. In contrast, ‘reverse category errors’ although theoretically postulated, have never been empirically demonstrated. Diagnostic criteria of an established South Asian culture specific neurosis, Dhāt syndrome, were deployed by a psychiatrist of South Asian origin, amongst 47 white Britons in London, UK, presenting for the first time with a clinic diagnosis of ICD-9 Depressive Neurosis (Dysthymic Disroder, ICD-11). The proceedure yielded a new disorder, Semen Retention Syndrome. Based on narrative accounts and quantitative scores on the Hamilton Depression Rating Scale, the evidence suggests that a significant subset of white British subjects diagnosed with Dysthymic Disorder, may in fact be expressing a psychological variation of a previously unknown local White British somatisation phenomena labelled Semen Retention Syndrome. Anxiety and depressive symptoms presented by this subset of subjects were primarily attributed to a core irrational belief and a cognitive error centered around misunderstood concepts of semen physiology. Consequently, the undue focus on mood idioms by both white British patients and their health professionals, leads to a mistaken diagnosis of Mood Disorder, and results in incorrect treatment. The implications of this ethnocentric mode of reasoning raises concerns about existing concepts in psychiatric phenomenology and for official international diagnostic classificatory systems. The paper concludes by arguing that category errors in both directions are instances of cultural iatrogenesis, and underscore the importance of a culturally valid psychiatry.
_________________________
I was unable to find support for any of the above-listed effects of semen retention. So, claims like “Semen Retention is life-changing, especially for men. Not only, it help you turn into a real alpha male but also offers great health benefits” need to be taken with a pinch of salt. Yet, it did occur to me that semen retention might have one positive outcome:
It reduces the chances of stupid people multiplying!
It has been reported, at the German Medical Congress (DÄT) a year ago, that it was decided to delete the additional title of homeopathy from the model further training regulations of the German Medical Association. And Federal Health Minister Karl Lauterbach (SPD) tweeted applause: “Homeopathy has no place in modern medicine.”
Now the ‘ Bundesverband der Pharmaziestudierenden in Deutschland’ (BPhD), the German Pharmacists Organization, even goes a few steps further. The position paper distinguishes between evidence-based medicine (EBM) and unproven therapeutic methods. According to the BPhD, these include homeopathy, but also anthroposophy, traditional Chinese medicine, and traditional medicines.
Among other things, the BPhD is disturbed by the way homeopathy presents itself as an alternative, because an alternative means “a choice between two equally suitable possibilities” to achieve a goal, and this is not the case. Compared to evidence-based medicine (EBM), homeopathy is a “constructed, illusory concept” and “the principles of homeopathic teachings and principles” are to be rejected as “unscientific”. According to the BPhD, a designation as “alternative” for advertising purposes should no longer be allowed.
They would also like to see a demarcation from naturopathy; the clear distinction between homeopathy and phytopharmacy has been lacking up to now. The advertising attribute “natural” should therefore also be banned in order to prevent equalization in advertising, the position paper states.
Like doctors, pharmacy students point to the lack of proof of efficacy beyond the placebo effect. According to the BPhD, the dogma WER HEILT HAT RECHT, “he who heals is right” would “disregard all processes that work towards healing and glorify the result”. The “gold standard” of EBM – randomized, double-blind studies with placebo control – should in future also have to be fulfilled by homeopathic medicines, experience reports are not sufficient, it continues.
Homeopathic medicines are only registered as medicinal products without indication, which requires neither proof of efficacy nor clinical studies. The BPhD, therefore, demands that a warning be placed on the preparations that they have “no proven efficacy beyond the placebo effect”. Up to now, without this warning, patients have been “deceived about the efficacy”, and there is an “urgent need for detailed public information and counseling on homeopathy since its unjustified reputation poses a danger of not seeking treatment”. The BPhD also demands that the status of homeopathic medicines is withdrawn and that the pharmacy obligation for the preparations is abolished…
“In the health professions, no trivialization of unproven therapeutic procedures should be tolerated, as inadequate counseling or ignorance poses a danger to patients,” the BPhD said.
_________________________
When I first read this article – I translated and shortened it for those who cannot read German- I was truly dazzled. These are the suggestions that I have been making for around 20 years now, not specifically for Germany but for pharmacists in general. For many years, the Germans seemed the least likely to agree with me. But now they seem to be ahead of everyone else in Europe!
How come?
I suspect and hope that our recent initiative might have something to do with it.
Let’s hope that the pharmacists of other countries follow the German example.
It has recently been reported that a 39-year-old woman (a mother-of-three died) died after immersing herself in a river as part of a cold water therapy session. The woman died after paramedics were called to attend a riverside in Derbyshire. The session was run by Kevin O’Neill of ‘Breatheolution’, whose previous clients include Coleen Rooney and actor Stephen Graham. The woman, who was visiting with two friends after paying up to £200 for a two-hour cold water therapy session, was rushed to hospital where she died.
Mr. O’Neill commented: “I am heartbroken. I’ve not slept and I’m finding it hard to process. I cannot stop thinking about her family. It’s tragic.” An inquest is expected to be opened into the woman’s death. East Midlands Ambulance Service said they were called to Bankside, in Bridgemont. “The caller reported a medical emergency,” a spokesperson said. “We sent a paramedic in a fast response car and a double-crewed ambulance. The air ambulance was also in attendance.”
Derbyshire Fire and Rescue Service, which was called to assist the paramedics, has warned people about the dangers of entering open water. “While we cannot and will not comment or speculate on the circumstances and cause of this tragic death, we would like to remind people of the dangers of entering open water and cold water shock,” said group manager Lee Williams.
_____________________
Breatheolution’ has a website where a whole page is dedicated to its leader Kevin O’Neill. I wondered what qualifications Kevin has, but all it tells us about him is this: “I struggled for so long with alcohol and other substance abuse that something had to give, I lost my sister Yvonne in 2019 and I think it was enough trauma to make me think a lot more about my own life”
The website also explains what the cold water sessions are about:
1-2-1 Breath Coaching, practice & Cold water session (river or tank)
2 hours @ £110.00
These sessions are proving popular with those who are not keen on group sessions or just prefer to have a more personal experience. The 2-3 hour sessions will be tailored to you and your breathing and will include potentially life-changing tools and methods to allow you to witness your breathing and physiology differently in the future, its all about feeling and awareness.
Another section of the site is dedicated to celebrities who Kevin seems to have treated. And then there is a video of the treatment. What I did not find anywhere, however, are the conditions that Kevin claims to treat with his cold water therapy.
In any case, it would have been wise for Kevin to read up about the risks of cold water immersion (CWI) before going into business. Perhaps this review would have helped:
In 2012, an estimated 372,000 people (42 per hour) died from immersion, assumed to be drowning. Immersion is the third leading cause of unintentional injury-related death, accounting for 7% of all such deaths (World Health Organization, 2014). These figures are underestimations owing to poor reporting in many Third World countries that have a high number of deaths. The data also do not include life-long morbidity caused by immersion-related injuries, estimated to be a much bigger numerical problem.
There is no strict definition of ‘cold water’. Given that some of the hazardous responses to cold water appear to peak on immersion somewhere between 15 and 10°C, it is reasonable to say that cold water is water <15°C (Tipton et al. 1991). However, the thermoneutral water temperature for a resting naked individual is ∼35°C, so it is possible for individuals to become very cold, with time, on immersion in water below this temperature. The corresponding temperature for those exercising (including shivering) is ∼25°C (Tipton & Golden, 1998).
Historically, the threat associated with CWI was regarded in terms of hypothermia or a reduction in deep body temperature below 35°C. This belief was established as a result of the Titanic disaster and supported by data obtained during maritime conflicts of World War II. However, more recently, a significant body of statistical, anecdotal and experimental evidence has pointed towards other causes of death on immersion. For example, in 1977 a Home Office Report revealed that ∼55% of the annual open water deaths in the UK occurred within 3 m of a safe refuge (42% within 2 m), and two-thirds of those who died were regarded as ‘good swimmers’. This evidence suggests more rapid incapacitation than can occur with whole-body cooling and consequent hypothermia.
The following four stages of immersion have been associated with particular risks (Golden & Hervey, 1981; Golden et al. 1991); the duration of these stages and the magnitude of the responses evoked within them vary significantly, depending on several factors, not least of which is water temperature:
- Initial immersion (first 3 min), skin cooling;
- Short-term immersion (3 min plus), superficial neuromuscular cooling;
- Long-term immersion (30 min plus), deep tissue cooling (hypothermia); and
- Circum-rescue collapse: immediately before, during or soon after rescue.
As a result of laboratory-based research, the initial responses to immersion, or ‘cold shock’, were identified as particularly hazardous (Tipton, 1989), accounting for the majority of immersion deaths (Tipton et al. 2014). These deaths have most often been ascribed to drowning, with the physiological responses of a gasp and uncontrollable hyperventilation, initiated by the dynamic response of the cutaneous cold receptors, resulting in the aspiration of the small volume of water necessary to initiate the drowning process (Bierens et al. 2016). Relatively little is known about the minimal rates of change of cold receptor temperature necessary to cause cold shock. The response has been reported to begin in water as warm as 25°C but is easy to suppress consciously at that temperature. In laboratory conditions, the respiratory frequency response (an indication of respiratory drive) peaks on naked immersion in a water temperature between 15 and 10°C, and is no greater on immersion in water at 5°C (Tipton et al. 1991). The corresponding average rates of change of chest skin temperature over the first 20 s of these immersions was 0.42 (water temperature 15°C), 0.56 (water temperature 10°C) and 0.68°C s−1 (water temperature 5°C). This suggests that an average rate of change in chest skin temperature between 0.42 and 0.56°C s−1 on the first 20 s of immersion is sufficient to evoke a maximal respiratory cold shock response.
More recently, it has been suggested (Shattock & Tipton, 2012) that a larger number of deaths than once thought may be attributable to arrhythmias initiated on immersion by the coincidental activation of the sympathetic and parasympathetic division of the autonomic nervous system by stimulation of cutaneous cold receptors around the body [sympathetic activation (cold shock)] and in the oronasal region on submersion or with wave splash [vagal stimulation (diving response)]. This ‘autonomic conflict’ is a very effective way of producing dysrhythmias and arrhythmias even in otherwise young and healthy individuals, particularly, but not necessarily, if a prolonged breath hold is involved in the immersion (Tipton et al. 1994). It seems that predisposing factors, such as long QT syndrome, ischaemic heart disease or myocardial hypertrophy, are necessary for fatal arrhythmias to evolve (Shattock & Tipton, 2012); many of these factors, including drug-induced long QT syndrome, are acquired. Non-fatal arrhythmias could still indirectly lead to death if they cause incapacitation and thereby drowning (Tipton, 2013). The hazardous responses associated with the cold shock response are presented in Fig. 2.
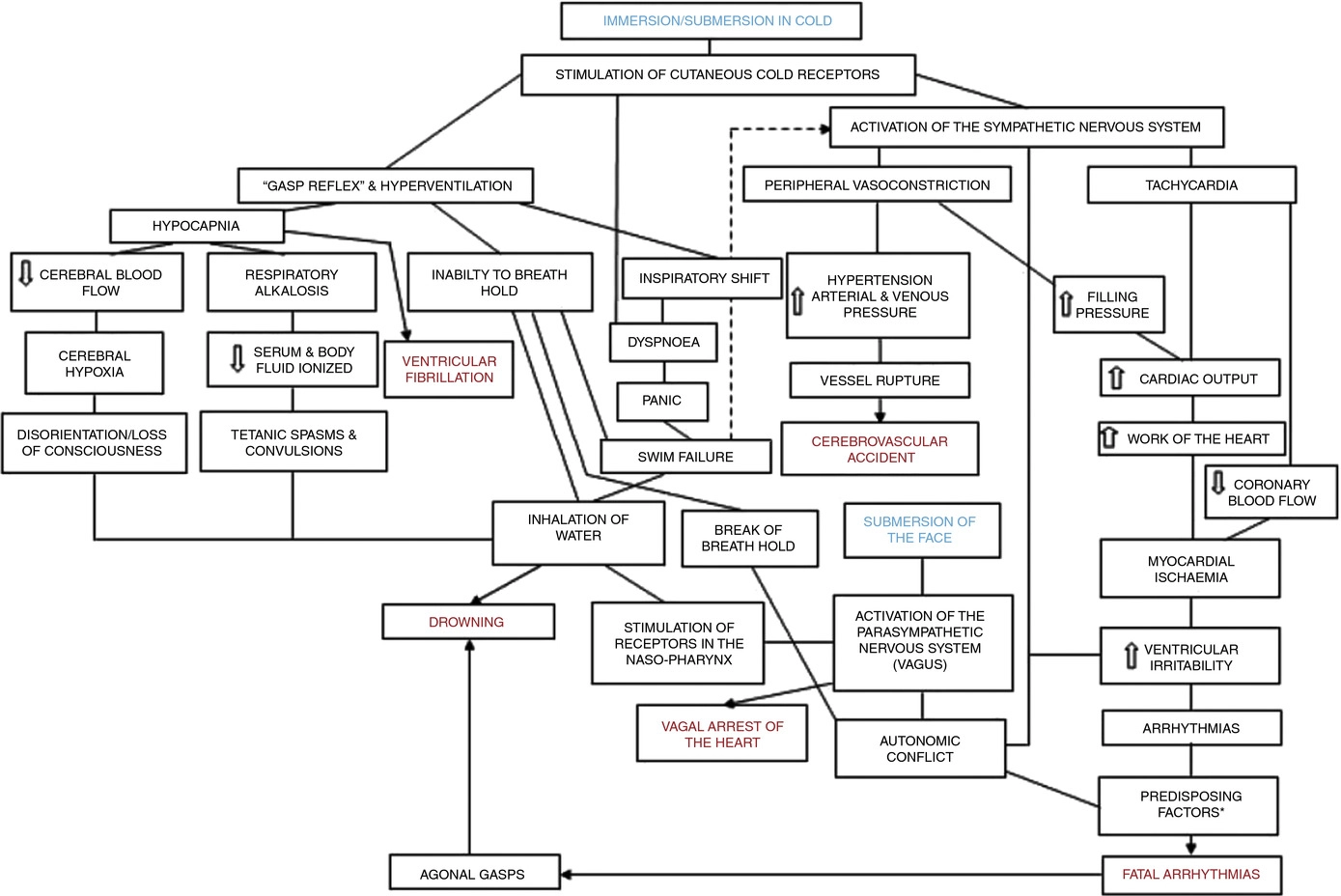
Figure 2. A contemporary view of the initial responses to immersion and submersion in cold water (‘cold shock’)
The problems encountered in short-term immersions are primarily related to physical incapacitation caused by neuromuscular cooling (Castellani & Tipton, 2015). The arms are particularly susceptible because of their high surface area to mass ratio. Low muscle temperatures affect chemical and physical processes at the cellular level. This includes metabolic rate, enzymatic activity, calcium and acetylcholine release and diffusion rate, as well as the series elastic components of connective tissues (Vincent & Tipton, 1988). Maximal dynamic strength, power output, jumping and sprinting performance are related to muscle temperature, with reductions ranging from 4 to 6% per degree Celsius reduction in muscle temperature down to 30°C (Bergh & Ekblom, 1979). At nerve temperatures below ∼20°C, nerve conduction is slowed and action potential amplitude is decreased (Douglas & Malcolm, 1955). Nerve block may occur after exposure to a local temperature of between 5 and 15°C for 1–15 min. This can lead to dysfunction that is equivalent to peripheral paralysis and can, again, result in drowning owing to the inability to keep the airway clear of the water (Clarke et al. 1958; Basbaum, 1973; Golden & Tipton, 2002; Fig. 3).
Figure 3. The ‘physiological pathways to drowning’ after immersion or submersion in cold water, with possible interventions for partial mitigation (dashed)
Abbreviations: EBA, emergency breathing aid; IS, immersion suit; and LJ, lifejacket. Reproduced with permission, from Tipton (2016b).
Even in ice-cold water, the possibility of hypothermia does not arise for at least 30 min in adults. Hypothermia affects cellular metabolism, blood flow and neural function. In severe hypothermia, the patient will be deeply unconscious. The progressive signs and symptoms (approximate deep body temperature) are shivering (36°C), confusion, disorientation, introversion (35°C), amnesia (34°C), cardiac arrhythmias (33°C), clouding of consciousness (33–30°C), loss of consciousness (30°C), ventricular fibrillation (28°C) and death (25°C) (Bierens et al. 2016). There is great variability between deep body temperature and the signs and symptoms of hypothermia. For example, although the deep body temperature associated with death is often quoted as 25°C, the lowest temperature recorded to date after accidental exposure to cold (air) and with full recovery was 12.7°C in a 28-month-old child (Associated Press, 2014). The coldest adult survivor of CWI followed by submersion had a body temperature of 13.7°C (Gilbert et al. 2000). There is also a large amount of variation in the rate at which people cool on immersion in cold water, owing to a combination of thermal factors (including water temperature and water movement, internal and external insulation) and non-thermal factors (including body size and composition, blood glucose, motion illness, racial and sex differences; Haight & Keatinge, 1973; Gale et al. 1981; White et al. 1992; Mekjavic et al. 2001; Golden & Tipton, 2002).
The most significant practical consequence of hypothermia in water is loss of consciousness; this prevents individuals from undertaking physical activity to maintain a clear airway and avoid drowning. Thus, once again, drowning is often the end-point (Fig. 3).
About 17% of those who die as a result of immersion die immediately before, during or after rescue (Golden et al. 1991). The deaths immediately before rescue are intriguing and probably related to behavioural changes at this time or the relief and psychophysiological alterations associated with imminent rescue, including a reduction in circulating stress hormone concentration and an increase in vagal tone. Death during rescue is most commonly associated with a collapse in arterial pressure when lifted vertical from the water and kept in that position for some time (Golden et al. 1991).
_____________________________
The tragic death of the woman should perhaps remind us that
- there is no SCAM or wellness treatment that is entirely harmless,
- and there are only few ‘would-be gurus’ who know what they are doing.


